Abstract
Objective
To evaluate long-term change in fruit and vegetable intake following a group randomized trial of worksites.
Methods
Medium-sized blue-collar businesses in the Seattle metropolitan area were recruited. Intake was assessed using serial cross-sectional samples of current workforce at 3 time points. The multilevel 18-month intervention involved partnership with the companies. Long-term follow-up was at 4.4 years postbaseline. Statistical analysis used general linear models, adjusting for worksite random effects.
Results
Initially, 45 worksites were randomized, with 29 agreeing to participate in a new study. Fruits and vegetable intake increased, with larger sustained changes in the intervention worksites, resulting in a long-term differential change of 0.25 servings per day, 95% confidence interval (0.09 to 0.40).
Conclusions
Intervention sustained small effects at 4 years, including 2 years with no contact. Although effects were not large, this low-intensity intervention approach could provide an important public health model.
Keywords: Intervention evaluation studies, behavior change persistence, food, fruits and vegetables, long-term effects
Information on long-term behavior change in community settings is sparse. Intervention evaluation studies are usually interested in answering one primary question: Does the intervention have an effect? Once the efficacy or effectiveness of an intervention has been established, related questions may arise that are important to the community: Will the effect last? Will long-term behavior change be seen? Will the intervention program endure? Given the role of increased fruit and vegetable intake in chronic disease prevention,1,2 the importance of identifying effective strategies for increasing fruit and vegetable consumption is clear. Indeed, the overall goal of any successful community-based health promotion program is that the behavior change be sustained indefinitely. Our series of worksite studies are able to contribute answers to these questions as they apply to dietary behavior change.
Surveys of food intake nationwide have shown that not all groups have reached recommended levels of fruit and vegetable intake, even at the 5 servings per day level that was recommended explicitly 20 years ago.3 During the 1990s, several demonstration and research programs were instituted, and the surveys showed average intake of fruits and vegetables rose to about 3.4 servings per day.4 Unfortunately this increase was markedly less among people with no more than a high school education, particularly men,5, 6 and national rates declined somewhat around 2000.4 People in low socioeconomic status groups are at increased risk for many chronic diseases,7 and the degree to which healthful diets are adopted by these groups appears to be lower than average.8 These observations reinforce the importance of targeting population groups with low socioeconomic status as well as of maintaining whatever changes in fruit and vegetable (F&V) intake behavior have been made.
Behavior change is a gradual process, especially in the context of relatively low-intensity interventions. At least one study showed evidence of larger changes at 12 months compared to at 3 months when the intervention was a single occasion, with delivery of a self-help manual.9 Once behavior change has started, many studies have shown that continued intervention activities are necessary to maintain behavior change.10–12 This is particularly true in intensive intervention studies.11, 13 Nonetheless, the ability to sustain activities initiated in a research context has not been demonstrated in most community intervention studies, and long-term effects of low-intensity interventions are lacking.
Worksites provide an ideal environment to promote and sustain dietary change because they function as small communities and members can encourage and support increased fruit and vegetable consumption as a means of improving one’s health.14–16 Worksites offer access to large populations as over 62% of the US population is employed.17 For employees, worksite-located activities are convenient to attend and often less costly than similar activities outside of the workplace. Further, worksites offer the opportunity to deliver intervention messages that encourage simple steps to behavior change.
In this paper, we report the long-term effects of an intervention to increase fruit and vegetable intake among employees of blue-collar and service industry worksites. We conducted a group randomized trial of worksites, followed later by a new follow-up study. Because of these 2 related studies, we were able to evaluate the long-term effects of our intervention more than 2 years after the active intervention was completed.
METHODS
Study Population and Recruitment
Small to medium-sized worksites in the general Seattle area that had standardized industrial classification (SIC) codes consistent with large proportions of blue-collar or service worksites were identified in 2000–2001 using a purchased list. From this sampling frame worksites were recruited for a Seattle 5 a Day intervention trial and randomized to intervention or comparison condition. A new continuation of that study offered the opportunity to evaluate long-term change in fruit and vegetable behavior in response to a 5 a Day intervention program.
The Seattle 5 a Day Study recruited worksites from Skagit, King, and Pierce counties in Washington State, with the stipulation that they be able to be reached within an hour’s driving time from the study center. A majority of the worksites were located in the Seattle metropolitan area. The SIC codes included were 20–39, manufacturing; 40–49, transportation, utilities; 70–79, personal services; 88–89, household & miscellaneous services; and 99, nonclassifiable worksites. All worksites underwent a 2-stage telephone screening process to determine eligibility prior to a final face-to-face recruitment meeting. Eligibility criteria included company size of between 50 and 150 employees, no established health promotion programs, and no on-site cafeteria services available. In addition worksites were required to have 70% English-speaking population and attrition rate of less than 20% per year; the company had to be in existence for a minimum of 3 years and have no more than 2 locations. The 5 a Day intervention started in worksites between 2000 and 2002.
