Abstract
Background & objectives:
Perioperative antimicrobial prophylaxis constitutes the bulk of antimicrobial consumption in any hospital. This study was conducted at a level 1 Trauma Centre of a tertiary care hospital of India to assess the efficacy of a short (24 h) course of perioperative antibiotic prophylactic regimen in preventing surgical site infections (SSI) in open reduction and internal fixation (ORIF) of closed fractures of limbs and to assess if the same can be implemented as a general policy.
Methods:
Patients of either sex, aged 18 yr or more, who were scheduled for ORIF and were willing and able to give informed consent, were included in the study. Patients were randomly allocated into two groups. Group 1 (n=100) received 3 doses of 1 g i.v. cefuroxime perioperatively spaced 12 h apart and group 2 (n=97) received the conventional existing regimen [5 days of i.v. antibiotics (cefuroxime 1 g twice daily along with amikacin 15 mg/kg in 2 divided doses), followed by oral cefuroxime, 500 mg twice daily till suture removal].
Results:
Of the 197 patients, four patients developed a surgical site infection (three with methicillin resistant Staphylococcus aureus and one Acinetobacter baumanii). Of these, two patients were in group 1 and the remaining two in group 2. These patients were treated with i.v. antibiotics based on the culture and antimicrobial sensitivity reports. The cost of the short course treatment was  150 per patient as compared to
150 per patient as compared to  1,900 per patient for conventional regimen.
1,900 per patient for conventional regimen.
Interpretation & conclusions:
There was no significant difference in rates of SSI among the two groups in our study. Cost evaluation revealed that shorter course was less expensive than conventional long course regimen. Implementation of a short course perioperative regimen will go a long way in reducing antimicrobial resistance, cost and adverse reactions to antimicrobials.
Keywords: Antimicrobial prophylaxis, cefuroxime, closed fractures, internal fixation, open reduction
Perioperative antimicrobial prophylaxis constitutes the bulk of antimicrobial consumption in any hospital. Studies done on perioperative prophylactic antibiotics for open reduction and internal fixation of closed fractures are mostly three decades old and do not reflect current orthopaedic management practices, which are now usually done in ultra-clean ventilated operation rooms1–7. Usually, long courses of antibiotic prophylaxis are administered, which are often associated with increasing antimicrobial resistance, super infection with resistant pathogens, toxicity and unnecessary cost8. Rampant and unnecessary administration of antibiotics is one of the major contributors for development of drug resistance9. Large scale interventional studies are required to formulate evidence based guidelines for antibiotic administration. Therefore, this study was conducted at a level 1 Trauma Centre of a tertiary care hospital of India to assess the efficacy of a short course (24 h) of perioperative antibiotic prophylactic regimen in preventing surgical site infections (SSI) in open reduction and internal fixation (ORIF) of closed fractures of limbs and to assess if the same can be implemented as a general policy.
Material & Methods
The study was planned as a two group parallel randomized control trial on the basis of a previous pilot study conducted by us10. Since the expected rate of SSI in both the groups was not very different based on literature and our pilot observation, a large sample size was required to ascertain statistical significance. In view of this, the study was planned for a period of one and a half years. All cases attending Jai Prakash Narayan Apex Trauma Centre, All India Institute of Medical Sciences, New Delhi, and fulfilling the inclusion criteria and willing to enroll were included. The study was conducted from April 2009 to December 2010 and the protocol was approved by the Institute's ethical Committee and registered with Clinical Trial Registry-India (CTRI-2022 - 000243). All patients of either sex, aged 18 yr or more, who were scheduled for open reduction and internal fixation of closed limb fractures and were willing and able to give informed consent were included in the trial. Patients undergoing simple percutaneous Kirschner wire fixation or external fixation; known hypersensitivity to cephalosporins; antimicrobial use or symptoms of infection in the week before surgery; pregnant females; patients on immunosuppressive treatment; patients suffering from compound fractures; patients suffering from multiple fractures; patients having underlying illnesses like diabetes, coronary artery disease, hypertension, chronic obstructive airway disease, any other chronic ailment were excluded.
Participants were randomly allocated to two groups. Group 1 (n=100) received 3 doses of 1 g intravenous (iv) cefuroxime perioperatively spaced 12 h apart (the first dose of which was administered 15-30 min before tourniquet inflation). Group 2 (n=97) received the conventional existing regimen of 5 days of i.v. antibiotics [cefuroxime 1 g twice daily along with amikacin (15 mg/kg in 2 divided doses)], followed by oral cefuroxime, 500 mg twice daily till suture removal.
