Abstract
Background:
Psychiatric problems in children are rising and reported cases represent only the tip of the iceberg; large number remains unreported in India. There is limited data on childhood mental disorders and mental health needs in Northern-India.
Aims and Objective:
The main objective of this research was to study the extent and nature of psychiatric disorders in school children in a defined geographical area and to study their psychosocial correlates.
Materials and Methods:
In this cross sectional study, Childhood Psychopathology Measurement Schedule (CPMS) was used to measure the magnitude of 982 students in the age group of 10-15 years from four randomly selected schools in a city of North India. Screening stage was followed by detailed evaluation stage in which children were diagnosed by ICD-10 criteria. Statistical analysis was done by percentage and Chi-square test.
Results:
The results showed that among 982 students, 199 (20.2%) had psychiatric morbidity. Most of them were in the age group of 13-14 yrs, from middle income group and were second in birth order. No significant sexual preference was found regarding distribution of the disorders. Specific phobia; other non organic sleep disorders like sleep talking, bruxism; tension headache found to be the most prevalent disorders followed by sleep terror, hyperkinetic disorder, pica, enuresis.
Conclusion:
Epidemiological studies should be started early in childhood and carried longitudinally for development of preventive, promotional and curative programme in the community.
Keywords: Prevalence, child psychopathology, mental illness, schoolchildren
INTRODUCTION
Research on child psychopathology has been traditionally treated like a step child. Despite clinical emphasis on the childhood roots of adult disorders, psychopathology has been studied more intensively in adults. One of the greatest handicaps to research and communication on child psychopathology has been the lack of standardised objectives and reliable way of describing and classifying behavioural disorders.[1]
Children under 16 years of age constitute over 40 percent of India's population and information about their mental health needs is a national imperative. Till date, Indian studies reported prevalence rates of psychiatric disorders among children ranging from 2.6 to 35.6 percent.[2–6] small group of community-based studies provided some benchmarks for the rates of psychiatric disturbance among Indian children.
The term psychopathology in children covers various psychological problems such as behavioural problems, low intelligence, anxiety, conduct disorders, psychotic symptoms, and physical illness with emotional problems and somatic disorders. Thus clinically significant psychopathology can be defined as a disorder in one or more of the following areas i.e. overt behaviour, emotional states, interpersonal relationships and cognitive functions. The abnormality must be of sufficient duration and severity to cause functional impairment.
Mental health of a child is greatly influenced by many environmental factors and life events such as adverse family circumstances, maternal separation or deprivation, birth of a sibling, parental divorce, bereavement, physical handicap, urbanism and maternal depression. In a particular socio-cultural context these events assume etiological significance.
Kim-Cohen et al in their follow back study from New Zealand reported that 50% of adult psychiatric disorder cases had onset by age of 15 years.[7] Costello alin their updated review of epidemiology of childhood psychiatric disorders have opined that onset before adulthood may be a characteristic of the majority of adult psychiatric disorders.[8] Early intervention for these has the potential to substantially alter the developmental course of these adult disorders, significantly reducing the morbidity.
Psychiatric problems in children in India are rising and reported-cases represent only the tip of the iceberg, large number remains unreported. There is a need to conduct a large scale survey of childhood psychiatric disorders in India to see the nature and extent of prevailing morbidity to trace its developmental course and study its psychosocial determinants which are known to contribute to psychiatric disorders. Studies of psychiatric disorders in children would give us baseline data for mental health planning for children, identify children at risk, generate hypothesis for aetiology and suggest strategies for preventive intervention. The present study focuses on the findings related to the prevalence of psychiatric morbidity at different schools in a city of North India.
MATERIALS AND METHOD
The study was carried out at four randomly selected boys’ and girls’ schools during the month of July-August 2010 in a city of North India. Children in the age group of 10-15 years were included which covered classes from fifth to ninth standard. The total no of children in these four schools were 3928. Every fourth student was included for the study purpose. The tools used in this study were Childhood Psychopathology Measurement Schedule (CPMS) developed and standardized by Malhotra et al,[9] and another schedule consisting of questions pertaining to socio-demographic data of the children which was prepared separately and pre-tested before final administration. CPMS contained 74 questions pertaining to 8 factors i.e. intelligence with behaviour problems, conduct disorders, anxiety, depression, psychotic symptoms, special symptoms, physical illness emotional problems and somatisation. Each question was directed to the mother regarding the child's behaviour during past one year. These answers were scored on two-point scale i.e., ‘0’ if that particular behaviour is not present and ‘1’, if present. Those children who scored 10 or more on this score were considered positive for psychopathological disorders. All the children were clinically examined and anthropometric measurements were recorded. Using this cut-off score, the sensitivity and specificity for detecting probable psychopathological disorders reported by authors was 82% and 87% respectively. After taking permission of respective principals and parents of the children, personal data sheets were distributed separately for each school on separate days. After collecting the data sheet, CPMS was distributed to the same children. After completion of CPMS by parents of the children, these were collected back and analysed. The children who scored more than 10 were assessed further and interviewed clinically and were diagnosed according to International Classification of Diseases-10 (ICD-10) criteria. Data was tabulated and Chi-Square test was used for statistical analysis. P value less than 0.05 was considered significant.