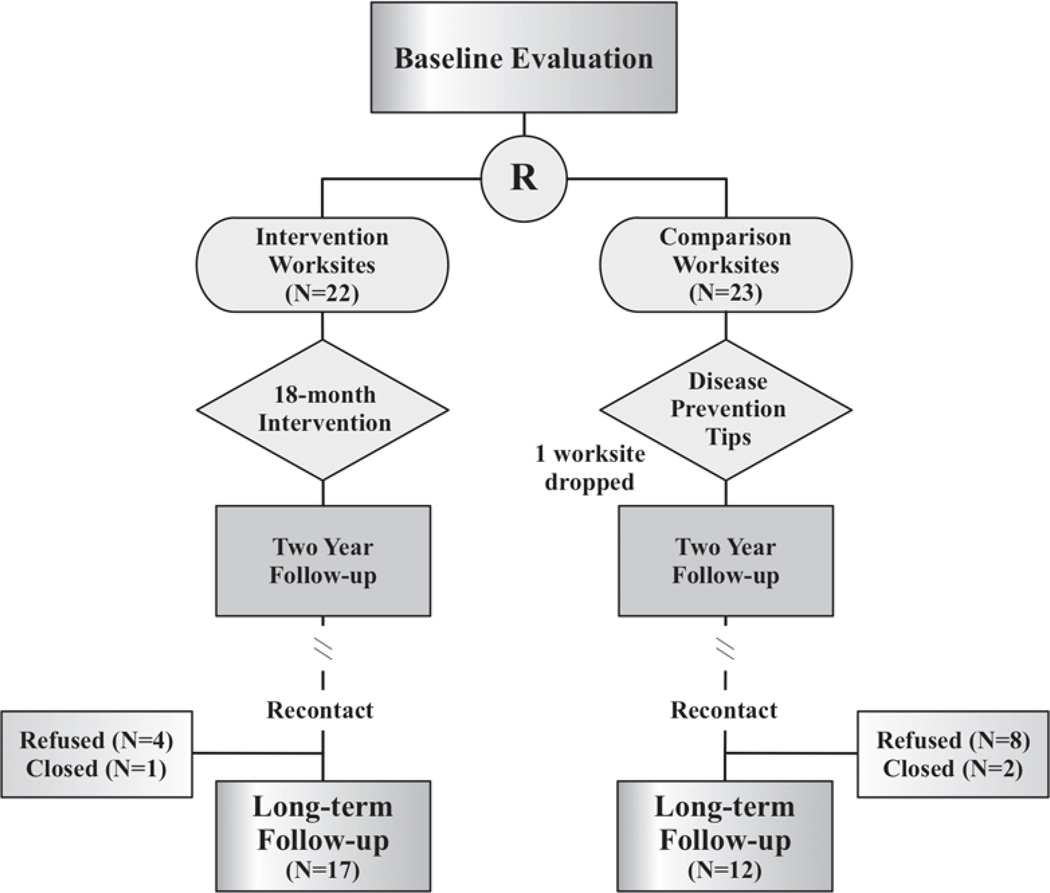
In 2005 to 2006, the worksites were re-recruited for a follow-up study. All 44 of the original Seattle 5 a Day worksites that completed the first study were sent a recruitment letter detailing the new study and encouraging worksites to participate. After the letter was received, a face-to-face meeting was arranged to explain the study in further detail and provide the worksite with all necessary paperwork for the new study. Of the 44 original Seattle 5 a Day worksites, 29 worksites signed consent to participate in the new study. Of the 29 worksites, 17 were original intervention worksites (Group 1), and 12 were original comparison worksites (Group 2). The study design is shown in Figure 1. As is apparent, a higher proportion of intervention worksites than of control worksites were willing and able to participate in the new study. Both the original Seattle 5 a Day study and the new study were reviewed by the institutional review board (IRB) of our institution and approved for implementation.
Figure 1.
Design of Seattle 5 a Day Showing Long-term Follow-up After Recontact for New Study
Assessment
As part of the run-in period, companies were asked to complete a company questionnaire. Three rounds of surveys were administered: at baseline, at 2-year follow-up, and at long-term follow-up (at the beginning of the new study). The surveys were administered to serial cross-sections of employees working for the participating companies at the time of the assessments. As part of the original processes for the Seattle 5 a Day in blue-collar and service industry worksites, each worksite was required to provide access to names of all employees within the worksite who were full- or part-time permanent employees. In that study, each employee was provided a unique study identification number that provided confidentiality for collecting data from the baseline survey. Although voluntary, each employee was encouraged to complete the baseline survey. A small monetary token, worksite-wide raffles, or study-catered “coffee breaks” were provided as incentives. All employees received a survey packet that included a letter from the study principal investigator, a support letter from the worksite CEO, owner or HR management, information regarding the importance of the study and the questionnaire. Depending on the demands of the worksite, 2 main delivery options for the questionnaire were provided. These were a proctored group administration or survey packets delivered to each department supervisor to hand out to the employee or to attach with the employee paycheck. Hand-delivering the packets and attaching to paychecks yielded a lower survey response rate as the employee had to complete the survey on his or her own time. For these methods, each survey packet included a postage-paid return envelope for returning the completed questionnaire directly to the research center. For all methods of survey administration, second and third administrations of the survey packet were either hand-delivered to the employee or attached to the employee paycheck.
The questionnaire consisted of 46 questions pertaining to individual dietary behaviors, stages of change, taste preferences and perceptions, barriers to eating fruits and vegetables, autonomy in meal preparation, and social support. The survey took 15 minutes on average to complete. At the 2-year anniversary of baseline the worksite again provided names of employees for the purpose of a second cross-sectional survey of employees, and this occurred again after we had recontacted the worksites, at the beginning of the new study. For original control sites, this third round of surveys used shorter questionnaires. This is because the questions used on the shorter survey were the same as those on the baseline survey, but there were fewer of them. These were number of servings of fruits and vegetables consumed daily, barriers to eating fruits and vegetables, and demographic questions. On average the short survey took 10 minutes to complete.
Measures
The main outcome measure was fruit and vegetable intake, as assessed by a single question asked at the beginning of each of the surveys. To reduce the information bias that might arise from intervention worksite employees’ increased awareness of portion size conventions at follow-up, we included a small set of pictures of common portion sizes on the survey itself. This question has been found to be correlated (0.62) with the more commonly used set of 7 food frequency fruit and vegetable questions used in the NCI 5 a Day studies18 and to be responsive to change.19
The secondary outcome measure is stage of readiness to increase fruit and vegetable intake. The 5 questions and corresponding algorithm were used in the Seattle 5 a Day worksite trial in worksites with cafeterias,19 where the progression of stage from precontemplation to maintenance was associated with increasing fruit and vegetable intake at baseline in that study. The measure also was demonstrated to be responsive to change, with intervention worksites having a higher proportion of employees at follow-up in action or maintenance compared to the control worksites.
Characteristics of the worksites were mostly determined from the company questionnaire, which was completed prebaseline by the company contact or head of human resources. This included percent blue collar, percent employees leaving the company each year. The standardized industrial code classification used was the one provided on the purchased company list. A qualitative evaluation of management support came from the key informant interviews, and turnover in company contact person was abstracted from research coordinator notes.
Intervention
The Seattle 5 a Day intervention was designed to increase fruit and vegetable consumption among all employees at the worksite. A required component of the intervention was the establishment of a worksite Employee Advisory Board (EAB). Members for the EAB were recruited from various sectors of the worksite so that it represented the entire worksite. The EAB was responsible for adapting the intervention menu to the specific worksite. Further, the EAB assisted in the implementation of activities.
