Abstract
Background & objectives:
Metabolic syndrome (MS) is an important determinant of cardiovascular (CV) risk. Framingham Risk Scores (FRS) often underestimate the CV risk in Asians, younger patients and those with MS. Asians often develop coronary artery disease (CAD) at a younger age and also have a high prevalence of MS. Only limited data are available on the relationship between MS and FRS in such patients and the present study was undertaken to report on this aspect in an Indian patient population with angiographically documented CAD.
Methods:
Two hundred patients undergoing coronary angiography during a three months study period were included. Diagnosis of MS was based on modified south Asian guidelines.
Results:
Of the 200 patients (age 56.5 ± 8.6 yr) undergoing coronary angiography, MS was diagnosed in 77 per cent n=154; abdominal obesity, low HDL and hypertension were the commonest of the diagnostic criteria of MS, being present in >70 per cent cases. Patients with MS had significantly higher mean FRS than those without MS (15.1 vs 8.65, P<0.0001). Most patients with MS (74%, n=148) had an intermediate to high 10-year CV risk (>10%) as estimated by FRS. The proportion of patients with MS progressively increased in those with low, intermediate and high FRS (61, 87 and 92%, respectively). Though the prevalence of MS was uniformly similar (74-84%) in all age groups (<45, 45-55, 55-65 and > 65 yr, respectively), amongst those <45 yr, none of the patients could be categorized as having high CV risk as estimated by FRS despite having angiographic CAD, highlighting the limitation of age dependence of FRS.
Interpretation & conclusions:
MS is common in Indian patients with angiographically documented CAD; most patients with MS have 10-year risk of >10 per cent as estimated by FRS. Though MS is uniformly prevalent across all age groups, using the FRS may underestimate the CV risk in Indian patients despite documented CAD. These findings have significant implications for Asian patients with CAD in whom onset of CAD is often at a younger age than their Western counterparts. There should be continued health care emphasis on detection of MS and intensification of targeted preventive strategies.
Keywords: Coronary angiography, Framingham Risk Score, metabolic syndrome
Metabolic syndrome (MS), which is a clustering of atherogenic metabolic abnormalities, has emerged as an important determinant of cardiovascular risk1,2. Different guidelines issued by WHO, National Cholesterol Education Program-Adult Treatment Panel III (NCEP-ATP-III) and International Diabetes Federation (IDF) have been proposed to identify MS in clinical practice3–6. Irrespective of the criteria used, MS is associated with increased risk of developing type 2 diabetes mellitus (DM) as well as cardiovascular (CV) disease in different ethnic populations.
Framingham risk Score (FRS) has traditionally been used as a predictor of the 10-year risk of coronary heart disease and takes into account age, smoking status, lipid profile, blood pressure and presence or absence of DM. It predicts the 10-year CV risk of having cardiac events and categorizes patients into low (risk <10%), intermediate (risk 10-20%) and high risk groups (>20%)7. The incremental value of MS over the traditionally used FRS as a marker of future CV events is debatable, with studies suggesting that it may be inferior to FRS in predicting this risk6,8,9. However, since FRS is dependent on age and estimates only the 10-year CV risk, it may underestimate the overall risk in young patients (with a longer life expectancy) as well as in those with MS, many of whose individual components are not included in the risk score10–13.
Though the frequency of MS in the Indian patients has been reported in previous population based studies14–16, there are scant data on its prevalence in patients with angiographically proven coronary artery disease (CAD). Moreover, little is known about the relationship of FRS and MS in these patients who are often prone to develop CAD at a younger age as compared to Western counterparts17,18. In this study we sought to estimate the prevalence of MS in Indian patients undergoing coronary angiography and assess the relationship between MS and FRS in such a patient population.
Material & Methods
A total of 200 consecutive patients undergoing coronary angiography at Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, north India, during a period of three months (October-December 2010) were included in the study. All patients gave informed consent for participation in the study and the study protocol was approved by the institutional ethics committee. The diagnosis of MS was based on the modified South Asian guidelines and required the presence of three or more of the following five components: (i) abdominal obesity (waist circumference: men >90 cm, women >80 cm), (ii) elevated triglycerides (>150 mg/dl), (iii) low HDL (<40 mg/dl in men, <50 mg/dl in women), (iv) elevated blood pressure, BP (systolic or diastolic >130/85 mmHg or use of antihypertensive medication), and (v) elevated fasting glucose (>100 mg/dl rather than the NCEP threshold of >110 mg/dl, based on a revision of the blood glucose criterion for the MS)5,19,20. Angiographic CAD was defined as >50 per cent of diameter stenosis in any of the major epicardial coronary arteries21.
