Abstract
BACKGROUND
To date, work-hour restrictions have not been imposed on attending surgeons in the United States. The purpose of this study was to investigate the impact of working an overnight trauma shift on outcomes of general surgery operations performed the next day by the post-call attending physician.
STUDY DESIGN
Consecutive patients over a 3.5-year period undergoing elective general surgical procedures were reviewed. Procedures were limited to hernia repairs (inguinal and ventral), cholecystectomies, and intestinal operations. Any operations that were performed the day after the attending surgeon had taken an overnight trauma shift were considered post-call (PC) cases; all other cases were considered nonpost-call (NP). Outcomes from the PC operations were compared with those from the NP operations.
RESULTS
There were 869 patients identified; 132 operations were performed PC and 737 were NP. The majority of operations included hernia repairs (46%), followed by cholecystectomies (35%), and intestinal procedures (19%). Overall, the PC operations did not differ from the NP operations with respect to complication rate (13.7% vs 13.5%, p = 0.93) or readmission within 30 days (5% vs 6%, p = 0.84). Additionally, multivariable logistic regression failed to identify an association between PC operations and the development of adverse outcomes. Follow-up was obtained for an average of 3 months.
CONCLUSIONS
Performance of general surgery operations the day after an overnight in-hospital trauma shift did not affect complication rates or readmission rates. At this time, there is no compelling evidence to mandate work-hour restrictions for attending general surgeons.
In 2003, the Accreditation Council for Graduate Medical Education (ACGME) instituted restrictions on resident physician work hours that collectively became known as the “80-hour work week.”1 As expected, these restrictions have posed considerable challenges for surgical training programs, particularly with respect to the provision of both sufficient educational experiences for residents and continuity of care for patients. In July 2011, in part as a result of ongoing concern over the effect of resident physician sleep deprivation on patient safety, the ACGME imposed tighter constraints, limiting continuous inhospital duty to a maximum of 16 hours for first-year resident physicians and 24 hours for more senior residents.2
Almost a decade after the implementation of resident work-hour limitations, the benefit of these restrictions with regard to both patient care and resident training remains disputed. Studies to date have generally focused on patient mortality,3,4 prevention of diagnostic and medication errors,5–7 resident emotional wellbeing,8,9 accidental percutaneous injuries,10,11 and motor vehicle accidents among resident physicians.12 It remains unclear whether there is, in fact, a measurable benefit from work-hour restrictions with respect to patient safety. In addition, the unintended consequences of both increased patient handovers and reduced clinical exposure for residents remain inadequately explored.13
To date, work-hour restrictions have not been imposed on attending physicians in the United States.14,15 The argument for resident work-hour restrictions may be similarly and rationally made for attending surgeons, given the known deleterious effects of sleep deprivation on cognitive function and dexterity. However, practical barriers to the implementation of surgeon work-hour rules include the logistical and economic constraints of the current surgical practice paradigm, as well as the established public expectation concerning the doctor-patient relationship with a single surgeon, rather than a group of surgeons doing shift work.
Although much remains unsettled concerning the effect of resident work-hour restrictions on patient safety, even less is known regarding the potential benefit of attending surgeon work-hour limitations on patient outcomes. At our medical center (a regional trauma center and safety net hospital), general surgery (both elective and emergency), trauma surgery, and surgical critical care are covered by a single surgical division. Resource constraints result in occasions in which the surgeons in this division are responsible for the elective operative schedule on days immediately after an overnight, in-hospital trauma shift. The purpose of this study was to investigate the effect of working an overnight trauma shift on the outcomes of general surgery operations performed the next day.
METHODS
Approval for this study was obtained from the Institutional Review Board at the University of Tennessee Health Science Center. The patient study base was derived from inpatient and outpatient surgical cases performed during a 3.5-year period (January 2006 to April 2009) at the Regional Medical Center in Memphis, TN. The Regional Medical Center includes a level 1 trauma center (Elvis Presley Memorial Trauma Center) that receives more than 12,000 annual visits. Approximately 500 trauma and/or emergency laparotomies are performed per year. Overnight attending trauma shifts are in-hospital from 5:00 PM to 7:00 AM and cover the trauma/general surgery patient census, which includes 40 surgical ICU beds, emergency department evaluation of all trauma patients, general surgery consultations, and surgical procedures.
