Abstract
Background:
Clinically optimized focusing of drug administration to specific need of patient with bispectral index (BIS) monitoring results in reduced dose and faster recovery of consciousness. This study was planned with an aim to study and compare the conventional clinical end point or BIS on the requirement of dosage of propofol, hemodynamic effects, and BIS alterations following propofol induction.
Methods:
70 patients, ASA I and II, 20-60 years undergoing elective surgical procedure under general anesthesia with endotracheal intubation were selected and divided into two groups. Group A received (inj.) fentanyl (2 μg/kg), followed 3 min later by inj. propofol at the rate of 30 mg/kg/hr infusion till the loss of response to verbal command while group B received inj. fentanyl (2 μg/kg), followed 3 min later by inj. propofol at the rate of 30 mg/kg/hr infusion. The end point of hypnosis was when the BIS value was sustained for 1 min at 48±2. The patients were intubated. Total induction dose of propofol was noted in each group. The value of BIS and hemodynamic parameters (heart rate, systolic/diastolic blood pressure) were noted at the time of loss of consciousness, at the time of intubation, and 1 min after intubation, thereafter every minute for first 10 min and thereafter every 10 min till end of surgery. Any involuntary muscle activity such as jerky movements, dystonic posturing, and opisthotonos were also recorded.
Results:
The mean dose of propofol used in groups A and B were 1.85±0.48 mg/kg and 1.79±0.41 mg/kg, respectively. The dosage used in group B were less but not clinically significant (P=0.575). On comparing the dosage of propofol in males among the groups there was a significantly lower dosage of propofol required in group B (2.06±0.45 mg/kg and 1.83±0.32 mg/kg, respectively, P=0.016). This decrease however was not seen in female patients dosage being 1.65±0.44 mg/kg and 1.75±0.49 mg/kg, respectively (P=0.372). The hemodynamic variables including heart rate, systolic/diastolic blood pressure and BIS were comparable within the group at induction, post-induction, and intubation. However, there was a significant increase in all the parameters at postintubation readings (P<0.001).
Conclusion:
No significant difference in the induction dose of propofol was observed when assessed clinically (loss of verbal response) or by BIS monitoring. Traditional teaching to titrate the dose of propofol and depth of anesthesia during intubation by loss of verbal response is as good as BIS value monitoring.
Keywords: Anesthesia management, bispectral index, dosage, propofol
INTRODUCTION
Anesthesia is a balance between anesthetic drug requirement and the state of arousal of the patient. Inadequate doses lead to increased incidence of awareness, while generous administration of drugs leads to hemodynamic instability, delayed recovery, and increase in other complications.[1]
In the absence of central nervous system monitoring, hypnotic agents are traditionally administered on the basis of fixed dose regimen adjusted to the response of patient judged by clinical parameters including loss of verbal response. The fixed dosing regimen however does not take into account the pharmacokinetic or pharmacodynamic variability between patients and may be a cause of frequent over or under dosing of induction agent in patients. Bispectral index (BIS) monitor is used to monitor hypnosis and depth of anesthesia. Clinically optimized focusing of drug administration to a specific need of patient with BIS monitoring results in reduced dosage of anesthetic agents and faster recovery of consciousness. BIS value between 40 and 60 reflects adequate hypnotic effect of general anesthesia with reasonably rapid recovery of consciousness.[2]
We hypothesized that BIS-guided propofol induction leads to an optimal depth of anesthesia without causing hemodynamic fluctuations as compared to a conventional clinical technique of propofol induction. This study was planned with an aim to study the clinical characteristics and hemodynamic alterations during propofol induction guided by clinical signs or BIS level.
METHODS
This randomized, prospective, controlled trial was undertaken after taking the Institutional Ethics Committee approval and written informed consent from patient. The study involved 70 patients of either sex, 20-60 year old, American Society of Anesthesiologists (ASA) physical class I and II undergoing surgical procedures under general anesthesia and requiring endotracheal intubation. Patients having history of stroke, stupor, dementia, long-term use of central nervous system (CNS) activator drugs, benzodiazepines and/or opiates therapy, and pregnant females were excluded from the study.
