Sir,
All countries should immunize their health care workers (HCWs) as a priority to protect the essential health infrastructure. As vaccines available initially will not be sufficient, a step-wise approach to vaccinate particular groups may be considered. Strategic Advisory Group of Experts (SAGE) on immunization suggested the following groups for consideration, noting that countries need to determine their order of priority based on country-specific conditions: pregnant women; those aged above 6 months with one of several chronic medical conditions; healthy young adults of 15 to 49 yr of age; healthy children; healthy adults of 50 to 64 yr of age; and healthy adults of 65 yr of age and above1. The use of influenza vaccine during outbreak of Influenza, whether seasonal or pandemic, is associated with many issues. There are issues of availability, acceptability and adverse reactions. The HCWs belong to high risk category and therefore, should be considered as a priority group for vaccination.
With evidence on the effectiveness of vaccination in the control and prevention of seasonal influenza, vaccination for pandemic influenza is one of the most important primary preventative measures to reduce the disease burden associated with influenza A (H1N1) infection2. Several high risk groups have been identified as “the priority group” to receive the influenza A (H1N1) vaccination and among these, healthcare workers have been identified “as a first priority” to be vaccinated against influenza A (H1N1) by the World Health Organization3. Previous studies that have examined the acceptability of seasonal influenza vaccination among health care workers have generally demonstrated a low acceptance rate of vaccination in this group4.
The present study was a cross-sectional, self administered questionnaire based KAP (knowledge, attitude, practice) study amongst HCWs and medical students in a Armed Forces medical college in Pune. Taking the forecasted prevalence of 50 per cent accepting vaccination and taking the error as 10 per cent, alpha as 0.05 assuming 95 per cent CI, the sample size for health care workers was 96. For a student population of 600, assuming 50 per cent students having been vaccinated, with an error of 10 per cent, alpha as 0.05, applying finite population correction the sample size was calculated to be 90. A list of all the HCWs (Doctors, Nurses and Paramedics) and the medical students was obtained and the desired numbers of subjects were drawn using simple random sampling after getting their consent to be part of the study. The selected subjects were given the questionnaire and were asked to fill it up. Known cases of influenza A H1N1 [A (H1N1) pdm09] either currently or in the recent past and those who did not give consent were excluded. A total of 90 medical students and 100 HCWs were included, of whom 31 were doctors, 40 were nurses, and 29 included paramedics and laboratory staff.
Amongst 190 study participants, 52 (27.4%) reported that they had symptoms suggestive of influenza during the last one year. Regarding exposure to a known case of H1N1 [A (H1N1) pdm09] 40 (21.3%) reported contact with a known case of H1N1 [A (H1N1) pdm09th ] influenza. Of the total 190 participants, 157 (82.6%) were vaccinated with H1N1 influenza vaccine [81 of 90 (90%) medical students and 17 of 31 (54.8%) doctors, 39 of 40 (97.5%) nurses, 20 of 29 (60%) paramedics and laboratory staff]. The difference in the vaccination proportion amongst different categories was statistically significant (Chi square test, P<0.005). When asked “Is the vaccine protective?” 67 (35.3%) strongly agreed, 78 (41.1%) agreed, 42 (22.1%) somewhat agreed, and 3 (1.65) participants disagreed. None of the participants strongly disagreed with the statement. “Is the vaccine safe?” 41 (21.6%) strongly agreed, 88 (46.3%) agreed, 55 (28.9%) somewhat agreed, and 6(3.2%) disagreed. A large percentage of medical students (73.3%) and doctors (71%) believed the vaccine had side effects while only a quarter or more amongst nurses and paramedics believed that vaccine had side effects. This difference in perception was found to be statistically significant (Chi square test, P<0.05).
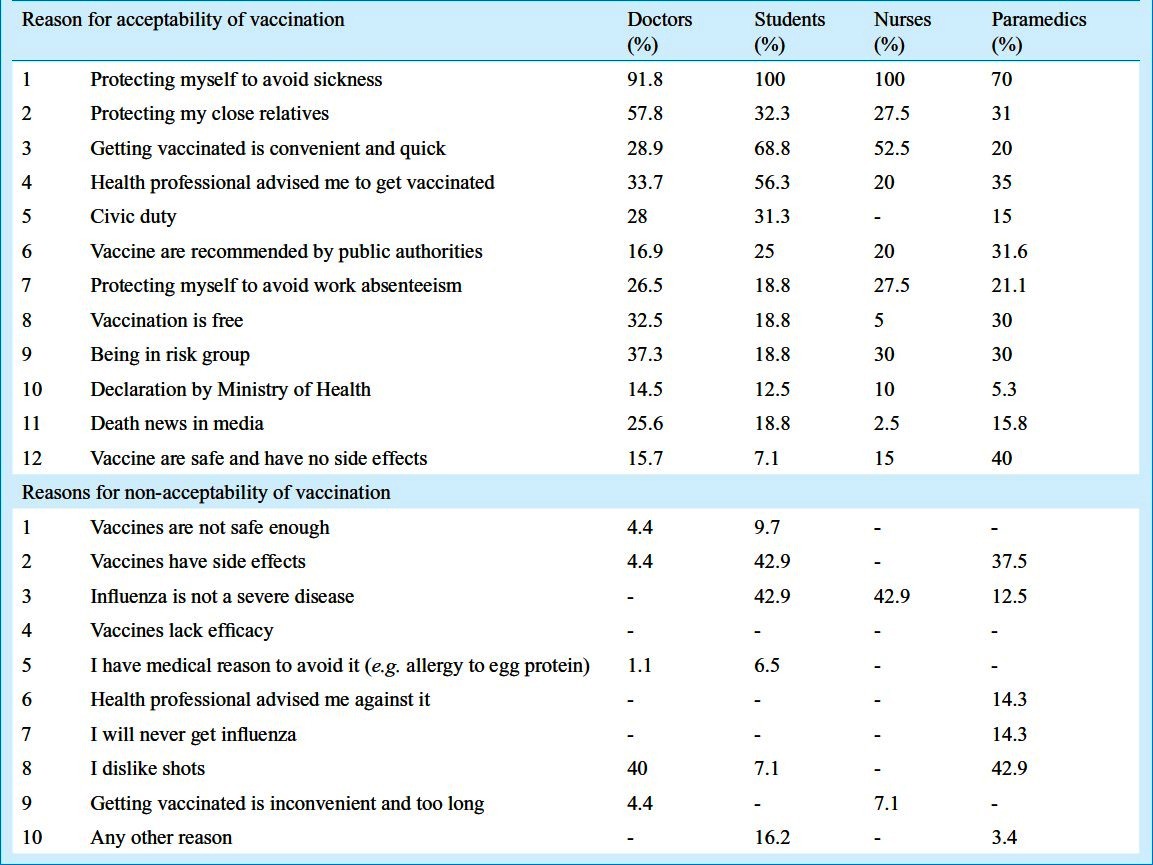