For study purposes, cases for analysis were limited to inguinal and ventral hernias, cholecystectomies, and intestinal resections. To reduce the probability of creating a heterogeneous study cohort with a diluted incidence of postoperative complications, all other general surgery cases (such as excision of cutaneous or subcutaneous lesions, breast biopsy, etc.) were not abstracted. Hospital and clinic charts were reviewed for data regarding patient demographics, medical comorbidities, attending surgeon of record, operative management, follow-up, and outcomes. The State of Tennessee Health Department database was used to screen for statewide postoperative 30-day readmission for patients potentially lost to follow-up at the Regional Medical Center. Records of the attending surgeon trauma schedule were obtained from the University of Tennessee Health Science Center Department of Surgery. Operations that were performed by an attending surgeon on a day after an overnight trauma shift were categorized as post-call (PC) cases; all other cases were categorized as nonpost-call (NP).
The operations of interest included both elective and urgent procedures. All operations involving trauma were excluded. Urgent procedures included incarcerated or strangulated hernias, acute cholecystitis, bowel obstruction, gastrointestinal bleeding, and ischemic bowel. Hernia repairs included both laparoscopic and open repair of inguinal and ventral hernias (umbilical, epigastric, incisional, and abdominal wall reconstruction after planned ventral hernia). Cholecystectomies included laparoscopic, open, and laparoscopic converted to open removal of the gallbladder. Intestinal operations included any surgical procedure that involved resection of either large or small intestine, as well as colostomy or ileostomy creation or reversal.
Surgical complications were defined as any deviation from a normal postoperative course, including wound infection, seroma, perforation of gallbladder during cholecystectomy, intra-abdominal abscess, postoperative hemorrhage, development of seroma, wound dehiscence, injury to adjacent structure, and hollow organ leak. Wound infection, seroma, and gallbladder perforation were classified as “minor” complications and the remaining complications were classified as “major.” Readmission was defined as a patient requiring admission to any hospital in the state of Tennessee within 30 days of discharge from the primary hospital stay.
Statistical analysis was performed using Student’s t-test, chi-square, or Fisher’s exact test, where appropriate, to compare the relationship between PC operations and the development of complications or readmission within 30 days for demographic and characteristic variables. Variables that had a p value < 0.2 on univariable analysis were chosen as prospective covariates. Multivariable logistic regression analysis was used to perform the comparison of the 2 groups for the risk of complication after adjusting for potential confounders. Outcomes between the 2 groups were stratified by the attending surgeon. The multivariable logistic regression analysis was then repeated for subgroup analysis with respect to each type of surgical procedure (hernia repair, cholecystectomy, intestinal operation). Power analysis was performed to detect a difference in the complication rate of 4% between PC procedures and NP procedures to satisfy 80% power and 5% significance level with medium effect size assumption. A p value < 0.05 was considered statistically significant. Adjusted odds ratios (OR) and 95% confidence intervals (CI) were derived. Statistical computations were performed with SAS software, version 9.2 (SAS Institute).
RESULTS
Patient characteristics
From January 2006 to April 2009, 869 operations were performed that met inclusion criteria. The study population was 55% male, with an average age of 42 years. Thirteen percent of the cases were considered urgent. The majority of the cases involved hernia repairs (46%), followed by cholecystectomies (35%), and intestinal operations (19%). Two hundred sixty patients (30%) had at least 1 medical comorbidity and 8% had multiple medical comorbidities. The most common medical comorbidities were cancer and diabetes, which affected 7% and 6% of the study population, respectively. Other common associated medical disorders included coronary artery disease (3%), liver disease (3%), and congestive heart failure (2%).
The length of follow-up ranged from 0.1 to 50.3 months (average 2.91 months). Overall, the complication rate was 13% and the 30-day readmission rate was 6%. Wound infection was observed to have been the most common complication over the study period (Fig. 1). Fifty-nine percent of the complications were minor; the remaining 41% were major. Sixteen patients had multiple complications, and overall 30-day mortality was 0.3%.
Figure 1.