The patients were premedicated with oral diazepam 10 mg on the night before and 2 hr prior to surgery. On arrival to the operating room, intravenous access was established with an 18 G intravenous cannula. Standard monitoring like 5-lead electrocardiogram (ECG), non-invasive blood pressure (NIBP), pulse oximeter, BIS sensor, and BIS monitor A-2000TM were applied and baseline parameters were noted.
The patients were divided into two groups by simple random sampling by sealed envelope method:
Group A: The induction of anesthesia was done with intravenous injection of fentanyl (2 μg/kg), followed 3 min later by infusion of propofol at the rate of 30 mg/kg/hr till the loss of response to verbal command
Group B: The induction of anesthesia was performed with intravenous fentanyl (2 μg/kg), followed 3 min later by propofol infusion at the rate of 30 mg/kg/hr. The end point of hypnosis was sustained BIS value of 48±2 for 1 min.
In each group, after induction of anesthesia with end point of hypnosis as per group allocation the ease of mask ventilation was checked, vecuronium bromide in dose of 0.1 mg/kg was administered and patients were ventilated with 66% nitrous oxide in oxygen for 3 min. Tracheal intubation was completed with appropriate sized cuffed endotracheal tube. Anesthesia was maintained with 66% nitrous oxide in oxygen, isoflurane to maintain BIS value between 40 and 60, intermittent boluses of vecuronium and fentanyl 1 μg/kg. At the end of surgery, the residual neuromuscular block was reversed with intravenous neostigmine (0.05 mg/kg) and glycopyrrolate (0.01 mg/kg) and trachea was extubated, and patients were shifted to post anesthesia care unit. Neuromuscular monitoring was not used in our study.
The total dose of propofol administered to attain the desired end points as loss of verbal response (group A) or BIS of 48±2 (group B) were recorded. The values of BIS and hemodynamic parameters (heart rate, systolic/diastolic blood pressure) were recorded at the time of loss of consciousness, intubation, every minute for first 10 min after intubation and thereafter every 10 min till the end of surgery. Any involuntary muscle activity after propofol induction such as jerky movements, dystonic posturing, and opisthotonos was also recorded.
Statistical analysis
Data processing was done utilizing Excel and SPSS package. The unpaired t test was used for comparison of data between the different groups while the paired t test was utilized for comparison of data within the same group. P<0.05 was considered statistically significant.
RESULTS
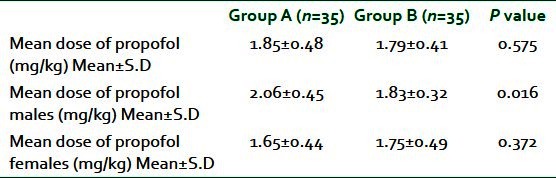
Seventy patients were randomized into two groups and no patient was excluded from the study analysis. The demographic parameters were comparable between the groups [Table 1]. The mean dose of propofol used for induction was 1.85±0.48 mg/kg (group A) and 1.79±0.41 mg/kg (group B), respectively. The dosage of propofol in group B were less compared to group A, but it was not statistically significant (P=0.575) [Table 2]. Males in group A required 2.06±0.45 mg/kg propofol for induction, while the female patients required the dose of 1.65±0.44 mg/kg. This difference in dosage of propofol was statistically significant (P=0.0002). In group B, mean dose of propofol for induction for male and female patients was 1.83±0.32 and 1.75±0.49 mg/kg respectively and was statistically insignificant (P=0.421). On comparing the dosage of propofol among males of the two groups, a significantly lower dosage of propofol was observed in group B (2.06±0.45 mg/kg and 1.83±0.32 mg/kg, respectively, P=0.016). This decrease however was not observed among female patients, dosage being 1.65±0.44 mg/kg and 1.75±0.49 mg/kg, respectively (group A versus group B) (P=0.372).
Table 1.
