Abstract
Primary lumbar hernias are rarest form of hernias as compared to other ventral abdominal wall hernias. Only scattered reports of hernias of both superior and inferior lumbar triangles have appeared in both the English and foreign literature. There are only about 300 cases of primary lumbar hernia being reported. Being a rare entity, it had always posed diagnostic and treatment dilemma to the surgeons. The diagnosis requires imaging studies in such cases. Treatment of lumbar hernia is always surgical and requires prosthetic reinforcement for the best result. We are reporting here a case of primary lumbar hernia of the superior lumbar triangle with a successful repair with a sheet of polypropylene mesh. In our case, acquired primary lumbar hernia was emerging from superior lumbar triangle, associated with congenital right scoliosis, which is a rare occurrence.
Keywords: Extraperitoneal meshplasty, lumbar triangles, primary lumbar hernia
INTRODUCTION
Lumbar hernias are very uncommon entity, constituting less than 1.5% of all the abdominal wall hernias. It can be either congenital (20%) or acquired (80%) and occur in lumbar region of the posterior abdominal wall. About 25% of lumbar hernias have a traumatic or post-surgical etiology,[1] Presenting a challenge for surgical management. De Garangeot reported the first known case of lumbar hernia in 1731, the hernia being reduced at autopsy. In 1783, Petit reported a case of strangulated lumbar hernia coming through the inferior lumbar triangle, which is now named after him. A strangulated lumbar hernia was successfully operated and treated by Ravaton in 1750. Almost 100 years later, Grynfeltt reported a case of hernia emerging through the superior lumbar triangle which was distinctly separate from the inferior lumbar triangle. Lesshaft in 1870 confirmed the existence of superior lumbar triangle separately, distinguishing it from inferior lumbar triangle and reported a similar case. Primary lumbar hernias are very rare and commonly occur through the inferior lumbar triangle of Petit. Till date, about 300 cases of primary lumbar hernias have been reported in literature.[2] Secondary lumbar hernias commonly occur through superior lumbar triangle of Grynfeltt–Lesshaft, mainly following renal operations or direct trauma to the lumbar region.
CASE REPORT
An 86-year-old female presented with a swelling over the back in left lateral aspect since 5 years, which was initially small in size, reducible, painless, and gradually increased. The swelling had become irreducible and associated with pain since last 2 months. There was no other significant history in the form of trauma, previous surgery, and chronic infections like tuberculosis or altered bowel habits. On examination at admission, there was 15 × 12 × 10 cm, non-tender, non-pulsatile, irreducible swelling, soft in consistency in the left lumbar region with an expansile cough impulse. There was congenital right scoliosis [Figure 1].
Figure 1.

Left lumbar swelling with right side scoliosis of spine
Examination of right flank, rest of the abdomen and other hernial orifices was normal. Plain radiograph of the abdomen revealed a gas shadow within the swelling. Ultrasonography revealed well-defined, elongated and rounded mixed echogenic masses of about 3.7 × 2.2 × 1.4 cm and about 2 cm diameter in the left lumbar region, which appeared most probably to be herniated bowel loops. Computed tomography (CT) scan of the abdomen revealed 3 cm defect in the left lumbar region at the level of L3 vertebra, with a hernial sac containing large bowel loops, confirming the presence of left lumbar hernia containing large bowel. A diagnosis of irreducible left lumbar hernia was made and the patient was taken up for the surgery after she was examined for anesthetic fitness. The patient was placed in the right lateral decubitus position and the operating table was angulated to achieve the same effect as a kidney rest. The left flank incision was given over the swelling for exploration. The sac was herniating through the superior lumbar triangle and was covered by the muscles forming the boundaries of the triangle [Figure 2]. There were dense adhesions around the sac which had made it irreducible. There were no features of strangulations.
Figure 2.

Large bowel herniating through the superior lumbar triangle
The dense adhesions were released meticulously and the sac was reduced completely and intact. A sheet of polypropylene mesh was fashioned as inlay prosthesis and was placed in the extraperitoneal space by umbrella placement technique through the defect in the muscle layer [Figures 3 and 4]. The defect was repaired with prolene continuous suturing and the rest of the posterior abdominal wall was closed in layers.
Figure 3.
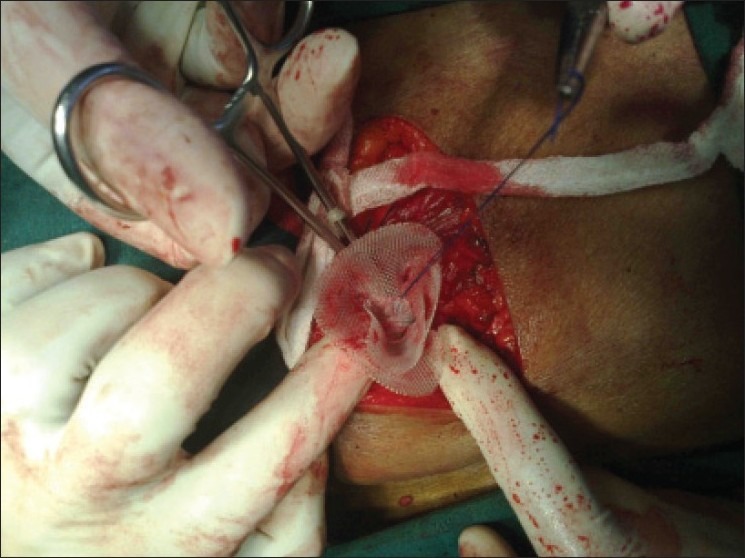
Umbrella technique for placement of mesh
Figure 4.
