Abstract
Background:
Laparoscopic cholecystectomy is associated with shorter hospital stay and less pain in comparison to open surgery. The aim of this study was to evaluate the effect of intraperitoneal hydrocortisone on pain relief following laparoscopic cholecystectomy.
Methods:
Sixty two patients were enrolled in a double-blind, randomized clinical trial. Patients randomly received intraperitoneal instillation of either 250 ml normal saline (n=31) or 100 mg hydrocortisone in 250 ml normal saline (n=31) before insufflation of CO2 into the peritoneum. Abdominal and shoulder pain were evaluated using VAS after surgery and at 6, 12, and 24 hours postoperatively. The patients were also followed for postoperative analgesic requirements, nausea and vomiting, and return of bowel function.
Results:
Sixty patients completed the study. Patients in the hydrocortisone group had significantly lower abdominal and shoulder pain scores (10.95 vs 12.95; P<0.01). The patients were similar regarding analgesic requirements in the recovery room. However, those in the hydrocortisone group required less meperidine than the saline group (151.66 (±49.9) mg vs 61.66 (±38.69) mg; P=0.00). The patients were similar with respect to return of bowel function, nausea and vomiting. No adverse reaction was observed in either group.
Conclusion:
Intraperitoneal administration of hydrocortisone can significantly decrease pain and analgesic requirements after laparoscopic cholecystectomy with no adverse effects.
Keywords: Cholecystectomy, intraperitoneal hydrocortisone, laparoscopy, postoperative pain
INTRODUCTION
Laparoscopic cholecystectomy is the treatment of choice for symptomatic cholelithiasis. Although there are clear benefits compared with open surgery, postoperative pain is still a common complaint after laparoscopic cholecystectomy. Pain can prolong hospital stay and lead to increased morbidity, which is particularly important in centers performing this operation as a day-case procedure.[1] Different methods have been proposed to relieve postoperative pain following laparoscopic cholecystectomy.[2–4]
Administration of intraperitoneal local anesthetics alone[5–7] or in combination with nonopioid analgesics[8,9] have been used to reduce postoperative pain following laparoscopic cholecystectomy. This might reduce adverse effects of opioids′
On the other hand, steroids have also been used successfully for postoperative pain relief in different kinds of surgery.[10–12]
The purpose of this study was to assess the effect of intraperitoneal hydrocortisone to reduce postoperative pain after laparoscopic cholecystectomy under general anesthesia. The primary outcome was to compare pain scores. The secondary outcomes included postoperative analgesic requirements, frequency of nausea and vomiting, length of hospital stay, time of return of bowel function, time of unassisted ambulation, and time of oral intake.
METHODS
After approval of the local ethics committee and informed consent, 62 patients of ASA physical status I-II scheduled for elective laparoscopic cholecystectomy were recruited for the study. The exclusion criteria were chronic pain diseases other than gallstone disease, use of opioids, tranquilizers, steroids, NSAIDs, and alcohol, patients with acute cholecystitis, allergy to corticosteroids, neuromuscular diseases and bleeding disorders.
After receiving 5 ml/kg crystalloids, preoxygenation with 100% O2 for 3 minutes, 2 μg/kg of fentanyl and 0.05 mg/kg of midazolam, anesthesia was induced with thiopenthal 5 mg/kg followed by 0.15 mg/kg of cisatracurium to facilitate endotracheal intubation. Anesthesia was maintained with 60% N2O in oxygen and propofol 4-6 mg/kg/hr (to keep cerebral state index at 40-60) and remifentanyl 0.05-0.5 μg/kg/min (to maintain mean arterial blood pressure and pulse rates within 20% of the baseline). All patients received 1 μg/kg of fentanyl 5 minutes before the end of operation to reduce postoperative pain.