The randomization was done by the treatment team by the block randomization method (in blocks of 10). The assessor was blinded to the allocation. The follow up of all participants was done by the assessor.
All participants were treated by the standard surgical techniques. They were evaluated for development of wound infections daily till the time of discharge. The wound was clinically observed at 24 and 72 h post-surgery, when the dressings were done. Apart from this, the patients were asked daily for any local pain/discomfort and daily temperature charting was done. A clinical follow up was done between10-14 days when the patient's sutures were removed. Surgical site assessment was also done for patients who came after suture removal for routine follow up in OPD. All surgical wounds infections were initially diagnosed clinically. Surgical wound infection was defined as one or more of classic signs and symptoms of inflammation together with pus at the operation site5,11. The classification of surgical wound infections was done as per standard definitions5,11.
In any case of clinical suspicion of wound infection at surgical site in either group, the following work-up was done: A thorough clinical examination of the wound was done as per standard protocols11. A complete systemic examination was also done. A complete haemogram (haemoglobin, total and differential leucocyte counts, platelet counts and ESR) and liver and kidney function tests were conducted on the first day of clinical suspicion of SSI. The Microbiological investigations included samples like wound swab/ pus/ wound aspirate from the surgical site collected as per standard protocols12. These samples were immediately transported to the Microbiology laboratory in a transport medium. The further processing of samples (culture, identification and antimicrobial susceptibility) was done according to standard microbiological methods12,13. Samples of peripheral blood (5 ml) and urine were taken for culture at the clinician's discretion to rule out other causes of fever.
If infection was either suspected or confirmed clinically in patients of either group, the following protocol was followed to manage them: the specific antibiotics were immediately administered based on the culture and sensitivity report. The wound was managed according to the standard surgical protocols11. If the patients did not respond to medical management, they were scheduled for thorough surgical debridement and irrigation, with or without implant removal, depending on whether the implant was infected or not.
Surveillance cultures of operation theatres, Centre Sterile Supply Department (CSSD), orthopaedics ward and health care workers were taken randomly during the entire study period. The average cost incurred on antimicrobials in both the regimens was also calculated which included the cost of medicine and the hospital stay of the patient during the treatment.
Statistical analysis: For calculating difference in rates of infection, Chi-square test, and relative risk, with 95% confidence interval were used.
Results
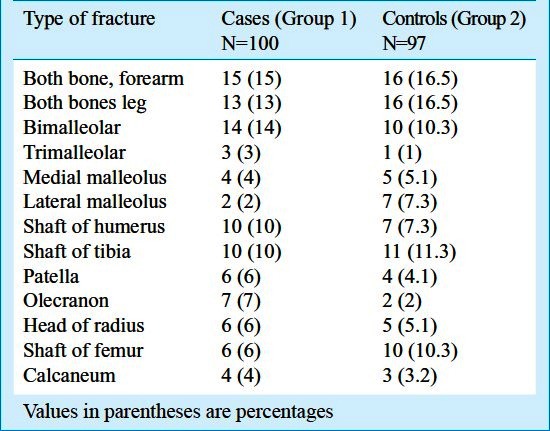
A total of 197 participants were enrolled in the study. The demographic characteristics of the participants are shown in Table I. Both the groups formed after random allocation were matched for their age, gender, type of trauma and distribution of surgeries (Fig.). Of these 197 surgeries, 114 (54.8%) were done under spinal anaesthesia, 56 (28%) were done under general anaesthesia and 27 (14%) were done under epidural anaesthesia. The details of fractures in both groups are shown in Table II. Out of 197 surgeries, ORIF was done in 95 (48%), screw fixation in 41 (21%), plating in 32 (16%), interlocking in 15 (8%) and tension band wiring in 14 (7%) cases.
Table I.
Demographic characteristics of participants in both groups
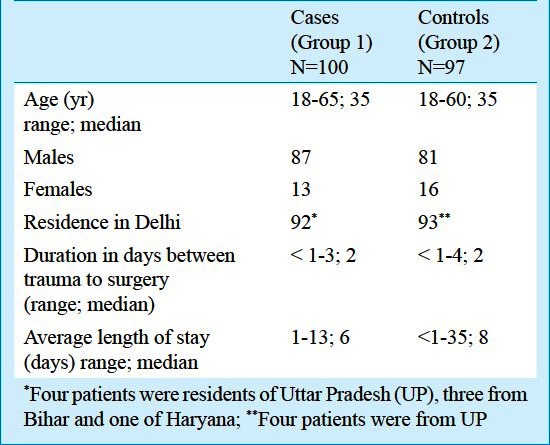
Fig.
