Abstract
One of the most intriguing aspects of male reproductive physiology is the ability to generate spermatogenic cells - which are “foreign” to the host - without triggering immune activation. After leaving the testis, spermatozoa enter the epididymis where they mature and are stored. We report here a previously unrecognized dense network of dendritic cells located at the base of the epididymal epithelium. This network was detected in transgenic mice expressing CD11c-EYFP and CX3CR1-GFP reporters. Epididymal dendritic cells (eDCs) establish intimate interactions with the epithelium and project long dendrites between epithelial cells toward the lumen. We show that isolated eDCs express numerous leukocyte markers described previously in other organs that are in contact with the external environment, and present and cross-present ovalbumin to T cells in vitro. eDCs are, therefore, strategically positioned to regulate the complex interplay between immune tolerance and activation, a balance that is fundamental to male fertility.
Introduction
Although a significant proportion of male infertility cases are thought to have an immunological cause (Stedronska & Hendry 1983, Pattinson & Mortimer 1987, McLachlan 2002, Meinhardt & Hedger 2010), the cellular and molecular basis of immune regulation in the epididymis – the site of sperm maturation and storage - remains poorly understood. The establishment and maintenance of male fertility requires close and tightly regulated interactions between the reproductive, endocrine and immune systems. Spermatozoa acquire motility and the ability to fertilize an egg during their transit in the epididymis, a single, long and convoluted duct with a large epithelial-luminal interface located downstream of the testis. Post-testicular sperm maturation involves numerous mechanisms mediated by the pseudostratified epithelium that lines the epididymis, including protein secretion and reabsorption, as well as fluid and ion exchanges (Da Silva et al. 2007, Cornwall 2009, Shum et al. 2009). One of the most striking characteristics of spermatozoa is their immunological status: post-meiotic germ cells start expressing new surface and intracellular molecules at puberty, long after the establishment of systemic immune tolerance. They are, therefore, foreigners in the environment in which they were produced (Fijak & Meinhardt 2006, Hedger & Hales 2006). Despite this apparent paradox, they are tolerated and even pampered all along the excurrent duct (efferent ducts, epididymis, vas deferens and ejaculatory ducts), as they are prepared to face the challenging environment of the female genital tract. The immunological status of spermatozoa would not be particularly intriguing if the barriers lining the male reproductive system were totally efficient, but the physical separation between the immune system and germ cells is far from perfect (Pelletier 1994, Pollanen & Cooper 1994, Levy & Robaire 1999, Hedger & Hales 2006). In addition, the male reproductive tract is contiguous with the external environment and, therefore, continuously challenged by potential pathogenic microorganisms and viruses. Inflammation of the epididymis can cause obstruction or destruction of the duct leading to transient or permanent infertility (Chan & Schlegel 2002, Cunningham & Beagley 2008). Yet the mechanisms that prevent the development of an autoimmune response against millions of autoantigenic spermatogenic cells and mature spermatozoa, while maintaining the ability to initiate efficient immune responses against pathogenic microorganisms and cancer cells, are still superficially understood. These mechanisms have been studied mostly in the testis (Meinhardt & Hedger 2010), largely underestimating the immune function of the epididymis and the post-testicular environment in general. Intraepithelial lymphocytes and other immunocompetent cells have been observed in the epididymis (Ritchie et al. 1984, Nashan et al. 1989, Barratt et al. 1990, Nashan et al. 1990, Tomlinson et al. 1992, Nashan et al. 1993, Yeung et al. 1994, Hooper et al. 1995, Flickinger et al. 1997, Rossi & Aitken 1997, Serre & Robaire 1999), but the precise nature of these cells and their immunological properties remain to be elucidated. Dendritic cells (DCs), the specialized antigen-presenting cells (APCs) that are key regulators of immune responses in numerous organs (Banchereau & Steinman 1998, Steinman et al. 2003, Steinman & Banchereau 2007, Helft et al. 2010), are thought to be absent from the epididymal epithelium (Seiler et al. 2000). Here, we describe a surprisingly extensive network of stellate cells visualized in the epididymis of CD11c-EYFP (Lindquist et al. 2004) and CX3CR1-GFP (Jung et al. 2000) reporter mice. Based on their striking dendriform morphology, their intimate interactions with the epididymal epithelium, their phenotype and antigen-presenting capabilities, we named these cells “epididymal dendritic cells” (eDCs). eDCs and other cells from the mononuclear phagocyte system are ideally positioned to play a major role in male reproductive physiology and pathophysiology. Unraveling their function in the unique environment constituted by the epididymis may also help to better understand the mechanisms of tolerance and autoimmunity in male reproductive function.
Results
CD11c+ and CX3CR1+ DCs cells form a dense network localized at the base of the epididymal epithelium