Breakdown of complications by type observed over study period. GB, gallbladder; Inj, injury; adj, adjacent.
Comparison of nonpost-call and post-call cohorts
Of the 869 operations, 737 (85%) were categorized as NP and 132 (15%) were categorized as PC. Table 1 shows a comparison of the clinical characteristics between these cohorts. The groups were clinically similar with respect to age, presence and type of medical comorbidity, minimally invasive technique, and type of operation performed. However, the PC cohort had a slightly higher proportion of male patients (62% vs 53%, p = 0.06) and a larger proportion of urgent cases (21% vs 11%, p = 0.001) compared with the NP cohort.
Table 1.
Comparison of Clinical Characteristics and Operations Between the Study Groups
| Characteristic | NP | PC | p Value |
|---|---|---|---|
| n | 737 | 132 | |
| Age, mean (SD), y | 41 (14) | 43 (14) | 0.18 |
| Male, n (%) | 393 (53) | 83 (62) | 0.06 |
| Presence of comorbidity, n (%) | 222 (30) | 38 (28) | 0.61 |
| CAD | 22 (3) | 4 (3) | 0.78 |
| Diabetes | 44 (6) | 7 (5) | 0.70 |
| Cancer | 51 (7) | 8 (6) | 0.72 |
| CHF | 15 (2) | 3 (2) | 0.99 |
| Renal disease | 7 (1) | 0 (0) | 0.37 |
| Liver disease | 22 (3) | 5 (4) | 0.59 |
| COPD | 15 (2) | 5 (4) | 0.21 |
| IBD | 4 (0.5) | 2 (1) | 0.56 |
| Steroids | 6 (1) | 3 (2) | 0.65 |
| HIV | 7 (1) | 4 (3) | 0.12 |
| Urgent procedure, n (%) | 81 (11) | 29 (21) | 0.001 |
| Laparoscopic procedure, n (%) | 228 (31) | 36 (27) | 0.42 |
| Hernia, n (%)* | 334 (45) | 67 (50) | 0.25 |
| Cholecystectomy, n (%) | 263 (35) | 42 (32) | 0.39 |
| Intestinal operation, n (%)* | 144 (20) | 24 (18) | 0.72 |
Continuous variables were compared using a Student’s t-test. Dichotomous variables were compared using chi-square analysis and Fisher’s exact test.
Five of the surgical procedures were a combination of both a hernia repair and a bowel operation.
CAD, coronary artery disease; CHF, congestive heart failure; IBD, inflammatory bowel disease; NP, non-postcall; PC, postcall.
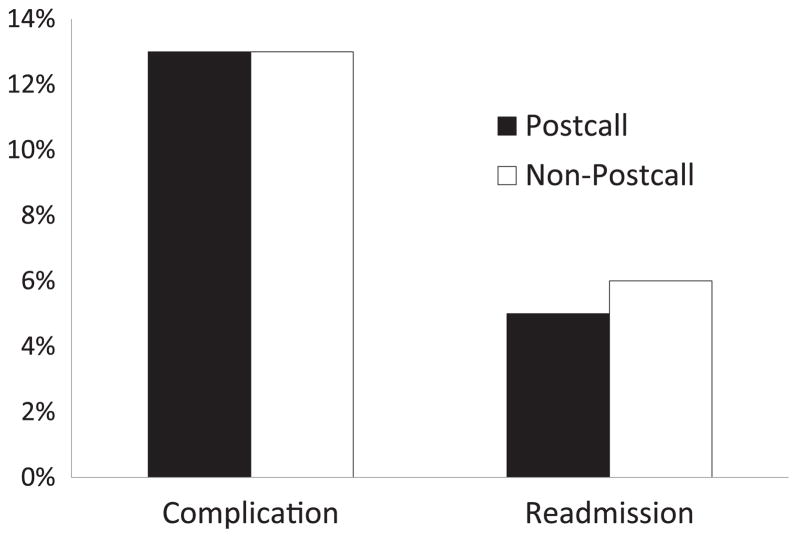
As illustrated in Figure 2, the groups did not differ with respect to complication rates (13.5% vs 13.7%, p = 0.93) or readmission rates (6% vs 5%, p = 0.84). In addition, there were no differences between groups with respect to the incidence of major (5.4% vs 6.9%, p = 0.83) or minor (8.1% vs 6.8%, p = 0.73) complications. There was also no difference observed between the 2 groups with respect to overall mortality (0% vs 0.4%, p = 0.99).
