Abstract
Knowledge of variations in arteries and nerves of infratemporal fossa may be helpful in radical neck dissection and in dental procedures to avoid the complications. We present an unusual case in which maxillary artery was found deep (medial) to lateral pterygoid muscle. Lingual nerve originated from two roots: anterior and posterior. Anterior root originated from common trunk and the posterior root directly from mandibular nerve. Inferior alveolar nerve was a continuation of the common trunk. Branches of mandibular nerve formed a loop through which passed the second part of maxillary artery. The clinical significance of the present variations has been discussed.
Keywords: Inferior alveolar nerve, lateral pterygoid muscle, lingual nerve, maxillary artery
INTRODUCTION
Knowledge of maxillary artery (MA) and its branches in the infratemporal region is of great importance in dental, oral, and maxillofacial surgeries.[1] MA is the largest terminal branch of the external carotid artery. It arises behind the mandibular neck, then passes medial to the mandibular neck and superficial or deep to the lower head of lateral pterygoid to reach the pterygoid fossa.[2]
The inferior alveolar nerve (IAN) is a mixed nerve that provides sensory innervation to the lower teeth, lower lip, and buccal mucosa located between the premolars and lower central incisor through the mental nerve, and the motor innervation to the mylohyoid muscle and anterior belly of the digastric muscle through the mylohyoid nerve. The lingual nerve (LN) carries sensory fibers to the mucosa of the floor of the mouth, the ventral side of the tongue and to the anterior 2/3 of the tongue and secretary fibres to the sublingual and submandibular glands.[3]
Literature is replete with variations in infratemporal region, in the form of communication between branches of mandibular nerve (MN), entrapment of nerves by bony bridges, abnormal course and branching pattern of arteries.[1,4,5] We present a rare case of complex relation of LN and IAN with second part of MA and discussed its clinical implications.
CASE REPORT
The described variations were found in left infratemporal fossa of a 65-year-old male cadaver during routine dissection. The history of the individual and the cause of death were not known. The infratemporal fossa was exposed by resection of ramus of mandible, zygomatic arch, and lateral pterygoid muscle. The topographic details of the fossa were examined by causal dissection and photographed. We came across the following variations.
In nerves
LN was formed by two roots: anterior and posterior. Posterior root (PR) originated from the MN directly, while the anterior root (AR) was a branch of common trunk (CT). CT originated from MN directed downward anterior to second part of MA and was about 2 cm in length. CT was divided into two branches, AR of LN which was about 4 mm in length directed downwards and medially, and other branch continued downwards as IAN [Figure 1a].
Figure 1.
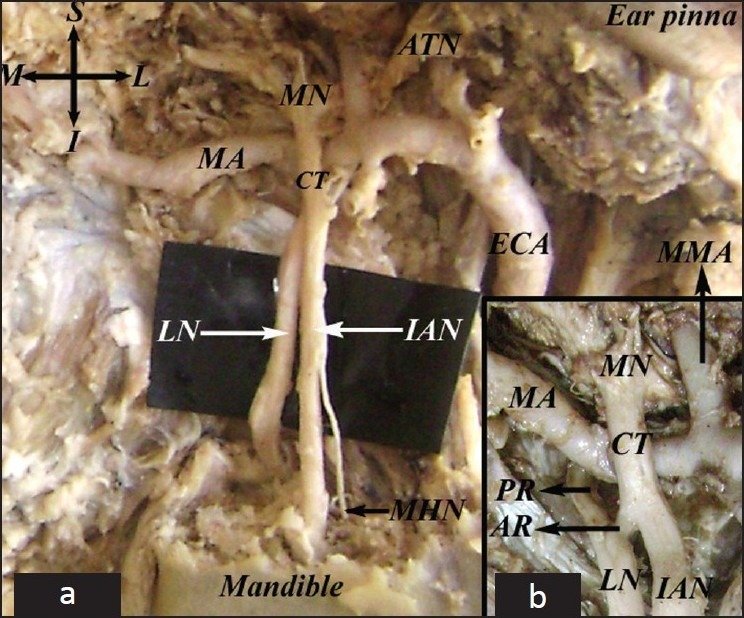
(a) Second part of maxillary artery (MA) passing through the nerve loop formed by mandibular nerve (MN), common trunk (CT), anterior root of lingual nerve (AR), and posterior root of lingual nerve (PR). Also seen are mylohyoid nerve (MHN) and auriculotemporal nerve (ATN). (b) (Inset) Close view of the artery-nerve complex showing common trunk (CT) arise from mandibular nerve (MN), anterior root of lingual nerve (AR), posterior root of lingual nerve (PR), and maxillary artery (MA).