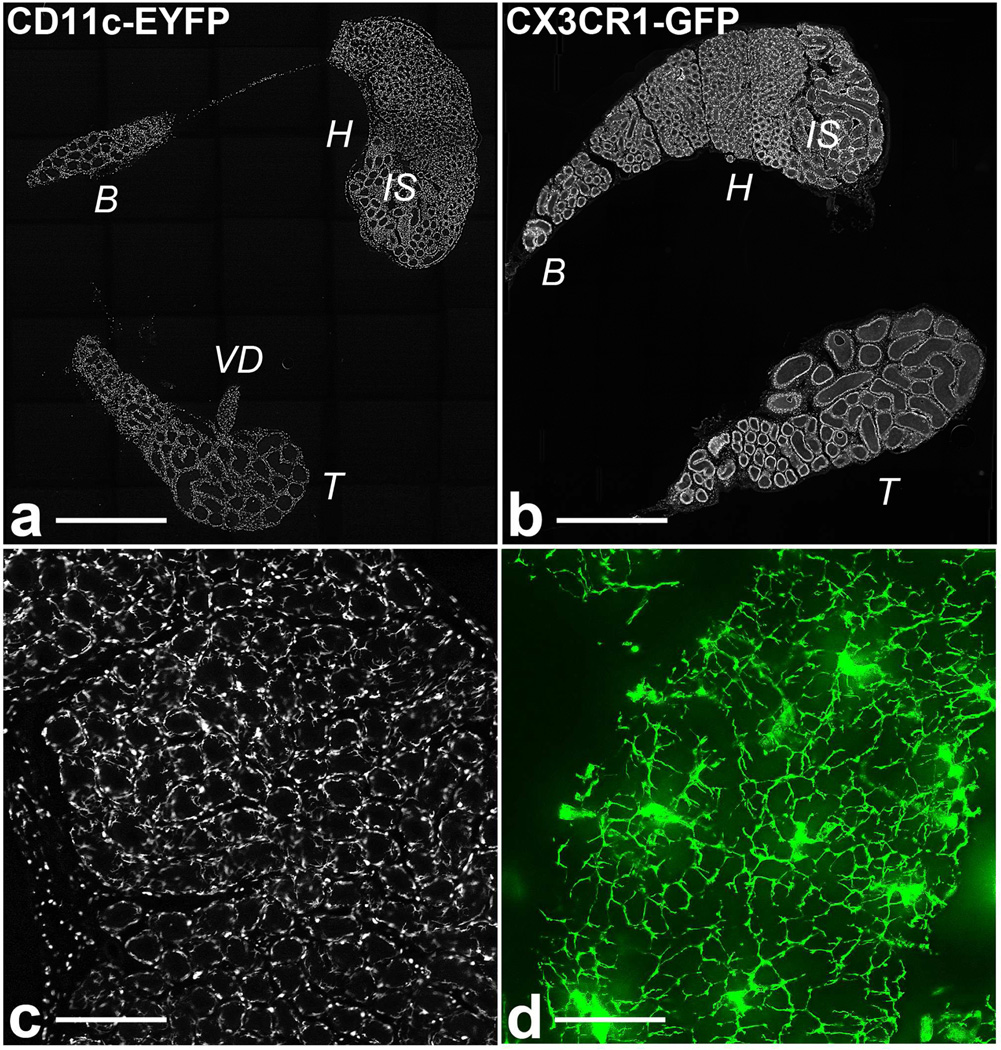
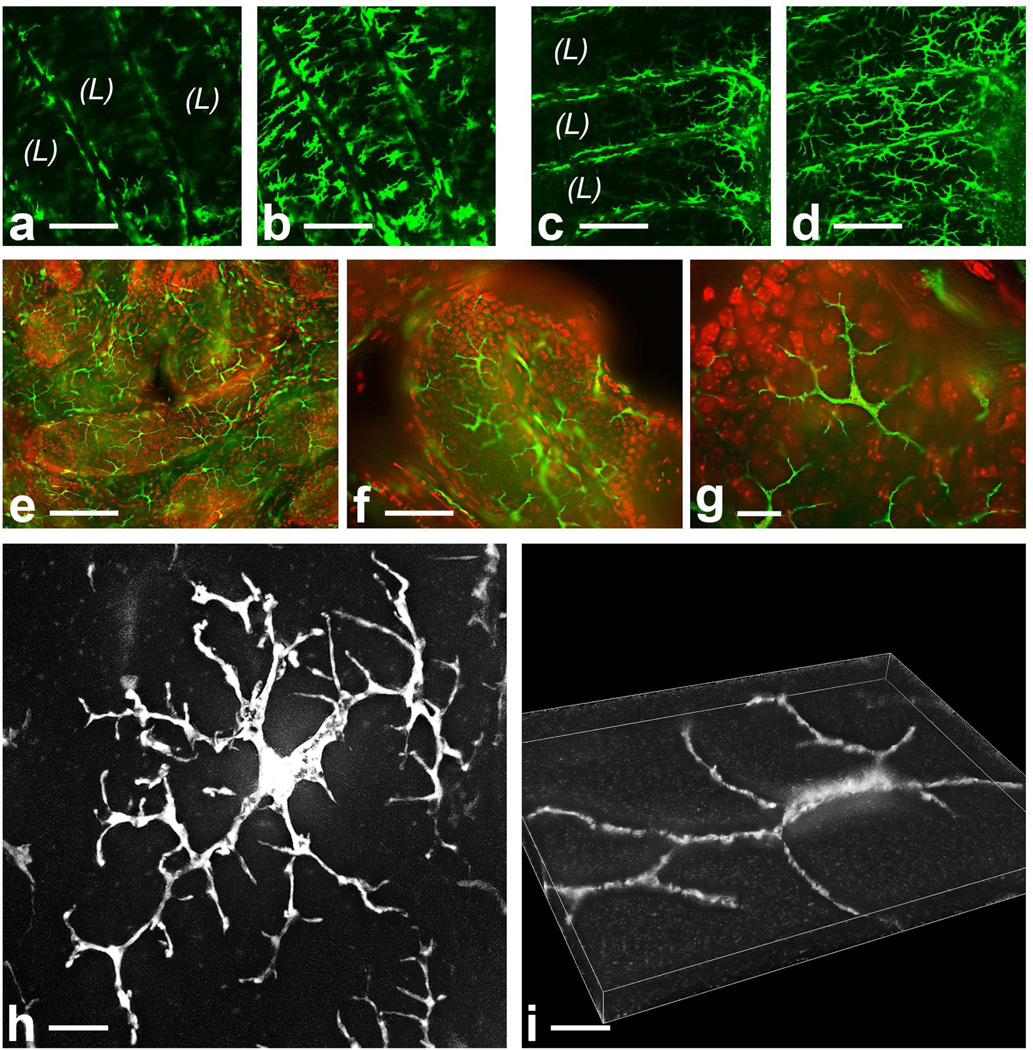
We examined 50-µm sections of epididymis from CD11c-YFP and CX3CR1-GFP adult mice by fluorescence microscopy and generated large mosaic images representing complete sections of the entire organ (Fig.1 and Supplementary Figures 1 and 2). The epididymis is a continuous tubule, but a portion of the body (or corpus), which is very narrow, is often absent from thick sections. The entire murine epididymis is heavily populated by a network of CD11c-YFP+ and CX3CR1-GFP+ DCs (Fig. 1a, b, respectively), located mostly in the peritubular region (Fig.1 c and d). In the proximal epididymis, eDCs exhibit numerous ramifications that cover the basal side of the epithelium (Fig. 1d). To better examine the distribution and the morphology of eDCs, we generated high magnification epifluorescence and confocal pictures of live (examined within 15 min after dissection) and fixed tissue sections. Most, if not all, eDCs have a stellate / dendriform morphology and are located at the base of the epithelium (Fig. 2). CD11c+ (Fig. 2a, b, h) and CX3CR1+ (Fig. c-g) cell morphology and distribution appear very similar, but our microscopic analysis cannot rule out that these transgenes may, in fact, highlight several overlapping subsets of cells in the epididymis. In addition, eDCs are more ramified in the proximal epididymis (head, Fig. 2h) than in the distal segment (tail, Fig. 2i).
Figure 1.
The epididymis is densely populated by CD11c+ and CX3CR1+ cells. (a and b) “mosaic” pictures of whole CD11c-EYFP and CX3CR1-GFP mouse epididymis sections, respectively. IS: initial segments, H: head (caput), B: body (corpus), T: tail (cauda), VD: vas deferens. (c and d) higher magnification pictures of the initial segments, showing numerous CD11c-EYFP+ cells located at the periphery of the epididymal tubule. Bars = 2 mm (a and b), 250 µm (c) and 50 µm (d). High-resolution pictures for panels a and b are available online (online material S1 and S2).
Figure 2.
Epididymal CD11c+ and CX3CR1+ cells are peritubular and have stellate/dendriform morphology. (a-d) Visualization of CX3CR1-GFP+ and CD11c-EYFP+ eDCs using live cell confocal microscopy. Unfixed tissue slices were observed within 15 minutes after dissection. (a and b) and (c and d) represent 2 confocal planes of the same field in CD11c-EYFP and CX3CR1-GFP tissues, respectively. The lumen (L) is populated by spermatozoa that are invisible in these pictures; eDCs are located at the periphery of the epididymal tubule (e-g). Conventional fluorescence microscopy visualization of CX3CR1-GFP-positive eDCs (20, 40 and 60X objectives, respectively). Nuclei were stained (red) to better appreciate the organization of the tissue. (h and i) High magnification pictures of CD11c-EYFP+ cells in caput and cauda epididymidis, respectively, showing the distinctive morphology of eDCs in these regions. Cells are more ramified in the head compared to the tail. Bars = 100 (a-e), 50 (f) and 10 µm (g-i).
eDCs project numerous intraepithelial processes in the proximal epididymis
High-resolution fluorescence cross-section images (Fig. 3a and Supplementary Movie 1) revealed that eDCs project slender processes (diameter < 1µm) between epithelial cells, toward the lumen. 3D reconstruction showed that the dendritic cell bodies lie on the basal surface of the epithelium and send narrow projections that run along the basal axis of the epithelium (Fig. 3b). Perpendicular dendritic processes arise from these projections (Supplementary Movie 2) and plunge deeply between the epithelial cells. A single eDC can survey a considerable region (up to 10,000 sq µm) (Fig. 2h and 3c) and can project up to 40 processes that penetrate the lateral compartment of the epithelium (Fig. 3d). Intraepithelial dendrites that extend toward the tightjunction barrier of the epithelium (visualized using a ZO-1 immunolabeling) are visible primarily in the initial segments (Fig. 3e). In the distal epididymis (tail), eDCs are flat and interact with the basal surface of the epithelium, but they do not project visible intraepithelial dendrites (Fig. 2i and 3f). Occasionally, some CD11c-GFP+ and CX3CR1+ cells appear to be embedded within the epithelium rather than being exclusively peritubular (not shown).
Figure 3.
In the proximal epididymidis, eDCs project thin processes toward the epididymal lumen. (a) Cross section of the epididymal duct of a CD11c-EYFP mouse (initial segments) showing numerous intraepithelial dendrites converging toward the lumen (L). (b) Three-dimensional view of a CD11c-EYFP+ eDC, showing the bright cellular body, long lateral extensions (arrows) and slender transepithelial processes (arrowheads). (c and d) Two optical sections of epididymal CD11c-EYFP+ DCs taken at different depths. (c) The section runs through the cellular body of one DC (arrow), which has numerous lateral extensions. (d) The perpendicular intraepithelial processes appear as circular dots (arrowheads) in this section taken closer to the lumen. (e) Cross-section of the epididymal duct (initial segments) showing CX3CR1-GFP+ eDCs (green) projecting processes toward the tight junctions labeled with ZO-1 (red). In contrast, DC do not project visible intraepithelial dendrites in the epididymis tail (f). E: epithelium. Blue = DAPI. Bars = 10 µm (a-e) and 20 µm (f).