Statistical analysis: The sample size of the patient population was calculated based on the overall prevalence of MS in the general population15. Since our patient population was at a slightly higher risk, we assumed at least 1.5 times higher prevalence of MS among them as compared to the general population (approximately 35%). An estimate of that magnitude with 95 per cent confidence limits and 20 per cent relative precision required a sample size of 180. With a 10 per cent allowance for any non or partial response the calculated sample size was 200. All data were analyzed using SPSS 16 statistical software (SPSS Inc., Chicago, Illinois, USA). Data are expressed as mean ± standard deviation; Student t-test was used to compare means between groups, and chi-square test to compare proportions between groups. Univariate and bivariate logistic regression analyses were done and a P<0.05 was considered statistically significant. Post-hoc power analysis of variables which were statistically significant at 5 per cent level indicated that the hypothesis of equality of the two groups (Type II error) can be rejected with over 90 per cent power in all except DM, double and triple vessel disease (DVD/TVD) and fasting blood sugar, in which the power was between 65 to 70 per cent.
Results
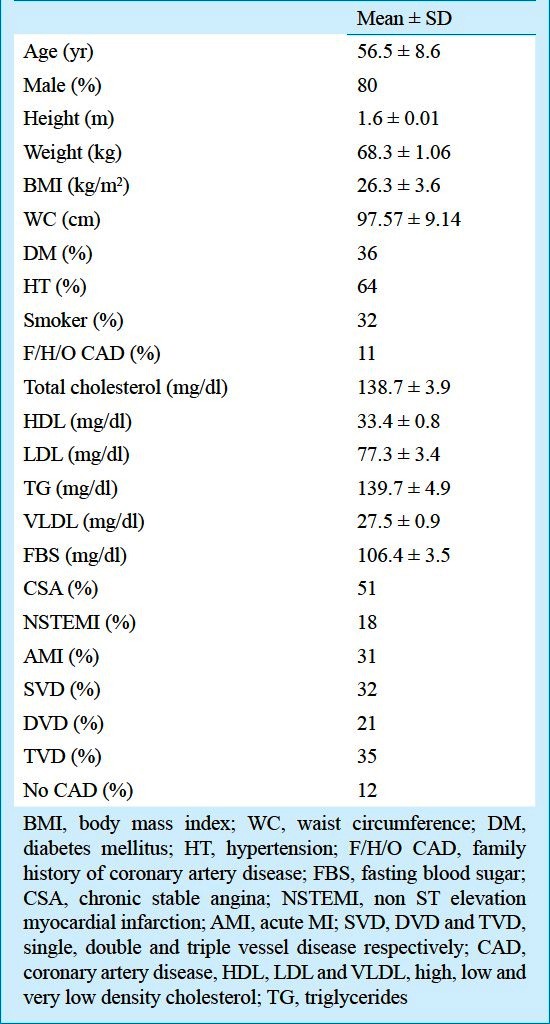
The patients’ characteristics are summarized in Table I; mean age was 56.5 ± 8.6 yr (range 35-79 yr) and 160 (80%) were males. Diabetes was present in 72 (36%), hypertension (HT) in 128 (64%), 64 (32%) were smokers while a family history of CAD was present in 22 (11%). Chronic stable angina was present in 102 (51%) patients, non-ST elevation myocardial infarction (NSTEMI) or unstable angina in 36 (18%), while recent MI (within last 4 wk) was present in 62 (31%). Coronary angiography revealed the presence of single vessel disease in 64 (32%), double vessel disease in 42 (21%) and triple vessel disease in 70 (35%), while 24 (12%) patients had no/insignificant disease. Diffuse CAD was present in 60 (30%), while left ventricular (LV) dysfunction (EF <50%) was present in 84 (42%) patients. Overall, using the FRS, 70 (35%) were categorized as having a low 10-year CV risk, while 82 (41%) had intermediate and 48 (24%) had high 10-year CV risk.