After receiving the standard anesthesia and before insufflations of CO2, the patients were randomized to receive either instillation of 250 ml of normal saline or 100 mg hydrocortisone in 250 ml normal saline into the peritoneum by a surgical scrub nurse who was blind to the study. The patients were then rotated into Trendelenburg, anti-Trendelenburg, left and right lateral decubitus, and finally supine positions (each for 2 minutes). Nasogastric tube was inserted for all patients after induction and was removed at the end of the surgery. All surgical procedures were performed by a single surgeon. During laparoscopy, intra-abdominal pressure was maintained at 14 mmHg. Carbon dioxide was carefully evacuated at the end of surgery by manual compression of the abdomen with open trocars. Ten milliliters of bupivacaine 0.25% was injected in laparoscopy entering sites. Patients were followed by a blind investigator for postoperative abdominal and shoulder pain using VAS based on a 0-10 scale (with 0 meaning no pain and 10 meaning the most intense pain ever experienced), postoperative analgesic requirements, presence of nausea and vomiting, time of unassisted ambulation, time of oral intake and time of return of bowel function in the recovery room and at 6, 12 and 24 hours after operation. Time of return of bowel function was defined as the time from end of anesthesia until presence of intestinal sound or first passage of flatus.
We used intramuscular meperidine 0.5 mg/kg and 1 mg/kg as rescue analgesic for VAS 4-7, and 8-10, respectively.
Using SPSS software for Windows, version 11(SPSS Inc, Chicago, IL, USA), arithmetic mean and standard deviation values for different variables were calculated and statistical analyses were performed for each group. We used independent Student t-test to compare continuous variables exhibiting normal distribution, and Chi-square test and Mann-Whitney U test for noncontinuous variables. P value less than 0.05 was considered significant.
RESULTS
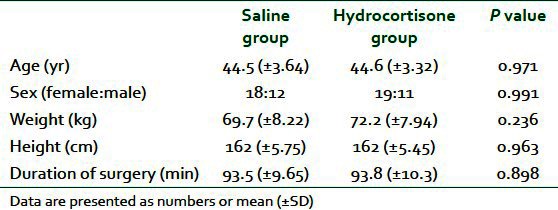
Sixty patients completed the study. Two were excluded since conversion to open cholecystectomy was necessary in both cases because of dense inflammatory adhesions. There were no statistically significant differences between the two groups in terms of demographic data and duration of surgery [Table 1].
Table 1.
Patients data and operation characteristics
The patients were similar with respect to factors likely to increase postoperative pain including: Bile spillage from punctured gallbladder, difficult dissection due to adhesions from previous surgery, bleeding, need to cholangiography, injury to bowels or other organs, and insertion of drain.
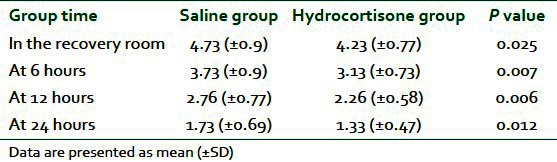
The abdominal and shoulder pain scores were significantly lower in the hydrocortisone group in the recovery room and at 6, 12, and 24 hours postoperatively (total scores 10.95 vs 12.95 in the hydrocortisone and saline group, respectively; P<0.01) [Table 2].
Table 2.
Visual analog pain scores in the two groups
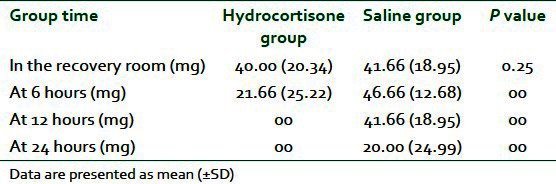
The patients were similar regarding analgesic requirements in the recovery room. Nevertheless, patients in the saline group required more meperidine than the hydrocortisone group (151.66 (±49.9) mg vs 61.66 (±38.69); P=0.00)] [Table 3].
Table 3.
Postoperative meperidine requirements in the two groups
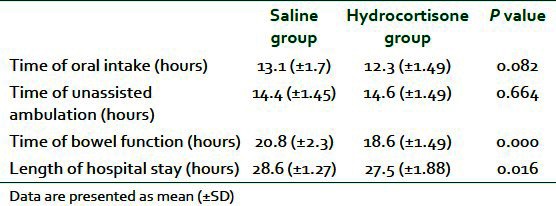
The patients were similar with respect to frequency of nausea and vomiting, length of hospital stay, time of return of bowel function, time of unassisted ambulation, and time of oral intake [Table 4].
Table 4.
Recovery variables between two groups
DISCUSSION
We demonstrated that intraperitoneal injection of hydrocortisone can reduce pain and analgesic requirements following laparoscopic cholecystectomy without significant side effects.