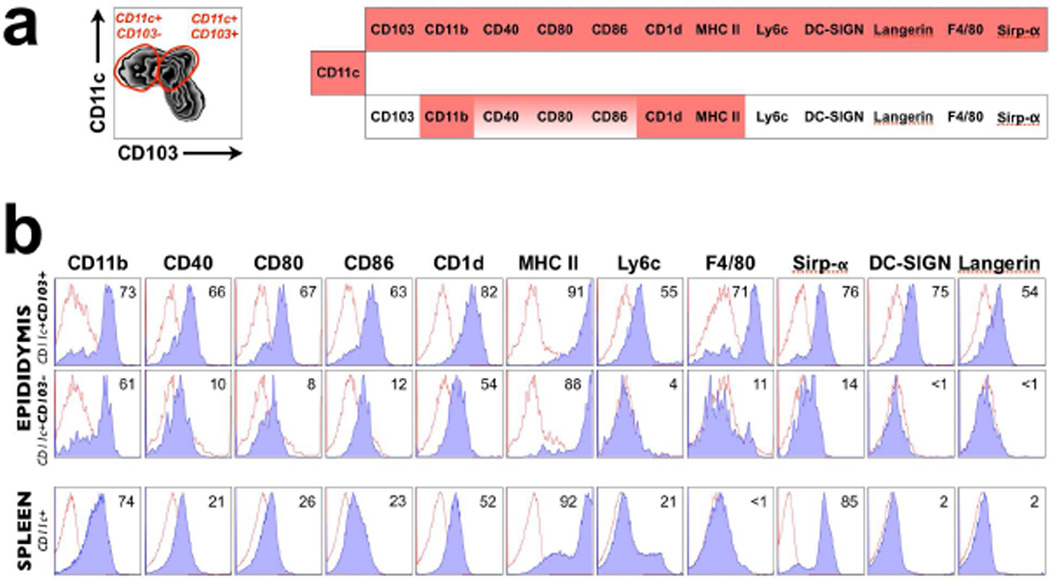
Phenotype of eDCs
Next, we phenotyped eDCs with antibodies against surface markers typically used for the characterization of leukocytes and APCs (Choi et al. 2009, Ginhoux et al. 2009, Miloud et al. 2010). Our preliminary flow cytometry analyses showed that most epididymal CX3XR1-GFP+ cells express CD11c (Supplementary Figure 3). To exclude any possible abnormality of the phenotype and/or number of DCs in transgenic animals, we performed all the subsequent analyses with wild type C57BL/6 mice. We identified two major populations of eDCs: CD11c+ CD103+ eDCs and CD11c+ CD103− eDCs (Fig. 4a). Both populations of eDCs express CX3CR1 and MHC class II molecules, similar to DCs in the small intestine (Niess et al. 2005). Epididymal CD11c+ cells share numerous similarities with the so-called “classical” DCs (tissue-resident steady-state DCs) described in other non-lymphoid organs such as the gut, lung, skin and aorta (Choi et al. 2009, Helft et al. 2010). As such, CD11c+ CD103+ cells express CD11b and the co-stimulatory molecules CD40, CD80 and CD86, as well as CD1d and the macrophage marker F4/80 (Fig. 4a and 4b). They also express Ly6C, the C-type lectins langerin and DC-SIGN, as well as the signal regulatory protein alpha, Sirp-α, which interacts with CD47 to regulate immune homeostasis (Barclay 2009, Matozaki et al. 2009). In contrast, CD11c+ CD103− eDCs express lower or undetectable levels of co-stimulatory molecules, Ly6C, DC SIGN, langerin, F4/80 and Sirp-α, but express CD1d, MHC class II and, surprisingly, CD11b (Fig. 4a and 4b). Splenic DCs (Fig. 4b, bottom row) express lower levels of co-stimulatory molecules when compared with CD103+ eDCs, indicating their less mature status, and insignificant levels of Ly6C, F4/80, DC-SIGN and langerin.
Figure 4.
Flow cytometry analysis of cell surface markers in epididymal and splenic DCs isolated from C57BL/6 mice. Cell suspensions were prepared from C57BL/6 mouse whole epididymis and spleen and stained with monoclonal antibodies to 13 markers. (a) Recapitulation of the phenotype of 2 major CD11c+ eDC populations that express or do not express CD103 (gated from the histogram shown on the left). (b) Representative histograms of the phenotype of epididymal and splenic DCs. The percentage represents the mean of at least two independent experiments. Red histograms represent isotype controls
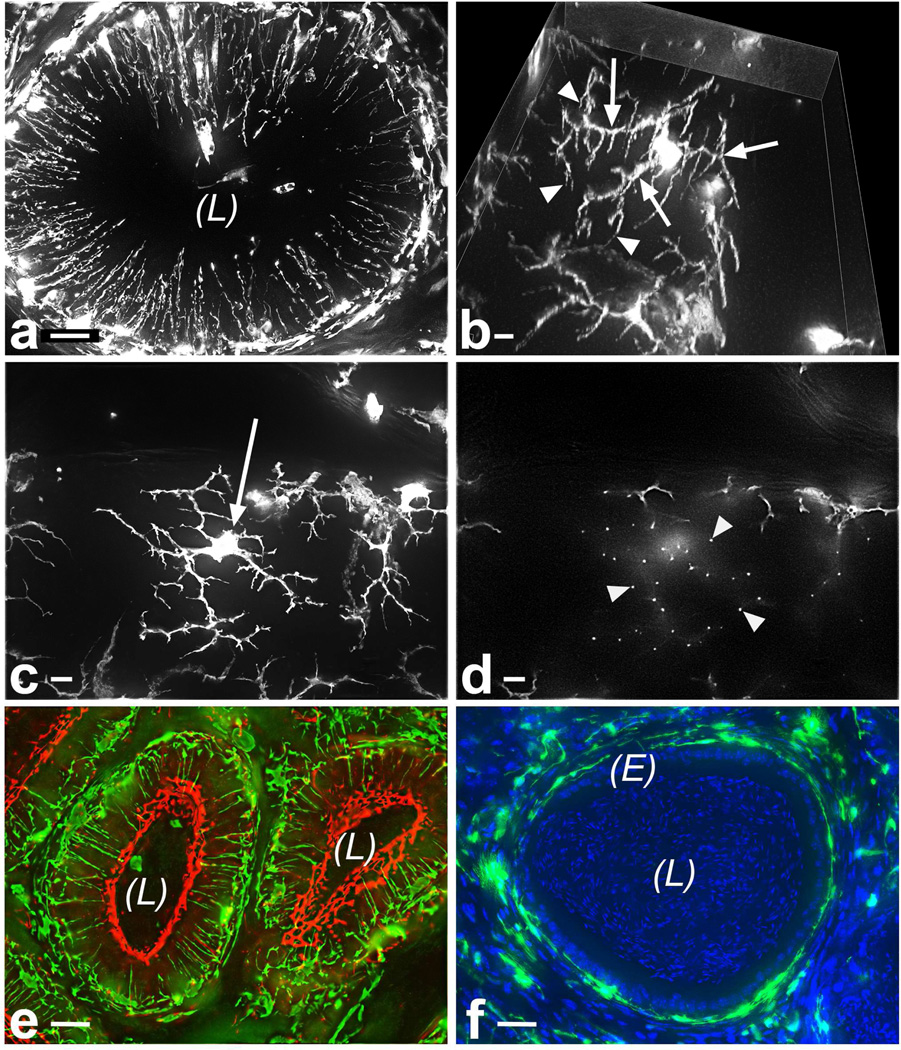
Expression of macrophage markers in the epididymis
DCs and macrophages belong to the notably heterogeneous mononuclear phagocyte system (MPS), and the distinction between these two cell types is still controversial (Geissmann et al. 2010). The expression of F4/80 (a macrophage marker involved in the induction of peripheral tolerance (Lin et al. 2005)) in CD11c-positive cells led us to refine the analysis of macrophage markers in the epididymis by immunofluorescence microscopy. CD11c-EYFP and the F4/80 antibody revealed three distinct populations of cells that express one marker or both (Fig 5a-e). In addition, the mannose receptor (CD206) is expressed exclusively by a population of CD11c-negative cells that are located in the interstitium and are morphologically distinct from the peritubular eDCs (Fig. 5f). Higher magnification pictures clearly showed that CD11c+ and CD206+ cells are distinct populations (Fig. 5g, h). Thus, the epididymal tubule and interstitium are populated by several subsets of mononuclear phagocytes that express a complex combination of markers traditionally described as “dendritic cell” or “macrophage” markers.
