Abstract
Reduction of weight in obese type 2 diabetes mellitus (T2DM) individuals is emerging as a significant strategy in the reduction of proteinuria in diabetic nephropathy along with control of hyperglycemia, hypertension, and dyslipidemia. The objective was to evaluate the reduction in 24-h proteinuria in T2DM patients with nephropathy by weight loss, with conventional therapy (angiotensin-converting enzyme [ACE] inhibitors) as the control arm. A prospective, randomized controlled trial was conducted between June 2010 and May 2011. T2DM patients with confirmed nephropathy by 24-h urinary protein estimation with a body mass index (BMI) of >25 kg/m2 were studied. Patients who had nondiabetic nephropathy, uncontrolled hypertension (>125/75 mmHg) irrespective of antihypertensive drugs, excess weight due to edema or obesity due to other specific diseases, alcoholics, smokers, and patients who were on hemodialysis were excluded from the study. The patients were divided into three groups, namely, group A, patients on ACE inhibitor therapy; group B, patients on lifestyle modifications for weight loss; and group C, patients on an antiobesity drug (orlistat) and lifestyle modifications. At the end of 6 months, all the three groups were compared. Data were analyzed using software SPSS version 15.0. This study encompassed a total of 88 patients; 12 patients were dropped during the study period and 76 (group A: 22, group B: 23, and group C: 31) patients remained. The mean age of the patients was 58.36 ± 10.87 years (range: 30-70 years). At baseline, age, gender, mean BMI, waist-to-hip ratio (WHR), and 24-h proteinuria did not vary significantly among the three groups. At 6 months, the mean BMI significantly decreased in group C (P < 0.001) compared to that in the other two groups. Among the parameters BMI and WHR, the proportional form of BMI correlated well with the degree of reduction in proteinuria (r = 0.397, P = 0.01). Reduction in weight using lifestyle modifications and antiobesity drugs might improve renal function and proteinuria safely as observed in obese patients with diabetic nephropathy.
Keywords: Diabetes mellitus, diabetic nephropathy, obesity, proteinuria, weight loss
Introduction
Diabetic nephropathy remains a leading cause of end-stage renal disease (ESRD).[1] In patients with type 2 diabetes mellitus (T2DM), microalbuminuria is associated with a two-to four-fold increase in the risk of death.[1] In patients with overt proteinuria and hypertension, the risk is even higher.[1] It is estimated that 25-40% of the patients with type 1 diabetes mellitus (T1DM) and 5-40% of patients with T2DM develop diabetic kidney disease.[1] Interventions effective in slowing the progression from microalbuminuria to macroalbuminuria include (1) normalization of glycemia, (2) strict control of blood pressure, and (3) administration of angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs).[1,2] Newer approaches include protein restriction to 0.75 g/kg per day, and the use of lipid-lowering agents as renoprotective drugs, protein kinase C inhibitors, and sulodexide, an agent postulated to restore the glomerular charge by repleting the loss of glycosaminoglycans, thus acting as an antiproteinuric and ultimately a renoprotective drug.[1] In dietary treatment of diabetic nephropathy, several studies reported that a high-calorie, low-protein diet was beneficial for renal function and proteinuria.[3–5]
Moreover, obesity has emerged as a significant risk factor for renal dysfunction.[6] It is observed that a reduction in weight in obese people leads to an improvement in parameters of renal dysfunction, with overall reduction in the level of proteinuria unrelated to medications for reducing proteinuria provided to patients with diabetic nephropathy.[6] A definitive classified protocol is yet to be developed to address this unique observation where nonpharmacologically or by the use of weight-reducing medication, the hallmark of diabetic nephropathy, that is, proteinuria, can be reduced. Considering this, we planned this study to demonstrate the improvement in proteinuric status in nephropathy by reducing the weight of the patient in a stipulated time frame.
Materials and Methods
We conducted a prospective, randomized controlled trial with the approval of the institutional Ethical Committee. Informed consent was obtained from all the participants. Consecutive T2DM patients, attending the outdoor clinic at our institute, with nephropathy confirmed by 24-h urinary protein estimation and patients having both micro- and macro-albuminuria with a body mass index (BMI) of >25kg/m2 were included in the study. Patients who had nondiabetic nephropathy, uncontrolled hypertension (>125/75 mmHg) irrespective of antihypertensive drugs, excess weight due to edema or obesity due to other specific diseases, alcoholics, smokers, and patients who were on hemodialysis were excluded from the study.