Figure 2.
Comparison of incidences of complications and readmission within 30 days between the study groups.
As demonstrated in Table 2, multivariable logistic regression failed to identify PC cases as an independent predictor of either the development of a complication or 30-day readmission after adjusting for age, sex, HIV status, and urgent operation. In order to account for attending surgeon experience level, the association between the PC cohort and complications was then analyzed after stratification by individual attending surgeon. Once again, neither the development of a complication (OR 0.86, CI 0.50 to 1.48) nor 30-day readmission (OR 0.68, CI 0.30 to 1.55) was associated with the PC cohort.
Table 2.
Multivariable Logistic Regression for Development of a Complication and Readmission
| Variable | Complication
|
Readmission
|
||
|---|---|---|---|---|
| Adjusted odds ratio | 95% CI | Adjusted odds ratio | 95% CI | |
| Post-call | 0.98 | 0.57–1.70 | 0.82 | 0.36–1.87 |
|
| ||||
| Age | 1.01 | 0.99–1.02 | 1.00 | 0.98–1.02 |
|
| ||||
| Sex | 0.90 | 0.60–1.34 | 1.16 | 0.65–2.07 |
|
| ||||
| History of HIV | 3.00 | 0.90–9.95 | 3.00 | 0.64–14.00 |
|
| ||||
| Urgent | 1.26 | 0.72–2.21 | 1.08 | 0.47–2.51 |
Although the groups did not differ with respect to development of complications or readmission, morbidity rates may have varied depending on the type of operation performed. Therefore, subgroup analysis was performed as follows.
Hernia repair: Nonpost-call vs post-call
A comparison of the clinical characteristics and outcomes between the NP hernia repairs and the PC hernia repairs are shown in Table 3. Although these subgroups were similar with respect to most characteristics including type of hernia repair, a larger proportion of the PC hernia subgroup comprised urgent cases (19% vs 7%, p = 0.001). Both complication rates (11% vs 13%, p = 0.69) and readmission rates (5% vs 8%, p = 0.45) were similar. After adjusting for sex, history of COPD, type of hernia repair, and urgency of operation, multivariable logistic regression demonstrated that neither the development of a complication (OR 0.82, CI 0.33 to 2.02) nor readmission (OR 0.32, CI 0.04 to 2.72) was associated with the PC hernia subgroup.
Table 3.
Comparison of Hernia Operations Based on Study Group
| Characteristic | NP | PC | p Value |
|---|---|---|---|
| n | 334 | 67 | |
| Age, mean (SD), y | 42 (14) | 44 (13) | 0.26 |
| Male, n (%) | 231 (70) | 54 (81) | 0.07 |
| Patients with comorbidity, n (%) | 67 (20) | 13 (19) | 0.99 |
| CAD | 17 (5) | 1 (2) | 0.49 |
| Diabetes | 13 (4) | 4 (6) | 0.52 |
| Cancer | 3 (1) | 1 (2) | 0.99 |
| CHF | 7 (2) | 2 (3) | 0.68 |
| Renal disease | 3 (1) | 0 (0) | 0.99 |
| Liver disease | 7 (2) | 3 (5) | 0.22 |
| COPD | 7 (2) | 4 (6) | 0.09 |
| HIV | 2 (0.5) | 1 (2) | 0.31 |
| Urgent procedure, n (%) | 23 (7) | 13 (19) | 0.001 |
| Inguinal hernia, n (%) | 167 (50) | 40 (60) | 0.18 |
| Ventral hernia, n (%) | 167 (50) | 27 (40) | 0.18 |
| Laparoscopic procedure, n (%) | 20 (6) | 5 (8) | 0.78 |
| Complication, n (%) | 44 (13) | 7 (11) | 0.69 |
| Readmission, n (%) | 27 (8) | 3 (5) | 0.45 |
Continuous variables were compared using a Student’s t-test. Dichotomous variables were compared using chi-square analysis and Fisher’s exact test.