Figure 5.
Expression of macrophage markers in the epididymis. F4/80 immunolabeling of CD11c-EYFP mouse epididymis revealed 3 subsets of cells that express CD11c (green), F4/80 (red), or both markers (yellow). CD11c-F4/80+ cells (a, c, e, arrowheads) tend to be more interstitial than CD11c+F4/80− cells. However, high magnification pictures d and e show that cells positive for both markers are also present in the peritubular region. (f-h): the macrophage marker CD206 (mannose receptor) is expressed exclusively by interstitial cells. Sections of CD11c-EYFP (green) mouse epididymis were immunolabeled with an anti-CD206 antibody (red). While CD11c+ cells are located mostly in the peritubular region, the CD206+ macrophages are exclusively interstitial. Higher magnification (h) reveals the non-stellate morphology of interstitial CD206+ cells, contrasting with eDCs (green). DNA staining (in a, blue) helps to appreciate the structure of the tissue, with rows of nuclei from epithelial cells (E) and luminal nuclei from spermatozoa. Bars = 50 (a-c, f), 25 (g) and 10 µm (d, e, h). L = lumen.
eDCs are effective antigen-presenting cells in vitro
A prerequisite for any putative role in reproductive immunophysiology is the ability of eDCs to present antigens to T cells. Therefore, we determined the antigen presentation capabilities of isolated eDCs in vitro by culturing them with chicken ovalbumin (OVA) -specific OT-I and OT-II transgenic T cells, in the presence or absence of OVA, and by assessing for T cell proliferation. In the presence of OVA, CD11c+ CD11b+ eDCs induced strong proliferation of CD4+ (82% proliferating cells) and CD8+ (53%) OVA-specific T cells (Fig. 6, left panels). As control, the effect of splenic DC on T cell proliferation was examined. Splenic DCs induced CD4+ and CD8+ T cell proliferation by 90 and 80%, respectively (Fig. 6, right panels). Thus, isolated eDCs appear to be very effective at processing and presenting antigens to CD4+ and CD8+ T cells in vitro.
Figure 6.
In vitro antigen presentation to T cells by epididymal and splenic DCs. CD11b+ CD11c+ DCs were isolated from C57BL/6 epididymis and spleen by FACS, as well as CD4+ OTII and CD8+ OT-I T cells. DCs and CFSE-labeled T cells were cocultured for 5 days in the presence (blue) or absence (red) of OVA protein. Proliferation of T cells was assessed by flow cytometry. The percentage of proliferating cells is indicated in blue. Histograms are representative of two independent experiments.
Discussion
In order to perpetuate the species, all male amniotes have developed an epididymis, a small organ located downstream of the testis that is responsible for making gametes able to fertilize an oocyte and storing them (Da Silva et al. 2007, Cornwall 2009, Shum et al. 2009). Sperm maturation and proper storage involve complex mechanisms, which are regulated by the pseudostratified epithelium that lines the entire excurrent ductal system and is under the control of the endocrine system (Ezer & Robaire 2002, Hess et al. 2002, Robaire et al. 2007, Cornwall 2009, Shum et al. 2009). Surprisingly, one of the most understudied aspects of epididymal physiology is its interaction with the immune system (Hedger & Hales 2006). The epididymal mucosal system must protect autoantigen-coated spermatozoa from destruction by the immune system as well as invading pathogens. Dendritic cells (DCs), the specialized antigen-presenting cells (APCs) that are key regulators of immune responses in numerous organs (Banchereau & Steinman 1998, Steinman et al. 2003, Steinman & Banchereau 2007, Helft et al. 2010), had been thought to be absent from the epididymal epithelium in order to prevent immune activation (Seiler et al. 2000). However, we describe here an extensive network of dendritic cells and macrophages that populate the entire organ and seem to be strategically positioned to actively regulate the interactions between the reproductive and immune systems. Two transgenic mouse models, which have been widely used to characterize DCs in numerous organs, revealed the presence of CD11c+ and CX3CR1+ cells that establish close contact with the epididymal epithelium.
The mouse epididymis is a continuous but segmented organ that has at least two clearly distinct functions: spermatozoa mature mostly in the most proximal segments (head), while the distal regions (body and tail) are also sites of storage. Although all epididymal DCs express the markers CD11c and CX3CR1, we show here that intraepithelial dendrites are particularly abundant in the initial segments. These cells resemble the F4/80+ cells observed by Mullen et al., although all the epididymal leukocytes described by this group were CD11b-negative (Mullen et al. 2003). In the initial segments, most, if not all, epithelial cells seem to be in direct contact with an eDC, and we determined that each eDC extends dozens of intraepithelial dendrites toward the tight junctions that constitute the so-called blood-epididymis barrier. This portion of the tubule is the first segment encountered by spermatozoa after their short transit in the efferent ducts. The initial segments are, therefore, likely to play a primary role in the acceptance of maturing sperm cells by the immune system. Interestingly, the initial segments are also the most vascularized region of the epididymis (Suzuki 1982, Abe et al. 1984) and, consequently, the most readily accessible region for blood-borne differentiated cells and/or progenitors. In addition, the lumen in these segments is relatively narrow (its diameter represents about one tenth of the tubular diameter in the distal epididymis tail), which increases the probability of direct interactions between spermatozoa, epithelial cells, and any cell type capable of projecting intraluminal extensions such as basal cells (Shum et al. 2008) and, possibly, DCs (Niess et al. 2005) and other leukocytes (Mullen et al. 2003). Finally, the initial segments are the region of the epididymis that is least likely to be infected by ascending pathogens. It has been suggested that the CX3CR1-expressing intestinal DCs with transepithelial sampling capabilities are essentially macrophages involved in maintaining the mucosa rather than initiating T cell responses (Geissmann et al. 2010). If scavenging activity is necessary in the male excurrent duct, it should occur all along the epididymal duct and particularly in the distal region, which is the site where sperm are stored for a long period of time (several days to several weeks). Thus, we believe that intraepithelial dendrites are present in the initial segments because it is the region where they are the most likely to interact with sperm and/or luminal components released by spermatozoa very early in the post-testicular maturation process. In doing so, eDCs could be involved in the establishment and maintenance of immune tolerance to maturating spermatozoa that express new autoantigens, which is a critical step in the establishment of male fertility. In contrast, the exclusively peritubular DCs observed in the steady-state cauda epididymidis might be “sentinels” that regulate, when necessary, inflammation and immune responses against ascending pathogens. eDCs could complement the action of testicular DCs, which have been detected in the normal and inflamed testis but are, by definition, never in contact with fully mature spermatozoa (Fijak & Meinhardt 2006, Rival et al. 2006, Rival et al. 2007, Guazzone et al. 2010).