The patients were divided into three groups; namely, group A, who were kept on ACE inhibitor therapy; group B, who were provided with specific guidelines for lifestyle modifications to be followed strictly for weight loss; and group C, who were put on an antiobesity drug (orlistat) and also provided the above-mentioned guidelines for weight loss.
A thorough clinical examination was carried out in all the patients with special attention given to edema over the feet, any evidence of endocrine dysfunction, and recording of blood pressure. The patients were in normotensive state (with or without antihypertensive treatment) but were not on antihypertensives which reduce proteinuria. The three groups were matched according to age, gender, BMI, waist-to-hip ratio (WHR), blood urea, serum creatinine, and 24-h urinary protein. Obesity parameters such as weight, height, BMI, waist circumference, hip circumference, and WHR were calculated in all the patients, and routine blood tests for diabetes and 24-h estimation of urinary protein were performed in all patients at enrolment. Obesity parameters and routine tests for diabetes, blood urea, serum creatinine, and 24-h estimation of urinary protein were repeated at 6-month follow-up.
Lifestyle modifications involved attention to three essential elements of lifestyle: dietary habits, physical activity, and modification of behavior.[7] The primary focus on diet therapy was to reduce overall consumption of calories.[7] The target was to decrease the caloric intake of about 500-1000 kcal/day in the routine dietary intake of the patient.[7] This calorie deficit was compensated by suggesting substitutions or alternatives to the diet; examples included choosing smaller meal portions, eating more fruits and vegetables, consuming more whole-grain cereals, selecting leaner cuts of meat, skimmed dairy products, reducing fried foods, avoiding other added fats and oils, and drinking water instead of caloric beverages.[7]
The combination of dietary modification and exercise is the most effective behavioral approach for the treatment of obesity.[7] A 30-min moderate-intensity physical activity on most, and preferably all, days of the week was advised to all the patients. Focusing on simple ways to add physical activity into the normal daily routine through leisure activities, travel, and domestic work was suggested; examples included walking, using the stairs, doing home and yard work, and engaging in sport activities.[7] These tips were given by a registered dietician of the hospital. Behavioral therapy was monitored by frequent enquiries with their caregivers on the telephone and checking the data sheet given to the patients about duration and type of exercise done and food habits.
Among the medications used in this study, the antiobesity drug orlistat was used in the group C patients along with lifestyle modifications. Orlistat is a synthetic hydrogenated derivative of a naturally occurring lipase inhibitor.[7] The patients were advised to take 120 mg of orlistat with every major meal like breakfast, lunch and dinner for a period of 6 months. They were sufficiently informed about the dose, dosage, side effects, and complications of the drug.[7] All the groups were followed for a period of 6 months. Obesity parameters, routine tests for diabetes, and 24-h estimation of urinary protein were carried out at 6 months. The patients in group A were provided with ACE inhibitor therapy (ramipril 5-10mg/day), which is a well-known drug to reduce proteinuria as observed in many studies.[2]
At the end of 6 months, all the groups were compared and statistical analysis was carried out. This was done using the SPSS (Statistical Package for Social Sciences) version 15.0.
Results
This study encompassed a total of 88 patients; 12 patients were dropped from the study and 76 (22 in group A, 23 in group B, and 31 in group C) remained. The mean age of the patients was 58.36 ± 10.87 years (range 30-70 years). Age (P = 0.89) and gender (0.29) did not show significant difference among the groups.