Demographic profile in the two groups
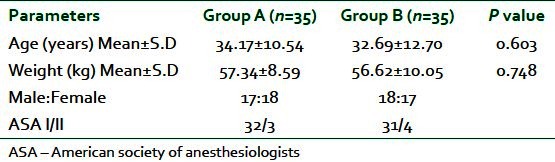
Table 2.
Dosage of propofol in the two groups
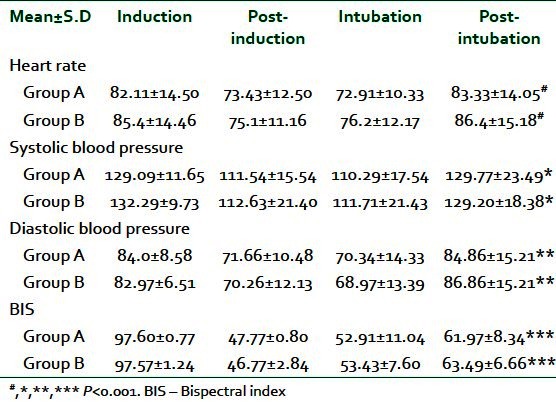
The hemodynamic variables including heart rate, systolic/diastolic blood pressure, and BIS were comparable between the groups at time of induction, post-induction, and intubation. A significant increase in heart rate, blood pressure, and BIS values was observed post-intubation (P<0.001) [Table 3]. The BIS value was then maintained between 40 and 60 throughout the surgical procedure except for the last 10 min of surgery where it was allowed to rise for the extubation of the patient. Involuntary movements were observed in five patients in group A while only in one patient in group B.
Table 3.
Changes in hemodynamic parameters and BIS values at different times in groups
DISCUSSION
We observed that titration of propofol for induction of anesthesia either by conventional clinical or BIS-guided evaluation is comparable in respect to the dosage, BIS values, and hemodynamic variables. A higher incidence of involuntary movements during induction occurred when dosage were titrated by clinical parameters.
A BIS range between 40 and 60 is recommended for surgical anesthesia. It allows for precise dosing of anesthetics, avoiding unnecessarily deep anesthesia as well as reducing the risk of awareness. Plasma concentration of propofol depends on factors such as age, gender, body weight, dose, infusion rate, and cardiac output.[3] It is generally assumed that the rate of equilibration between the plasma and effect site of drug is independent of rate of drug administration, several studies suggest that this may not be the case for intravenous anesthetics. A complex interaction of rate, dosage and duration of anesthetic exposure as well as physiological factors might influence the plasma effect site concentration.[4] Various infusion rates of propofol have been used by different authors[5–7] to achieve a therapeutic blood concentration of propofol. Target-controlled infusion provides a precise blood concentration of propofol, but due to its unavailability in our setup at the time of study, we used the infusion of propofol at the rate of 30 mk/kg/hr in lieu of the study of Wei-Dong.[6] Use of BIS was associated with a reduction in dosage of propofol for induction in our study though it was found to be statistically insignificant (1.79±0.41 mg/kg compared to 1.85±0.48 mg/kg) (P>0.05). This reduction in dosage was consistent with the findings of several investigators;[5,8] however the decrease in our study was less compared to the other studies. A reduction of 10-40% in dosage has been reported in literature though we found the difference of only about 3% overall. A decrease in dosage of 11% was observed in males with the use of BIS. The exact basis of such variation is not known though. Ethnicity of patients has been shown to have an influence.[9] The female patients in our study required a lower dose of propofol for induction compared to males whether clinically or BIS guided with comparable BIS values. Kodaka et al.[10] found that men required significantly more propofol than women at induction (2.9±0.2 v/s 2.7±0.1 mg/kg respectively) but there was no difference in the BIS value at loss of consciousness for men and women. Our study also showed that the decrease in dose of propofol in females compared to males and utilization of propofol for induction in both sexes were less compared to the study of Kodala et al. This difference may have been due to the following reasons: The subjects in the study of Kodala et al. were younger in age and had a mean weight much higher than our subjects. Ethnicity may have also played a role. Ward et al.[11] found that women had a smaller volume of distribution for propofol and a larger clearance resulting in a larger initial peak and smaller final concentration during similar continuous infusions. Our findings correlated with these studies. On comparing the mean dose of induction in males between the two groups, BIS monitoring was associated with the decrease in the mean dose of propofol (1.83±0.32 mg/kg in the BIS group compared to 2.06±0.45 mg/kg in the clinical group), a reduction of 11%. Paradoxically, in females the mean dose of propofol was found to be higher in the BIS-guided induction group i.e. 1.75±0.49 mg/kg in comparison to the clinically monitored group where the mean dose of propofol was 1.65±0.44 mg/kg. Similar findings were seen in the studies of Kodaka et al. and Wilhelm et al.[10,12]
