Abstract
Background:
Male infertility is a serious problem all over the world. Nutritional deficiency of trace element Zinc (Zn) may play a role in male infertility as Zn plays an important role not only in normal testicular development, but also in spermatogenesis and sperm motility. Deficiency of Zn is associated with hypogonadism and insufficient development of secondary sex characteristics.
Objective:
The present study was designed to analyze the level of seminal Zn among different groups of infertile patients and to correlate it with sperm concentration, active, sluggish and immotile fractions of seminal parameters, with an objective to establish the role of Zn in male infertility.
Setting and Design:
The present study was carried out in five- years period from 2004 to 2009. It was a descriptive analytical study with non probability sampling.
Materials and Methods:
Semen examination of the patients was carried out according to the standardized method of the World Health Organization. Semen Zn was estimated by color 5 Br. PAPS method.
Statistical Analysis:
All statistical analyses were performed by using SPSS (Version 14.0 for windows) software, by applying student's t-test.
Results:
The result showed that seminal Zn was 702.92±10.60, 598.48±12.95, 617.54±9.55, 542.29±22.75, 710.36±7.87, 712.06±7.96, 789.36±21.33, and 762.06±8.99 mg/dl in azoospermic, oligozoospermic, asthenozoospermic, oligoasthenozoospermic, teratozoospermic, normozoospermic, polyzoospermic, and proven fathers group, respectively.
Conclusions:
Decreased concentration of seminal Zn do affect the sperm count, while increased level of seminal plasma Zn causes decreased sperm motility; so, it is suggested that administration of Zn should be very carefully monitored in such patients having low sperm count but normal sperm motility, as adequate seminal Zn is required for normal sperm function.
Keywords: Asthenozoospsermia, azoospermia, male infertility, oligozoospermia, seminal zinc
INTRODUCTION
Infertility is defined as the inability to conceive after one year of unprotected sexual interaction.[1] It has been reported that it affects about 15% of couples and a male factor alone is responsible in about 50% of these cases.[2] Lower sexual and poor personnel quality of life has been reported in infertile males.[3] Besides this, there are some other risk factors leading to defective spermatogenesis, and hence male infertility, like varicocele, cryptorchidism, infections, obstructive lesions, cystic fibrosis, trauma, genitourinary infection, environmental agents, and nutritional deficiency of trace elements like, selenium, zinc (Zn), vitamins, and oxidative stress.[4,5]
The Zn which is second only to iron as the most abundant element in the body is found in chicken, nuts, meat, fish, milk, and legumes. Despite this, the World Health Organization (WHO) estimates that one-third of world population is deficient in Zn. Zn is critical to reproduction potential. The Zn content of semen is 87 times that in the blood and has been reported to protect sperm from bacteria and chromosomes damage.[6] Zn in the body plays an important role in normal testicular development, spermatogenesis, and sperm motility.[7]
Deficiency of Zn is associated with hypogonadism and insufficient development of secondary sex characteristics in human beings and can cause atrophy of the seminiferous tubules in the rat, leading to failure in spermatogenesis and impotence.[8–10] Low seminal Zn levels were correlated with a decrease in fertilizing ability of sperm,[11] while some other studies with adult males experimentally deprived of Zn showed that leydig cell synthesis of testosterone was decreased.[12]
Prostate gland contains high concentration of Zn; however, lower concentration of seminal Zn has been reported because of its dilution with vaginal and cervical fluids after ejaculation. It is not clear with certainty, as to how Zn level in seminal plasma affects the sperm function. Keeping all these in mind, the present study was designed with an objective to establish the possible role of Zn with infertility in our population.
MATERIALS AND METHODS
The present descriptive analytical study was carried out in the Department of Reproductive Physiology/Health, Public Health Laboratories Division, of a tertiary care centre. A total of 2 000 subjects were referred for semen analysis from different infertility clinics in a five-year period from 2004 to 2009. Complete medical history and informed consent from the patients was taken. Of 2000 subjects, 1521 were finally analyzed and included in the study, along with 97 proven fathers, as control.