Provision of adequate postoperative pain relief is of considerable importance following day-case laparoscopic cholecystectomy.[1] Pain after laparoscopic cholecystectomy is affect by several factors including patient demographics, nature of underlying disease, surgical factors, volume of residual gas, type of gas used for pneumoperitoneum, and the pressure created by the pneumoperitoneum.[13–18] A number of techniques have been described for reducing postlaparoscopy pain including: Preincisional infiltration and intraperitoneal instillation of levobupivacaine 0.25%;[19] intraperitoneal ropivacaine and a gas drain;[20] intraperitoneal levobupivacaine with epinephrine;[21] intraperitoneal application of bupivacaine plus morphine;[22] preincisional injection of bupivacaine;[23] pre-emptive intraperitoneal injection of ropivacaine;[24] and intraperitoneal lidocaine combined with intravenous or intraperitoneal tenoxicam.[25] It is suggested that post-laparoscopic cholecystectomy pain is multifactorial and methods for short term analgesia cannot improve postoperative functions or shortened hospitalization.[26]
It has been shown that glucocorticoids can play a crucial role in the regulation of inflammatory responses through both genomic and nongenomic mechanisms and therefore may reduce pain.[27] Among corticosteroids, dexamethasone has been used widely to reduce postoperative pain.[28–30] The mechanism of analgesic effect of steroids is not well known.
The proposed mechanisms include: Suppression of tissue levels of bradykinin and the release of neuropeptides from nerve endings; reduction in prostaglandin production resulting in inhibition of the synthesis of the cyclooxygenase isoform-2 in peripheral tissues and in the central nervous system; and inhibition of other mediators of inflammatory hyperalgesia, for example, tumor necrosis factor-a, interleukin-17b, and interleukin-6.
The effect of intraperitoneal corticosteroids on pain after elective laparoscopic cholecystectomy has not been investigated. We assumed that early postoperative pain was mainly generated by irritation of the peritoneum, and the application of corticosteroids may attenuate this pain.
We used intraperitoneal hydrocortisone successfully to reduce pain following laparoscopic cholecystectomy. Although meperidine requirement was similar in both groups in the recovery room, patients in the hydrocortisone group required less analgesic afterwards. This might be attributed to short analgesic effect of intraoperative remifentanil.
In conclusion, our study showed that intraperitoneal injection of hydrocortisone before gas insufflation in laparoscopic cholecystectomy can reduce postoperative pain with no significant postoperative adverse effect.
ACKNOWLEDGMENT
We would like to thank Imam Ali hospital personnel in the general operating room and surgical ward for their contribution to this study. This study was financially supported by the research deputy of Zahedan University of Medical Sciences, Zahedan, Iran.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Boddy AP, Mehta S, Rhodes M. The effect of intraperitoneal local anesthesia in laparoscopic cholecystectomy: A systematic review and meta-analysis. Anesth Analg. 2006;103:682–8. doi: 10.1213/01.ane.0000226268.06279.5a. [DOI] [PubMed] [Google Scholar]
- 2.Abdulla S, Eckhardt R, Netter U, Abdulla W. A randomized double-blind, controlled trial on non-opioid analgesics and opioid consumption for postoperative pain relief after laparoscopic cholecystectomy. Acta Anaesthesiol Belg. 2012;63:43–50. [PubMed] [Google Scholar]
- 3.Salihoglu Z, Yildirim M, Demiroluk S, Kaya G, Karatas A, Ertem M, et al. Evaluation of intravenous paracetamol administration on postoperative pain and recovery characteristics in patients undergoing laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2009;19:321–3. doi: 10.1097/SLE.0b013e3181b13933. [DOI] [PubMed] [Google Scholar]