Baseline estimation of study parameters
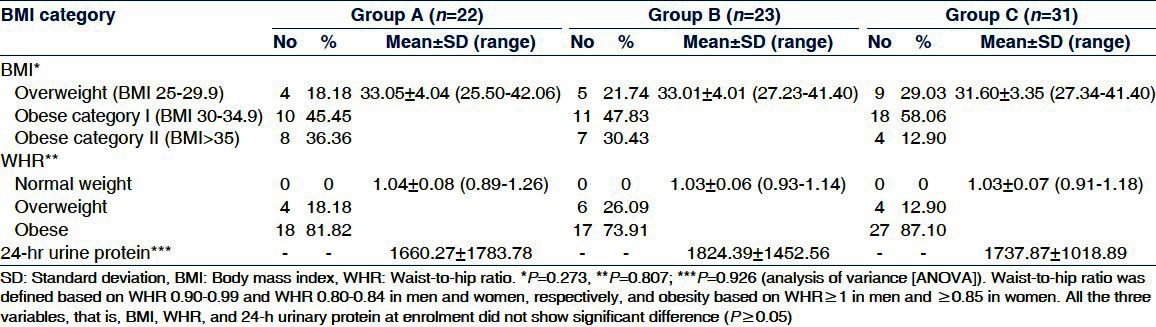
The mean BMI in group A was 33.05 ± 4.04 kg/m2 (range: 25.50-42.06 kg/m2), in group B it was 33.01 ± 4.01 (range: 27.23-41.40 kg/m2), and in group C it was 31.60 ± 3.35 kg/m2 (range: 27.34-41.40 kg/m2) [Table 1]. On comparing the data statistically, the difference was found to be nonsignificant statistically (P = 0.273). According to the WHR criteria, none of the patients were in the normal weight category. Mean WHR in group A was 1.04 ± 0.08 (range: 0.89-1.26), in group B it was 1.03 ± 0.06 (range: 0.93-1.14), and in group C it was 1.03 ± 0.07 (0.91-1.18) [Table 1]. On comparing the mean WHR in the three groups, no statistically significant difference was observed (P = 0.807). Mean 24-h urine protein level was maximum in group B (1824.39) and minimum in group A (1660.27) [Table 1]. On comparing the data statistically, there was no significant difference among the groups for any of these three parameters (P = 0.926).
Table 1.
Distribution of subjects in the three groups according to body mass index, waist-to-hip ratio, and 24-h urinary protein at enrolment
Six-month follow-up estimation of parameters
Majority of the patients in all the three groups were in the obese category I and obese category II. Mean BMI in group A was 32.90 ± 4.07 kg/m2 (range: 25.50-42.06 kg/m2), in group B it was 31.06 ± 3.53 kg/m2 (range: 25.95-37.50 kg/m2), and in group C it was 29.04 ± 3.35 kg/m2 (range: 24.00-39.90 kg/m2) [Table 2]. On comparing the data statistically, the difference was found to be significant (P = 0.001). According to the WHR criteria, one patient achieved normal weight at the 6-month follow-up. The proportion of overweight subjects ranged from 13.6% (group A) to 34.78% (group B). In group C, the proportion of overweight subjects was 16.13%. All the remaining patients were obese according to the WHR criteria. Mean WHR in group A was 1.05 ± 0.09 (range: 0.89-1.26), in group B it was 1.00 ± 0.06 (range: 0.92-1.11), and in group C it was 1.00 ± 0.06 (0.91-1.17) [Table 2]. On comparing the mean WHR in the three groups, a statistically significant difference was observed (P = 0.040).
Table 2.
Distribution of subjects in the three groups according to BMI, WHR, and 24-h urinary protein at 6-month follow-up
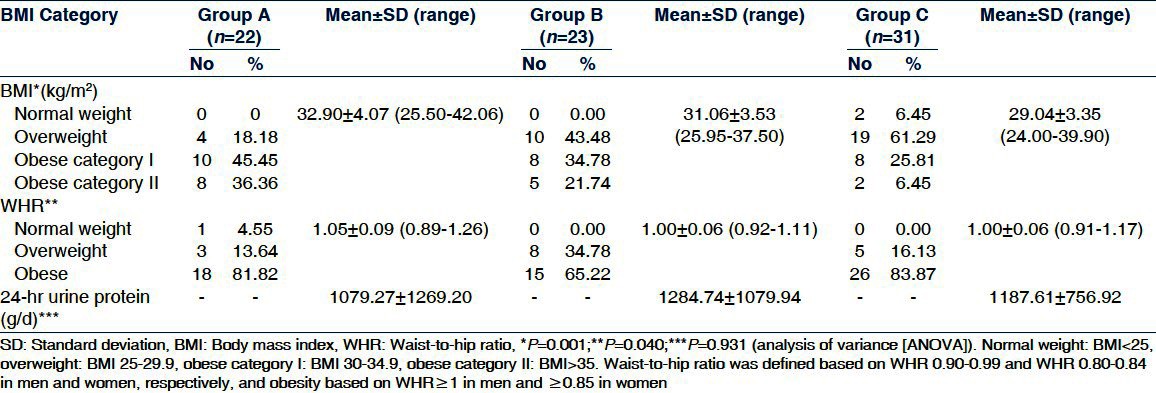
At the 6-month follow-up, the mean urinary protein was minimum in group A (1079.27 + 1269.20 mg/24 h) [Table 2]. However, on comparing the data statistically, there was no significant difference among the groups for any of these three parameters (P > 0.05).