These subjects were divided into seven groups on the basis of sperm count, motility, and morphology. Their selection was based on inclusion and exclusion criteria.
Inclusion criteria
Males with primary and secondary infertility without treatment and having no relatable cause of infertility were included in the study.
Exclusion criteria
The patients who had undergone pelvic surgery or hernia repair, patients with diabetes mellitus, thyroid disease, and subjects who were on medicine were not included in this study.
Collection and examination of semen samples
The collection and examination of semen were done by properly standardized procedures, as mentioned in WHO laboratory manual.[13,14]
Storage of seminal plasma
After performing semen analysis, the rest of the semen samples were centrifuged at 2 000 rpm for 15 to 20 minutes. The pellet was discarded, while the supernatant of the semen samples were aliquoted and stored at -20°C for evaluation of seminal Zn.
Determination of seminal plasma zinc
Semen Zn was estimated by color 5 Br. PAPS method (order No. ZF 01000050; Centronic GmbH, Germany) using the basic principle that at pH 9.8, Zn forms a red chelated-complex with 2-(5-brom-2-pyridylazo)-5-(N -propyl--N--sulfopropylamino)-phenol.[15]
STATISTICAL ANALYSIS
Statistical analysis was performed by using SPSS (Version 14.0) software, by applying student's t-test.
RESULTS
The patients (n=1521) were divided into different groups on the basis of concentration, motility, and morphology of sperms. According to the nomenclature of semen recommended by WHO,[14] semen sample were categorized as--without spermatozoa (azoospermia), sperm concentration <20 million/ml (oligozoospermia), sperm concentration >250 million/ml (polyzoospermia), sperms having disturbed morphology of more than 30% of normal (teratozoospermia), motility <50% (asthenozoospermia), while the semen sample having progressive activity >25% (overall motility >50%) with sperm concentration within the range of 20 to 250 million/ml were classified as normozoospermia. A group representing 97 proven fathers was taken as a control.
Sperm concentration was 6.99 ± 0.35, 50.11 ± 2.12, 4.45 ± 0.42, 5.64 ± 1.15, 87.49 ± 3.51, 402.23 ± 39.70, and 102.12 ± 1.34 millions/ml in oligozoospermic, asthenozoospermic, oligoasthenozoospermic, teratozoospermic, normozoospermic, polyzoospermic, and proven fathers group, respectively, while it was nil in azoospermics. Seminal Zn was 702.92 ± 10.60, 598.48 ±12.95, 617.54 ± 9.55, 542.29 ± 22.75, 710.36 ± 7.87, 712.06 ± 7.96, 789.36 ± 21.33, and 762.06 ± 8.99 ΅g/dl in azoospermic, oligozoospermic, asthenozoospermic, oligoasthenozoospermic, teratozoospermic, normozoospermic, polyzoospermic, and proven fathers group, respectively [Table 1].
Table 1.
Seminal parameters in relation to semen zinc levels
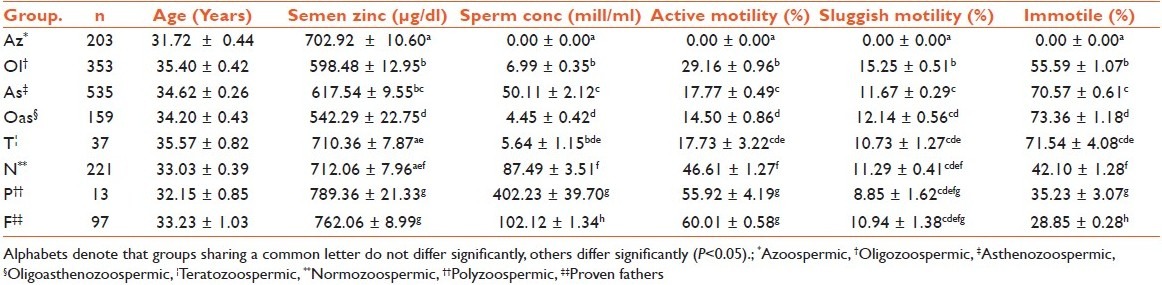
Results of the study showed that semen Zn was several folds higher in case of polyzoospermic subjects. In case of proven fathers, the levels of semen Zn differ nonsignificantly (P>0.05) from polyzoospermia cases only.