The intervention included a formalized schedule of worksite-wide events interspersed with tailored newsletter mailings to employees. The intervention was based on and had many components of our first Seattle 5 a Day study, described in detail elsewhere.19,20 The intervention, based on the “stages of change” or the transtheoretical model,21 was designed to occur in 4 phases. Based on our earlier study,19 we expected employees to range from pre-contemplation—not even thinking of eating more fruits and vegetables—to maintaining an increased level of fruit and vegetable intake, with employees at each stage of readiness to change and we designed the intervention activities to move employees from their existing stage to subsequent stages. The intervention phases represented the transitions between neighboring stages of readiness to change.20 Thus, a first activity in worksites was the creation of an awareness campaign to get employees to think about eating more fruits and vegetables (contemplation stage). Posters were distributed throughout the worksite; these advertised a soon-to-come program at the worksite. The idea was to encourage motivation on the part of employees so they would attend a worksite-wide “kick-off” event. Events to move employees from contemplation to preparation included the teaching of simple skills such as what a serving size was, and ways to increase consumption of fruits and vegetables at specific meals. In keeping with moving people gradually through stages of change, we broke complicated activities down into simple steps that could easily be taught in the worksite before continuing with more complex steps (which was done in the action phase). This was accomplished through the positioning of table tents throughout worksite places, new posters, and taste tests held in the worksite. Moving from preparation to action required more complex skills. We prepared and disseminated to all employees a manual on how to increase fruits and vegetables consumption. We also held cooking demonstrations and prepared and distributed brown bag lunches with 4 servings of fruits and vegetables. Finally, to encourage maintenance, we held company-wide challenges and events to foster healthy eating at all company activities. We also encouraged the use of farmers’ markets, and we distributed recipes for cooking meals with more fruits and vegetables. All worksite-wide events were implemented in partnership with the EAB.
In addition, we produced 4 tailored employee newsletters that were sent to employees throughout the intervention period. The newsletters were a combination of theme-related sections and tailored messages, using information from baseline questionnaire responses (for the first newsletter, and to fill in information for the subsequent newsletters), and information provided on short postcard surveys that respondents mailed back to the study institution (for the subsequent newsletters). The postcards contained 4 questions sent with the newsletters, and were returned by about 40% of the employees. These newsletters showed employees where they were in terms of stages of change, consumption of fruits and vegetables compared to the rest of the worksite, the barriers they had in terms of eating more fruits and vegetables, and ways to sustain their consumption of fruits and vegetables. The tailoring was done through computerized algorithms based on the individual employees’ responses to the questions about stage, consumption, and barriers to change.
Statistical Methods
Choice of statistical method was dictated by the following considerations: The unit of randomization assignment in this group randomized trial is the worksite. Worksite effects result in correlated response values (fruit and vegetable intake and stage of readiness to change) for individuals from the same worksite. Responses at different time points are also assumed to be correlated. Finally, though the total number of individuals is large (n=2018 at baseline and n=1579 at long-term follow-up), the number of worksites available for the analysis of long-term effects of the intervention is only 29.
General linear mixed models were used, with worksite-level period (baseline or long-term follow-up) random effects, and fixed effects for intervention arm, assessment time, the time by arm interaction, and within-worksite lag time between administration of the baseline survey and the survey at long-term follow-up. Variances of the random effects for both survey periods were assumed to be the same and to have positive covariance. Similarly, residual variances were assumed to be the same for both periods, and to be positively correlated for individuals observed at both time points. Adjustment for lag time between survey administrations was employed to account for variation across worksites arising from different spacings between waves of recruitment for the Seattle 5 a Day study and for the new study.
F&V servings and stage of readiness for change from both baseline and long-term follow-up surveys were response variables. F&V servings (after adding a constant of 1) were transformed using a natural logarithm. The SAS MIXED procedure was employed to estimate parameters for F&V servings as the response. The SAS GLIMMIX procedure was used to estimate parameters for the binary response stage of readiness for change. Estimated mean values for each treatment arm at baseline and long-term follow-up were back-transformed to the original scale. Similarly differences in the means and their confidence intervals were back-transformed for reporting purposes.
Secondary analyses explored whether worksite level factors are related to the long-term effects of the Seattle 5 a day intervention. Mixed linear models as described above were fit, with additional terms to assess whether or not worksite characteristics modified the intervention effect. Worksite characteristics examined included factors evaluated prior to the baseline survey: industry classification (service or manufacturing), worksite size, percent blue collar, percent turnover, management support for the baseline survey; and an additional variable describing the worksite that was obtained over time from both intervention and control worksites. This latter variable was whether the contact person changed during the course of the study. All worksite characteristics were constructed as binary variables.
Key Informant Data
Key informant interviews were conducted at long-term follow-up in Group 1 companies. Approximately 5 key informants were identified at each company. They were selected based on the following criteria: Employed at worksite for at least 24 months; interact throughout the worksite; critically evaluate and address situations; good communication skills; and willing to participate. Thus, they were intended to be key players in the company. They were asked a series of open-and closed-ended questions related to the current status of the Seattle 5 a Day program in their company. The responses from the interviews were transcribed into an excel spreadsheet. Three questions were used to examine intervention worksites as to whether aspects of the intervention were still continuing. The 3 questions included evidence of a) ongoing inclusion of health related messages in regular communication systems, b) ongoing conduct of 5 a Day activities , and c) visible promotional 5 a Day materials. These data were treated descriptively.
RESULTS
As has been mentioned, a higher proportion of worksites in the Seattle 5 a Day intervention group (Group 1) agreed to participate in the new study than did companies in the comparison group (Group 2), as shown in Table 1. The differential agreement rate was most pronounced in the manufacturing companies. Demographic characteristics of the companies were similar between the intervention and comparison group companies. As shown in Table 2, about equal numbers of employees were aged 25 to 39 years as were aged 40 to 54 years, together forming more than 75% of the workforce. Comparison companies had a slightly higher percentage of female employees (37.8%) than did the intervention companies (27.5%), and less than 30% had no education beyond high school in both intervention arms.
Table 1.
Standardized Industrial Classification of Worksites: Randomized to Seattle 5 a Day with Subset Continuing Participation in EAT 5 for LIFE
| Intervention |
Comparison |
|||||
|---|---|---|---|---|---|---|
| SIC | Randomized | Continuing | %continuing | Randomized | Continuing | %continuing |
| Manufacturing | 15 | 11 | 73% | 11 | 3 | 27% |
| Service | 4 | 3 | 75% | 8 | 6 | 75% |
| Transportation or Other | 3 | 3 | 100% | 4 | 3 | 75% |
| Total | 22 | 17 | 77% | 23 | 12 | 52% |
Table 2.