We characterized distinct populations of CD11c+ CD103+ and CD11c+ CD103− DCs in the epididymis. In this respect, eDCs resemble resident DCs described in other non-lymphoid tissues such as the skin, liver, kidney and intestine (Helft et al. 2010). CD103+ DCs exhibit tolerogenic properties in the gut (Coombes et al. 2007, Coombes & Powrie 2008, Matteoli et al. 2010) and they are also functionally specialized in the skin and in the lung (Ginhoux et al. 2009). Although the epididymis and the gut are functionally unrelated, the DCs that populate their mucosae may have to face similar challenges. Epididymal and intestinal mucosa survey a luminal environment in which they have to make the distinction between pathogens and hundred of millions of spermatozoa, or pathogens and the very abundant and heterogeneous commensal flora, respectively (Niess & Reinecker 2005, Niess & Reinecker 2006). In both organs, the “sentinels” of the immune system must sample the luminal environment without disrupting the barrier function of the epithelium. Any alteration of the fragile balance between tolerance and immunogenicity has the potential to trigger autoimmune or inflammatory disorders such as autoimmune infertility in the testis and the epididymis, and inflammatory bowel disease in the gastrointestinal tract (Niess & Reinecker 2005, Niess & Reinecker 2006). Peripheral tolerance involves complex mechanisms aiming at selecting negatively autoreactive T cells, controlling locally the T cells that escape thymic selection, and separating these cells from the autoantigens (Mueller 2010). The density of the eDC network described here is such that low-avidity T cells that express self-peptide MHC are likely to react, causing a failure of peripheral tolerance and, ultimately, autoimmune infertility. In the gut, a population of CD11c+ CD103+ DCs exhibit tolerogenic (Steinman et al. 2003) properties via indoleamine2,3-dioxygenase (IDO) –dependent mechanisms and play, therefore, a critical role in the establishment of oral tolerance to food antigens (Iliev et al. 2009, Matteoli et al. 2010). Interestingly, IDO is abundantly expressed in the epididymis (Britan et al. 2006, Drevet 2006, Jrad-Lamine et al. 2010), but its potential roles in adaptive immunity in this organ remain to be elucidated.
The microscopic analysis of three markers (CD11c, F4/80 and CD206 / mannose receptor) revealed the presence of at least four distinguishable cell types in the epididymis. CD206- positive cells do not express CD11c, they are exclusively interstitial and do not exhibit the stellate morphology of CD11c+ cells. F4/80 is expressed by a subset of CD11c+ cells as well as some CD11c− cells. In fact, flow cytometry and microscopic analyses are snapshots that are not sufficient to reveal the dynamics and phenotypical modulation of DCs and macrophages. In the absence of inflammation, the epididymis is heavily populated by the “infamously heterogeneous” (Geissmann et al. 2010) mononuclear phagocyte system and this heterogeneity might reflect, at least in part, the dual function of this organ. The maturation, storage and perhaps selection (Sutovsky et al. 2001, Cooper et al. 2002) processes that occur in the epididymis are likely to involve phenotypically and functionally distinct subsets of cells with antigen-presenting capabilities, including “immunogenic” and “tolerogenic” DCs. A region-specific characterization of eDCs will help to better understand the heterogeneity observed in the whole organ. Interestingly, the CD103+ eDCs expressed relatively high levels of DC-SIGN (CD209) and langerin (CD207). These markers, which are C-type lectins that bind mannose-containing glycoproteins, are involved in infection by viruses such as human immunodeficiency virus (HIV) (de Witte et al. 2007, de Witte et al. 2008). The role of DC-SIGN- and langerin-positive eDCs during HIV infection should be further investigated, as the epididymis is a major target and reservoir of HIV (Mullen et al. 2003, Shehu-Xhilaga et al. 2007).
In accordance with their high level of expression of MHC and co-stimulatory molecules, we show that isolated CD11c+ eDCs have strong antigen-presenting and cross-presenting capabilities in vitro. The antigen-presenting capabilities of eDCs, as well as their migratory properties, should be established in vivo in future studies. However the results described here leave little doubt that the abundant eDCs play a critical immunological role in the male excurrent duct, in close relationship with epithelial cells, which may regulate the delivery of antigens to peritubular DCs as well as the dynamics of DC processes as they extend towards the lumen (possibly via a CX3CR1-dependent mechanism). In addition, we cannot exclude complementary direct antigen-presenting capabilities of epithelial cells during inflammation, as was described in the gut (Shale & Ghosh 2009). The influence of sex hormones on eDC distribution and function should also be investigated. Indeed, female sex steroids directly regulate the function of DCs (Hughes & Clark 2007) and, surprisingly, estrogens are abundant in the epididymis (Hess et al. 2002). Finally, the abundance of DCs in the epididymis in the absence of infection / inflammation also raises the possibility of additional and non-immune roles for these cells. In the steady-state brain, CD11c+ DCs are particularly abundant in the regions where the blood-brain barrier is weak or absent, and a possible role of DCs in neurogenesis and regulation of central nervous system plasticity was suggested (Bulloch et al. 2008). Similarly, eDCs could be actively involved in the maintenance of the complex epididymal epithelium. In contrast with immunologically privileged sites such as the anterior chamber of the eye (Streilein 1993, Stein-Streilein 2008) and the brain, which are partially isolated from the immune system by a deficient lymphatic drainage, the epididymis contains abundant lymphatic channels (Kazeem 1983, Kazeem 1988). Therefore, immunological information gathered by eDCs could be processed in local lymph nodes to generate regulatory T cells and T effector cells. The functions of DCs and other antigen-presenting cells in reproductive biology have been studied mostly in the female genital tract and in the testis (Bizargity & Bonney 2009, Guazzone et al. 2010, Ivanisevic et al. 2010). Their role in the post-testicular environment must be unraveled, and studying the cellular mechanisms of mucosal immunity in the epididymis will require massive efforts aiming at adapting intravital imaging and in vivo antigen stimulation protocols to this small but relatively accessible organ.
Materials and methods
Mice
CD11c-EYFP mice (Lindquist et al. 2004) are a gift from the laboratory of M.C. Nussenzweig (The Rockefeller University, New York, NY). CX3CR1-GFP mice (Jung et al. 2000) are a gift from D.R. Littman (Skirball Institute, New York, NY). The mice referred as “CX3CR1-GFP” in this manuscript are exclusively Cx3cr1gfp/+ mice, obtained by breeding Cx3cr1gfp/gfp males with wild type females (C57BL/6, Jackson Laboratories). Transgenic and wild type mice were maintained free of common rodent pathogens and on a standard diet. Mouse protocols were approved by the Massachusetts General Hospital Institutional Animal Care and Use Committee.
eDC isolation
For eDC isolation, we modified a protocol used previously to prepare epididymal single cell suspensions (Da Silva et al. 2010). Briefly, epididymides were dissected and cut into small pieces with scissors in dissociation medium (RPMI 1640 with 0.5 mg/ml collagenase type I and 0.5 mg/ml collagenase type II, 1 ml per epididymis pair). Tissues were incubated for 30 min at 37°C with gentle shaking. After enzymatic digestion, cells were passed through a 70-µm nylon mesh strainer, washed in PBS with 1% bovine serum albumin, and stored on ice until processing.
Antibodies, negative selection of eDCs and flow cytometry
For negative selection of eDCs, cell suspensions were incubated with a cocktail of mAbs against T cells (CD90-PE, 53-2.1), B cells (B220-PE, RA3-6B2), NK cells (CD49b-PE, DX5 and NK1.1-PE, PK136), and granulocytes (Ly- 6G-PE, 1A8). After washing, the cells were incubated with anti-PE microbeads as indicated by the manufacturer’s protocol (Miltenyi Biotec, Auburn, CA) and pass thereafter through a MACS LD column. eDCs were then labeled with CD11c-FITC (HL3), CD11c-Alexa 700 (HL3), CD11b- APC-Cy7 (M1/70), Ly-6C-biotin (AL-21), MHC class II-APC (M5/114.15.2), CD86-PE (GL1), CD1d-biotin (CD1.1, Ly-38), CD40-APC (3/23), DC-SIGN-biotin (5H10), CD80-APC (16-10A1), langerin-biotin (eBioL31), Sirp alpha-FITC (P84), CD206-biotin. Antibodies were purchased from BD Biosciences (San Jose, CA) or eBioscience (San Diego, CA). Data were acquired on an LSRII flow cytometer (BD Biosciences) and analyzed with FlowJo 8 or 9 (Tree Star, Ashland, OR). For in vitro proliferation assays, DCs and T cells were sorted on a BD FACSAria (BD Biosciences) based on CD11b and CD11c expression.