Similarly, serum Zn concentration varies with percentage of actively motile sperms, sluggish motility, and immotile sperms in different groups studied [Figure 1].
Figure 1.
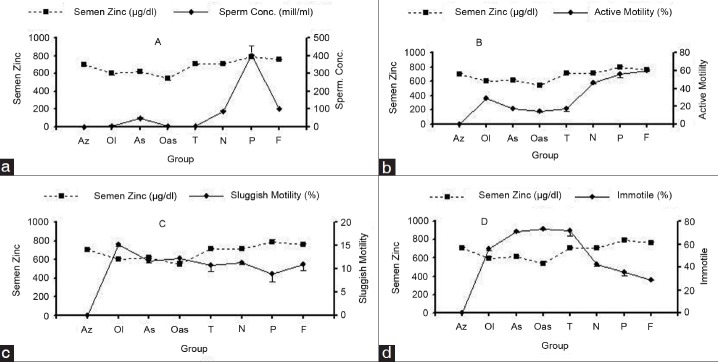
Semen zinc levels in relation to sperm concentration (a), active motility (b), sluggish motility (c) and immotile fraction (d) in different groups
DISCUSSION
The trace elements Zn and magnesium (Mg) found in seminal plasma originate primarily from the prostate gland and may reflect prostatic secretary function. Studies have suggested that Mg may play a role in spermatogenesis, particularly in sperm motility.[16] The same is true for Zn, although the results of several studies are still contradictory.[17] Zn, B complex vitamins (B6, B12 and folic acid), vitamin C, and antioxidants are critical nutrients in the male reproductive system for proper hormone metabolism, sperm formation, and motility.[18,19] Moreover, a positive correlation has been observed between the sperm count and seminal plasma Zn concentration in oligozoospermic and azoospermic patients.[20]
Sperm motility is significantly influenced by Zn. Stiffening of the outer dense fibers by formation of disulfide bridges during epididymal sperm maturation seems to be an essential physiologic step for the generation of sperm motility; especially progressive motility.[21] Zn deficiency has been linked with male sterility and subfertility. According to a study conducted in five middle-aged men following a Zn-restricted diet, the men underwent Zn depletion and their sperm counts dropped from a mean of 283 million/ml to 45 million/ml within 2 to 14 months.[22] Similarly, pathozoospermia is associated with low seminal Zn levels. Severe Zn depletion causes a 50% decrease in the amount of Zn per ejaculate,[23] which affect the semen quality either by reducing the antioxidant capacity or by counteracting the effects of other heavy metals. In another study, geometric means of the seminal plasma Zn concentration was found to be significantly lower (P<0.05) in infertile group compared with fertile group.[24]
In contrast to these studies, other authors had reported normal and even increased seminal plasma Zn levels in infertile males.[17,25] The probable explanation could be that Zn in semen is responsible for motility, therefore, it may not affect in both oligozoospermic and azoospermic groups.[26] In contrast to these findings, we found decreased level of seminal Zn in both azoospermic and oligozoospermic patients, which may be because of the presence of large number of pus cells in the seminal fluid of these patients.