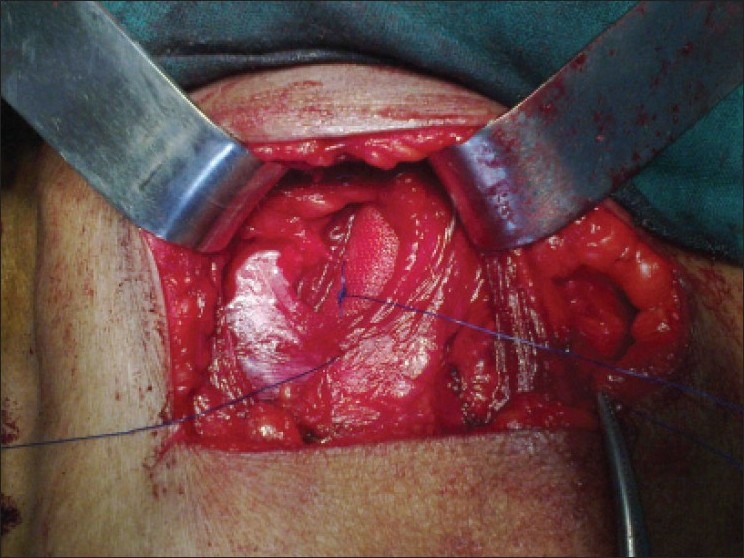
Extraperitoneal in lay meshplasty
The immediate postoperative period was uneventful. Oral sips were started after 4 hours of operation. The patient was discharged after removal of sutures on 10th postoperative day, with a healed scar. On follow-up visit after 2 weeks, the patient was absolutely asymptomatic with a well-healed operation scar.
DISCUSSION
All congenital hernias reported have been through the inferior lumbar triangle. Acquired traumatic lumbar hernias are probably more frequent in the superior lumbar triangle because of operations performed in this area,[1] and also because it is the thinnest point in the lateral and posterior abdominal wall. This hernia results from direct trauma, penetrating wound, abscess, or flank incision.[3] Removal of bone from the iliac crest for autogenous bone grafting may lead to massive lumbar incisional hernias. Secondary acquired hernia constitutes about 25%, whereas primary or spontaneous acquired hernias constitute about 55% of all reported cases. Old age, emaciation, degenerative changes and debilitating disease may be contributing factors, along with loss of fat which normally pads the neurovascular orifices, facilitating the rupture.
Lumbar hernias occur more commonly in males as compared to females and are twice as common on the left side as compared to the right side.[1] Patient presents with hernia usually between fifth and eighth decades of life. Patients are generally asymptomatic. They may at times complain of backache, pain over the swelling or dragging sensation. These swellings are initially small in size and gradually increase and may assume large proportions.[4] They are also generally reducible swellings. The hernial sac may contain retroperitoneal fat, kidney, colon or less commonly small bowel, omentum, ovary, spleen or appendix.[3] It is difficult to make diagnosis in obese patients.
CT scan of abdomen should be the investigation of choice if a suspicion of lumbar hernia is present.[5] All lumbar hernias should be surgically treated to avoid complications like incarceration (25% cases) or strangulation (although rare because of wide hernia neck).[6] The aim of the surgery should be to reduce the sac, repair the defect and to strengthen the posterior abdominal wall to withstand the raised intra-abdominal pressure due to daily physical activity. It includes simple anatomical closure, overlapping of the aponeurosis, use of musculofascial flaps, prosthetic meshes and laparoscopic mesh repair in case of uncomplicated lumbar hernias.
Currently, evidence-based studies suggest the lumbar hernia repair is best done by placement of extraperitoneal prosthetic mesh,[7] which can be sutured to the margins of hernia. Extraperitoneal position of the mesh is advantageous as no bony anchorage is essential. Umbrella technique of mesh placement helps in proper placement of mesh covering the defect completely and reduces the chances of injury to structures beneath it. Laparoscopic[8,9] transabdominal preperitoneal mesh repair for lumbar hernia is a tensionless repair.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Sharma P. Lumbar hernia. Med J Armed Force India. 2009;65:178–9. doi: 10.1016/S0377-1237(09)80140-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Russell RC, Norman S. Bailey and Love's Short Practice of Surgery. 25th ed. London: Edward Arnold; 2007. p. 983. [Google Scholar]
- 3.Nyhus LM, Harkins HN. Hernia. Philadelphia: J. B. Lippincott Co; 1964. [Google Scholar]
- 4.Geis WP, Hodakowski GT. Lumbar hernia. In: Nyhus L, Condon R, editors. Hernia. 5th edition. Philadelphia: 2001. pp. 425–7. [Google Scholar]
- 5.Baker ME, Weinerth JL, Andriani RT. Lumbar hernia: Diagnosis by CT. AJR Am J Roentgenol. 1987;148:565–7. doi: 10.2214/ajr.148.3.565. [DOI] [PubMed] [Google Scholar]
- 6.Leber GE, Garb JL, Albert Al. Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg. 1998;132:1141–4. doi: 10.1001/archsurg.133.4.378. [DOI] [PubMed] [Google Scholar]
- 7.Meinke AK. Totally extraperitoneal laparoendoscopic repair of lumbar hernia. Surg Endosc. 2003;17:734–7. doi: 10.1007/s00464-002-8557-8. [DOI] [PubMed] [Google Scholar]
- 8.Heniford BT, Iannitti DA, Gagner M. Laparoscopic inferior and superior lumbar hernia repair. Arch Surg. 1997;132:1141–4. doi: 10.1001/archsurg.1997.01430340095017. [DOI] [PubMed] [Google Scholar]
- 9.Chowbey PK, Sharma A, Khullar R. Laparoscopic Ventral hernia repair. J Laparoendosc Adv Surg Tech. 2000;10:79–84. doi: 10.1089/lap.2000.10.79. [DOI] [PubMed] [Google Scholar]