Thus between baseline and the 6-month follow-up, a mean fall in BMI was observed in all the three groups which was maximum in group C and minimum in group A [Table 3]. The change in BMI was evident only in groups B (P ≤ 0.001) and C (P ≤ 0.001). Thus between baseline and the 6-month follow-up, the fall in mean BMI in the different groups was in the order of group C > group B > group A.
Table 3.
Change in mean body mass index, waist-to-hip ratio, and 24-h urine protein levels in the three groups at 6 months (paired t-test)
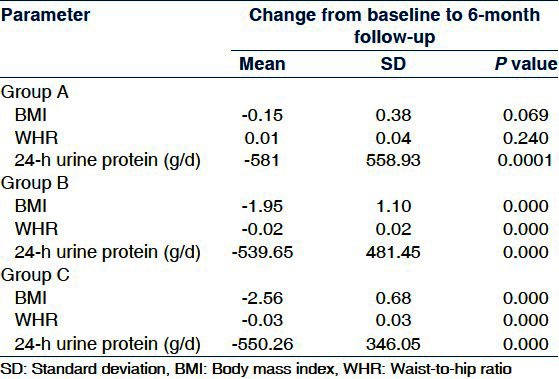
At the 6-month follow-up, the mean WHR increased in group A, whereas groups B and C showed a fall in the mean WHR, a greater fall in group C than in group B [Table 3]. The mean fall in WHR in the three groups was in the order of group C > group B > group A.
At 6 months, all the three groups showed a significant decrease in the mean 24-h urine protein from baseline levels, and the mean decrease was the maximum in group A and minimum in group B [Table 3]. The fall in the mean 24-h urinary protein levels in the three groups was in the order of group A > group C > group B.
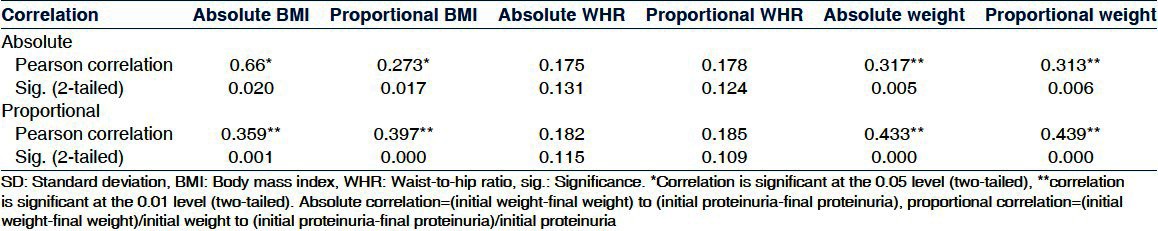
BMI and WHR (in absolute and proportional forms) correlated significantly with both weight loss and reduction in proteinuria [Table 4]. It was observed further that the proportional form of BMI correlated with the degree of reduction in proteinuria more significantly.
Table 4.
The correlation between body mass index, waist-to-hip ratio, and weight loss and proteinuria
The side effects observed in group C were change in bowel habits (n = 10), loose stools (n = 8), abdominal discomfort (n = 5), and oily staining of inner garments (n = 2). These patients were frequently supplemented with fat-soluble vitamins. Of the total 88, 12 patients were dropped out (group A: 3, group B: 3, and group C: 6). The reason for dropping out was side effects of orlistat in group C, whereas in the other groups, the patients were noncompliant to therapy. In all the three groups, very few (10%, n = 8) patients were on diuretic therapy and were distributed as four in group A, two in group B, and two in group C.