Immunofluorescence and microscopy analyses
Mice were anesthetized with nembutal (50 mg/kg, intraperitoneal). Epididymides were fixed by perfusion through the left ventricle with PLP fixative (periodate-lysine-paraformaldehyde), as we have described previously (Da Silva et al. 2006), or PBS with 4% paraformaldehyde. Cryoprotected tissues were sectioned (10 to 50 µm) in a cryostat. Immunolabeling was performed as described previously (Da Silva et al. 2006) with the following antibodies: ZO-1 (R40.76, kindly provided by Dr. Eveline Schneeberger), CD206 (MR5D3, AbD Serotec, Raleigh, NC), Cy3 goat anti-rat IgG (Invitrogen, Eugene, OR,), DyLight 649 goat anti-rat IgG (Jackson ImmunoResearch, West Grove, PA). F4/80 labeling was performed using the tyramide signal amplification system (Perkin Elmer, Waltham, MA), anti- F4/80 IgG (BM8, eBioscience) and a horseradish peroxidase-coupled donkey anti-rat IgG (Jackson ImmunoResearch). Microscopic images were acquired using Eclipse 80i and 90i epifluorescence microscopes (Nikon Instruments, Melville, NY), a Radiance 2000 confocal microscope (Zeiss and Bio-Rad), and an Olympus FV1000 multiphoton microscope. Digital images were processed with IPLab (Scanalytics), NIS Elements (Nikon Instruments), Volocity 5 (Perkin Elmer), ImageJ or Matlab (MathWorks).
In vitro OVA presentation
Single-cell suspensions pooled from mesenteric lymph nodes and spleen of OT-I and OT-II C57BL/6 mice were flow sorted for the isolation of CD4+ and CD8+ T cells obtaining a purity >98% for each T cell population. Purified T cells were labeled with carboxyfluorescein succinimidyl ester (CFSE, 5 µM) and then stimulated in vitro in complete medium (RPMI medium 1640 with sodium 1 mM pyruvate, 10 mM Hepes, 2 mM glutamin, 1% penicillin-streptomycin, 50 µM mercaptoethanol and 10% heat-inactivated FCS) for 5 days in the presence or absence of eDCs (4-5:1 ratio respectively) and/or 200 µg/ml ovalbumin (OVA, Sigma Aldrich), and maintained at 37°C. Cells were harvested and proliferation was measured based on CFSE dilution by flow cytometry.
Supplementary Material
Acknowledgments
Acknowledgements and Funding
We thank Michael Waring (Ragon Institute Flow Cytometry Facility) for FACS sorting, Claudio Vinegoni for some image acquisition and processing, and Dr Siamon Gordon for his kind advice. This study was supported by National Institutes of Health grants DK085715 and DK38452 (SB), MGH Center for the Study of Inflammatory Bowel Disease (CSIBD) pilot feasibility grant (DK43351, NDS), CA086355 and AI084880 (MJP), R01HL095612 (FKS). The Microscopy Core facility of the MGH Program in Membrane Biology receives support from the Boston Area Diabetes and Endocrinology Research Center (DK57521) and the CSIBD (DK43351).
Footnotes
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
References
- Abe K, Takano H, Ito T. Microvasculature of the mouse epididymis, with special reference to fenestrated capillaries localized in the initial segment. Anat Rec. 1984;209:209–218. doi: 10.1002/ar.1092090208. [DOI] [PubMed] [Google Scholar]
- Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature. 1998;392:245–252. doi: 10.1038/32588. [DOI] [PubMed] [Google Scholar]
- Barclay AN. Signal regulatory protein alpha (SIRPalpha)/CD47 interaction and function. Curr Opin Immunol. 2009;21:47–52. doi: 10.1016/j.coi.2009.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barratt CL, Bolton AE, Cooke ID. Functional significance of white blood cells in the male and female reproductive tract. Hum Reprod. 1990;5:639–648. doi: 10.1093/oxfordjournals.humrep.a137162. [DOI] [PubMed] [Google Scholar]
- Bizargity P, Bonney EA. Dendritic cells: a family portrait at mid-gestation. Immunology. 2009;126:565–578. doi: 10.1111/j.1365-2567.2008.02918.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britan A, Maffre V, Tone S, Drevet JR. Quantitative and spatial differences in the expression of tryptophan-metabolizing enzymes in mouse epididymis. Cell Tissue Res. 2006;324:301–310. doi: 10.1007/s00441-005-0151-7. [DOI] [PubMed] [Google Scholar]
- Bulloch K, Miller MM, Gal-Toth J, Milner TA, Gottfried-Blackmore A, Waters EM, Kaunzner UW, Liu K, Lindquist R, Nussenzweig MC, Steinman RM, McEwen BS. CD11c/EYFP transgene illuminates a discrete network of dendritic cells within the embryonic, neonatal, adult, and injured mouse brain. J Comp Neurol. 2008;508:687–710. doi: 10.1002/cne.21668. [DOI] [PubMed] [Google Scholar]
- Chan PTK, Schlegel PN. The epididymis: from molecules to clinical practice: a comprehensive survey of efferent ducts, the epididymis and the vas deferens. 2002. Epididymitis and other conditions of the male excurrent ductal system; pp. 533–553. [Google Scholar]
- Choi JH, Do Y, Cheong C, Koh H, Boscardin SB, Oh YS, Bozzacco L, Trumpfheller C, Park CG, Steinman RM. Identification of antigen-presenting dendritic cells in mouse aorta and cardiac valves. J Exp Med. 2009;206:497–505. doi: 10.1084/jem.20082129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coombes JL, Powrie F. Dendritic cells in intestinal immune regulation. Nat Rev Immunol. 2008;8:435–446. doi: 10.1038/nri2335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coombes JL, Siddiqui KR, Arancibia-Carcamo CV, Hall J, Sun CM, Belkaid Y, Powrie F. A functionally specialized population of mucosal CD103+ DCs induces Foxp3+ regulatory T cells via a TGF-beta and retinoic acid-dependent mechanism. J Exp Med. 2007;204:1757–1764. doi: 10.1084/jem.20070590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper TG, Yeung CH, Jones R, Orgebin-Crist MC, Robaire B. Rebuttal of a role for the epididymis in sperm quality control by phagocytosis of defective sperm. J Cell Sci. 2002;115:5–7. doi: 10.1242/jcs.115.1.5. [DOI] [PubMed] [Google Scholar]
- Cornwall GA. New insights into epididymal biology and function. Hum Reprod Update. 2009;15:213–227. doi: 10.1093/humupd/dmn055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham KA, Beagley KW. Male genital tract chlamydial infection: implications for pathology and infertility. Biol Reprod. 2008;79:180–189. doi: 10.1095/biolreprod.108.067835. [DOI] [PubMed] [Google Scholar]
- Da Silva N, Pisitkun T, Belleannee C, Miller LR, Nelson RD, Knepper MA, Brown D, Breton S. Proteomic analysis of V-ATPase-rich cells harvested from the kidney and epididymis by fluorescence activated cell sorting. Am J Physiol Cell Physiol. 2010 doi: 10.1152/ajpcell.00552.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da Silva N, Shum WW, Breton S. Regulation of vacuolar proton pumping ATPasedependent luminal acidification in the epididymis. Asian J Androl. 2007;9:476–482. doi: 10.1111/j.1745-7262.2007.00299.x. [DOI] [PubMed] [Google Scholar]
- Da Silva N, Silberstein C, Beaulieu V, Pietrement C, Van Hoek AN, Brown D, Breton S. Postnatal expression of aquaporins in epithelial cells of the rat epididymis. Biol Reprod. 2006;74:427–438. doi: 10.1095/biolreprod.105.044735. [DOI] [PubMed] [Google Scholar]
- de Witte L, Nabatov A, Geijtenbeek TB. Distinct roles for DC-SIGN+-dendritic cells and Langerhans cells in HIV-1 transmission. Trends Mol Med. 2008;14:12–19. doi: 10.1016/j.molmed.2007.11.001. [DOI] [PubMed] [Google Scholar]
