Abstract
Ischemia and reperfusion injury (IRI) is a dynamic process that involves two distinctive yet interrelated phases of ischemic organ damage and inflammation-mediated reperfusion injury. Although multiple cellular and molecular pathways contribute and regulate tissue/organ damage, integration of different players into a unified mechanism is warranted. The crosstalk between innate and adaptive immune systems plays a significant role in the pathogenesis of liver IRI. In this review, we focus on recent progress in the mechanism of liver innate immune activation by IR. Kupffer cells, DCs, NK, as well as T cells initiate local inflammation response, the hallmark of IRI, by utilizing distinctive immune receptors to recognize and/or trigger various molecules, both endogenous and exogenous. The interlocked molecular signaling pathways in the context of multiple liver cell types, the IRI kinetics, and positive vs. negative regulatory loops in the innate immune activation process are discussed. Better appreciation of molecular interactions that mediate these intricate cascades, should allow for the development of novel therapeutic approached against IRI in liver transplant recipients.
Keywords: Liver, ischemia/reperfusion injury, innate immunity, Toll-like receptors, T cells, Neutrophils
Introduction
Orthotopic liver transplantation (OLT) is an effective therapeutic modality for the treatment of end-stage liver disease. However, ischemia and reperfusion injury (IRI), the major component of the organ “harvesting” insult, remains one of the key limitations (1). The hepatocellular damage surrounding liver removal, storage and engraftment is critical to primary OLT non-function or late dysfunction, leads to a higher incidence of acute and chronic rejection, and contributes to the acute shortage of organs available for transplantation (2, 3). Hence, minimizing the adverse consequences of IRI should improve not only OLT outcomes, but also increase the number of patients that can be successfully transplanted. The mechanism of liver IRI, however, remains one of the most understudied areas in clinical and experimental organ transplantation.
The IR insult to the transplanted liver is a multifaceted process that combines elements of “warm” and “cold” injury. The process of warm organ damage, occurring in-situ in low flow states, is dominated by Kupffer cell (KC)-derived cytotoxic molecule-mediated hepatocellular injury. Cold IRI, experienced during ex-vivo preservation, is dominated by the damage to the liver sinusoidal endothelial cells (SEC) and disruption of the microcirculation (4, 5). These seemingly distinct processes share common mechanisms and overlapping effects upon non-parenchymal (KCs/lymphocytes) and parenchymal (hepatocytes) cell functions, both of which lead to the ultimate organ failure.
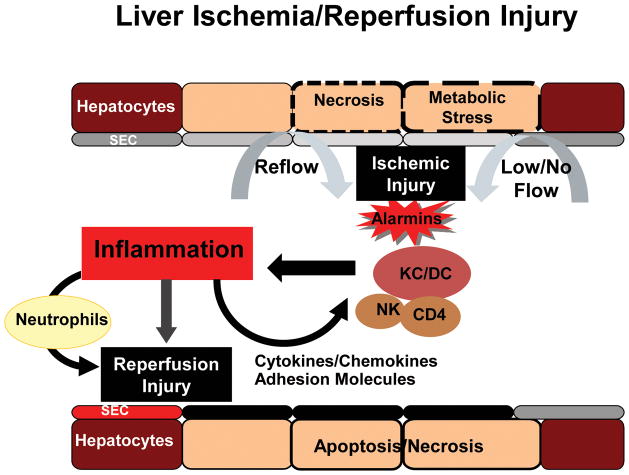
Two distinctive stages of liver IRI, with unique mechanisms of tissue damage, have been identified (Figure 1). The ischemic injury itself, a localized process of cellular metabolic disturbances, results from glycogen consumption, lack of oxygen supply, and adenosine triphosphate (ATP) depletion. The reperfusion injury, on the other hand, involves both direct and indirect cytotoxic mechanisms. The liver inflammation response is of a paramount importance, as prevention of local immune activation consistently ameliorates IRI cascade. Multiple innate immune activation pathways have been identified, with some exerting opposite pro- and anti-inflammatory functions, often in a cell-type specific and IR-stage dependent manner. Comprehensive dissection of liver innate immune activation mechanisms is critical for identifying novel therapeutic targets to alleviate pro-inflammatory while sparing or augmenting anti-inflammatory mechanism. Here, we review recent progress on the IR-triggered innate–adaptive crosstalk and immune activation, which is able to convert an immunologically quiescent liver to an inflammatory organ, even in the sterile environment. Most of the studies were performed in a mouse in-situ model of segmental hepatic warm ischemia and reperfusion. Although partially reflecting the real-life transplant setting, the model takes advantage of the genetically-targeted mouse strains for mechanistic studies. The clinically relevant mouse model, combining cold and warm IRI components of prolonged donor liver cold storage followed by OLT, has only recently been established (6).