The commonest reason given by all for accepting vaccination (Table) was self protection against illness. Other important reasons given were health advice by health care professionals, protecting relatives, getting vaccinated was easy and quick. Death news in the media and declaration by Ministry of Health were found to be the least cited reasons for getting vaccinated. In the reasons for non-acceptability of vaccination (Table) the commonest reasons were the belief that influenza is not a severe disease and vaccines have side effects besides a dislike for shots. Some people had allergy to egg proteins and thus did not accept vaccination. Under “any other reason” some gave reasons that they were away on leave or stocks were over and thus could not take vaccine. Lack of efficacy of vaccine was not an important factor as no individual chose it as a reason for non-acceptability of vaccination.
Table.
Reasons for acceptability and non-acceptability of vaccination in health care workers & students
Among all healthcare workers, nurses constituted the largest group with the highest frequency of contacts with patients and staff. A previous study on the acceptability of seasonal influenza vaccination in nurses showed that their acceptance of vaccination was lowest among all healthcare workers5. A study of Italian healthcare workers showed 31 per cent of nurses willing to accept vaccination compared to 67 per cent of physicians6. In a study conducted on Hong Kong healthcare workers, it was found that only 25 per cent of nurses were willing to accept influenza A (H1N1) vaccination, compared with 47 per cent of doctors and 29 per cent of allied professionals7. In a cross-sectional survey on experienced nurses in Hong Kong, the vaccination rate for seasonal influenza vaccination was about 50 per cent8. Compared to these studies, our study demonstrated a better acceptance of vaccination amongst nurses with almost all accepting vaccination. The acceptance of vaccination by doctors was similar to other studies.
In conclusion, our findings showed that the vaccine acceptance was good amongst medical students and nurses. The HCWs belonging to category of doctors and paramedics had lower vaccine coverage.
Acknowledgment
The study was conducted under the Short Term Studentship 2011 ID (2011-02500) of Indian Council of Medical Research, New Delhi, India.
References
- 1.Strategic Advisoty Group of Eperts on immunization – report of the extraordinary meeting on the influenza A (H1N1) 2009 pandemic, 7 July 2009. [accessed on February 2, 2012];WHO. Weekly epidemiological record No. 30. 2009 84:301–308. Available from: http://www.who.int/wer . [PubMed] [Google Scholar]
- 2.Jennings LC, Monto AS, Chan PK, Szucs TD, Nicholson KG. Stockpiling prepandemic influenza vaccines: a new cornerstone of pandemic preparedness plans. Lancet Infect Dis. 2008;8:650–8. doi: 10.1016/S1473-3099(08)70232-9. [DOI] [PubMed] [Google Scholar]
- 3.WHO global influenza preparedness plan: Pandemic influenza preparedness and response: a WHO guidance document. Geneva: World Health Organization; 2009. [PubMed] [Google Scholar]
- 4.Martinello RA, Jones L, Topal JE. Correlation between healthcare workers’ knowledge of influenza vaccine and vaccine receipt. Infect Control Hosp Epidemiol. 2003;24:845–7. doi: 10.1086/502147. [DOI] [PubMed] [Google Scholar]
- 5.Qureshi AM, Nughes NJ, Murphy E, Primrose WR. Factors influencing update of influenza vaccination among hospital-based healthcare workers. Occup Med (London) 2004;54:197–201. doi: 10.1093/occmed/kqg087. [DOI] [PubMed] [Google Scholar]
- 6.La Torre G, Di Thiene D, Cadeddu C, Ricciardi W, Boccia A. Behaviours regarding preventive measures against pandemic H1N1 influenza among Italian healthcare workers, October 2009. Euro Surveill. 2009;14(49) pii=19432. [PubMed] [Google Scholar]
- 7.Chor JS, Ngai KL, Goggins WB, Wong MC, Wong SY, Lee N, et al. Willingness of Hong Kong healthcare workers to accept pre-pandemic influenza vaccination at different WHO alert levels: two questionnaire surveys. BMJ. 2009;339:3391. doi: 10.1136/bmj.b3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tam DKP, Lee SS, Lee S. Impact of severe acute respiratory sundrome and the perceived avian influenza epidemic on the increased rate of influenza vaccination among nurses in Hong Kong. Infect Control Hosp Epidemiol. 2008;29:256–61. doi: 10.1086/527507. [DOI] [PubMed] [Google Scholar]