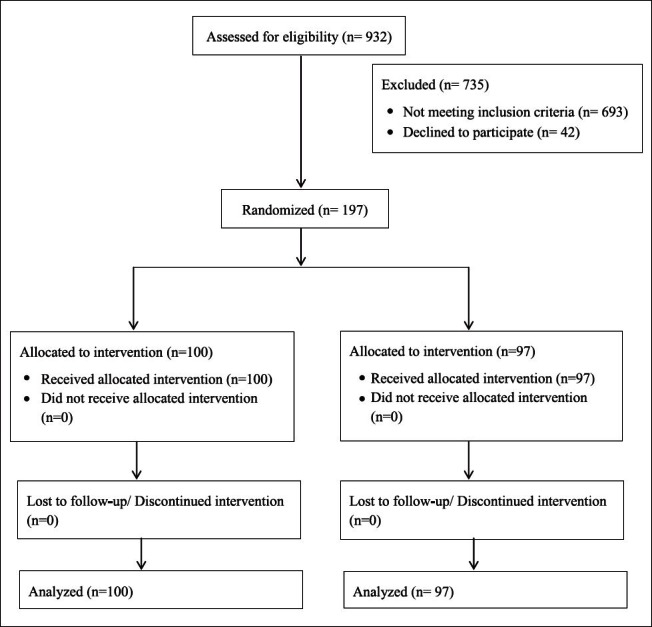
Allocation sequence of participants.
Table II.
Details of type of fractures in study and control groups
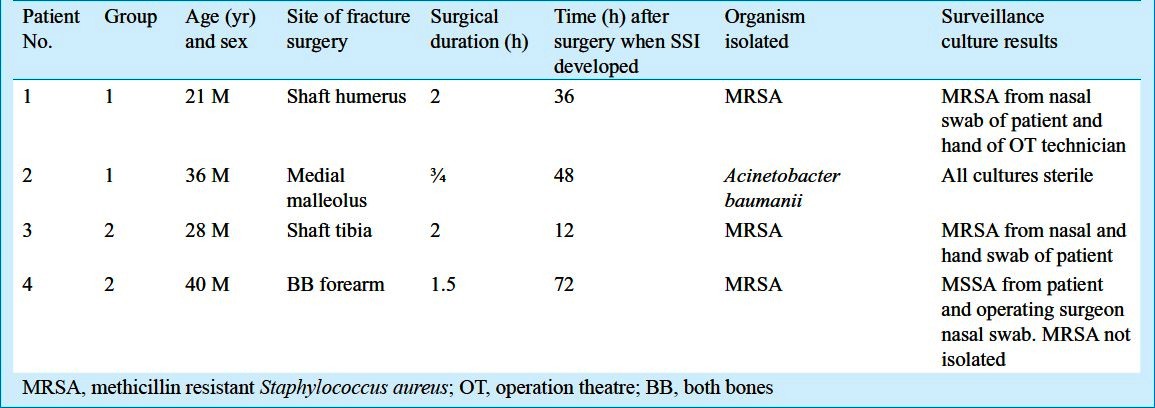
Of the 197 patients enrolled, four developed a surgical site infection. Of these, two patients were in group 1 and the remaining two in group 2. The details of these patients are shown in Table III. Apart from random surveillance cultures as part of Infection Control Programme, surveillance cultures of operation theatres, CSSD, orthopaedics ward and health care workers were taken immediately after finding of SSI in patients. Surveillance cultures of patients and their attendants were also taken in cases of SSIs. In general, the rate of SSI at our centre considering all orthopaedic trauma surgeries has varied from 0.7 to 4.06 per cent over the study period. All these patients were administered culture result based antibiotics. Thus, the first patient in group 1 (whose culture grew methicillin resistant Staphylococcus aureus, MRSA) was administered i.v. vancomycin (1 g B.D) till suture removal. The second patient's sample grew Acinetobacter baumannii, sensitive to piperacillin/tazobactam, cefoperazone/sulbactam, ceftriaxone/sulbactam; cefepime/tazobactam, imipenem, amikacin, netilmicin, meropenem, polymyxin and tigecycline. On the basis of this report, his treatment was modified to include i.v. cefoperazone/sulbactam (2 g, B.D). On examination after 24 h of this regimen, there was good clinical response. Hence the same regimen was continued for 10 days. The first patient in group 2 (whose culture grew MRSA) was already on i.v. antibiotics (amikacin and cefuroxime). He was taken up for exploration and lavage in OT on an urgent basis. The MRSA strain isolated from his pus sample was sensitive only to vancomycin, teichoplanin, linezolid and rifampicin. The patient was administered i.v. teichoplanin (loading dose of 400 mg once, followed by maintenance dose of 200 mg daily), along with the other i.v. antibiotics for 5 days, to which he responded. At the time of discharge, his surgical site was totally healthy. The second patient in group 2 also had MRSA in his wound sample. The patient was treated with i.v. amikacin (already receiving), along with i.v. teichoplanin. The MRSA strain was sensitive to vancomycin, teichoplanin, linezolid, rifampicin, amikacin and levofloxacin.