CAD, coronary artery disease; CHF, congestive heart failure; NP, non-postcall; PC, postcall.
Cholecystectomy: Nonpost-call vs post-call
Table 4 demonstrates a comparison of the clinical characteristics and outcomes between the NP cholecystectomies and the PC cholecystectomies. Again, the subgroups did not differ with respect to most characteristics, including the proportion of cases performed using laparoscopy and conversion to an open procedure. Although the groups had equal proportions of patients with medical comorbidities, the NP cholecystectomy subgroup had more patients with diabetes mellitus (11% vs 0%, p = 0.02) compared with the PC cholecystectomy subgroup. Furthermore, the PC cholecystectomy subgroup seemed to trend toward a higher complication rate (17% vs 10%, p = 0.19) and readmission rate (7% vs 2%, p = 0.06) compared with the NP cholecystectomy subgroup. However, multivariable logistic regression demonstrated that neither development of a complication (OR 1.51, CI 0.60 to 3.82) nor readmission (OR 4.73, CI 0.84 to 26.6) was associated with the PC cholecystectomy subgroup after adjusting for sex, HIV status, and diabetes mellitus.
Table 4.
Comparison of Cholecystectomies Based on Study Group
| Characteristic | NP | PC | p Value |
|---|---|---|---|
| n | 263 | 42 | |
| Age, mean (SD), y | 38 (14) | 40 (14) | 0.36 |
| Male, n (%) | 52 (20) | 12 (28) | 0.19 |
| Patients with comorbidity, n (%) | 76 (29) | 12 (29) | 0.97 |
| CAD | 5 (2) | 1 (2.5) | 0.59 |
| Diabetes | 29 (11) | 0 (0) | 0.02 |
| Cancer | 5 (2) | 1 (2) | 0.99 |
| CHF | 3 (1) | 0 (0) | 0.99 |
| Renal disease | 5 (2) | 0 (0) | 0.99 |
| Liver disease | 11 (4) | 2 (5) | 0.67 |
| COPD | 3 (1) | 0 (0) | 0.99 |
| IBD | 0 (0) | 0 (0) | |
| Steroids | 3 (1) | 0 (0) | 0.99 |
| HIV | 5 (2) | 2 (5) | 0.19 |
| Urgent procedure, n (%) | 34 (13) | 5 (12) | 0.99 |
| Laparoscopic procedure, n (%) | 205 (78) | 31 (74) | 0.51 |
| Laparoscopic converted to open, n (%) | 37 (14) | 6 (14) | 0.99 |
| Complication, n (%) | 26 (10) | 7 (17) | 0.19 |
| Readmission, n (%) | 5 (2) | 3 (7) | 0.06 |
Continuous variables were compared using a Student’s t-test. Dichotomous variables were compared using chi-square analysis and Fisher’s exact test.
CAD, coronary artery disease; CHF, congestive heart failure; NP, non-postcall; PC, postcall.
Intestinal operation: Nonpost-call vs post-call
Comparison of the clinical characteristics and outcomes between the NP bowel operations and the PC bowel operations is demonstrated in Table 5. Once again, the groups had equal proportions of patients with medical comorbidities. However, the PC intestinal subgroup had a larger proportion of patients with coronary artery disease (8% vs 1%, p = 0.05) as well as more urgent cases (46% vs 17%, p = 0.001) compared with the NP intestinal subgroup. The subgroups were similar with respect to complication rate and readmission rate. After adjusting coronary artery disease, diabetes mellitus, and urgency of procedure, multivariable logistic regression failed to identify intestinal operations being performed PC as an independent predictor of either a complication (OR 0.81, CI 0.25 to 2.68) or readmission (OR 0.35, CI 0.04 to 2.89).
Table 5.