Demographic Characteristics of Intervention and Comparison Worksites at Baseline: Mean (SD) of Worksite Means or Percentages
| Intervention (N=17, n=1157)a |
Comparison (N=12, n=852) |
|||
|---|---|---|---|---|
| Mean Age | 41.2 | (3.0) | 42.2 | (3.8) |
| % <25 | 8.2 | (6.7) | 6.9 | (5.7) |
| % 25–39 | 36.9 | (9.0) | 36.2 | (13.3) |
| % 40–54 | 39.0 | (8.4) | 39.1 | (9.7) |
| % 55+ | 14.0 | (5.1) | 15.7 | (8.6) |
| % Female | 27.5 | (13.9) | 37.8 | (23.9) |
| % White | 77.4 | (19.7) | 83.1 | (9.6) |
| Education | ||||
| % Less than high school | 5.0 | (5.1) | 2.8 | (3.9) |
| % High school education | 23.0 | (8.2) | 24.1 | (10.5) |
| % Technical college | 45.1 | (8.0) | 49.2 | (9.8) |
| % College graduate | 21.9 | (9.5) | 19.0 | (10.6) |
| % Postgraduate | 5.1 | (6.8) | 4.9 | (4.5) |
Note.
N = number of worksites, n = number of employees responding
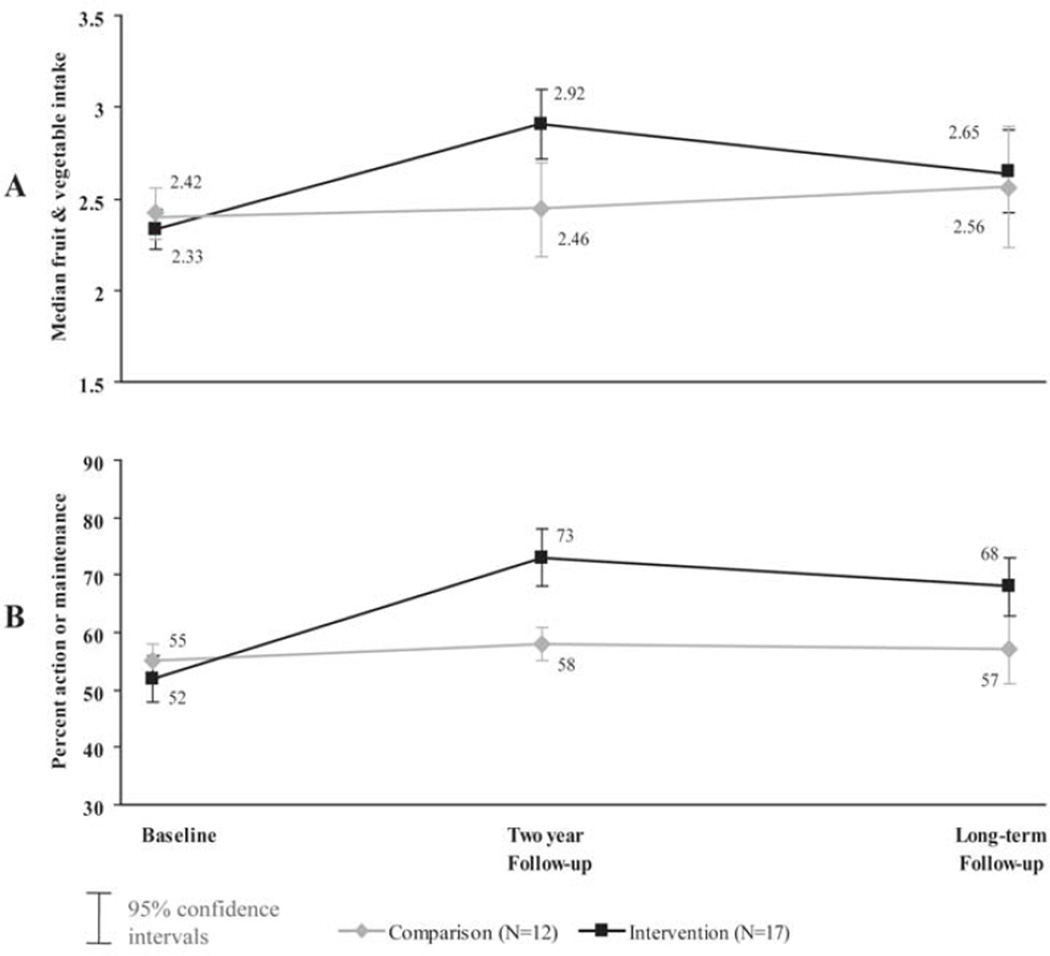
Employees reported eating an average of just over 2 servings daily at the original baseline. Servings of fruits and vegetables in these blue-collar worksites increased over the 2 year period in the Seattle 5 a Day study, especially in the intervention group, and then decreased slightly to the long-term follow-up evaluation point, as is shown in Figure 2A. The long-term follow-up evaluation took place an average of 4.4 years after the baseline evaluation in both groups. The percentage of the workforce in action or maintenance stage of readiness to increase fruit and vegetable consumption was about 50% at baseline in both groups, increasing to nearly three-quarters at 2-year follow-up in the intervention group and then decreasing slightly by long-term follow-up, as shown in Figure 2B. Table 3 shows the change from baseline to long-term follow-up in both groups. The differential change in the intervention group compared to the comparison group at 4.4 years postbaseline (the intervention effect) was 0.21 servings of fruits and vegetables, with 95% confidence interval (C.I.) of 0.02 to 0.39 servings. There was a corresponding differential change in percent in action or maintenance stage of readiness to change, with an intervention effect of 12% (96% C.I. 5% to 19%).
Figure 2.
Fruit and Vegetable Intake (A) and Readines to Change (B)Over Time by Intervention Arm in 29 Worksites
Table 3.