- de Witte L, Nabatov A, Pion M, Fluitsma D, de Jong MA, de Gruijl T, Piguet V, van Kooyk Y, Geijtenbeek TB. Langerin is a natural barrier to HIV-1 transmission by Langerhans cells. Nat Med. 2007;13:367–371. doi: 10.1038/nm1541. [DOI] [PubMed] [Google Scholar]
- Drevet JR. The antioxidant glutathione peroxidase family and spermatozoa: a complex story. Mol Cell Endocrinol. 2006;250:70–79. doi: 10.1016/j.mce.2005.12.027. [DOI] [PubMed] [Google Scholar]
- Ezer N, Robaire B. The epididymis: from molecules to clinical practice: a comprehensive survey of efferent ducts, the epididymis and the vas deferens. 2002. Androgenic regulation of the structure and function of the epididymis; pp. 297–316. [Google Scholar]
- Fijak M, Meinhardt A. The testis in immune privilege. Immunol Rev. 2006;213:66–81. doi: 10.1111/j.1600-065X.2006.00438.x. [DOI] [PubMed] [Google Scholar]
- Flickinger CJ, Bush LA, Howards SS, Herr JC. Distribution of leukocytes in the epithelium and interstitium of four regions of the Lewis rat epididymis. Anat Rec. 1997;248:380–390. doi: 10.1002/(SICI)1097-0185(199707)248:3<380::AID-AR11>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Geissmann F, Gordon S, Hume DA, Mowat AM, Randolph GJ. Unravelling mononuclear phagocyte heterogeneity. Nat Rev Immunol. 2010 doi: 10.1038/nri2784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginhoux F, Liu K, Helft J, Bogunovic M, Greter M, Hashimoto D, Price J, Yin N, Bromberg J, Lira SA, Stanley ER, Nussenzweig M, Merad M. The origin and development of nonlymphoid tissue CD103+ DCs. J Exp Med. 2009;206:3115–3130. doi: 10.1084/jem.20091756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guazzone VA, Hollwegs S, Mardirosian M, Jacobo P, Hackstein H, Wygrecka M, Schneider E, Meinhardt A, Lustig L, Fijak M. Characterization of dendritic cells in testicular draining lymph nodes in a rat model of experimental autoimmune orchitis. Int J Androl. 2010 doi: 10.1111/j.1365-2605.2010.01082.x. [DOI] [PubMed] [Google Scholar]
- Hedger MP, Hales DB. Immunophysiology of the male reproductive tract. Knobil and Neill's physiology of reproduction. 2006:1195–1286. [Google Scholar]
- Helft J, Ginhoux F, Bogunovic M, Merad M. Origin and functional heterogeneity of nonlymphoid tissue dendritic cells in mice. Immunol Rev. 2010;234:55–75. doi: 10.1111/j.0105-2896.2009.00885.x. [DOI] [PubMed] [Google Scholar]
- Hess RA, Zhou Q, Nie R. The epididymis: from molecules to clinical practice: a comprehensive survey of efferent ducts, the epididymis and the vas deferens. 2002. The role of estrogens in the endocrine ad paracrine regulation of the efferent ductules, epididymis and vas deferens. In; pp. 317–337. [Google Scholar]
- Hooper P, Smythe E, Richards RC, Howard CV, Lynch RV, Lewis-Jones DI. Total number of immunocompetent cells in the normal rat epididymis and after vasectomy. J Reprod Fertil. 1995;104:193–198. doi: 10.1530/jrf.0.1040193. [DOI] [PubMed] [Google Scholar]
- Hughes GC, Clark EA. Regulation of dendritic cells by female sex steroids: relevance to immunity and autoimmunity. Autoimmunity. 2007;40:470–481. doi: 10.1080/08916930701464764. [DOI] [PubMed] [Google Scholar]
- Iliev ID, Spadoni I, Mileti E, Matteoli G, Sonzogni A, Sampietro GM, Foschi D, Caprioli F, Viale G, Rescigno M. Human intestinal epithelial cells promote the differentiation of tolerogenic dendritic cells. Gut. 2009;58:1481–1489. doi: 10.1136/gut.2008.175166. [DOI] [PubMed] [Google Scholar]
- Ivanisevic M, Segerer S, Rieger L, Kapp M, Dietl J, Kammerer U, Frambach T. Antigen-presenting Cells in Pregnant and Non-pregnant Human Myometrium. Am J Reprod Immunol. 2010 doi: 10.1111/j.1600-0897.2010.00858.x. [DOI] [PubMed] [Google Scholar]
- Jrad-Lamine A, Henry-Berger J, Gourbeyre P, Damon-Soubeyrand C, Lenoir A, Combaret L, Saez F, Kocer A, Tone S, Fuchs D, Zhu W, Oefner PJ, Munn DH, Mellor AL, Gharbi N, Cadet R, Aitken RJ, Drevet JR. Deficient-tryptophan catabolism along the kynurenine pathway reveals that the epididymis is in a unique tolerogenic state. J Biol Chem. 2010 doi: 10.1074/jbc.M110.172114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung S, Aliberti J, Graemmel P, Sunshine MJ, Kreutzberg GW, Sher A, Littman DR. Analysis of fractalkine receptor CX(3)CR1 function by targeted deletion and green fluorescent protein reporter gene insertion. Mol Cell Biol. 2000;20:4106–4114. doi: 10.1128/mcb.20.11.4106-4114.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazeem AA. The assessment of epididymal lymphatics within the concept of immunologically privileged sites. Lymphology. 1983;16:168–171. [PubMed] [Google Scholar]
- Kazeem AA. A critical consideration of the rat epididymis as an immunologically privileged site. Scand J Immunol. 1988;27:149–156. doi: 10.1111/j.1365-3083.1988.tb02333.x. [DOI] [PubMed] [Google Scholar]
- Levy S, Robaire B. Segment-specific changes with age in the expression of junctional proteins and the permeability of the blood-epididymis barrier in rats. Biol Reprod. 1999;60:1392–1401. doi: 10.1095/biolreprod60.6.1392. [DOI] [PubMed] [Google Scholar]
- Lin HH, Faunce DE, Stacey M, Terajewicz A, Nakamura T, Zhang-Hoover J, Kerley M, Mucenski ML, Gordon S, Stein-Streilein J. The macrophage F4/80 receptor is required for the induction of antigen-specific efferent regulatory T cells in peripheral tolerance. J Exp Med. 2005;201:1615–1625. doi: 10.1084/jem.20042307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindquist RL, Shakhar G, Dudziak D, Wardemann H, Eisenreich T, Dustin ML, Nussenzweig MC. Visualizing dendritic cell networks in vivo. Nat Immunol. 2004;5:1243–1250. doi: 10.1038/ni1139. [DOI] [PubMed] [Google Scholar]
- Matozaki T, Murata Y, Okazawa H, Ohnishi H. Functions and molecular mechanisms of the CD47-SIRPalpha signalling pathway. Trends Cell Biol. 2009;19:72–80. doi: 10.1016/j.tcb.2008.12.001. [DOI] [PubMed] [Google Scholar]
- Matteoli G, Mazzini E, Iliev ID, Mileti E, Fallarino F, Puccetti P, Chieppa M, Rescigno M. Gut CD103+ dendritic cells express indoleamine 2,3-dioxygenase which influences T regulatory/T effector cell balance and oral tolerance induction. Gut. 2010;59:595–604. doi: 10.1136/gut.2009.185108. [DOI] [PubMed] [Google Scholar]
- McLachlan RI. Basis, diagnosis and treatment of immunological infertility in men. J Reprod Immunol. 2002;57:35–45. doi: 10.1016/s0165-0378(02)00014-1. [DOI] [PubMed] [Google Scholar]
- Meinhardt A, Hedger MP. Immunological, paracrine and endocrine aspects of testicular immune privilege. Mol Cell Endocrinol. 2010 doi: 10.1016/j.mce.2010.03.022. [DOI] [PubMed] [Google Scholar]
- Miloud T, Hammerling GJ, Garbi N. Review of murine dendritic cells: types, location, and development. Methods Mol Biol. 2010;595:21–42. doi: 10.1007/978-1-60761-421-0_2. [DOI] [PubMed] [Google Scholar]
- Mueller DL. Mechanisms maintaining peripheral tolerance. Nat Immunol. 2010;11:21–27. doi: 10.1038/ni.1817. [DOI] [PubMed] [Google Scholar]
- Mullen TE, Jr, Kiessling RL, Kiessling AA. Tissue-specific populations of leukocytes in semen-producing organs of the normal, hemicastrated, and vasectomized mouse. AIDS Res Hum Retroviruses. 2003;19:235–243. doi: 10.1089/088922203763315740. [DOI] [PubMed] [Google Scholar]