High Zn content in seminal plasma had also been associated with a high degree of sperm cell motility.[26] In another study, it has been demonstrated that extracellular Zn acts as an inhibitor of human sperm motility and acrosome reaction.[27] We found decreased level of semen Zn in azoospermic, oligozoospermic, asthenozoospermic, and oligozoospermic groups. However, seminal plasma Zn in those patients having >50% of motility had significantly increased concentration than those having decreased (<50%) motility, which is in contrast to the study conducted by Dissanayake et al.[23]
In our study, semen Zn showed a direct relationship to active motility and inverse relation with immotile fraction. As motility is Zn dependent, when Zn level increases, motility also increases and vice versa [Table 1 and Figure 1]. This has been observed in polyzoospermic, normozoospermic, oligozoospermic, asthenozoospermic, and oligoasthenozoospermic patients. Similarly, concentration of Zn decreases when count decreases, except in azoospermic patients.
It is concluded that decreased concentration of seminal plasma Zn do affect the sperm count and sperm motility. It can be suggested that the administration of Zn should be very carefully monitored in those patients having low sperm count but normal sperm motility. In such cases, seminal plasma Zn level should be measured before treatment, since adequate seminal plasma content of Zn is required for normal sperm function.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Turek PJ. Male infertility. In: Tanagho EA, McAninch JW, editors. Smith's Genreral Urology. 17th ed. USA: The McGraw-Hill Companies; 2008. p. 684. [Google Scholar]
- 2.Abid S, Maitra A, Meherji P, Patel Z, Kadam S, Shah J, et al. Clinical and Laboratory Evaluation of Idiopathic Male Infertility in a Secondary Referral center in India. J Clin Lab Anal. 2008;22:29–38. doi: 10.1002/jcla.20216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith JF, Walsh TJ, Shindel AW, Turek PJ, Wing H, Pasch L, et al. Sexual, Marital and social impact of a man's Perceived Infertility Diagnosis. J Sex Med. 2009;6:2505–15. doi: 10.1111/j.1743-6109.2009.01383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agarwal A, Makker K, Sharma R. Clinical relevance of oxidative stress in Male Factor Infertility. Am J Reprod Immunol. 2007;59:02–11. doi: 10.1111/j.1600-0897.2007.00559.x. [DOI] [PubMed] [Google Scholar]
- 5.Wong WY, Thomas CM, Merkus JM, Zielhuis GA, Steegers-Theunissen RP. Male factor sub-fertility: Possible causes and the impact of nutritional factors. Fertil Steril. 2000;73:435–42. doi: 10.1016/s0015-0282(99)00551-8. [DOI] [PubMed] [Google Scholar]
- 6.Judith EB. Nutrition through life cycle. 3rd ed. St. Paul, Minnesota: Brooks/Cole publishing company; 2008. [Google Scholar]
- 7.Madding Cl, Jacob M, Ramsay VP, Sokol RZ. Serum and semen zinc levels in normospermic and oligozoospermic men. Ann Nutr Metab. 1986;30:213–8. doi: 10.1159/000177196. [DOI] [PubMed] [Google Scholar]
- 8.Sandstead HH, Prasad AS, Schulert AR, Farid Z. Human zinc deficiency, endocrine manifestation and response to treatment. Am J Clin Nutr. 1967;20:422–42. doi: 10.1093/ajcn/20.5.422. [DOI] [PubMed] [Google Scholar]
- 9.Sandstorm B, Sandberg AS. Inhibitory affects of isolated inositol phosphates on zinc absorption in humans. J Trace Elem Electrolytes Health Dis. 1992;6:99–103. [PubMed] [Google Scholar]
- 10.Endre L, Beck F, Prasad A. The role of zinc in human health. J Trace Elem Exp Med. 1990;3:333–75. [Google Scholar]
