Abstract
Background and Objective:
Worldwide, many neonates with sepsis die due to lack of early diagnosis. In this study we attempt to analyze the value of various immunological and hematological parameters, singly and in combination, for the diagnosis of neonatal sepsis, with the aim being to formulate guidelines for the early diagnosis of the condition.
Materials and Methods:
In this prospective study, 62 patients having clinical suspicion of neonatal sepsis were evaluated with a battery of investigations. Neonates admitted for other causes and without clinical suspicion of sepsis were selected as controls (n=40). The tests included blood culture, hemoglobin level, total and differential blood count, absolute neutrophil count, ratio of immature to total neutrophil count (I/T ratio), micro-erythrocyte sedimentation rate (m-ESR), C-reactive protein (CRP), platelet count, serum IgM level, and plasma fibrinogen level. Patients were divided into proven cases (positive blood culture) and probable cases (negative blood culture).
Results:
Positive blood culture was seen in 38 cases (61.3%). Raised m-ESR (>8 mm in the first hour) was seen in 63.2% of proven and 66.7% of probable cases. I/T ratio of ≥0.2 was seen in 63.2% and 58.3% of proven and probable cases, respectively. Morphological changes in neutrophils were detected in 68.4% of proven cases and 91.7% of probable cases. Positive CRP test (≥6 mg/l) was found in 84.2% of proven cases and 100% of probable cases. Raised serum IgM, leucopenia, and neutropenia were seen in a small number of patients (11%–37%). Raised fibrinogen level (>400 mg/l) was seen in patients as well as in controls.
Conclusions:
The four useful tests that we identified were m-ESR, I/T ratio, morphological changes in neutrophils, and CRP; and role of these tests in early diagnosis of neonatal sepis were statistically significant (P<.05). The most sensitive test was CRP (84%) and the most specific test was m-ESR (94%). A combination of three or all of these four tests was highly specific (95%–100%).
Keywords: Laboratory tests, neonatal sepsis, early diagnosis
INTRODUCTION
Neonatal sepsis is a clinical syndrome resulting from the pathophysiological effects of severe bacterial infection in the first month of life. In contrast to bacteremia (bacteria in blood), septicemia usually consists of bacteriemia plus a constellation of signs and symptoms caused by microorganisms or their toxic products in circulation. There may be progression of bacteriemia to septicemia depending on clinical manifestations. However, septicemia may also occur without bacteriemia, such as in culture-negative sepsis associated with pyelonephritis or pneumonia due to endotoxemia.
The clinical diagnosis of neonatal sepsis is difficult because the signs and symptoms are not always specific. There is no laboratory test with 100% sensitivity and specificity.[1,2] Blood culture has been considered the gold standard for confirmation of diagnosis but the results are available only after 48–72 hours. Moreover, in many cases blood culture fails to detect the offending organism/bacteria. So, the search for a reliable test continues, especially one that is useful in culture-negative cases.
We planned this study to identify cost-effective markers/tests for the diagnosis of early neonatal sepsis so that prompt treatment can be initiated and neonatal deaths can be minimized.
MATERIALS AND METHODS
A total of 62 neonates (infants <1 month of age) with clinical suspicion of septicemia were selected for this prospective study that was conducted over a period of 1 year, from June 2008 to May 2009, in our institute. Septicemia was suspected from clinical history, signs, symptoms, and presence of predisposing factors in mothers and neonates. Maternal factors included illness during pregnancy, e.g., hypertension, chronic renal disease, diabetes mellitus, toxemia of pregnancy, antepartum hemorrhage, maternal fever during the last 2 weeks of pregnancy, prolonged rupture of membranes (>18 hours), meconium-stained liquor amnii, and difficult labor with instrumentation. Neonatal factors included artificial resuscitation, intravenous fluid administration, umbilical vein catheterization, failure to thrive, refusal to suck, abdominal distension, jaundice, recurrent attacks of apnea and cyanosis, hypothermia, sclerema, and convulsion.
Before collection of blood, the puncture site and adjacent area were sterilized by swabbing with spirit. Blood was collected by femoral vein puncture and transferred into culture broth as well as into three different vials for the different hematological and immunological tests. Ethylenediaminetetraacetic acid (EDTA)–mixed venous blood was used to estimate hemoglobin (Hb), total leukocyte count, and platelet count. Citrated blood was used to estimate plasma fibrinogen level. For estimation of serum IgM and C-reactive protein (CRP), clotted blood was used. To estimate micro-erythrocyte sedimentation rate (m-ESR), capillary blood was taken in a heparinized micro-hematocrit tube. Blood smears were made on glass slides for differential leukocyte count, absolute neutrophil count, morphological changes in neutrophils (toxic granules, vacuoles, and Dohle bodies in the cytoplasm), and ratio of immature to total neutrophils (I/T ratio). Plasma fibrinogen was estimated by a reagent kit that was based on a modified Clauss method. A diagnostic kit was also used to determine serum IgM level by an immunochemical assay. The cutoff values of the tests were taken from the literature and diagnostic kits. Statistical analysis was done using SPSS® software, version 17.