Table I.
Demographic, clinical and coronary angiographic profile of the patient population (n=200)
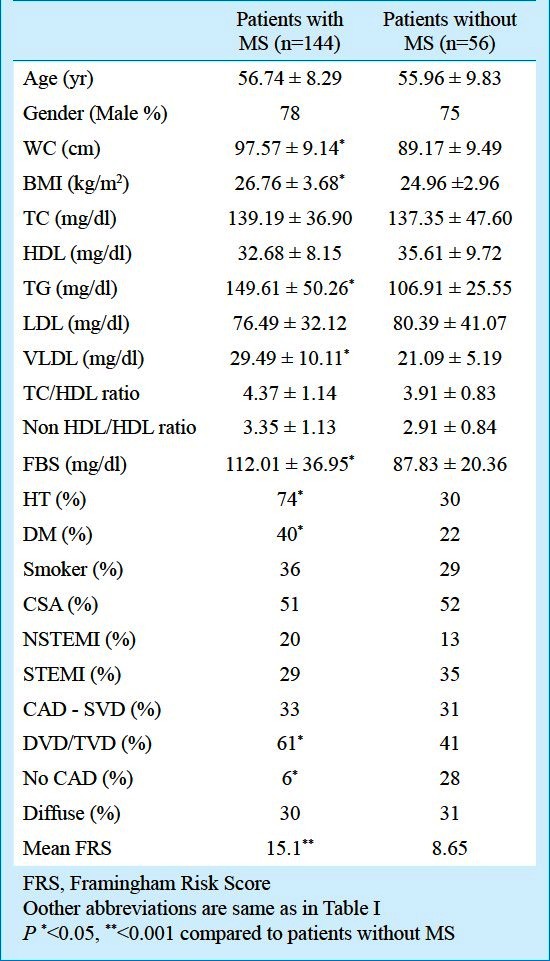
Metabolic syndrome and traditional risk factors: Using the revised South Asian Modified National Cholesterol Education Program criteria, MS was diagnosed in 154 (77%) patients. However, considering abdominal obesity as an essential and not optional criterion, reduced the prevalence of MS from 122(77 to 61%). The clinical characteristics of patients with and without MS are summarized in Table II. There was no significant difference amongst patients with MS and those without, in terms of clinical presentation of chronic stable angina, NSTEMI or STEMI. Significantly fewer patients with MS had normal coronary arteries as compared to those without MS (12(6%) vs 56(28%), P<0.05). The prevalence of double or triple vessel CAD was also significantly more common in patients with MS as compared to those without MS 122 (61%) vs 82 (41%), P<0.05.
Table II.
Clinical characteristics of patients with and without metabolic syndrome
Overall, of the required components for defining MS, three criteria were fulfilled in 106 (53%), four fulfilled in 72 (36%) while all five were fulfilled in 72 (11%). Abdominal obesity was the commonest feature [being present in 189 (94.8%), followed in order of prevalence by low HDL in 162 (81%), HT in 148 (74%), high TG in 82 (41%) and DM in 80 (40%). With progressively increasing BMI, the prevalence of MS also increased 62 (31%) and 94 (47%) in those with BMI 23-24.9 and BMI > 25 kg/m2 respectively; interestingly despite having a normal BMI (< 23 kg/m2, 24 (12%) patients satisfied the diagnostic criteria of MS.
Metabolic syndrome and association with Framingham Risk Scores: Patients with MS had higher mean FRS (15.1 vs 8.65, P<0.001) as compared to those without MS. Majority of the patients with MS 148 (74%) had a 10-year CV risk of >10 per cent as estimated by FRS while a low 10-year CV risk (<10%) was seen in only 52 (26%) patients with MS. Amongst patients with low, intermediate and high FRS the prevalence of MS also increased progressively [122 (61%), 174 (87%) and 184 (92%) respectively, Fig. 1].
Fig. 1.