In artery
MA instead of being lateral (superior) to lateral pterygoid muscle was found medial (deep) to the muscle. Second part of MA passed through the nerve loop which was superiorly formed by MN, anteriorly by CT, posteriorly by PR and inferiorly by AR [Figure 1b].
DISCUSSION
Hussain et al. (2008) reported in a study that the relationship of the MA and lateral pterygoid muscle (LPM) is still a controversial topic. They reported that the MA was lateral (superficial) to the LPM in 68% (30) and medial (deep) in 32% (14) of cases.[6]
The communicating branches between the IAN and LN are well described in the literature and these communications have been identified as a possible explanation for the inefficient mandibular anesthesia and also suggested that it will affect the mobility of the nerves.[1] Erdogmus et al observed that the LN was divided into anterior and posterior parts by pterygospinous bony bridge. The anterior part passed medially and posterior part lateral to the bony bridge.[5] In our case the two roots were separated by MA. Sandoval et al presented a similar case in which second part of maxillary artery passes through the nerve loop formed anteriorly by IAN and posteriorly by LN.[3] The communicating nerve between IAN and LN was thin compared to the present case.
Arterial variations in infratemporal region cause failure of inferior alveolar nerve block and intravascular injection during the procedure which leads to serious systemic complications which may endanger the life of patient. Frangiskos et al reported arterial penetration during mandibular block in up to 20% of cases.[7] The infratemporal fossa is a complex region on the skull base that is affected by benign and malignant tumors. This type of anatomical knowledge is essential in choosing the best approach to treat lesions in this area.[8]
As in the present case, a close approximation of MA to the LN and IAN may lead to arterial penetration during IAN anesthesia and cause systemic complications. MA puncture during administration of local anesthetic can cause a hematoma which can exert a soft pressure in surrounding structures such as LN and the IAN leading to sensory alterations which must be considered in the differential diagnosis of facial pain, hyperalgesia, and allodynia.[3] If the artery is passing through the nerve loop, increased blood flow may irritate the surrounding nerves, leading to tingling and numbness in their area of distribution. Knowledge of such arterial and nervous complex may be helpful in radical neck dissection and in dental procedures to avoid untoward complications.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Nayak SR, Rai RL, Krishnamurthy A, Prabhu LV, Ranade AV, Mansur DI, et al. An unusual course and entrapment of the lingual nerve in the infratemporal fossa. Bratisly Lek Listy. 2008;109:525–7. [PubMed] [Google Scholar]
- 2.Williums PL, Warwick R, Dyson M, Banister HL. Gray's Anatomy. 37th ed. London: ELBS, Churchill Livingstone; 1993. p. 582. [Google Scholar]
- 3.Sandovalo MC, Lopez FB, Suazo GI. An unusual relationship between the inferior alveolar nerve, lingual nerve and maxillary artery. Int J Odontostomat. 2009;3:51–3. [Google Scholar]
- 4.Potu AK, Pulakunta T, Ray B, Rao MS, Bhat KM, D’silva SS, et al. Unusual communication between the lingual nerve and mylohyoid nerves in a south Indian male cadaver: Its clinical significance. Rom J Morphol Embryol. 2009;50:145–6. [PubMed] [Google Scholar]
- 5.Erdogmus S, Pinar Y, Celik S. A cause of entrapment of the lingual nerve: Ossified pterygospinous ligament- a case report. Neuroanatomy. 2009;8:43–5. [Google Scholar]
- 6.Hussain A, Binahmed A, Karim A, Sondor KG. Relationship of the maxillary artery and lateral pterygoid muscle in a Caucasian sample. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:32–6. doi: 10.1016/j.tripleo.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 7.Frangiskor F, Stavou E, Merenditis N, Tsitsogianis H, Vardas E, Antonopoulou I. Incidence of penetration of a blood vessel during inferior alveolar nerve block. Br J Oral Maxillofac Surg. 2003;41:188–9. doi: 10.1016/s0266-4356(03)00045-7. [DOI] [PubMed] [Google Scholar]
- 8.Isolan GR, Rowe R, Al-Mefty O. Microanatomy and surgical approaches to the infratemporal fossa: An anaglyphic three-dimensional stereoscopic printing study. Skull Base. 2007;17:285–302. doi: 10.1055/s-2007-985193. [DOI] [PMC free article] [PubMed] [Google Scholar]