Long-Term Change in Fruit and Vegetable Intake and Readiness to Change
| Baseline Mean (S.E.) |
Long-Term Follow-up Mean (S.E.) |
Change Mean (95% C.I.) |
Long-Term Intervention Effect Estimate (95% C.I.) |
|
|---|---|---|---|---|
| Fruit & Vegetable Servings | ||||
| Comparison (n=12) | 2.38 (0.09) | 2.57 (0.09) | 0.19 (0.00, 0.37) | |
| Intervention (n=17) | 2.25 (0.07) | 2.62 (0.08) | 0.37 (0.27, 0.47) | 0.21 (0.02, 0.39) |
| Percent Action or Maintenance Stage | ||||
| Comparison (n=12) | 55 (2.2) | 58 (2.9) | 3 (−4, 9) | |
| Intervention (n=17) | 52 (1.9) | 67 (2.4) | 15 (9, 21) | 12 (5, 19) |
Although none of the interaction terms of worksite characteristic by intervention arm were statistically significant, some subgroups of worksites had strong evidence of an intervention effect in the secondary analyses. As shown in Table 4, in smaller worksites (no more than 75 employees) the differential change in fruit and vegetable intake was 0.34 servings (95% C.I. 0.02 to 0.67). The corresponding analysis of change in percent in action or maintenance (Table 5) revealed an intervention effect of 18% for small worksites (95% C.I. 0.07 to 0.30). Other significant effects on percent action or maintenance were found for subsets of companies, but the effects sizes in each complementary subset were of similar magnitude.
Table 4.
Intervention Effect on Fruit & Vegetable Servings by Company Characteristics at Baseline
| Intervention | Comparison | Intervention Effect |
Confidence Limits |
|||
|---|---|---|---|---|---|---|
| Industry Classification | Baseline |
Long-Term Change |
Baseline |
Long-Term Change |
||
| Service (n = 4, 6, respectively) | 2.42 | 0.30 | 2.36 | 0.06 | 0.24 | (−0.14,0.62) |
| Manufacturing or transportation (n = 13, 6, respectively) | 2.23 | 0.40 | 2.41 | 0.30 | 0.10 | (−0.20,0.40) |
| Worksite Size | ||||||
| ≤75 | 2.25 | 0.47 | 2.36 | 0.13 | 0.34* | (0.02,0.67) |
| >75 | 2.29 | 0.37 | 2.40 | 0.25 | 0.11 | (−0.18,0.41) |
| Percent Blue Collar | ||||||
| ≤50 | 2.38 | 0.39 | 2.37 | 0.17 | 0.22 | (−0.03,0.48) |
| >50 | 2.15 | 0.44 | 2.46 | 0.42 | 0.02 | (−0.51,0.55) |
| Percent Turnover | ||||||
| ≤10 | 2.26 | 0.49 | 2.30 | 0.20 | 0.29 | (−0.03,0.61) |
| >10 | 2.27 | 0.32 | 2.43 | 0.19 | 0.14 | (−0.14,0.42) |
| Management Support | ||||||
| Low | 2.24 | 0.33 | 2.37 | 0.22 | 0.10 | (−0.28,0.48) |
| High | 2.28 | 0.42 | 2.40 | 0.12 | 0.30 | (−0.02,0.61) |
| Contact Person* | ||||||
| Different over time | 2.19 | 0.43 | 2.28 | 0.13 | 0.30 | (−0.14,0.73) |
| Same over time | 2.29 | 0.41 | 2.46 | 0.22 | 0.19 | (−0.05,0.44) |
Note.
Over time from initial recruitment for the Seattle 5 a Day study and re-recruitment for follow-up study
P<0.05
Table 5.
Intervention Effect on Stage-of-Change by Company Characteristics at Baseline
| Intervention | Comparison | Intervention Effect |
Confidence Limits |
|||
|---|---|---|---|---|---|---|
| Industry Classification | Baseline |
Long-Term Change |
Baseline |
Long-Term Change |
||
| Service (n = 4, 6, respectively) | 0.54 | 0.10 | 0.57 | 0.01 | 0.08 | (−0.05,0.21) |
| Manufacturing or transportation (n = 13, 6, respectively) | 0.51 | 0.16 | 0.53 | 0.03 | 0.13* | (0.02,0.23) |
| Worksite Size | ||||||
| ≤75 | 0.51 | 0.15 | 0.54 | −0.03 | 0.18* | (0.07,0.30) |
| >75 | 0.53 | 0.15 | 0.56 | 0.06 | 0.09 | (−0.01,0.19) |
| Percent Blue Collar | ||||||
| ≤50 | 0.53 | 0.12 | 0.56 | 0.02 | 0.10* | (0.02,0.19) |
| >50 | 0.51 | 0.18 | 0.51 | 0.03 | 0.14 | (−0.04,0.32) |
| Percent Turnover | ||||||
| ≤10 | 0.55 | 0.13 | 0.56 | 0.00 | 0.13* | (0.02,0.24) |
| >10 | 0.49 | 0.16 | 0.55 | 0.03 | 0.12* | (0.03,0.22) |
| Management Support | ||||||
| Low | 0.47 | 0.24 | 0.55 | 0.05 | 0.19* | (0.07,0.31) |
| High | 0.54 | 0.12 | 0.56 | −0.04 | 0.15* | (0.05,0.26) |
| Contact Persona | ||||||
| Different over time | 0.55 | 0.12 | 0.54 | 0.04 | 0.16* | (0.01,0.30) |
| Same over time | 0.51 | 0.16 | 0.56 | 0.06 | 0.10* | (0.02,0.18) |
Note.
Over time from initial recruitment for the Seattle 5 a Day study and re-recruitment for follow-up study
P<0.05
There was good consistency between key informants interviewed at long-term follow-up. The interviews in the intervention companies suggested that 10 companies continued to have an EAB or other group concerned with health issues, 12 included health related messages in their regular communications systems (that could include flyers), 3 had 5 a Day activities currently being conducted in the worksite, and 14 companies still had 5 a Day promotional materials visible.