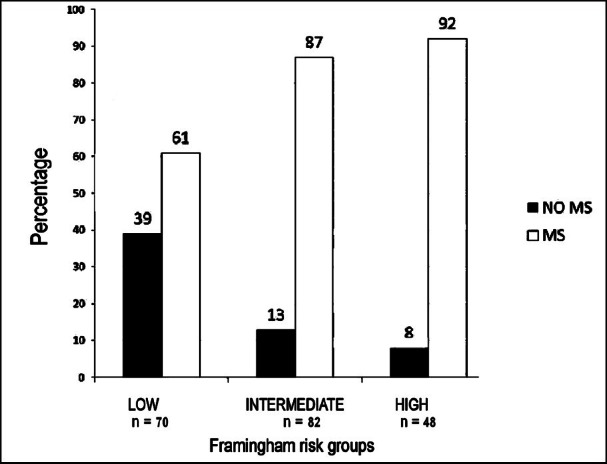
Proportion of patients in the low, intermediate and high FRS groups having MS (P value <0.05 for comparison between low and intermediate as well as low and high FRS groups).
Influence of age on MS and its individual components and FRS: To observer the independent effects of MS and FRS, all patients with angiographically documented CAD (n=176) were categorized into age quartiles (<45, 45-55, 55-65 and >65 yr). We observed a high and fairly constant prevalence of MS across all age quartiles (varying from 74-81%, Fig. 2). However distribution of FRS among different age groups revealed that despite angiographically documented CAD, in patients <45 yr none of the patients were categorized as high FRS. Only 26 (13%) and 30 (15%) patients could be categorized as having high FRS in age groups 45-55 and 55-65 yr, while in patients older than 65 yr, 30 per cent were classified as having high FRS.
Fig. 2.
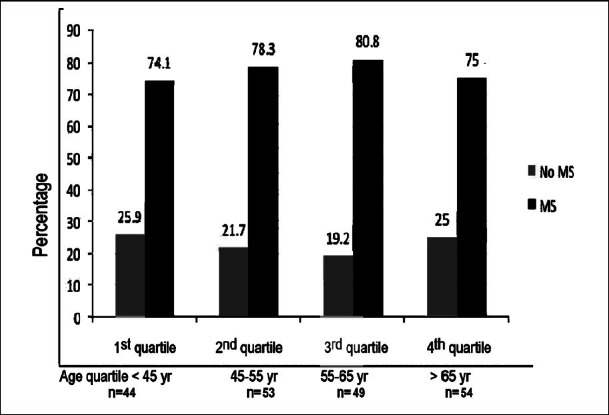
Prevalence of metabolic syndrome in different age quartiles in patients with CAD (P value ns for all distribution of MS across all age groups demonstrating that MS was common across all age quartiles).
Discussion
Metabolic syndrome (MS), major components of which include central obesity, hypertriglyceridaemia, low high-density lipoprotein levels, elevated BP and fasting hyperglycaemia has emerged as an important determinant of CV risk1,2. Using the South Asian Modified National Cholesterol Education Program criteria for diagnosis of MS in our study, 77 per cent patients with angiographically documented CAD were diagnosed to have MS19,20. Expectedly patients with MS more frequently had hypertension and diabetes; they also had a higher prevalence of double/triple vessel CAD and higher mean FRS.
The prevalence of MS in our patient population was higher than the reported prevalence rates of 18-48 per cent in previous studies conducted in the resident Indian population14–16. This may be explained by the fact that majority of our patients (88%) had CAD on coronary angiography, while most other studies were population based studies, in largely asymptomatic individuals. Though various diagnostic criteria for MS have been published, since Asian Indians have a tendency to develop metabolic abnormalities at a lower body mass index and waist circumference than other groups, conventional criteria may underestimate the prevalence of MS. This was also confirmed in our study; if abdominal obesity was considered an essential criterion (as recommended by the IDF guidelines)5 the prevalence of MS was underestimated (came down to 61% from 77%). Such a discrepancy has also been noted in previous studies and underscores the importance of using the modified South Asian guidelines to diagnose MS in the ethnic Indian population, (using obesity as an optional, and not an essential criterion, and the South Asian-specific waist circumference)22,23.
There is evidence to indicate that MS is associated with a 1.5-2-fold increase in cardiovascular risk of CVD, cardiovascular mortality, stroke, as well as all-cause mortality which has led to it being widely used as a tool for identifying patients at risk for CV events24–26. We also observed a high likelihood of angiographically documented CAD in patients with MS in our study; more than 90 per cent patients with MS had CAD on angiography, while the prevalence of double/triple vessel CAD was also higher in those with MS as compared to those without. This association of MS with CAD in the ethnic Indian population has also been reported in previous studies20,27,28.