Table III.
Details of patients who developed surgical site infections (SSIs) and surveillance culture results
The approximate cost incurred on each patient for antimicrobial prophylaxis was also calculated for both the groups. We observed that the average cost of short course treatment amounted to  150 per patient as compared to
150 per patient as compared to  1,900 per patient for prolonged combinational regimens. No adverse side effects were reported in either group due to antimicrobial treatment.
1,900 per patient for prolonged combinational regimens. No adverse side effects were reported in either group due to antimicrobial treatment.
Discussion
Antimicrobial prophylaxis for orthopaedic surgeries is the standard of care. However, the choice of antimicrobial agent and its duration of administration remains a matter of personal choice. With the widespread presence of multi-drug resistant pathogens and limited availability of therapeutic choices, it is important to restrict the usage of broad spectrum antimicrobials, especially their prolonged courses as perioperative prophylaxis. Since perioperative prophylaxis contributes a significant proportion of in-hospital antimicrobial use, its judicious use will also curtail the cost of hospital treatment.
In a systematic review on antibiotic prophylaxis for surgery for proximal femoral and other closed long bone fractures a single dose antibiotic prophylaxis was found to significantly reduce the risk of deep surgical site infections and the use of ceftriaxone was found to be a cost-effective intervention14. Several studies have justified the use of short courses ofa single cephalosporin for clean surgeries, since these act on the most likely organisms causing SSIs15–22. Many of these studies have recommended the use of cefuroxime or cefazoline for upto 24 h post-operation in an optimum dosage6,17. Cefuroxime gives a high bioavailability tissue and serum after a single dose23 and is also efficacious for preventing perioperative infections.
As compared to the developed countries, antimicrobials are overprescribed in developing countries, where an average 35 per cent of health budget is spent on antibiotics24. Perioperative prophylaxis constitutes a major bulk of hospital prescription in these countries. To formulate guidelines for Indian patients, indigenous studies are needed, taking into consideration the high rates of antimicrobial resistance in our population25, the difference in the spectrum of prevalent pathogens in our hospitals and the different socio-economic background of our population as compared to the West. India accounts for 6 per cent of the global vehicular traffic accidents26. Although an increasing number of cases of closed fracture are treated by internal fixation, the duration of antimicrobial treatment in such surgeries are still based on personal preferences.
In our study, there was no difference in rates of SSIs between the two groups. The present rate of SSI (2%) was similar that reported earlier27,28. Although we found no difference in SSI rates in the two groups, the interpretation of the finding is limited in view of the small sample size. The study is underpowered, and thus the confidence intervals are very wide. Thus, our study does not convincingly prove that a short course antimicrobial is more or less effective than the long course regimen.
Shorter courses of perioperative antimicrobials reduce cost, toxicity and development of drug resistance in the long run. Prolonged courses of prophylactic antimicrobials have tremendous economic consequences for health care facilities. In developing nations, such resource saving can be utilized for purchase of other life-saving drugs/devices.
The clean and planned orthopaedic surgeries need to be conducted with utmost aseptic precautions, undermining the importance of appropriate operation theatre protocols in preventing SSIs. Such best-practices should be incorporated in all hospitals as the single most important measure to prevent SSIs29.