Figure 1. Distinctive stages of liver IRI.
The ischemic injury, a localized process of hepatic metabolic disturbances, results from glycogen consumption, lack of oxygen supply, and ATP depletion. In the reperfusion injury, an immune activation-mediated amplification process, DAMPs (alarmins) produced during the initial cellular insult, trigger liver non-parenchymal cells (NPC) to generate the pro-inflammatory milieu, which damage the liver tissue directly or indirectly by activating neutrophils and recruiting immune cells from the circulation.
TLRs in liver IR Innate immune activation
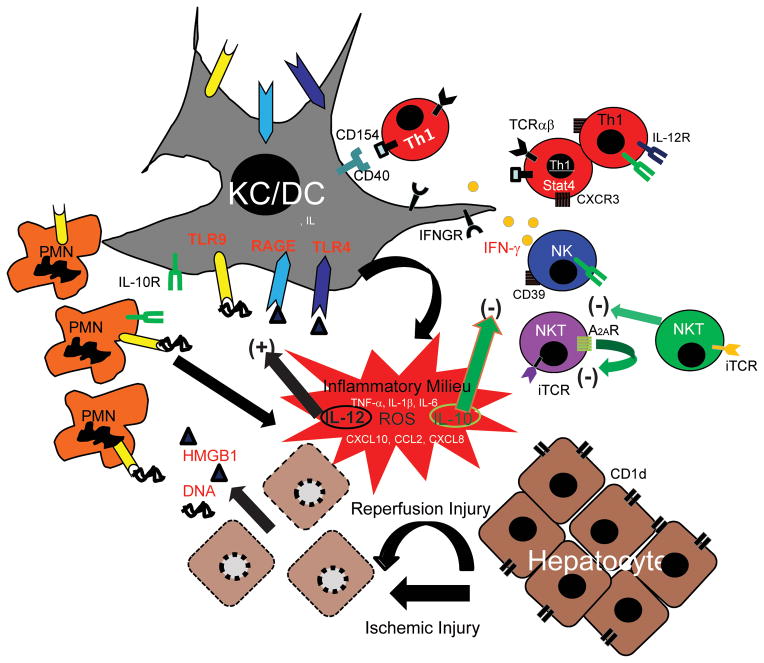
The role of liver pro-inflammatory response in the development of IRI has been documented since the early 1990ies. Although molecular details and putative mechanisms keep expanding, and remain controversial, its major role is to drive a self-amplified cytotoxic cascade towards liver parenchymal damage, by producing cytokines/chemokines/ROS and promoting local leukocyte sequestration and activation in the liver. The major cellular players in this local immune response are KCs, dendritic cells (DCs), neutrophils (PMNs), T cells and NK/NKT cells (Figure 2). Two distinct stages in IR-induced liver immune cascade have been defined. The first, immune triggering stage depends on liver resident KCs (and DCs), which become activated by endogenous damage-associated and/or pathogen-associated molecular pattern (DAMP/PAMP) molecules. These diverse “danger” molecules, termed “alarmins” are generated during states of cellular stress or damage. They facilitate pro-inflammatory milieu, the hallmark of liver IRI, which functions to propagate the inflammation response and damage to liver parenchymal cells. As a result, in the second stage, the circulating monocytes and PMNs, become activated and recruited into IR-livers to sustain the local immune response and to further amplify local tissue destruction.
Figure 2. An integrated mechanistic scheme of liver immune activation against IRI.
In the first phase of liver IRI, the ischemia insult induces necrotic cell death, which in turn provide diverse “danger” molecules, such as HMGB1 and DNA fragments to activate innate TLR4, RAGE and TLR9 signaling on KCs/DCs and neutrophils. T cells, particularly CD4 Th1 effectors, may also facilitate local innate immune activation via CD154-CD40 pathway. In the second phase of liver IRI, IFN-γ produced by T cells, NKT and NK cells enhances innate immune activation. In addition, CD1d and CD39 activate NKT and NK cells, respectively. The activation progresses via positive and negative regulatory loops. The pro-inflammatory milieu, composed of TNF-α, IL-1β, IL-6, IL-12, CXCL10, CCL2, CXCL8 and ROS, further activates local and recruits circulating immune cells, which promote cytotoxicity against liver parenchymal cells. Meanwhile, IL-10 counter-regulates the sustained pro-inflammatory activation, whereas adenosine receptor 2A inhibits NKT cell activation. Type II NKT cells may also down-regulate IFN-γ production by pro-inflammatory type I NKT cells.