Comparison of Intestinal Operations Based on Study Group
| Characteristic | NP | PC | p Value |
|---|---|---|---|
| n | 144 | 24 | |
| Age, mean (SD), y | 47 (14) | 46 (17) | 0.95 |
| Male, n (%) | 110 (77) | 17 (71) | 0.60 |
| Patients with comorbidity, n (%) | 79 (55) | 13 (54) | 0.99 |
| CAD | 1 (1) | 2 (8) | 0.05 |
| Diabetes | 6 (4) | 3 (13) | 0.09 |
| Cancer | 45 (31) | 5 (21) | 0.47 |
| CHF | 7 (5) | 1 (4) | 0.99 |
| Renal disease | 1 (1) | 0 (0) | 0.99 |
| Liver disease | 6 (4) | 1 (4) | 0.99 |
| COPD | 7 (5) | 1 (4) | 0.99 |
| IBD | 4 (3) | 1 (4) | 0.54 |
| Steroids | 6 (4) | 2 (8) | 0.32 |
| HIV | 3 (2) | 1 (4) | 0.54 |
| Urgent procedure, n (%) | 24 (17) | 11 (46) | 0.001 |
| Complication, n (%) | 32 (22) | 5 (22) | 0.99 |
| Readmission, n (%) | 16 (11) | 1 (4) | 0.47 |
Continuous variables were compared using a Student’s t-test. Dichotomous variables were compared using chi-square analysis and Fisher’s exact test.
CAD, coronary artery disease; CHF, congestive heart failure; NP, non-postcall; PC, postcall.
DISCUSSION
A sense of duty and commitment to one’s patients has been central to the identity of the surgeon from time immemorial. Patient perception of surgeons has, therefore, naturally evolved to include expectations of personal attention and availability from preoperative consultation through postoperative follow-up. In recent years, however, patient safety issues with regard to medical error have garnered much public interest, with particular focus on an alleged connection between medical error and physician fatigue. This concern, in great part led to the imposition of resident work hours by the ACGME. The general public demonstrates support for work hour limits for all surgeons, not just those in training, with 84% in support of work limits for attending surgeons and 82% stating that they would reschedule elective surgery if they knew their surgeon had less than 4 hours sleep the night before the procedure.16 Unfortunately, expectations of surgeon attention and availability and concern regarding surgeon fatigue may often be at odds. The economic and logistic realities of current surgical practice necessitate that, at times, the typical surgeon will be faced with scheduled procedures, office visits, and/or inpatient care duties after a sleepless night taking care of a surgical emergency.
Although it may be assumed that both surgeon and patient would prefer that the surgeon be well rested before embarking on a surgical procedure, it remains unclear as to whether operative outcomes are, in fact, adversely affected by surgeon fatigue. Surgeons rely on a combination of cognitive decision-making and fine motor skill on a daily basis, both of which fatigue has the potential to alter. Earlier studies investigating the impact of sleep deprivation on surgical residents failed to demonstrate a decline in cognitive function with less sleep.17–19 However, 2 recent reports using laparoscopic simulators showed an increase in technical errors and procedure time in sleep-restricted surgeons in training.20,21 These results are notable, but these data are also specific to residents in training. Relative experience, conditioning to performing cognitive tasks in the setting of sleep deprivation, and superior muscle memory may counteract the effects of fatigue on technical performance in attending surgeons.
In a recent study, Rothschild and colleagues15 retrospectively examined the association between sleep opportunities for attending surgeons and obstetricians/gynecologists and the development of complications concerning procedures performed the next day.15 Sleep opportunity was calculated as the time between the end of an overnight operation and the beginning of a procedure the next day. The authors found an increased risk of developing complications in procedures performed with sleep opportunities of 6 hours or less compared with those with sleep opportunities of more than 6 hours (OR 1.72, 95% CI 1.02 to 2.89). Although intriguing, the results stem from a heterogeneous study cohort that consisted of several different specialties, including obstetrics/gynecology, general surgery, orthopaedic surgery, and cardiac surgery, making it difficult to extrapolate any conclusions for one particular discipline.
An earlier study by Ellman and associates22 focused on outcomes in cardiothoracic surgery related to surgeon sleep opportunity. Sleep deprivation was defined as starting a case between 10:00 PM and 5:00 AM the previous evening or ending a case between 11:00 PM and 7:30 AM. The authors found that sleep deprivation did not increase mortality rates or complication rates related to cardiac surgical procedures and concluded that work-hour restrictions were unnecessary for trained cardiac surgeons.