DISCUSSION
The low-intensity multilevel worksite intervention that was our Seattle 5 a Day program in blue-collar and service industry worksites led to successfully sustained increased fruit and vegetable intake more than 2 years after the intervention ended, and a total of 4.5 years after baseline enrolment. Our study suggests that interventions to encourage and sustain higher consumption of fruits and vegetables can include simple, straightforward, and positive messages that are accessible to all educational levels. The estimated size of the intervention effect that had been sustained in our study (0.21 servings) compares favorably with other studies of fruit-and-vegetable behavior change, some of which have had much shorter follow-up periods. For example the Working Well Trial14 found an intervention effect of 0.18 servings of fruits and vegetables at 4 years follow-up, and the Next Step Trial22 and Treatwell23 in the worksite-alone arm found an intervention effect of 0.1 servings and 0.2 servings, respectively, at 2 years of follow-up. The finding of a sustained change associated with the intervention of 0.2 servings is a significant finding of potential public health importance, even though at an individual level the change is small. Because of the association between fruits and vegetables and lower risk of chronic diseases, including lung cancer and colorectal cancer,24 even small changes in fruit and vegetable daily servings, if made on a population-wide basis and sustained over time, would be expected to result in lower incidence of those diseases. The long-term intervention effect found in our study is supported by the significant increase in percent of the workforce engaged in increasing their fruit and vegetable consumption (percent in action or maintenance stage from the transtheoretical model9,21,25). Because there was an average of 2.4 years between the 2- year follow-up of Seattle 5 a Day in blue-collar and service industry worksites and the recontact for the new study, and our evaluations consist of a fresh cross-sectional sample of the workforce at each time point, changes were maintained or reinforced. It appears as though not only employees who were with the company throughout the intervention but perhaps also new employees who joined were able to maintain a higher fruit and vegetable intake in the absence of additional research team input. At the end of the intervention period, a big “close-out” event took place in the companies, during which the employee advisory board members were encouraged to accept the responsibility to maintain the program in their worksites. More than half of the intervention companies retained posters and flyers from the intervention and incorporated health-related messages in the company’s regular communication systems from interviews at long-term follow-up. It may be that social support at the workplace and a change in social norms may have played a role. This would be consistent with the findings of Wilfley and colleagues that social facilitation maintenance is an effective strategy in maintaining weight change.26 A change in social norms often requires more time than research projects allow. The North Karelia project, for example, did not see changes in smoking behavior until 10 years after the project was initiated.27,28 The Community Intervention Trial for Smoking Cessation (COMMIT) did not begin to see results in smoking cessation until 3 years after the communities were randomized.29 Other large randomized studies of smoking cessation or involving community interventions had mixed results with respect to ability to sustain change over time.30–34
The limitations of our study include the differential continuation rate between intervention and comparison group companies. This was particularly marked for the manufacturing companies. This may have led to misestimation of the intervention effect if the missing companies had employees who were making and sustaining large changes in fruit and vegetable behaviors in the absence of an intervention. It is more likely that companies who refused to participate in the second study were less interested in health promotion. The other limitation is that the worksite characteristics used to stratify companies to further evaluate the intervention effectiveness were aggregate measures of individual characteristics. This was a compromise made to retain the worksite as the unit of analysis and thereby retain the maximum information, rather than restrict analyses to the relatively small nested cohort of responders at baseline who also responded at long-term follow-up (39% of baseline responders). Use of key informant interviews enabled descriptive information about the company and the extent to which the intervention was continuing in the worksite. It might be considered to be a limitation that key informants cannot be considered to be representative of all employees in the worksite, so the information they provide is qualitative rather than quantitative.
Our research supports what has been shown many times, namely that changing health behavior is difficult and may be gradual.9,21,25 This is especially true in the context of an intervention that has relatively low intensity. It has been noted that behavior change in the general population is apt to occur in small steps, with individuals gaining confidence to make further change as their success in attaining the small changes is realized.35–37 As confidence increases, the small changes in behavior can increase over time.9,27,28,38 Successful individual level behavior-change strategies appear to be those that begin with understanding the individual’s current behavior and focus on helping him or her make small changes that then lead to larger changes.35,36 It is less clear whether or not changes at the worksite level occur and grow over time in the same way, and our findings suggest this may not be the case.
Low-intensity interventions do not provide the repeated personal interactions that help a single individual achieve small changes, relying instead on change messages communicated through posters, mail, demonstrations, short group meetings, and other delivery channels directed toward large groups.9 As a result, low-intensity interventions generally result in smaller health-behavior changes at the individual level than do more intense interventions.
Numerous worksite research studies, including this one, have formed partnerships with employees and the worksite.14,20,39 Based on community organization strategies and participation prin-ciples,40,41 the research studies have involved partners at various levels ranging from a group that supports the research agenda but has little decision-making power to almost autonomous groups that are involved in all aspects of decision making. The majority of research projects, however, try to strike a balance between worksite and research needs.42 Worksite partners who perceive some good coming out of the project often wish to have the means for project longevity.31,33,43,44 Unfortunately, many research organizations have simply removed themselves after the research phase of the project has ended, leaving the worksite partners without resources, capabilities, or other avenues to address the original problem or behavior change goal. Such an action on the part of researchers is considered inconsistent with the principles of community ownership and part-nership.41,45–48
Only recently have some trials built in transition time and resources to plan for activities beyond the research years.49 The largest worksite cancer-prevention research project (the Working Well Trial) expressed the goal of achieving long-term maintenance, but little was done to achieve the goal.44 In the Working Well Trial, investigators tried to encourage worksites to institutionalize project activities that resulted in decreased fat consumption and increased fiber consumption.14 Two years after the end of intervention, however, very little remained of the project activities.44 It is important to understand whether an intervention can help worksites continue project activities after the research ends. More and more worksites are including health promotion activities into their regular employee benefits.50 Worksite health-promotion programs offer many benefits for employee and employer alike. For employees, such activities are often convenient to attend and less expensive than seeking the same activities outside of the workplace. Coworkers are available to provide social support for continuing activities.16 As employees adopt healthful habits, they may be able to persuade the employer to adopt more programs to reinforce good health behavior. For employers, effective worksite health-promotion programs can lead to containment of medical and disability costs, reduction in absenteeism because of health problems, and enhancement of the corporate image.15,51 In addition, offering health care programs can increase employee morale and sense of belonging to the worksite. In the next phase of our studies, we plan to implement and evaluate a method of institutionalizing intervention activities around fruits-and-vegetable intake behaviors in the worksite.
From our present study, we conclude that the multilevel intervention in small to medium blue-collar worksites had sustained effects at the company level even after the companies had not been in touch with the research team for 2 to 3 years. Although the average effects were not large, this relatively low-intensity intervention approach could provide an important model in interventions to improve the health of the public.
Acknowledgments
Seattle 5 a Day was supported by R01 CA59731. The follow-up study is supported in part by R01 CA105835. Moreover, we are grateful to the interventionists and other staff who so ably implemented the 5 A Day intervention, in partnership with the worksites. We are indebted to all the participating worksites who allowed us to gather research data in addition to collaborating with us in the implementation of the intervention.