Among the 62 clinically suspected cases, blood culture was positive in 38 cases and these were regarded as proven cases. In 24 cases, though the blood culture reports were negative, there was strong clinical suspicion of neonatal sepsis, which was supported by other laboratory tests; this second group was regarded as probable cases.
RESULTS
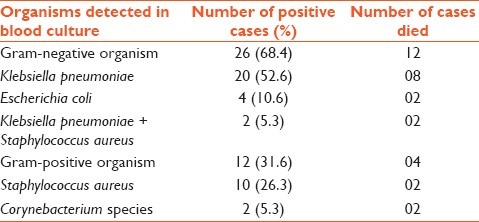
In the present study, of the 62 cases, 38 had positive blood culture reports (proven cases). Gram-negative organisms were commoner (n=26; 68.4%) than gram-positive organisms (n=12; 31.6%). Klebsiella pneumoniae was the commonest bacteria (52%), followed by Staphylococcus aureus (26%). In one case there was mixed infection with K pneumoniae and S aureus. Twelve neonates suffering from gram-negative bacteremia and four neonates suffering from gram-positive bacteremia died despite treatment [Table 1].
Table 1.
Bacteriological profile in blood culture–positive cases (proven cases) (n=38)
Of the 38 proven cases, 32 (84%) were low birth weight (LBW) infants (weight <2.5 kg), whereas 14/38 (37%) were preterm infants (<37 weeks of gestational age).
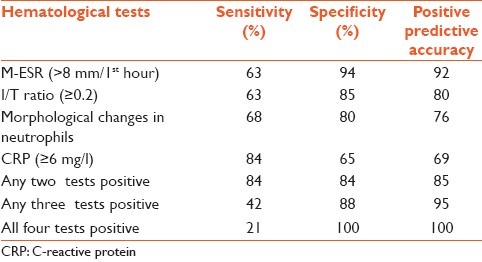
Among all the tests performed, four tests (CRP, m-ESR, I/T ratio, and morphological changes in the neutrophils) proved to be very useful tests to diagnose the early neonatal sepsis and test results were statistically significant [Table 2]. CRP had the highest sensitivity (84%) and m-ESR had the highest specificity (94%). The highest positive predictive accuracy of 92% was seen with m-ESR. We found that specificity and positive predictive value increased when the results of these tests were considered together. When two tests turned out to be positive the specificity and positive predictive value were 84% and 85%, respectively. When three tests showed positive results the specificity and positive predictive value were 88% and 95%, respectively. With all four tests positive, both specificity and positive predictive value were 100%. However, combination of these tests resulted in decreased sensitivity (84% when two tests were positive, 42% when three tests were positive, and 21% when all four tests were positive) [Table 3]. The best combination of two tests in this study was found to be CRP and I/T ratio (sensitivity 52% and specificity 95%). The second best combination was m-ESR and CRP, followed by m-ESR and I/T ratio.
Table 2.
The four most useful tests and their results in control, probable, and proven cases
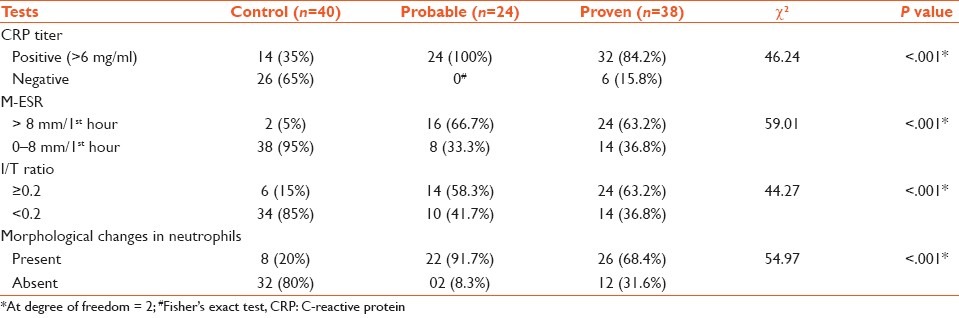
Table 3.