This study concerns general surgery procedures limited specifically to hernia repairs, cholecystectomies, and bowel operations, and corroborates the observations of Ellman and coworkers.22 In this study, the procedures of interest were started between 8:00 AM and 4:00 PM. All of the surgeons were board certified, with accredited fellowships in surgical critical care. Overall complication rates and readmission rates did not differ between operations performed after an overnight trauma shift and the control procedures. Although no disparities were found in outcomes, it is notable that the cumulative postresidency experience varied for the involved surgeons from 2 to 25 years. To adjust for the possibly confounding variable of surgeon experience, we stratified by individual surgeon, and the lack of difference between the PC and NP cohorts persisted with respect to complications and readmission.
Several limitations concerning this study are noteworthy. This study concerns outcomes from a single academic institution. Although the attending surgeons may have been in the hospital overnight, all other participants in the operations under study, particularly the surgical residents, had no clinical responsibilities the night before surgery. Therefore, the results of this study may not be generalizable to other practice settings, particularly in the nonteaching setting. It is also notable that the amount of sleep obtained by the attending surgeon, if any, was not quantified. From our collective experience with overnight trauma shifts at the Regional Medical Center at Memphis, we know well that these shifts rarely afford any opportunity for rest, and if sleep opportunities do present, they are often fragmented and amount to less than a few hours. It is highly unlikely that more than 6 hours of sleep were obtained in a night shift over the time period of this study, but this cannot be stated with certainty. Additionally, the operations of interest were limited to hernia repairs, cholecystectomies, and bowel operations because these are commonly performed procedures with reasonable potential for complication. Many other procedures were performed over the time period of study, and these procedures likely have varying risks of complications that may or may not be affected by sleep deprivation. It is presumable that a relatively simple operation, such as the excision of a subcutaneous lipoma, would be more resistant to the effect of sleep deprivation than a relatively more complicated and less often performed procedure such as pancreaticoduodenectomy. Finally, statistical power was sufficient for the primary analysis, but the sample sizes in the subgroup analyses were probably not large enough to demonstrate a significant difference in outcomes, if, in fact, one was present.
CONCLUSIONS
In an ideal world, all surgeons would have adequate recovery time to recuperate from nighttime work and avoid operating in the setting of sleep deprivation. To achieve this goal, the current practice model and culture of surgery, along with the public’s expectations of surgical care, would need to undergo significant changes. These changes would, by necessity, include expansion of the surgeon work force, which is unrealistic, or public acceptance of longer wait times and flexibility with respect to elective procedures. Before embarking on any significant reshaping of surgical practice in the United States, the question of whether there is a de facto patient benefit to surgeon work-hour restriction must be addressed. The results of this study suggest that at this time, there is no compelling evidence that work-hour restrictions for attending general surgeons would improve operative outcomes.
Abbreviations and Acronyms
- NP
nonpost-call
- OR
odds ratio
- PC
post-call
Footnotes
Disclosure Information: Nothing to disclose.
Presented at the Southern Surgical Association 124th Annual Meeting, Palm Beach, FL, December 2012.
Author Contributions
Study conception and design: Sharpe, Weinberg, Magnotti, Yoo, Zarzaur
Acquisition of data: Sharpe, Cullinan, Hendrick
Analysis and interpretation of data: Sharpe, Weinberg, Magnotti, Nouer, Yoo, Croce
Drafting of manuscript: Sharpe, Weinberg, Magnotti
Critical revision: Nouer, Fabian, Croce
References
- 1.Statement of Justification/Impact for the Final Approval of Common Standards Related to Resident Duty Hours. Chicago: Accreditation Council for Graduate Medical Education; 2003. [Google Scholar]
- 2.Accreditation Council for Graduate Medical Education. Duty Hours: ACGME Standards. 2011 Available at: http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramResources/Common_Program_Requirements_07012011%5b1%5d.pdf.