RESULTS
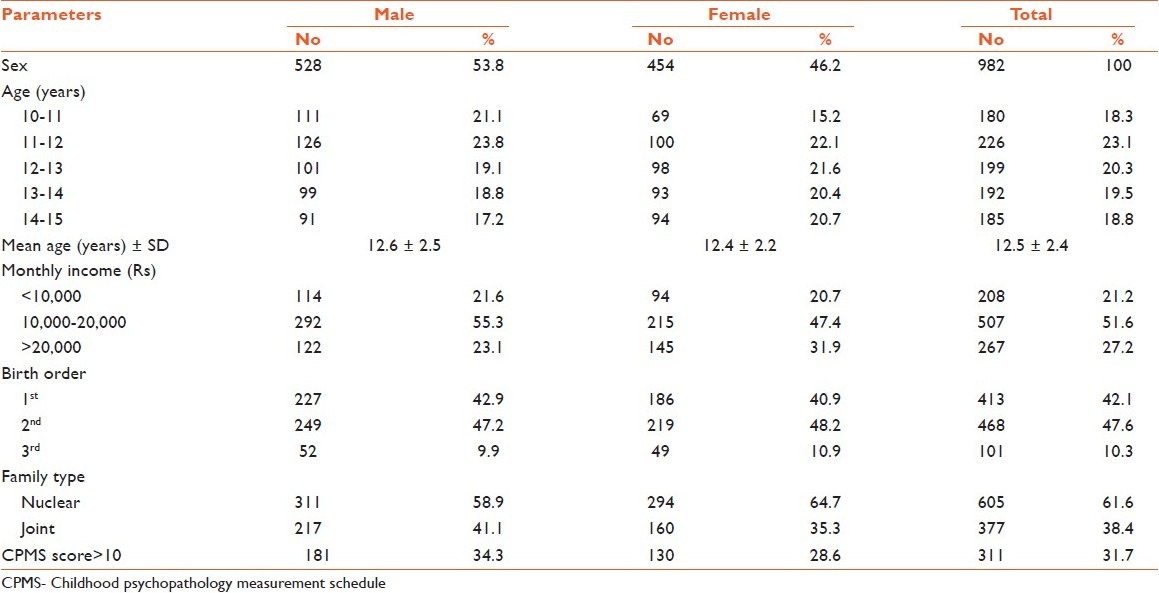
In the present study among 982 children, 528 (53.8%) were males and 454 (46.2%) were females. Mean age of the students was 12.5±2.4 years. Most of the children were from the income group of 10000-20000 INR/month, which was higher among the male students. Among 982 students, 181 students (31.7%) scored >10 in CPMS score. There was no significant difference between male and female groups regarding CPMS score [Table 1].
Table 1.