A paradoxical response between BIS value and total dose of propofol induction were observed in two cases. In the first case, a female patient weighing 51 kg had a sudden decrease of BIS value to 33 when only 30 mg (0.6 mg/kg) propofol was administered. In the second patient, again a female patient weighing 52 kg had no response to verbal command even though the dose of propofol administered was only 40 mg. The BIS value however in both cases was 63. Similar findings were also observed by Rudner in patients where he found that after 2 min of propofol administration at 1.26 mg/kg, the BIS value came down to 4 and an isoelectric EEG was observed. He opinioned that there is a wide variability in response of patient to propofol and continuous monitoring of cortical electrical activity is required to observe such changes.[13]
A comparison of BIS changes at different time of observations showed insignificant changes in BIS after induction; a significant increase in the BIS value was observed after intubation in both Groups. Studies by Dong et al. showed that BIS value increases significantly after tracheal intubation.[6] Use of opioids such as remifentanil has shown blunt increases in BIS after laryngoscopy and tracheal intubation in a dose-related fashion[14] under constant propofol infusion. Singh et al. found that the hypnotic interaction between propofol and fentanyl at 1-3 μg/kg during propofol i.v. anesthesia does not significantly lower the BIS and 95% SEF values. Higher doses of fentanyl have significant interaction with propofol and results in lowering the BIS and 95% SEF values.[7] The dose of fentanyl used by us in our study was only 2 μg/kg and this may have resulted in an increase in the value of post intubation BIS. Frakes et al.[15] found that at moderate doses of 2.5 to 3 μg/kg, fentanyl blocks roughly half of the sympathetic response. To effectively minimize the reflex sympathetic response to laryngoscopy, fentanyl doses of 5 μg/kg is needed but this increases the risk of adverse effects.
Choice of neuromuscular blocking agent has been implicated for changes in BIS. Use of depolarizing muscle relaxants has shown to decrease BIS, while use of non-depolarizing agents does not affect BIS.[16,17] So to prevent such interactions we have utilized vecuronium for facilitating intubation.
BIS have been found to be influenced by the addition of inhalational agents such as sevoflurane.[18] Use of nitrous oxide however has not been associated with any changes in BIS up to the concentration of 70%.[19,20] Considering these facts after induction of anesthesia we ventilated our patients with N2 O/O2 and did not use inhalational anesthetics until after the patient was intubated.
Involuntary movements were seen in six patients (two males and three females) in group A and in one female patient in group B. The females and group A patients had higher incidence of involuntary movements. During involuntary movements there were no changes in the BIS values. It has been established that the excitatory effects of propofol are sub-cortical in origin and are not associated with EEG activity. They may include occasional involuntary movements, myoclonus, dystonic posturing, and opisthotonos. Involuntary movements not related to light plane of anesthesia were seen in propofol induction (23.1%) compared to 3.9% in thiopentone induction in a study by Boey et al.[21]
A limitation of our study is that we have compared the younger age group with the range of age being 34±10 years. A wider range of age would have given an idea of influence of age of the patient on the dosage of propofol.