- 4.Akaraviputh T, Leelouhapong C, Lohsiriwat V, Aroonpruksakul S. Efficacy of perioperative parecoxib injection on postoperative pain relief after laparoscopic cholecystectomy: A prospective, randomized study. World J Gastroenterol. 2009;15:2005–8. doi: 10.3748/wjg.15.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khan MR, Raza R, Zafar SN, Shamim F, Raza SA, Inam Pal KM, et al. Intraperitoneal lignocaine (lidocaine) versus bupivacaine after laparoscopic cholecystectomy: Results of a randomized controlled trial. J Surg Res. 2012;178:662–9. doi: 10.1016/j.jss.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Beqiri AI, Domi RQ, Sula HH, Zaimi EQ, Petrela EY. The combination of infiltrative bupivacaine with low-pressure laparoscopy reduces postcholecystectomy pain. A prospective randomized controlled study. Saudi Med J. 2012;33:134–8. [PubMed] [Google Scholar]
- 7.El-Labban GM, Hokkam EN, El-Lab ban MA, Morsy K, Saadl S, Heissam KS. Intraincisional vs intraperitoneal infiltration of local anaesthetic for controlling early post-laparoscopic cholecystectomy pain. J Minim Access Surg. 2011;7:173–7. doi: 10.4103/0972-9941.83508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Golubović S, Golubović V, Cindrić-Stancin M, Tokmadzić VS. Intraperitoneal analgesia for laparoscopic cholecystectomy: bupivacaine versus bupivacaine with tramadol. Coll Antropol. 2009;33:299–302. [PubMed] [Google Scholar]
- 9.Roberts KJ, Gilmour J, Pande R, Nightingale P, Tan LC, Khan S. Efficacy of intraperitoneal local anaesthetic techniques during laparoscopic cholecystectomy. Surg Endosc. 2011;25:3698–705. doi: 10.1007/s00464-011-1757-3. [DOI] [PubMed] [Google Scholar]
- 10.Choi YS, Shim JK, Song JW, Kim JC, Yoo YC, Kwak YL. Combination of pregabalin and dexamethasone for postoperative pain and functional outcome in patients undergoing lumbar spinal surgery: A randomized placebo-controlled trial. Clin J Pain. 2012, In Press doi: 10.1097/AJP.0b013e318246d1a9. [DOI] [PubMed] [Google Scholar]
- 11.Buland K, Zahoor MU, Asghar A, Khan S, Zaid AY. Efficacy of single dose perioperative intravenous steroid (dexamethasone) for postoperative pain relief in tonsillectomy patients. J Coll Physicians Surg Pak. 2012;22:349–52. [PubMed] [Google Scholar]
- 12.Safavi M, Honarmand A, Habibabady MR, Baraty S, Aghadavoudi O. Assessing intravenous ketamine and intravenous dexamethasone separately and in combination for early oral intake, vomiting and postoperative pain relief in children following tonsillectomy. Med Arh. 2012;66:111–5. doi: 10.5455/medarh.2012.66.111-115. [DOI] [PubMed] [Google Scholar]
- 13.Koc M, Ertan T, Tez M, Kocpinar MA, Kilic M, Gocmen E, et al. Randomized, prospective comparison of postoperative pain in low-versus high-pressure pneumoperitoneum. ANZ J Surg. 2005;75:693–6. doi: 10.1111/j.1445-2197.2005.03496.x. [DOI] [PubMed] [Google Scholar]
- 14.Ekici Y, Bozbas H, Karakayali F, Salman E, Moray G, Karakayali H, et al. Effect of different intra-abdominal pressure levels on QT dispersion in patients undergoing laparoscopic cholecystectomy. Surg Endosc. 2009;23:2543–9. doi: 10.1007/s00464-009-0388-4. [DOI] [PubMed] [Google Scholar]
- 15.Bisgaard T, Kehlet H, Rosenberg J. Pain and convalescence after laparoscopic cholecystectomy. Eur J Surg. 2001;167:84–96. doi: 10.1080/110241501750070510. [DOI] [PubMed] [Google Scholar]
- 16.Sandhu T, Yamada S, Ariyakachon V, Chakrabandhu T, Chongruksut W, Ko-iam W. Low-pressure pneumoperitoneum versus standard pneumoperitoneum in laparoscopic cholecystectomy, a prospective randomized clinical trial. Surg Endosc. 2009;23:1044–7. doi: 10.1007/s00464-008-0119-2. [DOI] [PubMed] [Google Scholar]