In our study, the randomization was done by the treatment group and the clinical follow-up was done by the assessors. Though all measures were taken to reduce the bias, allocation bias and performance bias could have been present. Prolonged follow up of the patients was not done, thus late SSI could not be studied. Another drawback of our study was that molecular studies could not be performed to assess the relatedness of strains isolated from the patients to those from surveillance cultures (in two patients in whom similar organism was isolated). Such a study could have provided evidence of the exact source of perioperative infections.
In conclusion, our findings indicate that a short course of perioperative antimicrobial prophylaxis can be efficacious as well as cost-effective for prevention of infections in developing countries. However, since the sample size was less, larger and multicentric studies covering different regions of the country are required to substantiate the role of short-course prophylaxis in our country.
Acknowledgment
This study was funded by a grant from the Indian Council of Medical Research, New Delhi.
References
- 1.Dellinger EP, Gross PA, Barrett TL, Krause PJ, Martone WJ, McGowan JE, Jr, et al. Quality standard for antimicrobial prophylaxis in surgical procedures.Infectious Diseases society of America. Clin Infect Dis. 1994;18:422–7. doi: 10.1093/clinids/18.3.422. [DOI] [PubMed] [Google Scholar]
- 2.Stolle D, Naumann P, Kremer K, Loose DA. Antibiotic prophylaxis in traumatologie. HefteUnfallheilkd. 1980;143(Suppl):1–55. [PubMed] [Google Scholar]
- 3.Hughes SP, Miles RS, Littlejohn M, Brown E. Is antibiotic prophylaxis necessary for internal fixation of low - energy fractures? Injury. 1991;22:111–3. doi: 10.1016/0020-1383(91)90067-o. [DOI] [PubMed] [Google Scholar]
- 4.Bergman BR. Antibiotic prophylaxis in open and closed fractures: a controlled clinical trial. Acta Orthop Scand. 1982;53:57–62. doi: 10.3109/17453678208992179. [DOI] [PubMed] [Google Scholar]
- 5.Boxma H, Broekhuizen T, Patka P, Oosting H. Randomised controlled trial of single - dose antibiotic prophylaxis in surgical treatment of closed fractures: the Dutch trauma trial. Lancet. 1996;347:1133–7. doi: 10.1016/s0140-6736(96)90606-6. [DOI] [PubMed] [Google Scholar]
- 6.Yeap JS, Lim JW, Vergis M, Au Yeung PS, Chiu CK, Singh H. Prophylactic antibiotics in orthopedic surgery: guidelines and practice. Med J Malaysia. 2006;61:181–8. [PubMed] [Google Scholar]
- 7.Hauser CJ, Adams CA, Jr, Eachempati SR. Council of the Surgical Infection Society. Surgical Infection Society Guidelines: prophylactic antibiotic use in open fractures: an evidence based guideline. Surg Infect (Larchmt) 2006;7:379–405. doi: 10.1089/sur.2006.7.379. [DOI] [PubMed] [Google Scholar]
- 8.Wendy Munckhof Antibioties for surgical prophylaxes. Aus Prescr. 2005;28:38–40. [Google Scholar]
- 9.Mathur P, Kapil A, Das B, Dhawan B. Prevalence of extended spectrum beta lactamase producing Gram-negative bacteria in a tertiary care hospital. Indian J Med Res. 2002;115:153–7. [PubMed] [Google Scholar]
- 10.Kumar S, Behera B, Farooque K, Sharma V, Mathur P. Efficacy of a short course antibiotic prophylaxis for open reduction of closed fractures: first report from India. J Assoc Physicians India. 2010;58:124–5. [PubMed] [Google Scholar]
- 11.Leaper DJ. Wound infections. In: Russell RCG, Williams NS, Bulstrode CJK, editors. Bailey & Love's short practice of surgery. 24th ed. London: Arnold; 2004. [Google Scholar]
- 12.Collee JG, Miles RS, Watt B. Tests for the identification of bacteria. In: Collee JG, Fraser AG, Marmion BP, Simmons A, editors. Mackie and McCartney practical medical microbiology. 14th ed. New York: Churchill Livingstone; 1996. pp. 131–45. [Google Scholar]