REFERENCES
- 1.Bazzano LA, He J, Ogden LG, et al. Fruit and vegetable intake and risk of cardiovascular disease in US adults: the first National Health and Nutrition Examination Survey Epidemio-logic Follow-up Study. Am J Clin Nutr. 2002 Jul;76(1):93–99. doi: 10.1093/ajcn/76.1.93. [DOI] [PubMed] [Google Scholar]
- 2.Riboli E, Norat T. Epidemiologic evidence of the protective effect of fruit and vegetables on cancer risk. Am J Clin Nutr. 2003 Sep;78(3 Suppl):S559–S569. doi: 10.1093/ajcn/78.3.559S. [DOI] [PubMed] [Google Scholar]
- 3.National Academy of Sciences, Committee on Diet and Health, National Research Council. Diet and Health: Implications for Reducing Chronic Disease Risk. Washington, DC: National Academy Press; 1989. [Google Scholar]
- 4.Blanck HM, Gillespie C, Kimmons JE, et al. Trends in fruit and vegetable consumption among U.S. men and women, 1994–2005. [Accessed October 15, 2009];Prev Chronic Dis. 2008 Apr;5(2):A35. http:// www.cdc.gov/pcd/issues/2008/apr/07_0049.htm. [PMC free article] [PubMed] [Google Scholar]
- 5.Serdula MK, Coates RJ, Byers T, et al. Fruit and vegetable intake among adults in 16 states: results of a brief telephone survey. Am J Public Health. 1995 Feb;85(2):236–239. doi: 10.2105/ajph.85.2.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Serdula M, Coates RJ, Byers T, et al. Evaluation of a brief telephone questionnaire to estimate fruit and vegetable consumption in diverse study populations. Epidemiology. 1993;(4):455–463. doi: 10.1097/00001648-199309000-00012. [DOI] [PubMed] [Google Scholar]
- 7.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993 Nov 10;270(18):2207–2212. [PubMed] [Google Scholar]
- 8.Kumanyika S. Improving our diet—still a long way to go. N Engl J Med. 1996 Sep 5;335(10):738–740. doi: 10.1056/NEJM199609053351011. [DOI] [PubMed] [Google Scholar]
- 9.Beresford SAA, Curry SJ, Kristal AR, et al. A dietary intervention in primary care practice: the Eating Patterns Study. Am J Public Health. 1997 Apr;87(4):610–616. doi: 10.2105/ajph.87.4.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Estabrooks PA, Glasgow RE, Dzewaltowski DA. Physical activity promotion through primary care. JAMA. 2003 Jun 11;289(22):2913–2916. doi: 10.1001/jama.289.22.2913. [DOI] [PubMed] [Google Scholar]
- 11.Bowen DJ, Ehret C, Pederson M, et al. Results of an adjunct dietary intervention program in the Women’s Health Initiative. Journal of the American Dietetic Association. 2002;102:1631–1637. doi: 10.1016/s0002-8223(02)90347-0. [DOI] [PubMed] [Google Scholar]
- 12.Kahn EB, Ramsey LT, Brownson RC, et al. The effectiveness of interventions to increase physical activity. A systematic review. Am J Prev Med. 2002 May;22(4 Suppl):73–107. doi: 10.1016/s0749-3797(02)00434-8. [DOI] [PubMed] [Google Scholar]
- 13.Ritenbaugh C, Patterson RE, Chlebowski RT, et al. The Women’s Health Initiative Dietary Modification trial: overview and baseline characteristics of participants. Ann Epidemiol. 2003 Oct;13(Suppl 9):S87–S97. doi: 10.1016/s1047-2797(03)00044-9. [DOI] [PubMed] [Google Scholar]
- 14.Abrams DB, Boutwell WB, Grizzle J, et al. Cancer control at the workplace: the Working Well Trial. Prev Med. 1994 Jan;23(1):15–27. doi: 10.1006/pmed.1994.1003. [DOI] [PubMed] [Google Scholar]
- 15.Jacobson MI, Yenney SL, Bisgard JC. An organizational perspective on worksite health promotion. Occup Med. 1990 Oct-Dec;5(4):653–664. [PubMed] [Google Scholar]
- 16.Abrams D, Emmons K, Linnan L, Biener L. Interventions for Smokers: An International Perspective. In: Richmond R, editor. Smoking cessation at the workplace: Conceptual and practical considerations. Baltimore, MD: Williams and Wilkins; 1994. pp. 137–170. [Google Scholar]
- 17.US Bureau of Labor Statistics. Current Employment Statistics (CES) Washington, DC: Government Printing Office; 2001. [Google Scholar]
- 18.Thompson FE, Byers T. Dietary Assessment Resource Manual. J Nutr. 1994;124(Suppl):2305S. doi: 10.1093/jn/124.suppl_11.2245s. [DOI] [PubMed] [Google Scholar]
- 19.Beresford SA, Thompson B, Feng Z, et al. Seattle 5 a Day worksite program to increase fruit and vegetable consumption. Prev Med. 2001 Mar;32(3):230–238. doi: 10.1006/pmed.2000.0806. [DOI] [PubMed] [Google Scholar]
- 20.Thompson B, Shannon J, Beresford SAA, et al. Implementation aspects of the Seattle “5 a Day” intervention project: strategies to help employees make dietary changes. Topics Clin Nutr. 1995;11:58–75. [Google Scholar]
- 21.Prochaska JO, DiClemente CC. Transtheoretical therapy: toward a more inte-grative model of change. Psychotherapy: Theory, Research and Practice. 1982;19:276–288. [Google Scholar]
- 22.Tilley BC, Glanz K, Kristal AR, et al. Nutrition intervention for high-risk auto workers: results of the Next Step Trial. Prev Med. 1999;28(3):284–292. doi: 10.1006/pmed.1998.0439. [DOI] [PubMed] [Google Scholar]
- 23.Sorensen G, Stoddard A, Peterson K, et al. Increasing fruit and vegetable consumption through worksites and families in the treatwell 5-a-day study. Am J Public Health. 1999 Jan;89(1):54–60. doi: 10.2105/ajph.89.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gonzalez CA, Riboli E. Diet and cancer prevention: where we are, where we are going. Nutr Cancer. 2006;56(2):225–231. doi: 10.1207/s15327914nc5602_14. [DOI] [PubMed] [Google Scholar]
- 25.Prochaska OJ, DiClemente C. Stages and processes of self-change of smoking: Toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 26.Wilfley DE, Stein RI, Saelens BE, et al. Efficacy of maintenance treatment approaches for childhood overweight: a randomized controlled trial. JAMA. 2007 Oct 10;298(14):1661–1673. doi: 10.1001/jama.298.14.1661. [DOI] [PubMed] [Google Scholar]