Framingham Risk Score (FRS) has traditionally been used as a predictor of the 10-year risk of coronary heart disease. Studies in the Western population have indicated that MS may actually be inferior to FRS in predicting CHD risk6–9. However, other studies have also suggested that MS is an independent predictor of angiographic CAD in subjects stratified as low risk by FRS29. The FRS may actually underestimate the overall risk in younger patients, who are likely to have a longer life expectancy as well as in patients with MS10–13. Since CAD often develops at a younger age in the developing world, more data are needed on the relationship between MS and FRS in the resident Indian population.
In our study patients with MS had a higher overall FRS as compared to those without, and majority of patients with MS had a 10-year CV risk of >10 per cent as estimated by FRS. In a previous population based study, Bansal et al30 reported that though prevalence of MS was high in young Indians, only 23.2 per cent had a 10-year CV risk of >10 per cent as estimated by FRS. In young patients (age <45 yr) with acute MI, Zarich et al31 also reported that though the prevalence of MS was high, only 28 per cent patients with MS had high FRS with a 10-years CV risk >20 per cent. Since the mean age of patients in these studies30,31 was much lower than our patients, overall FRS scores may have been lower in their entire patient population, highlighting the heavy dependence of FRS on age. Moreover, most (88%) of our patients had manifest CAD, while the study by Bansal et al30 was a population based study of largely asymptomatic patients, accounting for higher overall FRS in our patients.
Patients of Indian origin often fit into the model of metabolically obese, normal weight individuals and are, therefore, at high risk for development of both MS and subsequent CVD. In our study, despite a mean weight of 68.3 ± 1.06 kg, the mean waist circumference was 97.57 ± 9.14 cm and the mean BMI was 26.8 ± 3.6 kg/m2, demonstrating that such patients would often be categorized as metabolically obese (BMI >25.0 kg/m2). The fact that MS can develop in Indians with “apparently normal” BMI (18.5-22.9 kg/m2), was also confirmed in our study, with MS being present in 12 per cent of patients with BMI <23 kg/m2. Similar trends have been observed in previous studies in Indian patients, confirming that Indians tend to develop MS at BMI levels generally considered normal among the Western population, leading to lower cut-off points for overweight (BMI >23 kg/m2) and obesity (BMI >25 kg/m2) for all Asians by the WHO15,32.
Our study revealed that among patient population with angiographic CAD MS was common across all age quartiles. However, despite angiographically documented CAD, none of the patients were categorized as high FRS in patients <45 yr; this discrepancy was somewhat less marked with increasing age. Hence, using FRS would significantly underestimate the CV risk in younger patients, highlighting the dependence of the traditional FRS scores on age. This issue is especially pertinent for the Asian patient population in whom CV disease is becoming increasingly common at younger age and metabolic syndrome is also on the rise.
Despite being a single point observational study, our findings carry significant implication for Indian patients with CAD. Both FRS and MS obviously do not assess the individual's life long CV risk and, therefore, each patient's risk profile should be frequently reassessed. FRS is primarily a tool used for stratification of largely asymptomatic individuals to predict their future CV risk, however, we have used it in patients with CAD as the purpose of our study was to see the relationship and possible interactions between MS, FRS and angiographic CAD in an Indian patient population.
In conclusion, our findings show that Indian patients with angiographically proven CAD commonly have MS. More than 70 per cent patients with MS had intermediate to high FRS. Prevalence of MS was high across all age groups. In Asian Indians, where patients often develop CAD at a younger age, FRS may underestimate the CV risk. With the rising incidence of CAD in the developing world, there should be continued health care emphasis on detection of MS and intensification of targeted preventive strategies. Prevention, detection and optimal management of metabolic syndrome are likely to reduce cardiovascular risk.