Socio-demographic characteristics and childhood psychopathology measurement schedule score
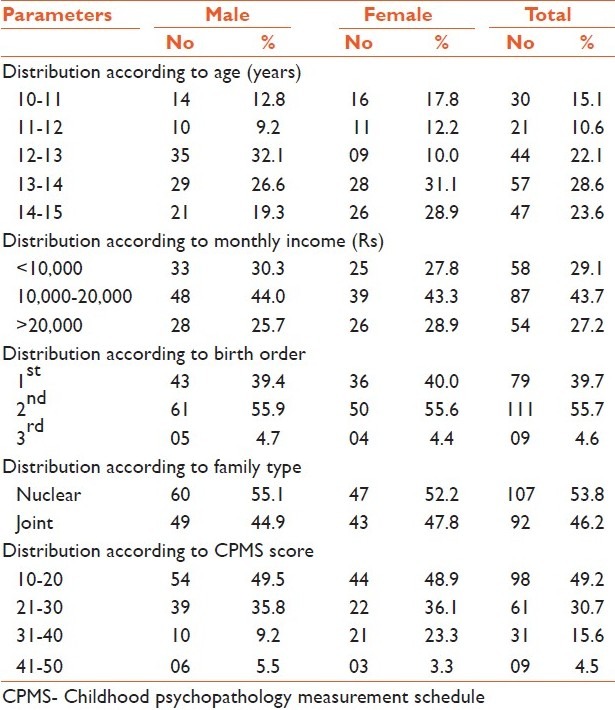
After screening 311 students, 199 students (20.2%) found to have psychiatric illness according to ICD-10 criteria. It was observed that most of the students (57 students, 28.6%) having psychiatric illness were in the age group of 13-14 years followed by 23.6% in age group of 14-15 years and 22.1% in the age of 12-13 years. There was no significant sexual preference. Children having psychiatric illness mostly (87 students, 43.7%) were from the income group 10,000-20,000 INR which was significantly higher (P<0.001) than the other two economical groups. Psychiatric disorders were seen prevalent in the children having second birth order (111 students, 55.7%) which was significantly higher (P<0.001) than two other groups. No significant difference was found among children from nuclear & joint family. The table also shows that significantly higher (P<0.001) number of students (98 students, 49.2%) were in the score of 10-20 in the CPMS scale [Table 2].
Table 2.
Socio-demographic variable wise distribution of children having psychiatric disorder
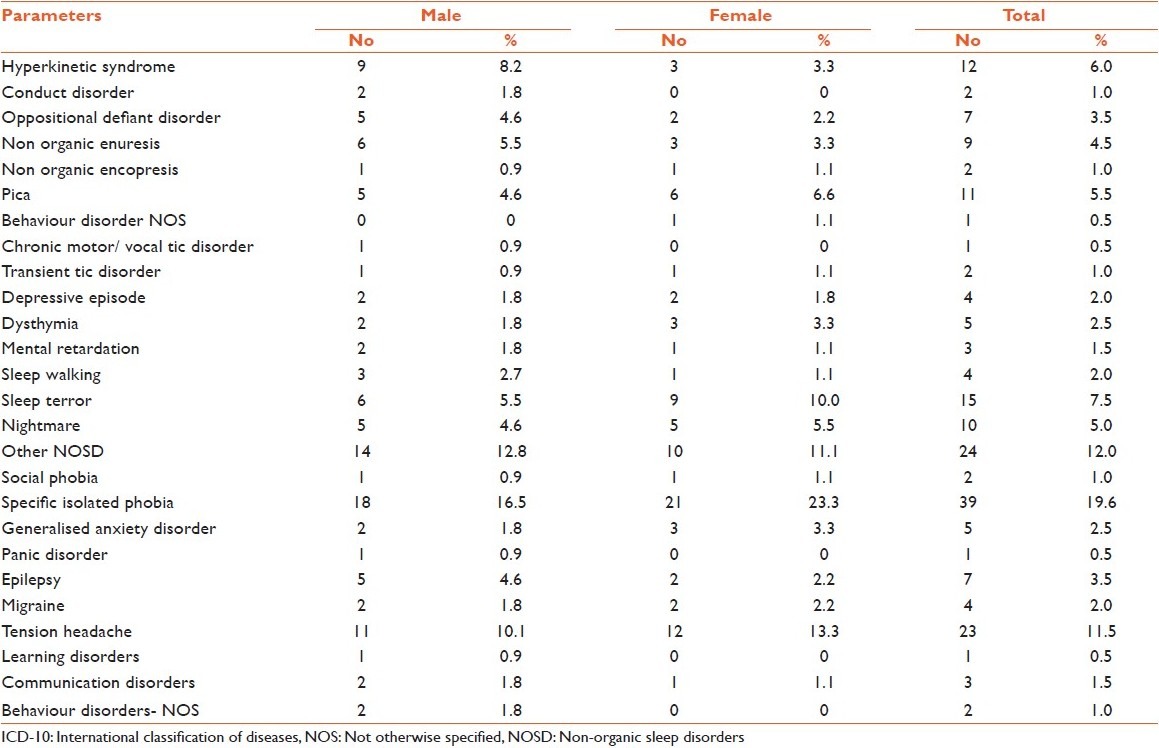
Most of the children (39 students) were having specific isolated phobia (19.6%), other non organic sleep disorders like sleep talking, bruxism etc (24 students, 12.0%) and tension headache (23 students, 11.5%). Hyperkinetic disorder found in 12 students (6%), pica in 11 students (5.5%), enuresis in 9 students (4.5%), sleep terror in 15 students (7.5%), and epilepsy in 7 (3.5%) of the students. No significant difference was found among male and female students [Table 3].