- 3.Afessa B, Kennedy CC, Klarich KW, et al. Introduction of a 14-hour work shift model for housestaff in the medical ICU. Chest. 2005;128:3910–3915. doi: 10.1378/chest.128.6.3910. [DOI] [PubMed] [Google Scholar]
- 4.Bhavsar J, Montgomery D, Li J, et al. Impact of duty hours restrictions on quality of care and clinical outcomes. Am J Med. 2007;120:968–974. doi: 10.1016/j.amjmed.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 5.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–1848. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 6.Gottlieb DJ, Parenti CM, Peterson CA, Lofgren RP. Effect of a change in house staff work schedule on resource utilization and patient care. Arch Intern Med. 1991;151:2065–2070. [PubMed] [Google Scholar]
- 7.Barger LK, Ayas NT, Cade BE, et al. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med. 2006;3:e487. doi: 10.1371/journal.pmed.0030487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cao CG, Weinger MB, Slagle J, et al. Differences in day and night shift clinical performance in anesthesiology. Hum Factors. 2008;50:276–290. doi: 10.1518/001872008X288303. [DOI] [PubMed] [Google Scholar]
- 9.Kiernan M, Civetta J, Bartus C, Walsh S. 24 hours on-call and acute fatigue no longer worsen resident mood under the 80-hour work week regulations. Curr Surg. 2006;63:237–241. doi: 10.1016/j.cursur.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 10.Ayas NT, Barger LK, Cade BE, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA. 2006;296:1055–1062. doi: 10.1001/jama.296.9.1055. [DOI] [PubMed] [Google Scholar]
- 11.Parks DK, Yetman RJ, McNeese MC, et al. Day-night pattern in accidental exposures to blood-borne pathogens among medical students and residents. Chronobiol Int. 2000;17:61–70. doi: 10.1081/cbi-100101032. [DOI] [PubMed] [Google Scholar]
- 12.Barger LK, Cade BE, Ayas NT, et al. Harvard Work Hours, Health, and Safety Group. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125–134. doi: 10.1056/NEJMoa041401. [DOI] [PubMed] [Google Scholar]
- 13.Reed DA, Fletcher KE, Arora VM. Systematic review: association of shift length, protected sleep time, and night float with patient care, residents’ health, and education. Ann Intern Med. 2010;153:829–842. doi: 10.7326/0003-4819-153-12-201012210-00010. [DOI] [PubMed] [Google Scholar]
- 14.Hyman NH. Attending work hour restrictions: is it time? Arch Surg. 2009;144:7–8. doi: 10.1001/archsurg.2008.518. [DOI] [PubMed] [Google Scholar]
- 15.Rothschild JM, Keohane CA, Rogers S, et al. Risks of complications by attending physicians after performing nighttime procedures. JAMA. 2009;302:1565–1572. doi: 10.1001/jama.2009.1423. [DOI] [PubMed] [Google Scholar]
- 16.Berg DB, Engel AM, Saba A, Hatton EK. Differences in public belief and reality in the care of operative patients in a teaching hospital. J Surg Educ. 2011;68:10–17. doi: 10.1016/j.jsurg.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 17.Reznick RK, Folse JR. Effect of sleep deprivation on the performance of surgical residents. Am J Surg. 1987;154:520–525. doi: 10.1016/0002-9610(87)90269-8. [DOI] [PubMed] [Google Scholar]
- 18.Deaconson TF, O’Hair DP, Levy MF, et al. Sleep deprivation and resident performance. JAMA. 1988;260:1721–1727. [PubMed] [Google Scholar]
- 19.Bartle EJ, Sun JH, Thompson L, et al. The effects of acute sleep deprivation during residency training. Surgery. 1988;104:311–316. [PubMed] [Google Scholar]
- 20.Eastridge BJ, Hamilton EC, O’Keefe GE, et al. Effect of sleep deprivation on the performance of simulated laparoscopic surgical skill. Am J Surg. 2003;186:169–174. doi: 10.1016/s0002-9610(03)00183-1. [DOI] [PubMed] [Google Scholar]
- 21.Taffinder NJ, McManus IC, Gul Y, et al. Effect of sleep deprivation on surgeons’ dexterity on laparoscopy simulator. Lancet. 1998;352:1191. doi: 10.1016/s0140-6736(98)00034-8. [DOI] [PubMed] [Google Scholar]
- 22.Ellman PI, Law MG, Tache-Leon C, et al. Sleep deprivation does not affect operative results in cardiac surgery. Ann Thorac Surg. 2004;78:906–911. doi: 10.1016/j.athoracsur.2004.04.006. [DOI] [PubMed] [Google Scholar]