References
- 1.Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–16. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 2.Girman CJ, Rhodes T, Mercuri M, Pyorala K, Kjekshus J, Pedersen TR, et al. The metabolic syndrome and risk of major coronary events in the Scandinavian Simvastatin Survival Study (4S) and the Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS) Am J Cardiol. 2004;93:136–41. doi: 10.1016/j.amjcard.2003.09.028. [DOI] [PubMed] [Google Scholar]
- 3.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 4.Balkau B, Charles MA European Group for the Study of Insulin Resistance (EGIR) Comment on the provisional report from the WHO consultation. Diabet Med. 1999;16:442–3. doi: 10.1046/j.1464-5491.1999.00059.x. [DOI] [PubMed] [Google Scholar]
- 5.The IDF consensus worldwide definition of the metabolic syndrome. Brussels, Belgium: International Diabetes Federation; 2006. International Diabetes Federation. [Google Scholar]
- 6.Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C. Definition of Metabolic Syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association Conference on Scientific Issues Related to Definition. Circulation. 2004;109:433–8. doi: 10.1161/01.CIR.0000111245.75752.C6. for the Conference P. [DOI] [PubMed] [Google Scholar]
- 7.Grundy SM, Bazzarre T, Cleeman J, D’Agostino RB, Sr, Hill M, Houston-Miller N, et al. Prevention Conference V: beyond secondary prevention. Identifying the high-risk patient for primary prevention. Medical office assessment. Writing Group I. Circulation. 2000;101:E3–E11. doi: 10.1161/01.cir.101.1.e3. [DOI] [PubMed] [Google Scholar]
- 8.Wannamethee SG, Shaper AG, Lennon L, Morris RW. Metabolic syndrome vs Framingham Risk Score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Arch Intern Med. 2005;165:2644–50. doi: 10.1001/archinte.165.22.2644. [DOI] [PubMed] [Google Scholar]
- 9.Stern MP, Williams K, Gonzalez-Villalpando C, Hunt KJ, Haffner SM. Does the metabolic syndrome improve identification of individuals at risk of type 2 diabetes and/or cardiovascular disease? Diabetes Care. 2004;27:2676–81. doi: 10.2337/diacare.27.11.2676. [DOI] [PubMed] [Google Scholar]
- 10.Berry JD, Lloyd-Jones DM, Garside DB, Greenland P. Framingham risk score and prediction of coronary heart disease death in young men. Am Heart J. 2007;154:80–6. doi: 10.1016/j.ahj.2007.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hemann BA, Bimson WF, Taylor AJ. The Framingham Risk Score: an appraisal of its benefits and limitations. Am Heart Hosp J. 2007;5:91–6. doi: 10.1111/j.1541-9215.2007.06350.x. [DOI] [PubMed] [Google Scholar]
- 12.Williams R, Bhopal R, Hunt K. Coronary risk in a British Punjabi population: comparative profile of non-biochemical factors. Int J Epidemiol. 1994;23:28–37. doi: 10.1093/ije/23.1.28. [DOI] [PubMed] [Google Scholar]
- 13.Linton MF, Fazio S. A practical approach to risk assessment to prevent coronary artery disease and its complications. Am J Cardiol. 2003;92:19i–26i. doi: 10.1016/s0002-9149(03)00505-8. [DOI] [PubMed] [Google Scholar]
- 14.Ramachandran A, Snehalatha C, Satyavani K, Sivasankari S, Vijay V. Metabolic syndrome in urban Asian Indian adults - a population study using modified ATP III criteria. Diabetes Res Clin Pract. 2003;60:199–204. doi: 10.1016/s0168-8227(03)00060-3. [DOI] [PubMed] [Google Scholar]
- 15.Deepa M, Farooq S, Datta M, Deepa R, Mohan V. Prevalence of metabolic syndrome using WHO, ATPIII and IDF defnitions in Asian Indians: the Chennai Urban Rural Epidemiology Study (CURES-34) Diabetes Metab Res Rev. 2007;23:127–34. doi: 10.1002/dmrr.658. [DOI] [PubMed] [Google Scholar]
- 16.Gupta R, Sarna M, Thanvi J, Rastogi P, Kaul V, Gupta VP. High prevalence of multiple coronary risk factors in Punjabi Bhatia community: Jaipur Heart Watch-3. Indian Heart J. 2004;56:646–52. [PubMed] [Google Scholar]
- 17.Misra A, Pandey RM, Devi JR, Sharma R, Vikram NK, Khanna N. High prevalence of diabetes, obesity, and dyslipidaemia in urban slum population in northern India. Int J Obes Relat Metab Disord. 2001;25:1722–9. doi: 10.1038/sj.ijo.0801748. [DOI] [PubMed] [Google Scholar]