Table 3.
Prevalence of specific disorder according to ICD-10 criteria
DISCUSSION
In the present study 311 (31.7%) students had CPMS score >10 whereas Rahi et al,[10] in 2005 showed 16.5% of children being CPMS positive. study conducted by WHO in four developing countries (1981) including India in the state Haryana, showed prevalence of 21%.[11] A study by Indian Council of Medical Research (ICMR) in 2001 showed prevalence to be 13.4% in the age group 0-16 years.[12] study have revealed the prevalence rates to be 12.5% in 0-16 yrs community based sample from Bangalore,[13] 9.4% in 8-12 yrs olds from a community sample in Kerala,[5] and 6.3% in 4-11 yrs old school children in Chandigarh.[14]
Overall rates of childhood and adolescent mental disorders in India and other middle and low income countries range between 6%-15% which are on the lower side as compared to reported rates from certain western countries such as Canada (18.1%),[15] Germany (20.7%),[16] (22.5%),[17] and USA (21%).[18] In our study prevalence of psychiatric disorder is 20.2% which corroborates with the findings of WHO study in India,[11] (21%) and by other studies too.[16–18]
Out of 199 students, children of the age group of 13-14 year and 14-15 year had more number of ill children as compared to younger age group. There may be number of factors operative for this phenomenon like increasing burden of studies in higher classes, emotional disturbances related to early adolescence, or mothers’ perception of any resultant undesired change in behaviour as abnormal. In the study of Rahi et al,[10] psychopathology was found more commonly in the age group of 7-10 years.
Most of the studies have shown a male preponderance for psychiatric disorders,[12,19,20] but the present study didn’t show any significant difference among male and female students.
Prevalence was significantly higher (P<0.001) in the middle income group (10000-20000INR) while in most of the studies the prevalence increased as the socio-economic status lowered, the highest in lower class.[2,6,21,22]
Distribution of family structure was of no significance as illness was equally distributed in both nuclear and joint family. It corroborates with the findings of Lal et al,[6] and Deivasigamini,[2] whereas Verghese et al,[20] more cases in nuclear families. Majority of the children with illness came from second birth order. Lack of awareness about child rearing practices, over protection of first child, neglect of second child, sibling rivalry, unwanted child, economic burden after second child could contribute to this finding. Other studies like studies by Offord,[15] and Rahi et al,[10] showed majority of the ill children were first born.
Among different disorders, most of the children were having specific isolated phobia (19.6%), other non organic sleep disorders like sleep talking, bruxism etc (12.0%) and tension headache (11.5%). Deivasinagamini,[2] found prevalent psychiatric disorders to be conduct disorder (14.3%), enuresis (14.3%), mental retardation (2.9%) and hyperkinetic disorder (1.7%). In our study hyperkinetic disorder found in 6% of the students, enuresis in 4.5% and mental retardation in 1.5% of the students. In another study in 4-16 yr age group children by Srinath et al,[13] was preceded by enuresis (6.2%) followed by specific phobia (2.9%) and hyperkinetic disorder (1.6%) and stuttering (1.5%).
In view of the above discussion, it is concluded that it is imperative to carry out this type of epidemiological survey more in number and to follow up them longitudinally to understand the natural history of childhood and adolescent disorders. The results of the study have implications for clinical training, practice and policy initiatives. Integrating mental health into general health care, effective mass media coverage, networking between mental health-professionals and other health professionals, community-based health services and involvement of professionals from the education sector, would be essential.