- 27.Puska P, Nissinen A, Salonen JT, Toumilehto J. Ten years of the North Karelia Project: results with community-based prevention of coronary heart disease. Scand J Soc Med. 1983;11(3):65–68. [PubMed] [Google Scholar]
- 28.Puska P, Tuomilehto J, Salonen J, et al. Changes in coronary risk factors during comprehensive five-year community programme to control cardiovascular diseases (North Karelia project) Br Med J. 1979;2(6199):1173–1178. doi: 10.1136/bmj.2.6199.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.COMMIT Research Group. Community Intervention Trial for Smoking Cessation (COMMIT): I. Cohort results from a four-year community intervention. Am J Public Health. 1995;85(2):183–192. doi: 10.2105/ajph.85.2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Altman DG. Sustaining interventions in community systems: on the relationship between researchers and communities. Health Psychol. 1995;14(6):526–536. doi: 10.1037//0278-6133.14.6.526. [DOI] [PubMed] [Google Scholar]
- 31.Lichtenstein E, Thompson B, Nettekoven L, Corbett K. Durability of tobacco control activities in 11 North American communities: life after the Community Intervention Trial for Smoking Cessation (COMMIT) Health Educ Res. 1996;11(4):527–534. doi: 10.1093/her/11.4.527. [DOI] [PubMed] [Google Scholar]
- 32.Thompson B, Lichtenstein E, Corbett K, Nettekoven L, Feng Z. Durability of tobacco control efforts in the 22 Community Intervention Trial for Smoking Cessation (COMMIT) communities 2 years after the end of intervention. Health Educ Res. 2000;15(3):353–366. doi: 10.1093/her/15.3.353. [DOI] [PubMed] [Google Scholar]
- 33.Bracht N, Finnegan JR, Jr, Rissel C, et al. Community ownership and program continuation following a health demonstration project. Health Educ Res. 1994;9(2):243–255. doi: 10.1093/her/9.2.243. [DOI] [PubMed] [Google Scholar]
- 34.LaFond AK. Improving the quality of investment in health: lessons on sustainability. Health Policy Planning. 1995;10:S63–S76. [Google Scholar]
- 35.Bandura A. Self Efficacy: The Exercise of Control. New York: W. H. Freeman; 1977. [Google Scholar]
- 36.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice-Hall; 1977. [Google Scholar]
- 37.Dye CJ, Haley-Zitlin V, Willoughby D. Insights from older adults with type 2 diabetes: making dietary and exercise changes. Diabetes Educ. 2003 Jan-Feb;29(1):116–127. doi: 10.1177/014572170302900116. [DOI] [PubMed] [Google Scholar]
- 38.Henderson M, Thompson B, Kristal A. Behavioural intervention versus chemoprevention. IARC Sci Publ. 1996;(136):123–130. [PubMed] [Google Scholar]
- 39.The COMMIT Research Group. Community Intervention Trial for Smoking Cessation (COMMIT): Summary of design and intervention. J Natl Cancer Inst. 1991;83(22):1620–1628. doi: 10.1093/jnci/83.22.1620. [DOI] [PubMed] [Google Scholar]
- 40.Bracht N, Kingsbury L, Rissel C. A five-stage community organization model for health promotion: Empowermenet and partnership strategies. In: Bracht N, editor. Health Promotion at the Community Level: New Advances. 2nd. Thousand Oaks, CA: Sage Publications; 1998. pp. 83–104. [Google Scholar]
- 41.Thompson B, Kinne S. Social Change Theory: Applications to Community Health. In: Bracht N, editor. Health Promotion at the Community Level: New Advances. 2nd. Thousand Oaks, CA: Sage Publications; 1999. pp. 45–65. [Google Scholar]
- 42.Mittelmark M. Balancing the requirements of research and the needs of communities. In: Bracht N, editor. Health Promotion at the Community Level. Newbury Park, CA: Sage Publications; 1990. pp. 125–142. [Google Scholar]
- 43.Altman DG, Endres J, Linzer J, et al. Obstacles to and future goals of ten comprehensive community health promotion projects. J Community Health. 1991;16(6):299–314. doi: 10.1007/BF01324515. [DOI] [PubMed] [Google Scholar]
- 44.Sorenson G, Thompson B, Basen-Engquist K, et al. Durability, dissemination, and institu-tionalization of worksite tobacco control programs: results from the Working Well Trial. Int J Behav Med. 1998;5(4):335–351. doi: 10.1207/s15327558ijbm0504_7. [DOI] [PubMed] [Google Scholar]
- 45.Green LW, McAlister AL. Macro-intervention to support health behavior: some theoretical perspectives and practical reflections. Health Educ Q. 1984;11(3):322–339. [PubMed] [Google Scholar]
- 46.Green LW. The theory of participation: a qualitative analysis of its expression in national and international health politics. Adv Health Educ Promot. 1986;(1A):211–236. [Google Scholar]
- 47.Thompson B, Wallack L, Lichtenstein E, Pechacek T. Principles of community organization and partnership for smoking cessation in the Community Intervention Trial for Smoking Cessation (COMMIT) Int Q Community Health Educ. 1991;(11):187–203. doi: 10.2190/1BQ5-K699-EWJP-8FP1. [DOI] [PubMed] [Google Scholar]
- 48.Wallack L, Wallerstein N. Health education and prevention: designing community initiatives. Int Q Community Health Educ. 1986–87;7(4):319–342. doi: 10.2190/0P5F-VWQ2-Q6M0-JBEL. [DOI] [PubMed] [Google Scholar]
- 49.The ASSIST Working Group on Durability. Turning Point for Tobacco Control: Toward a National Strategy to Prevent and Control Tobacco Use. Rockville, MD: Prospect Associates; 1996. [Google Scholar]
- 50.U.S. Department of Health and Human Services PHS. 1992 National survey of worksite health promotion activities: summary. Am J Health Promot. 1993;7(6):452–464. doi: 10.4278/0890-1171-7.6.452. [DOI] [PubMed] [Google Scholar]
- 51.Heimendinger J, Thompson B, Ockene J, et al. Reducing the risk of cancer through worksite intervention. Occup Med. 1990;5(4):707–723. [PubMed] [Google Scholar]