- 18.Enas EA. Coronary artery disease epidemic in Indians: a cause for alarm and a call for action. J Indian Med Assoc. 2000;98:697–702. [PubMed] [Google Scholar]
- 19.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. American Heart Association; National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–52. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 20.Enas EA, Mohan V, Deepa M, Farooq S, Pazhoor S, Chennikkara H. The metabolic syndrome and dyslipidemia among Asian Indians: A population with high rates of diabetes and premature coronary artery disease. J Cardiometab Syndr. 2007;2:267–75. doi: 10.1111/j.1559-4564.2007.07392.x. [DOI] [PubMed] [Google Scholar]
- 21.Meijboom WB, Van Mieghem CA, van Pelt N, Weustink A, Pugliese F, Mollet NR, et al. Comprehensive assessment of coronary artery stenoses computed tomography coronary angiography versus conventional coronary angiography and correlation with fractional flow reserve in patients with stable angina. J Am Coll Cardiol. 2008;52:636–43. doi: 10.1016/j.jacc.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 22.Chow CK, Naidu S, Raju K, Raju R, Joshi R, Sullivan D, et al. Significant lipid, adiposity and metabolic abnormalities amongst 4535 Indians from a developing region of rural Andhra Pradesh. Atherosclerosis. 2008;196:943–52. doi: 10.1016/j.atherosclerosis.2007.02.027. [DOI] [PubMed] [Google Scholar]
- 23.Reddy KS, Prabhakaran D, Chaturvedi V, Jeemon P, Thankappan KR, Ramakrishnan L, et al. Methods for establishing a surveillance system for cardiovascular diseases in Indian industrial populations. Bull World Health Organ. 2006;84:461–9. doi: 10.2471/blt.05.027037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, et al. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49:403–14. doi: 10.1016/j.jacc.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 25.Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med. 2006;119:812–9. doi: 10.1016/j.amjmed.2006.02.031. [DOI] [PubMed] [Google Scholar]
- 26.Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk: A systematic review and meta-analysis. J Am Coll Cardiol. 2010;56:1113–32. doi: 10.1016/j.jacc.2010.05.034. [DOI] [PubMed] [Google Scholar]
- 27.Tillin T, Forouhi N, Johnston DG, McKeigue PM, Chaturvedi N, Godsland IF. Metabolic syndrome and coronary heart disease in South Asians, African-Caribbeans and white Europeans: a UK population-based cross-sectional study. Diabetologia. 2005;48:649–56. doi: 10.1007/s00125-005-1689-3. [DOI] [PubMed] [Google Scholar]
- 28.Lee J, Ma S, Heng D, Tan CE, Chew SK, Hughes K, et al. Should central obesity be an optional or essential component of the metabolic syndrome? Ischemic heart disease risk in the Singapore Cardiovascular Cohort Study. Diabetes Care. 2007;30:343–7. doi: 10.2337/dc06-1866. [DOI] [PubMed] [Google Scholar]
- 29.Konstantinou DM, Chatzizisis YS, Louridas GE, Giannoglou GD. Metabolic syndrome and angiographic coronary artery disease prevalence inassociation with the Framingham risk score. Metab Syndr Relat Disord. 2010;8:201–8. doi: 10.1089/met.2009.0059. [DOI] [PubMed] [Google Scholar]
- 30.Bansal M, Shrivastava S, Mehrotra R, Agarwal V, Kasliwal RR. Low Framingham Risk Score despite high prevalence of metabolic syndrome in asymptomatic north-Indian population. JAPI. 2009;57:17–22. [PubMed] [Google Scholar]
- 31.Zarich S, Luciano C, Hulford J, Abdullah A. Prevalence of metabolic syndrome in young patients with acute MI: does the Framingham Risk Score underestimate cardiovascular risk in this population? Diab Vasc Dis Res. 2006;3:103–7. doi: 10.3132/dvdr.2006.012. [DOI] [PubMed] [Google Scholar]
- 32.Alberti KG, Zimmet P, Shaw J. The metabolic syndrome–a new worldwide definition; IDF Epidemiology Task Force Consensus Group. Lancet. 2005;366:1059–62. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]