- 11.Pandy VK, Parmeshwaran M, Soman SD, Dacosta JC. Concentrations of morphologically normal, motile spermatozoa: mg+2, ca+2 and zn+2 in semen of infertile men. Sci Total Environ. 1983;27:49–52. doi: 10.1016/0048-9697(83)90122-5. [DOI] [PubMed] [Google Scholar]
- 12.Prasad AS. Discovery of human zinc deficiency and studies in an experimental human model. Am J Clin Nutr. 1991;53:403–12. doi: 10.1093/ajcn/53.2.403. [DOI] [PubMed] [Google Scholar]
- 13.WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. Cambridge: Cambridge University Press; 1992. pp. 1–107. [Google Scholar]
- 14.Atiken RI, Aribarg A, Gopal Krishnan K, Hamiltion DW, Katz DF, Wang C, et al. WHO laboratory manual for the examination of human semen and sperm cervical mucus interaction. Cambridge: Cambridge University Press; 1980. Collection and examination of human semen. [Google Scholar]
- 15.Johnsen O, Eliasson R. Evaluation of a commercially available kit for the colorimetric determination of zinc. Int J Androl. 1987;10:435–40. doi: 10.1111/j.1365-2605.1987.tb00216.x. [DOI] [PubMed] [Google Scholar]
- 16.Abou-shakra FR, Ward NI, Everard DM. The role of trace elements in male infertility. Fertile. 1989;52:307–10. doi: 10.1016/s0015-0282(16)60860-9. [DOI] [PubMed] [Google Scholar]
- 17.Lewis-jones DL, Aird IA, Biljan MM, Kingsland CR. Effects of sperm activity on zinc and fructose concentration in seminal plasma. Hum Reprod. 1996;11:2465–7. doi: 10.1093/oxfordjournals.humrep.a019138. [DOI] [PubMed] [Google Scholar]
- 18.Geva E. The effect of antioxidant treatment on human spermatozoa and fertilization rate in an in-vitro fertilization program. Fertile Steril. 1996;66:430–4. doi: 10.1016/s0015-0282(16)58514-8. [DOI] [PubMed] [Google Scholar]
- 19.Czeizel AE. Periconceptual folic acid containing multivitamin supplementation. Eur J Obstet Gynecol Reprod Biol. 1998;78:151–61. doi: 10.1016/s0301-2115(98)00061-x. [DOI] [PubMed] [Google Scholar]
- 20.Ali H, Ahmed M, Baig M, Ali M. Relationship of zinc concentration in blood and seminal plasma with various semen parameters in infertile subjects. Pak J Med Sci. 2007:23111–4. [Google Scholar]
- 21.Henkel R, Bittner J, Weber R, Huther F, Miska W. Relevance of zinc in human sperm flagella and its relation to motility. Fertil Steril. 1999;71:1138–43. doi: 10.1016/s0015-0282(99)00141-7. [DOI] [PubMed] [Google Scholar]
- 22.Mc-Graw H. A study ties zinc deficiency to male infertility. Med World News. 1979;20:12–6. [Google Scholar]
- 23.Dissanayak D, Wijesinghe PS, Ratnasooriya WD, Wimalasena S. Relationship between seminal plasma zinc and semen quality in a subfertile population. J Hum Reprod Sci. 2010;3:124–8. doi: 10.4103/0974-1208.74153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chia SE, Ong CN, Chua LH, Ho LM, Tay SK. Comparison of zinc concentrations in blood and seminal plasma and the various sperm parameters between fertile and infertile men. J Androl. 2000;2:52–7. [PubMed] [Google Scholar]
- 25.Stankovic H, Mikac-devic D. Zinc and copper in human semen. Clin Chem Acta. 1976;70:123–6. doi: 10.1016/0009-8981(76)90013-9. [DOI] [PubMed] [Google Scholar]
- 26.Saeed S, Khan FA, Rehman SB, Khan DA, Ahmad M. Biochemical parameters in evaluation of oligospermia. J Pak Med Assoc. 1994;44:137–40. [PubMed] [Google Scholar]
- 27.Riffo M, Leiva S, Astudillo J. Effect of zinc on human sperm motility and acrosome reaction. Int J Androl. 1992;15:229–37. doi: 10.1111/j.1365-2605.1992.tb01343.x. [DOI] [PubMed] [Google Scholar]