Discussion
The mechanism by which obesity leads to a deterioration in the renal function is not fully understood.[6,8–12] Weight loss has been shown to induce a dramatic decrease in proteinuria in patients with obesity-related proteinuria.[6,8–12] Increase in body weight may have independent effects on increasing proteinuria in diabetic patients and, therefore, weight control remains an important target in overweight diabetic patients.[6,8–12] Weight loss is noted to decrease the excretion of urinary protein significantly in patients with diabetic nephropathy along with substantial improvement in renal functions.[6,8–12]
This study shows that weight loss decreases proteinuria proportionally in obese diabetic patients with nephropathy. It was observed in our study that a mean decrease in BMI and WHR of the subjects in group C was significantly higher than that in the other two groups as would be expected, because the patients in group C were maintained on advised guidelines of lifestyle modifications and antiobesity drugs for weight loss, but group B patients were maintained only on advised lifestyle modifications for weight loss. Group A patients were on ACE inhibitors without much emphasis on advised guidelines for lifestyle modifications, and ACE inhibitors were given with an eye on overall improvement in nephropathy. Our study findings were similar to that of the study conducted by Chagnac et al., who showed that after weight loss, BMI decreased by 32 ± 4% to 32.1 ± 1.5%.[10] Another study by Saiki et al. showed that mean body weight decreased by 6.273 kg.[9] Praga et al. showed in their study that weight loss was moderate (averaging 4.1 ± 3% at the end of the 5-month study), but the effect on the level of proteinuria was striking; a 31 ± 37% reduction in baseline values was found.[12] Navaneethan et al. in their study showed that weight loss was achieved with various nonsurgical interventions (diet, exercise, and/or antiobesity agents). In patients with chronic kidney disease (CKD), BMI decreased significantly (weighted mean difference [WMD]: −3.67 kg/m2; 95% confidence interval (CI): −6.56 to −0.78) at the end of the study period with nonsurgical interventions.[8]
In all the three groups, a mean decrease in 24-h urine protein levels was observed. Between baseline and the 6-month follow-up, mean change was maximum in group A and minimum in group B. These findings were similar to the study conducted by Chagnac et al., who, apart from showing a decrease in BMI, also showed that the rate of albumin excretion decreased from 16 μg/min (range: 4-152 μg/min) to 5 μg/min (range: 3-37 μg/min) (P < 0.01). Fractional clearance of albumin decreased from 3.2 × 10-6 (range: 1.1-23 × 10-6) to 1.2 × 10-6 (range: 0.5-6.8 × 10-6) (P < 0.02).[10] In a study, Saiki et al. significantly correlated that a decrease in weight results in a decrease in serum creatinine, blood urea nitrogen, and urinary protein. He showed that along with reduction in weight, the mean serum creatinine, blood urea nitrogen, and urinary protein decreased significantly by 41.6723.9 mmmol/L, 1.5071.61 mmol/L, and 1.871.7 g/day, respectively.[9] Decrease in serum creatinine and urinary protein correlated with decrease in body weight (r = 0.62 and 0.49, respectively), and he concluded that weight reduction using a formula diet might improve renal function and proteinuria safely for a short term in obese patients with diabetic nephropathy.[9]
All the studies mentioned have highlighted the importance of weight reduction for reduction of proteinuria.[11–13] Thus here we find weight reduction as a well-addressed entity in terms of management of patients with diabetes mellitus. Therefore, it is desired in future studies that both absolute and proportional forms of BMI and WHR are correlated with the amount of weight loss.
We cannot rule out the usual medical care as a cause for reduction in proteinuria, but difference in this reduction as observed in each of the study groups was significant [Table 3].
We acknowledge that possible limitations that could have caused fallacies in our study include small sample size and short follow-up. The study had a small sample size because of strict adherence to the exclusion of patients such as those with BMI <25, those with uncontrolled hypertension, smokers, alcoholics, and those who were not willing for drug therapy and lifestyle modifications.
An ideal control group of obese type 2 diabetic patients with proteinuria without any intervention for reduction in proteinuria was not permitted in the study by the Ethical Committee.
A randomized controlled trial with a large number of subjects and longer follow-up is needed to reinforce the outcome of the study that a reduction in weight may cause a reduction in proteinuria in diabetic nephropathy.