The identification of sentinel Toll-like receptor (TLR) family represented a breakthrough in the study of liver innate immune activation (7, 8). There is now convincing evidence that TLR4, but not TLR2 signaling, provides the triggering mechanism of liver inflammation. Although exact roles of exogenous PAMPs, in particular LPS from intestinal flora, remain to be determined (trigger or sustain inflammation), roles of endogenous DAMPs that activate liver TLRs during IR have been gradually elucidated. There are two broadly categorized endogenous TLR ligands: those released from necrotic cells, including heat shock proteins (60, 70, Gp96), high mobility group box-1 (HMGB1) and DNA or RNA-complexes; and those derived from degraded extracellular matrix, including heparan sulfate, hyaluronan, fibrinogen, fibronectin A domain and tenascin C. HMGB1 protein, the best characterized DAMP, is released from the necrotic cells, as well as actively secreted from hypoxic or inflamed live cells (9). Liver non-parenchymal TLR4 is the main target for HMGB1 (7). Hepatocyte TLR4, although detectable in low copies seems to have marginal role in the early liver inflammatory response (10). It is worth noticing that HMGB1 biology has recently became quite complex. Questions concerning the molecular nature of its TLR4 binding (direct stimulation or by enhancing LPS activity), and putative roles of its other binding receptors, such as RAGE (receptor for advanced glycation end products) remain wide open (11, 12). Indeed, RAGE has been shown essential in liver IRI by regulating MIP-2 production via Egr-1-dependent mechanism, as well as influencing cell death and TNF-α production via Egr-1-independent mechanism (13, 14). Interestingly, RAGE blockade has led to higher TNF-α expression levels in the late (18 h) phase of liver reperfusion (14).
TLR9, an intracellular molecule at the interface of microbial and sterile inflammation, detects bacterial and endogenous DNA, and serves as a sensor of tissue necrotic cell death that exacerbates liver innate immune activation (15). TLR9 expressed in liver NPCs, particularly PMNs, was found indispensible for IR-induced ROS, IL-6 and TNF-α, data supported by in vitro finding where DNA released from necrotic hepatocytes readily activated liver NPCs to produce a similar pro-inflammatory gene induction pattern in the culture. Since TLR9 signals exclusively via myeloid differentiation primary response gene-88 (MyD88) pathway, a question arises as to why TLR4-mediated hepatocellular damage appears MyD88 signaling-independent (8)? One possible explanation relates to phase- and cell-type-specific liver innate immune activation and injury during the reperfusion phase. Hence, it is likely that MyD88-independent activation of KC (and DC) by DAMPs in the early phase of liver injury (1–6 h) may depend on the direct cytotoxic effect of soluble TNF-α enriched inflammatory milieu. In the later stage (>12h), however, newly recruited and activated PMNs may require MyD88 signaling. The role of other TLR family members in liver innate immune activation remains to be elucidated. Recently, TLR3, which recognizes necrotic cell-derived RNA products, has been shown to sustain inflammation in a murine gastrointestinal ischemia model (16). Thus, different TLRs may operate at distinct stages and in different cell types during the course of hepatic IRI.
As the most abundant type of liver NPCs, sinusoidal endothelial cells (SECs) are the first innate immune barrier between blood-born infectious agents and liver parenchymal tissue and are constantly exposed to gut-derived endotoxin. Although first identified as the primary cellular target of cold IRI, they may also play active roles in liver innate immune activation. In fact, SECs express multiple innate immune receptors (17, 18) and vascular endothelia cells have been shown recently to respond directly to TLR2 ligands (19). SECs interact with CD4 T cells during IR and facilitate platelet adherence and neutrophil migration (20). One unique feature of liver SECs relates to their ability of enhancing T cell transmigration by transcytosis and surface presentation of chemokines (21).
Non-TLRs in liver IR innate immune activation
The role of non-TLR innate receptors, such as nucleotide-binding domain (NOD)-like receptor (NLR) and RIG-I-like receptor (RLR) proteins to induce cytokine/chemokine programs and regulate local immune responses has only recently become unraveled. Unlike TLRs, imbedded in cell surface or lysosomal-endosomal membranes, these non-TLR molecules are cytosolic and recognize PAMPs within the cytosol. Analogous to TLRs, they can trigger local inflammatory response leading to immune activation. The necrotic cells are sensed by the inflammasomes to release the pro-inflammatory mediators. One member of NLR family, NLRP3 (NLR family, pyrin domain containing 3) has been involved in the mechanism of PMN recruitment to sites of focal hepatic necrosis in the model of sterile in vivo inflammation (22). In addition, a recent study has shown that gene silencing of NALP3 attenuated liver damage, in association with reduced production of IL-1β, IL-18, TNF-α, and IL-6; diminished HMGB1 levels; and decreased local inflammatory cell infiltration (23), indicating that inflammasome signaling may be essential in liver IRI. Indeed, ATP released from liver necrotic cells may activate the Nlrp3 inflammasome to generate an inflammatory microenvironment, which in turn alerts circulating PMNs to adhere within liver sinusoids. Future studies are needed to address putative cooperation between TLR and inflammasome pathways in liver inflammation leading to IR-hepatocellular damage.