- Nashan D, Cooper TG, Knuth UA, Schubeus P, Sorg C, Nieschlag E. Presence and distribution of leucocyte subsets in the murine epididymis after vasectomy. Int J Androl. 1990;13:39–49. doi: 10.1111/j.1365-2605.1990.tb00958.x. [DOI] [PubMed] [Google Scholar]
- Nashan D, Jantos C, Ahlers D, Bergmann M, Schiefer HG, Sorg C, Nieschlag E. Immuno-competent cells in the murine epididymis following infection with Escherichia coli. Int J Androl. 1993;16:47–52. doi: 10.1111/j.1365-2605.1993.tb01152.x. [DOI] [PubMed] [Google Scholar]
- Nashan D, Malorny U, Sorg C, Cooper T, Nieschlag E. Immuno-competent cells in the murine epididymis. Int J Androl. 1989;12:85–94. doi: 10.1111/j.1365-2605.1989.tb01289.x. [DOI] [PubMed] [Google Scholar]
- Niess JH, Brand S, Gu X, Landsman L, Jung S, McCormick BA, Vyas JM, Boes M, Ploegh HL, Fox JG, Littman DR, Reinecker HC. CX3CR1-mediated dendritic cell access to the intestinal lumen and bacterial clearance. Science. 2005;307:254–258. doi: 10.1126/science.1102901. [DOI] [PubMed] [Google Scholar]
- Niess JH, Reinecker HC. Lamina propria dendritic cells in the physiology and pathology of the gastrointestinal tract. Curr Opin Gastroenterol. 2005;21:687–691. doi: 10.1097/01.mog.0000181710.96904.58. [DOI] [PubMed] [Google Scholar]
- Niess JH, Reinecker HC. Dendritic cells: the commanders-in-chief of mucosal immune defenses. Curr Opin Gastroenterol. 2006;22:354–360. doi: 10.1097/01.mog.0000231807.03149.54. [DOI] [PubMed] [Google Scholar]
- Pattinson HA, Mortimer D. Prevalence of sperm surface antibodies in the male partners of infertile couples as determined by immunobead screening. Fertil Steril. 1987;48:466–469. doi: 10.1016/s0015-0282(16)59420-5. [DOI] [PubMed] [Google Scholar]
- Pelletier RM. Blood barriers of the epididymis and vas deferens act asynchronously with the blood barrier of the testis in the mink (Mustela vison) Microsc Res Tech. 1994;27:333–349. doi: 10.1002/jemt.1070270408. [DOI] [PubMed] [Google Scholar]
- Pollanen P, Cooper TG. Immunology of the testicular excurrent ducts. J Reprod Immunol. 1994;26:167–216. doi: 10.1016/0165-0378(94)90019-1. [DOI] [PubMed] [Google Scholar]
- Ritchie AW, Hargreave TB, James K, Chisholm GD. Intra-epithelial lymphocytes in the normal epididymis. A mechanism for tolerance to sperm auto-antigens? Br J Urol. 1984;56:79–83. doi: 10.1111/j.1464-410x.1984.tb07169.x. [DOI] [PubMed] [Google Scholar]
- Rival C, Guazzone VA, von Wulffen W, Hackstein H, Schneider E, Lustig L, Meinhardt A, Fijak M. Expression of co-stimulatory molecules, chemokine receptors and proinflammatory cytokines in dendritic cells from normal and chronically inflamed rat testis. Mol Hum Reprod. 2007;13:853–861. doi: 10.1093/molehr/gam067. [DOI] [PubMed] [Google Scholar]
- Rival C, Lustig L, Iosub R, Guazzone VA, Schneider E, Meinhardt A, Fijak M. Identification of a dendritic cell population in normal testis and in chronically inflamed testis of rats with autoimmune orchitis. Cell Tissue Res. 2006;324:311–318. doi: 10.1007/s00441-005-0129-5. [DOI] [PubMed] [Google Scholar]
- Robaire B, Seenundun S, Hamzeh M, Lamour SA. Androgenic regulation of novel genes in the epididymis. Asian J Androl. 2007;9:545–553. doi: 10.1111/j.1745-7262.2007.00316.x. [DOI] [PubMed] [Google Scholar]
- Rossi AG, Aitken RJ. Interactions between leukocytes and the male reproductive system. The unanswered questions. Adv Exp Med Biol. 1997;424:245–252. doi: 10.1007/978-1-4615-5913-9_46. [DOI] [PubMed] [Google Scholar]
- Seiler P, Cooper TG, Nieschlag E. Sperm number and condition affect the number of basal cells and their expression of macrophage antigen in the murine epididymis. Int J Androl. 2000;23:65–76. doi: 10.1046/j.1365-2605.2000.00210.x. [DOI] [PubMed] [Google Scholar]
- Serre V, Robaire B. Distribution of immune cells in the epididymis of the aging Brown Norway rat is segment-specific and related to the luminal content. Biol Reprod. 1999;61:705–714. doi: 10.1095/biolreprod61.3.705. [DOI] [PubMed] [Google Scholar]
- Shale M, Ghosh S. How intestinal epithelial cells tolerise dendritic cells and its relevance to inflammatory bowel disease. Gut. 2009;58:1291–1299. doi: 10.1136/gut.2006.098475. [DOI] [PubMed] [Google Scholar]
- Shehu-Xhilaga M, Kent S, Batten J, Ellis S, Van der Meulen J, O'Bryan M, Cameron PU, Lewin SR, Hedger MP. The testis and epididymis are productively infected by SIV and SHIV in juvenile macaques during the post-acute stage of infection. Retrovirology. 2007;4:7. doi: 10.1186/1742-4690-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shum WW, Da Silva N, Brown D, Breton S. Regulation of luminal acidification in the male reproductive tract via cell-cell crosstalk. J Exp Biol. 2009;212:1753–1761. doi: 10.1242/jeb.027284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shum WW, Da Silva N, McKee M, Smith PJ, Brown D, Breton S. Transepithelial projections from basal cells are luminal sensors in pseudostratified epithelia. Cell. 2008;135:1108–1117. doi: 10.1016/j.cell.2008.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stedronska J, Hendry WF. The value of the mixed antiglobulin reaction (MAR test) as an addition to routine seminal analysis in the evaluation of the subfertile couple. Am J Reprod Immunol. 1983;3:89–91. doi: 10.1111/j.1600-0897.1983.tb00221.x. [DOI] [PubMed] [Google Scholar]
- Stein-Streilein J. Immune regulation and the eye. Trends Immunol. 2008;29:548–554. doi: 10.1016/j.it.2008.08.002. [DOI] [PubMed] [Google Scholar]
- Steinman RM, Banchereau J. Taking dendritic cells into medicine. Nature. 2007;449:419–426. doi: 10.1038/nature06175. [DOI] [PubMed] [Google Scholar]
- Steinman RM, Hawiger D, Nussenzweig MC. Tolerogenic dendritic cells. Annu Rev Immunol. 2003;21:685–711. doi: 10.1146/annurev.immunol.21.120601.141040. [DOI] [PubMed] [Google Scholar]
- Streilein JW. Immune privilege as the result of local tissue barriers and immunosuppressive microenvironments. Curr Opin Immunol. 1993;5:428–432. doi: 10.1016/0952-7915(93)90064-y. [DOI] [PubMed] [Google Scholar]
- Sutovsky P, Moreno R, Ramalho-Santos J, Dominko T, Thompson WE, Schatten G. A putative, ubiquitin-dependent mechanism for the recognition and elimination of defective spermatozoa in the mammalian epididymis. J Cell Sci. 2001;114:1665–1675. doi: 10.1242/jcs.114.9.1665. [DOI] [PubMed] [Google Scholar]
- Suzuki F. Microvasculature of the mouse testis and excurrent duct system. Am J Anat. 1982;163:309–325. doi: 10.1002/aja.1001630404. [DOI] [PubMed] [Google Scholar]
- Tomlinson MJ, White A, Barratt CL, Bolton AE, Cooke ID. The removal of morphologically abnormal sperm forms by phagocytes: a positive role for seminal leukocytes? Hum Reprod. 1992;7:517–522. doi: 10.1093/oxfordjournals.humrep.a137682. [DOI] [PubMed] [Google Scholar]
- Yeung CH, Nashan D, Sorg C, Oberpenning F, Schulze H, Nieschlag E, Cooper TG. Basal cells of the human epididymis--antigenic and ultrastructural similarities to tissuefixed macrophages. Biol Reprod. 1994;50:917–926. doi: 10.1095/biolreprod50.4.917. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.