Conclusion
These results suggested that a reduction in weight using lifestyle modifications and antiobesity drugs improves proteinuria safely for a short term in obese patients with diabetic nephropathy. It was also interesting to note that although BMI and WHR in both absolute and proportional forms correlated well with the amount of weight loss and degree of reduction in proteinuria, the proportional form of BMI was found to correlate more significantly with the degree of reduction in proteinuria in our study subjects.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Brownlee M, Ajello LP, Cooper ME, Vinik AL, Nesto RW, Boulton JM, et al. Diabetic nephropathy. In: Henry MK, Shlomo M, editors. Williams Textbook of Endocrinology. 11th ed. Philadelphia: Saunders; 2008. pp. 1417–49. [Google Scholar]
- 2.Alvin C, Powers . Diabetes Mellitus. In: Fauci AS, Braunwald E, editors. Harrison's Principle of Internal Medicine. 17th ed. New York: McGraw Hill; 2008. pp. 2275–304. [Google Scholar]
- 3.Walker JD, Bending JJ, Dodds RA, Mattock MB, Murrells TJ, Keen H, et al. Restriction of dietary protein and progression of renal failure in diabetic nephropathy. Lancet. 1989;2:1411–5. doi: 10.1016/s0140-6736(89)92032-1. [DOI] [PubMed] [Google Scholar]
- 4.Barsotti G, Ciardella F, Morelli E, Cupisti A, Mantovanelli A, Giovannetti S. Nutritional treatment of renal failure in type 1 diabetic nephropathy. Clin Nephrol. 1988;29:280–7. [PubMed] [Google Scholar]
- 5.Zeller K, Whittaker E, Sullivan L, Raskin P, Jacobson HR. Effect of restricting dietary protein on the progression of renal failure in patients with insulin-dependent diabetes mellitus. N Engl J Med. 1991;324:78–84. doi: 10.1056/NEJM199101103240202. [DOI] [PubMed] [Google Scholar]
- 6.Praga M, Hernández E, Andrés A, León M, Ruilope LM, Rodicio JL. Effects of body-weight loss and captopril treatment on proteinuria associated with obesity. Nephron. 1995;70:35–41. doi: 10.1159/000188541. [DOI] [PubMed] [Google Scholar]
- 7.Robert F, Kushner . Evaluation and Management of Obesity. In: Fauci AS, Braunwald E, editors. Harrison's Principle of Internal Medicine. 17th ed. New York: McGraw Hill; 2008. pp. 468–73. [Google Scholar]
- 8.Navaneethan SD, Yehnert H, Moustarah F, Schreiber MJ, Schauer PR, Beddhu S. Weight loss interventions in chronic kidney disease: A systematic review and meta-analysis. Clin J Am Soc Nephrol. 2009;4:1565–74. doi: 10.2215/CJN.02250409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saiki A, Nagayama D, Ohhira M, Endoh K, Ohtsuka M, Koide N, et al. Effect of weight loss using formula diet on renal function in obese patients with diabetic nephropathy. Int J Obes (Lond) 2005;29:1115–20. doi: 10.1038/sj.ijo.0803009. [DOI] [PubMed] [Google Scholar]
- 10.Chagnac A, Weinstein T, Herman M, Hirsh J, Gafter U, Ori Y. The effects of weight loss on renal function in patients with severe obesity. J Am Soc Nephrol. 2003;14:1480–6. doi: 10.1097/01.asn.0000068462.38661.89. [DOI] [PubMed] [Google Scholar]
- 11.Pérez G, Devaud N, Escalona A, Downey P. Resolution of early stage diabetic nephropathy in an obese diabetic patient after gastric bypass. Obes Surg. 2006;16:1388–91. doi: 10.1381/096089206778663733. [DOI] [PubMed] [Google Scholar]
- 12.Praga M. Therapeutic measures in proteinuric nephropathy. Kidney Int. 2005;68:S137–141. doi: 10.1111/j.1523-1755.2005.09925.x. [DOI] [PubMed] [Google Scholar]
- 13.Rossi MC, Nicolucci A, Pellegrini F, Comaschi M, Ceriello A, Cucinotta D, et al. Obesity and changes in urine albumin/creatinine ratio in patients with type 2 diabetes: The DEMAND study. Nutr Metab Cardiovasc Dis. 2010;20:110–6. doi: 10.1016/j.numecd.2009.02.013. [DOI] [PubMed] [Google Scholar]