Sensitivity, specificity, and positive predictive value of the hematological tests and their different combinations
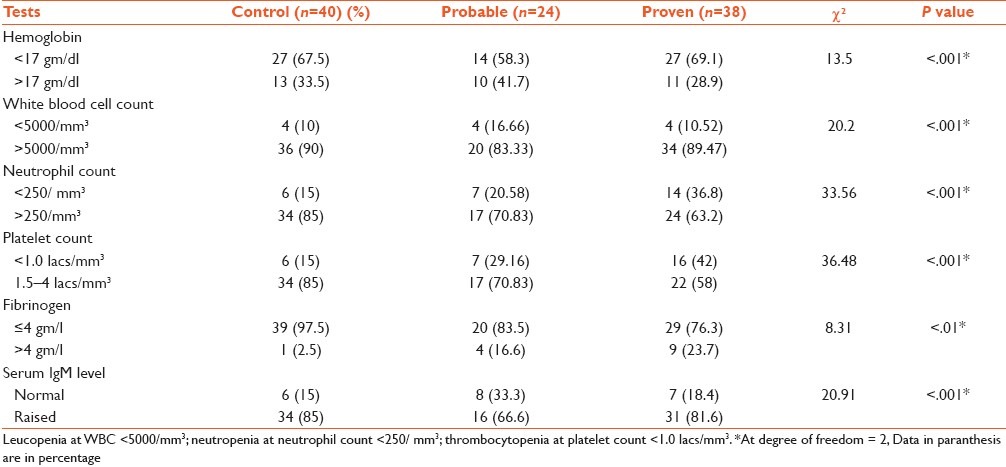
Of the 38 proven cases, 27 (69.1%) had low Hb (<17 gm/dl) and 22 had unconjugated hyperbilirubinemia that was neither due to Rh hemolytic disease nor due to ABO blood group incompatibility. Among the 24 probable cases, 14 (58.3%) had low Hb, and 10 had unconjugated hyperbilirubinemia. Leucopenia was seen in 4 of the 38 proven cases on day 4 investigations and all of these patients died. Only two patients developed leukocytosis on day 4 investigations, and both these patients survived. Among the probable cases of sepsis, the findings were similar. In both proven and probable cases of sepsis the percentage of neonates showing thrombocytopenia was higher than among control cases. High fibrinogen level was found in 4 of the 24 probable cases (16.6%), in 9 of the 38 proven cases (23.7%), and in 1 control case. Raised serum IgM level was seen in the majority of proven and probable cases, as well as in controls [Table 4].
Table 4.
Results of other tests in control, probable, and proven sepsis cases
DISCUSSION
The World Health Organization estimates that perinatal deaths are responsible for most of the childhood mortality below the age of 5 years in the developing countries.[3] Neonatal infections are by far the most common cause of such perinatal mortality.[4,5] Considering the high mortality and serious morbidity among neonates suffering from sepsis, a diagnostic marker with high sensitivity and specificity is desirable. However, there is no laboratory marker that has all the characteristics of an ideal infection marker. Interleukin-6 (IL-6) and interleukin-8, CD11b, and procalcitonin (PCT) are all sensitive markers of infections. CD64 is the most sensitive marker of late nosocomial infection.[6] CD64 can be used either alone or in combination with IL-6 and CRP for early diagnosis of neonatal sepsis. The advantages of CD64 when compared with IL-6 and CRP are rapid quantitation, the very small blood volume required, and easy handling.[7] PCT is also a very useful marker for diagnosis of early-onset neonatal sepsis (EONS). In very-low-birth-weight neonates, a serum PCT value >2.4 ng/ml justifies early empirical antibiotic therapy, while in normal-birth-weight infants a PCT value of 0.5–2.4 ng/ml indicates neonatal sepsis.[8]
In the present study, the majority of neonates with proven sepsis (32/38; 84.2%) had LBW and a fair number of them were preterm (14/38; 36.8%). Ng et al. used CRP, cytokines, and adhesion molecule to identify late-onset neonatal sepsis (LONS) in preterm infants with very low birth weight.[9] They found that IL-6 had the highest sensitivity (89%) and negative predictive value (91%) for detecting infection on day 0. However, between 24 hours and 48 hours of onset CRP was the best single marker. In another study it was found that IL-6 combined with PCT values was a fair way to evaluate EONS, and also that I/T ratio was as efficient as IL-6.[10] Walliullah et al. found the sensitivity and specificity of m-ESR to be 63.3% and 60%, respectively, and that of I/T ratio to be 70% and 56%, respectively, in neonatal sepsis.[11] They also found that a combination of m-ESR and I/T ratio showed high sensitivity (80%) and specificity (70%). However, in the present study, a combination of m-ESR and I/T ratio showed low sensitivity (31%) and high specificity (95%).