LIMITATIONS
The study has been done in a small number of children where male children are significantly higher in number than female. Cross sectional study should be followed by longitudinal study to find out the course and pattern of their disorder. Moreover, other socio-demographic entities should be searched for and compared to find out any possible correlation.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Thomas A, Chess S, editors. Temperament and development. New York: Brunner/Mazel; 1977. [Google Scholar]
- 2.Deivasigamini TR. Psychiatric morbidity in primary school children- an epidemiological study. Indian J Psych. 1990;32:235–40. [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmed A, Najam K, Khan Z, Ali A. Prevalence of psychosocial problems among school going male adolescents. Indian J Community Med. 2007;32:219–21. [Google Scholar]
- 4.Anita, Gaur DR, Vohra AK, Subash S, Khurana H. Prevalence of Psychiatric morbidity among 6 to 14 year old children. Indian J Community med. 2003;28:133–7. [Google Scholar]
- 5.Hackett R, Hackett L, Bakta P, Gowers S. The prevalence and association of psychiatric disorder in children in Kerala, South India. J Child Psychol Psychiatry. 1999;40:801–7. [PubMed] [Google Scholar]
- 6.Lal N, Sethi BB. Estimate of mental ill health in children in an urban community. Indian J Paediat. 1977;44:55–64. doi: 10.1007/BF02753627. [DOI] [PubMed] [Google Scholar]
- 7.Kim-Cohen J, Caspi A, Moffitt T, Harrington H, Milne B, Poulton R. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. 2003;60:709–17. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- 8.Costello EJ, Foley DL, Angold A. Tenyr research update review: The epidemiology of child and adolescent psychiatric disorders II, Developmental epidemiology. J Am Acad Child Adolesc Psychiatry. 2006;45:8–25. doi: 10.1097/01.chi.0000184929.41423.c0. [DOI] [PubMed] [Google Scholar]
- 9.Malhotra S, Varma VK, Verma SK, Malhotra A. Childhood Psychopathology Measurement Schedule: Development and Standardization. Indian J Psych. 1988;30:325–31. [PMC free article] [PubMed] [Google Scholar]
- 10.Rahi M, Kumavat AP, Garg S, Singh M. Socio-demographic correlates of psychiatric disorders. Indian J Pediatr. 2005;72:395–8. doi: 10.1007/BF02731734. [DOI] [PubMed] [Google Scholar]
- 11.Giel R, Arango MV, Climent CE. Childhood Mental disorders in primary health care: results of observations in four developing countries. Pediatrics. 1981;68:677–83. [PubMed] [Google Scholar]
- 12.Indian Council of Medical Research. Epidemiological study of child and adolescent psychiatric disorders in urban and ruralareas. ICMR Bull. 2001;31:54–5. [Google Scholar]
- 13.Srinath S, Girimaji SC, Gururaj G, Seshadri S, Subbakrishna DK, Bhola P, et al. Epidemiological study of child and adolescent psychiatric disorders in urban and rural areas of Bangalore, India. Indian J Med Res. 2005;122:67–79. [PubMed] [Google Scholar]
- 14.Malhotra S, Kohli A, Arun P. Prevalence of psychiatric disorders in school children in India. Indian J Med Res. 2002;116:21–8. [PubMed] [Google Scholar]
- 15.Offord DR. Ontario Child Health Study: II, Six month prevalence disorder and rates of service utilization. Arch Gen Psychiatry. 1987;44:832–6. doi: 10.1001/archpsyc.1987.01800210084013. [DOI] [PubMed] [Google Scholar]
- 16.Weyerer S, Castell R, Biener A, Artner K, Dilling H. Prevalence and treatment of psychiatric disorders in 3 to 14 year old children: Results of a representative field study in the small rural town region of Traunstein, Upper Bavaria. Acta Psychiatry Scand. 1988;77:290–6. doi: 10.1111/j.1600-0447.1988.tb05123.x. [DOI] [PubMed] [Google Scholar]
- 17.Steinhausen HC, Metzke CW, Meier M, Kannenberg R. Prevalence of child and adolescent disorders: The Zurich Epidemiological Study. ActaPsychiatrScand. 1998;98:262–71. doi: 10.1111/j.1600-0447.1998.tb10082.x. [DOI] [PubMed] [Google Scholar]
- 18.United States Department of Health and Human Services. Mental Health: A Report of the Surgeon General. Rockville, MD, United States Department of health and Human Services, Substance Abuse and Mental Health Service Administration, Centre for Mental Health Services, National Institutes of Health, National Institute of Mental Health. 1999 [Google Scholar]
- 19.Banerjee T. Psychiatric morbidity among rural primary school children in West Bengal. Indian J Psych. 1997;39:130–5. [PMC free article] [PubMed] [Google Scholar]
- 20.Verghese A, Beig A. Psychiatric disturbance in children – an epidemiological study. Indian J Med Res. 1974;62:1538–42. [PubMed] [Google Scholar]
- 21.Chadda RK. Psychiatric morbidity in primary school children- a clinic based study. Indian J Pediatr. 1995;62:77–81. doi: 10.1007/BF02752189. [DOI] [PubMed] [Google Scholar]
- 22.Shenoy J, Kapur M. Prevalence of scholastic backwardness among five to eight-year old children. Indian J Psych. 1996;38:201–7. [PMC free article] [PubMed] [Google Scholar]