A number of studies have cited the influence of increasing age of patient to decrease in the induction dosage of propofol.[22,23] These patients are also prone for hemodynamic variations in the perioperative period as a result of co morbid conditions which have been demonstrated with higher mortality in the post-operative period.[24,25]
In conclusion, there is no significant difference in the induction dose of propofol when assessed clinically (loss of verbal response) or by BIS monitoring. Female patients require lesser dose of propofol than male patients. The changes in BIS value and hemodynamic parameters are similar in both the groups. So, we conclude that traditional titration of the adequate dose of propofol and depth of anesthesia during intubation by loss of verbal response is as good as BIS value monitoring. Dose requirement of propofol was also not reduced significantly in BIS monitored group. Considering the cost and monetary burden on the patient in our set up, routine use of BIS for titrating the dosage of propofol is not justified. It can be used as a tool of monitoring depth of anesthesia, record keeping, research, and medico legal purposes.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Bruhn J, Myles PS, Sneyd R, Struys MM. Depth of anaesthesia monitoring: What's available, what's validated and what's next? Br J Anaesth. 2006;97:85–94. doi: 10.1093/bja/ael120. [DOI] [PubMed] [Google Scholar]
- 2.Donald RS, Steven LS. In: Miller's anesthesia. 6th ed. Miller RD, editor. Philadelphia: Elseiver Churchill Livingstone; 2005. pp. 1250–7. [Google Scholar]
- 3.Adachi YU, Wantanabe K, Higuchi H, Satoh S. The determinants of propofol induction of anesthesia dose. Anesth Analg. 2001;92:656–61. doi: 10.1097/00000539-200103000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Ludbrook GL, Visco E, Lam AM. Propofol: Relation between brain concentrations, electroencephalogram, middle cerebral artery blood flow velocity and cerebral oxygen extraction during induction of anesthesia. Anesthesiology. 2002;97:1363–70. doi: 10.1097/00000542-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Gurses E, Sungurtekin H, Tomatir E, Dogan H. Assessing propofol induction of anesthesia dose using bispectral index analysis. Anesth Analg. 2004;98:128–31. doi: 10.1213/01.ANE.0000090314.43496.1D. [DOI] [PubMed] [Google Scholar]
- 6.Dong W, Sakai T, Takahashi S, Matsuki A. Haemodynamic and electroencephalograph responses to intubation during induction with propofol or propofol/fentanyl. Can J Anaesth. 1998;45:19–22. doi: 10.1007/BF03011986. [DOI] [PubMed] [Google Scholar]
- 7.Singh H, Sakai T, Matsuki A. Movement response to skin incision: Analgesia vs. bispectral index and 95% spectral edge frequency. Eur J Anaesth. 1999;16:610–4. doi: 10.1046/j.1365-2346.1999.00549.x. [DOI] [PubMed] [Google Scholar]
- 8.Luginbuhl M, wuthrich S, Felix SP, Zbinden AM, schinder TW. Different benefits of bispectral index in desflurane and propofol anesthesia. Acta Anaesthesiol Scand. 2003;47:165–73. doi: 10.1034/j.1399-6576.2003.00041.x. [DOI] [PubMed] [Google Scholar]
- 9.Natarajan A, Stravdvik GF, Pattanayak R, Chakithandy S, Lewis CM, Morley AP. Effect of ethnicity on hypnotic and cardiovascular characteristic of propofol induction. Aaesthesia. 2011;66:15–9. doi: 10.1111/j.1365-2044.2010.06568.x. [DOI] [PubMed] [Google Scholar]
- 10.Kodaka M, Johansen JW, Sebel PS. the influence of gender on loss of consciousness with sevoflurane or propofol. Anesth Analg. 2005;101:377–81. doi: 10.1213/01.ANE.0000154534.71371.4F. [DOI] [PubMed] [Google Scholar]