Several other authors have studied CRP and hematological parameters in neonatal sepsis.[12–14] Most of them found that CRP especially in combination with other tests were very helpful to diagnose neonatal sepsis. During the first 3 days of life CRP, leucopenia, and neutropenia were reported to be comparatively good tests, while after 3 days of life CRP was the best single test for detecting EONS.[15,16] In our study, CRP was the most sensitive test (84%), though with a relatively low specificity of 65%. However, when CRP was combined with I/T ratio, the specificity increased to 95%. Combination of CRP with other tests also gave good results. CRP can be used to differentiate between positive and contaminated blood culture in children and has been shown to be a better predictor than white blood count (WBC) or absolute neutrophil count (ANC) for this purpose.[15] Morphological changes in neutrophils showed high sensitivity (68%) and specificity (80%) in our study, but other authors have found relatively lower sensitivity (44%) and higher specificity (94%).[13] Some authors formulated a hematological scoring system (HSS) to diagnose EONS;[10,12] a hematological score of ≥3 had sensitivity of 86% and a negative predictive value of 96%.[14]
Hematological tests like Hb level, total leukocyte count, differential leukocyte count, and platelet count, when combined with the four important tests mentioned earlier, have been found to be very useful to diagnose neonatal sepsis.[11,17,18] In our study, 27 of the 38 proven cases (69.1%) had low Hb. Many of them (n=18) had unconjugated hyperbilirubinemia that was not due to ABO or Rh incompatibility. In these cases, the low Hb level could have been due to increased hemolysis of red blood cells caused by bacterial infection in blood.
The first immunoglobulin produced by neonates is IgM and increased level of this antibody is found in acute bacterial, viral, and parasitic infections. In this study, serum IgM was raised in both proven sepsis cases and in controls. So, the test was not very helpful in diagnosing neonatal sepsis. A similar observation was made by Adhikari et al.[19] However, others have reported that IgM concentration in the sepsis group (median: 34 mg/dl) was significantly higher than that in the ‘no sepsis’ group (median: 10 mg/dl; P<.0001).[20] The death rate among neonates with IgM levels <20 mg/dl was five times higher than that among those with elevated IgM levels.[21]
In the present study, fibrinogen levels were not helpful for identifying cases of neonatal infection. Speer et al. made similar observations.[22] Recently, molecular analysis by polymerase chain reaction (PCR) for bacterial DNA component encoding 16s RNA has been found to be very useful and even superior to blood culture for early diagnosis of sepsis in neonates. PCR has a sensitivity of 100% and specificity of 95.6%.[23]
In this study we have assessed various immunological and hematological markers/tests to find out their efficacy, when used singly and in combination, in the diagnosis of neonatal sepsis. As we have evaluated different tests and not just a single test, this study, in our opinion, is more informative than many other previous studies. We found that four of the tests (m-ESR, I/T ratio, morphological changes in neutrophils, and CRP) are cost-effective and can be very useful in developing countries where neonatal death due to sepsis is very common.
The limitation of this study is that newer markers like PCT, CD64, and CD11b have not been included.
To conclude, though there are several markers to diagnose neonatal sepsis, the search for the ideal marker is still on. In this study, four tests (m-ESR, I/T ratio, morphological changes in neutrophils, and CRP) were found to be cost-effective and useful for the diagnosis of neonatal sepsis.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Plazek MM, White LA. Early and late neonatal septicemia. Arch Dis Child. 1983;58:728–31. doi: 10.1136/adc.58.9.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gluck L, Wood HF, Fousek MD. Septicemia of the newborn. Pediatr Clin North Am. 1966;13:1131–47. doi: 10.1016/s0031-3955(16)31911-3. [DOI] [PubMed] [Google Scholar]
- 3.Geneva: World Health Organization; 2005. WHO. World Health Report. [Google Scholar]