- 13.Performance standards for antimicrobial susceptibility testing. Wayne, PA: CLSI; 2005. Clinical and Laboratory Standard Institute. 15th informational supplement. CLSI/NCCLS document M 100-S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gillespie WJ, Walenkamp GHIM. Antibiotic prophylaxis for surgery for proximal femoral and other closed long bone fractures. Cochrane Database Syst Rev. 2010;(3):CD000244. doi: 10.1002/14651858.CD000244.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meehan J, Jamali AA, Nguyen H. Prophylactic antibiotics in hip and knee arthroplasty. J Bone Joint Surg Am. 2009;91:2480–90. doi: 10.2106/JBJS.H.01219. [DOI] [PubMed] [Google Scholar]
- 16.Percin S, Akbas L, Akbas A. A single preoperative dose of cefazolinvesuspost operative amoxicillin and gentamycin combination in prophylaxis of orthopaedic and traumatologic surgery. Mater Med Pol. 1992;24:24–7. [PubMed] [Google Scholar]
- 17.Wymenga A, van Horn J, Theeuwes A, Muytjens H, Slooff T. Cefuroxime for prevention of postoperative coxitis.One versus three doses tested in a randomized multicenter study of 2,651 arthoplasties. Acta Orthop Scand. 1992;63:19–24. doi: 10.3109/17453679209154842. [DOI] [PubMed] [Google Scholar]
- 18.Kaukonen JP, Kemppainen E, Mäkijärvi J, Tuominen T. One dose cefuroxime prophylaxis in hip fracture surgery. Ann Chir Gynaecol. 1995;84:417–9. [PubMed] [Google Scholar]
- 19.Queiroz R, Grinbaum RS, Galvao LL, Tavares FG, Bergsten-Mendes G. Antibiotic prophylaxis in orthopedic surgeries: the results of an implemented protocol. Braz J Infect Dis. 2005;9:283–7. doi: 10.1590/s1413-86702005000400003. [DOI] [PubMed] [Google Scholar]
- 20.Gyssens IC. Preventing postoperative infections: current treatment recommendations. Drugs. 1999;57:175–85. doi: 10.2165/00003495-199957020-00004. [DOI] [PubMed] [Google Scholar]
- 21.Court- Brown CM. Antibiotic prophylaxis in orthopaedic surgery. Scand J Infect Dis. 1990;70(Suppl):74–9. [PubMed] [Google Scholar]
- 22.Oishi CS, Carrion WV, Hoaglund FT. Use of parenteral prophylactic antibiotics in clean orthopaedic surgery. A review of the literature. Clin Orthop Relat Res. 1993;296:249–55. [PubMed] [Google Scholar]
- 23.Kaukonen JP, Tuomainen P, Mäkijärvi J, Mokka R, Männistö PT. Intravenous cefuroxime prophylaxis. Tissue levels after one 3-gram dose in 40 cases of hip fracture. Acta Orthop Scand. 1995;66:14–6. doi: 10.3109/17453679508994631. [DOI] [PubMed] [Google Scholar]
- 24.Ozkurt Z, Erol S, Kadanali A, Ertek M, Ozden K, Tasyaran MA. Changes in antibiotic use, cost and consumption after an antibiotic restriction policy applied by infectious disease specialists. Jpn J Infect Dis. 2005;58:338–43. [PubMed] [Google Scholar]
- 25.Behera B, Mathur P. High levels of antimicrobial resistance at a tertiary trauma care centre of India. Indian J Med Res. 2011;133:343–5. [PMC free article] [PubMed] [Google Scholar]
- 26.Joshipura MK, Shah HS, Patel PR, Divatia PA, Desai PM. Trauma care systems in India. Injury. 2003;34:686–92. doi: 10.1016/s0020-1383(03)00163-3. [DOI] [PubMed] [Google Scholar]
- 27.Suzuki T, Morgan SJ, Smith WR, Stahel PF, Gillani SA, Hak DJ. Postoperative surgical site infection following acetabular fracture fixation. Injury. 2010;41:396–9. doi: 10.1016/j.injury.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 28.Merrer J, Girou E, Lortat-Jacob A, Montravers P, Lucet JC. Surgical site infection after surgery to repair femoral neck fracture: a French multicenter retrospective study. Infect Control Hosp Epidemiol. 2007;28:1169–74. doi: 10.1086/520745. [DOI] [PubMed] [Google Scholar]
- 29.Ayliffe GA. Role of the environment of the operating suite in surgical wound infection. Rev Infect Dis. 1991;13(Suppl 10):S800–4. doi: 10.1093/clinids/13.supplement_10.s800. [DOI] [PubMed] [Google Scholar]