- 11.Ward DS, Norton JR, Guivare PH. Pharmacodynamics and pharmacokinetics of propofol in a medium chain triglyceride emulsion. Anesthesiology. 2002;97:1401–8. doi: 10.1097/00000542-200212000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Wilhelm W, Buchinger H, Bielder A, Altmann S, Kreuer R. Influence of gender on propofol consumption and recovery times. Anaesthetist. 2005;54:567–74. doi: 10.1007/s00101-005-0836-z. [DOI] [PubMed] [Google Scholar]
- 13.Rudner R, Jalowiecki P, Hagihira S. Abnormally low bispectral index and isoelectric electroencephalogram observed after administration of small doses of propofol during induction of anesthesia. J Anesth. 2005;19:339–42. doi: 10.1007/s00540-005-0346-9. [DOI] [PubMed] [Google Scholar]
- 14.Dahaba AA, Lisching U, Kronthaler R, Bornemann H, Georgiev V, Rehak PH, et al. Bispectral index guided v/s clinically guided remifentanil/propofol analgesia/sedation for interventional radiological procedures: An observer blinded randomized study. Anesth Analg. 2006;103:378–84. doi: 10.1213/01.ane.0000223681.77120.ca. [DOI] [PubMed] [Google Scholar]
- 15.Frakes MA. Rapid sequence induction medications: An update. J Emerg Nurs. 2003;29:533–40. doi: 10.1016/j.jen.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 16.Dahaba AA, Mattweber M, Fuchs A, Zenz W, Rehak PH, List WF, et al. The effect of different stages of neuromuscular block on the bispectral index and the bispectral index-XP under remifentanil/propofol anesthesia. Anesth Analg. 2004;99:781–7. doi: 10.1213/01.ANE.0000132997.19872.BC. [DOI] [PubMed] [Google Scholar]
- 17.Greif R, Greenwald S, Schweitzer E. Muscle relaxation does not alter hypnotic level during propofol anesthesia. Anesth Analg. 2002;94:604–8. doi: 10.1097/00000539-200203000-00023. [DOI] [PubMed] [Google Scholar]
- 18.Rinaldi S, Consales G, DeGaudio AR. State entropy and Bispectral index: Correlation with end tidal sevoflurane concentrations. Minerva Anestesiol. 2007;73:39–48. [PubMed] [Google Scholar]
- 19.Rampil IJ, Kim JS, Lenhardt R. Bispectral EEG index during nitrous oxide administration. Anesthesiology. 1998;89:671–7. doi: 10.1097/00000542-199809000-00017. [DOI] [PubMed] [Google Scholar]
- 20.Coste C, Guignard B, Menigaux C, Chauvin M. Nitrous oxide prevents movement during orotracheal intubation without affecting BIS value. Anesth Analg. 2000;91:130–5. doi: 10.1097/00000539-200007000-00024. [DOI] [PubMed] [Google Scholar]
- 21.Boey WK, Kumar A. Comparison of propofol and thiopentone as induction agents for laparoscopy. Singapore MED J. 1991;32:150–3. [PubMed] [Google Scholar]
- 22.Katoh T, Bito H, Sato S. Influence of age on hypnotic requirement, Bispectral index and 95% spectral edge frequency with sedation induced by sevoflurane. Anesthesiology. 2000;92:55–61. doi: 10.1097/00000542-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Renna M, Venturi R. Bispectral index and anaesthesia in elderly. Minerva Anestesiol. 2000;66:398–402. [PubMed] [Google Scholar]
- 24.Kalkman CJ, Peelen LM, Moons KG. Depth of anesthesia and long term mortality. Anesthesiology. 2011;114:485–7. doi: 10.1097/ALN.0b013e31820c2ba2. [DOI] [PubMed] [Google Scholar]
- 25.Kertai MD, Palanca BJ, Pal N, Burnside BA, Zhang L, Sadiq F, et al. Bispectral index monitoring, duration of Bispectral index below45, patient risk factors and intermittent term mortality after non cardiac surgery in B unaware trial. Anesthesiology. 2011;114:545–56. doi: 10.1097/ALN.0b013e31820c2b57. [DOI] [PubMed] [Google Scholar]