- 4.Largo MG, Stekelenburg J. The millennium project of the United Nations, focusing on adequate postpartum care to reduce maternal and neonatal mortality world-wide. Ned Tijdschr Geneeskd, 2006;150:1143–7. [PubMed] [Google Scholar]
- 5.Mufti P, Setna F, Nazir K. Early neonatal mortality: Effects of interventions on survival of low birth babies weighing 1000-2000g. J Pak Med Assoc. 2006;56:174–6. [PubMed] [Google Scholar]
- 6.Radulova P. Neonatal infections. Diagnostic markers of infection. Akush Ginekol. 2010;49:42–51. [PubMed] [Google Scholar]
- 7.Dilli D, Oguz SS, Dilmen U, Koker MY, Kizilgun M. Predictive values of neutrophil CD64 expression compared with interleukin-6 and C-reactive protein in early diagnosis of neonatal sepsis. J Clin Lab Anal. 2010;24:363–70. doi: 10.1002/jcla.20370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Auriti C, Fiscarelli E, Ronchetti MP, Argentieri M, Marrocco G, Quondamcarlo A, et al. Procalcitonin in detecting neonatal sepsis. Arch Dis Child Fetal Ed. 2011 Mar 15; doi: 10.1136/fetalneonatal-2010-194100. [DOI] [PubMed] [Google Scholar]
- 9.Ng PC, Lam HS. Biomarkers for late-onset neonatal sepsis: Cytokines and beyond. Clin Perinatol. 2010;37:599–610. doi: 10.1016/j.clp.2010.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bender L, Thaarup J, Varming K, Krarup H, Ellermann-Eriksen S, Ebbesen F. Early and late markers for the detection of early-onset neonatal sepsis. Dan Med Bull. 2008;55:219–33. [PubMed] [Google Scholar]
- 11.Walliullah SM, Islam SM, Siddika M, Hossain MA, Chowdhury AK. Role of micro-ESR and I/T ratio in the early diagnosis of neonatal sepsis. Mymensing Med J. 2009;18:56–61. [PubMed] [Google Scholar]
- 12.Ahmed Z, Ghafoor T, Waquar T, Ali S, Aziz S, Mahmud S. Diagnostic value of C-reactive protein and haematological parameters in neonatal sepsis. J Coll Physicians Surg Pak. 2005;15:152–6. [PubMed] [Google Scholar]
- 13.Berger C, Uehlinger J, Ghelfi D, Blau N, Fanconi S. Comparison of C-reactive protein and white blood cell count with differential in neonates at risk for septicaemia. Eur J Pediatr. 1995;154:138–44. doi: 10.1007/BF01991918. [DOI] [PubMed] [Google Scholar]
- 14.Manucha V, Rusia U, Sikka M, Faridi MM, Madan N. Utility of haematological parameters and C-reactive protein in the detection of neonatal sepsis. J Pediatr Child Health. 2002;38:459–64. doi: 10.1046/j.1440-1754.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- 15.Shaoul R, Lahad A, Tamir A, Lanir A, Srugo I. C Reactive Protein (CRP) as a predictor for the bacteremia in children. Med Sci Monit. 2008;14:255–61. [PubMed] [Google Scholar]
- 16.Ghosh S, Mittal M, Jaganathan G. Early diagnosis of neonatal sepsis using a hematological scoring system. Ind J Med Sci. 2001;55:495–500. [PubMed] [Google Scholar]
- 17.Varsha, Rusia U, Sikka M, Faridi MM, Madon N. Validity of hematologic parameters in identification of early and late onset neonatal infection. Indian J Pathol Microbiol. 2003;46:565–8. [PubMed] [Google Scholar]
- 18.Selimovic A, Skokic F, Selimovic Z, Bazardzanovic M. The predictive values of total white blood count and differential count in the diagnosis of early-onset neonatal sepsis. Med Arch. 2008;62:205–10. [PubMed] [Google Scholar]
- 19.Adhikari M, Coovadia HM, Coovadia YM. Predictive value of C-reactive protein in neonatal septicemia. Ann Trop Pediatr. 1986;6:37–40. doi: 10.1080/02724936.1986.11748408. [DOI] [PubMed] [Google Scholar]
- 20.Khassaweneh M, Hayajneh WA, Kofahi H, Khader Y, Amarian Z, Daoud A. Diadnostic markers for neonatal sepsis: Comparing C-reactive protein, interleukein-6 and immunoglobulin M. Scand J Immunol. 2007;65:171–5. doi: 10.1111/j.1365-3083.2006.01878.x. [DOI] [PubMed] [Google Scholar]
- 21.Krishna BV, Nadquir SD, Tallur SS. Immunoglobulin-M estimation and C-reactive protein detection in neonatal septicemia. Indian J Pathol Microbiol. 2000;43:35–40. [PubMed] [Google Scholar]
- 22.Speer CP, Gahr M, Schroter W. Early diagnosis of neonatal infection. Montsschr Kinderheilkd. 1985;113:665–8. [PubMed] [Google Scholar]
- 23.Yadav AK, Wilson CG, Prasad PL, Menon PK. Polymerase Chain Reaction in rapid diagnosis of neonatal sepsis. Indian Pediatr. 2005;42:681–5. [PubMed] [Google Scholar]