- 17.Wills VL, Hunt DR. Pain after laparoscopic cholecystectomy. Br J Surg. 2000;87:273–84. doi: 10.1046/j.1365-2168.2000.01374.x. [DOI] [PubMed] [Google Scholar]
- 18.O'Boyle CJ, deBeaux AC, Watson DI, Ackroyd R, Lafullarde T, Leong JY, et al. Helium Vs Carbon Dioxide gas insufflation with or without saline lavage during laparoscopy: A randomized trial. Surg Endosc. 2002;16:620–5. doi: 10.1007/s00464-001-8218-3. [DOI] [PubMed] [Google Scholar]
- 19.Louizos AA, Hadzilia SJ, Leandros E, Kouroukli IK, Georgiou LG, Bramis JP. Postoperative pain relief after laparoscopic cholecystectomy: A placebo-controlled double-blind randomized trial of preincisional infiltration and intraperitoneal instillation of levobupivacaine 0.25% Surg Endosc. 2005;19:1503–6. doi: 10.1007/s00464-005-3002-4. [DOI] [PubMed] [Google Scholar]
- 20.Readman E, Maher PJ, Ugoni AM, Gordon S. Intraperitoneal ropivacaine and a gas drain: Effects on postoperative pain in laparoscopic surgery. J Am Assoc Gynecol Laparosc. 2004;11:486–91. doi: 10.1016/s1074-3804(05)60080-1. [DOI] [PubMed] [Google Scholar]
- 21.Ng A, Swami A, Smith G, Robertson G, Lloyd DM. Is intraperitoneal levobupivacaine with epinephrine useful for analgesia following laparoscopic cholecystectomy? A randomized controlled trial. Eur J Anaesthesiol. 2004;21:653–7. doi: 10.1017/s0265021504008117. [DOI] [PubMed] [Google Scholar]
- 22.Hernandez-Palazon J, Tortosa JA, Nuno de la Rosa V, Gimenez-Viudes J, Ramirez G, Robles R. Intraperitoneal application of bupivacaine plus morphine for pain relief after laparoscopic cholecystectomy. Eur J Anaesthesiol. 2003;20:891–6. doi: 10.1017/s0265021503001431. [DOI] [PubMed] [Google Scholar]
- 23.Lepner U, Goroshina J, Samarutel J. Postoperative pain relief after laparoscopic cholecystectomy: A randomised prospective double-blind clinical trial. Scand J Surg. 2003;92:121–4. [PubMed] [Google Scholar]
- 24.Maestroni U, Sortini D, DEvito C, Pour Morad Kohan Brunaldi F, Anania G, Pavanelli L, et al. A new method of preemptive analgesia in laparoscopic cholecystectomy. Surg Endosc. 2002;16:1336–40. doi: 10.1007/s00464-001-9181-8. [DOI] [PubMed] [Google Scholar]
- 25.Elhakim M, Amine H, Kamel S, Saad F. Effects of intraperitoneal lidocaine combined with intravenous or intraperitoneal tenoxicam on pain relief and bowel recovery after laparoscopic cholecystectomy. Acta Anaesthesiol Scand. 2000;44:929–33. doi: 10.1034/j.1399-6576.2000.440806.x. [DOI] [PubMed] [Google Scholar]
- 26.Wills VL, Hunt DR. Pain after laparoscopic cholecystectomy. Br J Surg. 2000;87:273–84. doi: 10.1046/j.1365-2168.2000.01374.x. [DOI] [PubMed] [Google Scholar]
- 27.Lim G, Wang S, Zeng Q, Sung B, Mao J. Spinal glucocorticoid receptors contribute to the development of morphine tolerance in rats. Anesthesiology. 2005;102:832–7. doi: 10.1097/00000542-200504000-00020. [DOI] [PubMed] [Google Scholar]
- 28.Jo YY, Yoo JH, Kim HJ, Kil HK. The effect of epidural administration of dexamethasone on postoperative pain: A randomized controlled study in radical subtotal gastrectomy. Korean J Anesthesiol. 2011;61:233–7. doi: 10.4097/kjae.2011.61.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Oliveira GS, Jr, Almeida MD, Benzon HT, McCarthy RJ. Perioperative single dose systemic dexamethasone for postoperative pain: A meta-analysis of randomized controlled trials. Anesthesiology. 2011;115:575–88. doi: 10.1097/ALN.0b013e31822a24c2. [DOI] [PubMed] [Google Scholar]
- 30.Hong JY, Han SW, Kim WO, Kim EJ, Kil HK. Effect of dexamethasone in combination with caudal analgesia on postoperative pain control in day-case paediatric orchiopexy. Br J Anaesth. 2010;105:506–10. doi: 10.1093/bja/aeq187. [DOI] [PubMed] [Google Scholar]