IL-10 in liver IR innate immune activation
It becomes clear that IR-triggered liver innate immune activation is a self-limiting reaction with active regulatory mechanism. Key soluble factors capable of alleviating liver IRI include IL-4, IL-10 and IL-13 (24–26). These cytokines, readily expressed in IR-livers, and often spared or their expression heightened in IR-resistant animals. Although generally inhibitory to IR-induced pro-inflammatory TNF-α and IL-1β when administered exogenously, the endogenous role of IL-4, IL-10 and IL-13 may not necessarily be immune-regulatory. Indeed, although IL-13 deficient mice suffer from exacerbated liver injury, compared with IL-13 proficient (WT) counterparts, IR-induced TNF-α and CXCL8 (MIP-2) production in IL-13 KO and WT mice was comparable within the first 8 h of reperfusion (24). Although IL-13 deficiency alters PMN distribution in IR-livers, the most prominent effect of IL-13 seems to be the direct hepatocyte protection from ROS-induced cell death. The cellular sources of IL-4 and IL-13 in the liver, originally described as Th2 cell-derived cytokines, have not been defined. Nevertheless, the role of IL-10 as the key immune regulatory cytokine in the pathophysiology of liver IRI has been well documented. It becomes a recurring theme that IL-10 neutralization is both necessary and sufficient to recreate the pro-inflammatory gene profile in IR-resistant livers of otherwise immune-suppressed or deficient recipients (27, 28). It has been shown that multiple types of innate immune cells, DCs, macrophages and PMNs may all produce IL-10 and exert important auto-immune regulatory functions (29, 30). Recently, KCs were found to prevent organ damage in a bowel congested total liver IRI model by an IL-10 mediated mechanism (31). The question of which liver NPCs become IL-10 producers in response to IR remains to be addressed. Although KCs have been shown in vitro to produce IL-10 in response to endotoxin (32), its relevance to in vivo IR setting is not clear. Recently, liver conventional DCs have been shown to exert immune-regulatory functions during IR by producing IL-10 via a TLR9-mediated mechanism (33). Thus, the same liver NPCs, responsible for initiation of the pro-inflammatory immune response against IR (34), may also function to terminate their own initial reaction. Such a hypothesis is in agreement with in vitro studies in which macrophages (or DCs) produced both pro- and anti-inflammatory mediators in response to the very same TLR ligand supplied to the culture.
As IR readily activates pro- and anti-inflammatory gene programs, the critical question remains as to the mechanism that determined the nature of local immune responses, and dictates the outcome of liver injury. Is it merely the difference in the kinetics of innate immune gene induction or tissue/cell responsiveness to the gene products, in such a way that the pro-inflammatory program precedes the anti-inflammatory pattern, leading to the development of a self-limited tissue damaging response? Alternatively, endogenous ligands generated at different disease stages may trigger pro- and anti- inflammatory responses sequentially, possibly via distinct TLR pathways and/or in different liver cell types. One may also envision cell - cell interactions within livers, such as KC - T cell, may dictate the nature of local immune response by engaging additional activation signaling pathways. Addressing these questions should further our understanding of IRI mechanism, and help to identify novel therapeutic targets to suppress pro-inflammatory arm without interfering with the beneficial immune regulatory functions.
T cell-dependent liver IR innate immune activation
In addition to KCs and DCs, T cells, NK and NKT cells are also involved in IR-mediated liver innate immune activation (Figure 1). Although liver IRI occurs in the absence of exogenous T cell Ag in syngeneic recipients, and may proceed in the sterile environment, CD4 T cells are instrumental in promoting liver pro-inflammatory immune response (35). Indeed, livers in CD4-deficient hosts or WT mice depleted of CD4 T cells are protected from IR-damage. In sharp contrast, CD8 T cell depletion or targeted deficiency does not influence the severity of IRI. The immediate effect of putative Ag-specific CD4 T cells poses a series of questions regarding their activation and function in an innate immune response. Since naïve T cell activation requires not only specific Ags, but also takes more than a few hours to differentiate into the functional effectors, it is unlikely that they play a major role in the acute phase of liver IRI. Meanwhile, effector T cells can become activated quickly by pro-inflammatory mediators in the absence of cognate Ag stimulation, to either secrete cytokine/chemokine programs or upregulate cell surface costimulatory molecules (36). Such a scheme fits nicely with the kinetics of liver IRI. First, liver resident CD4 T cells were found to be enriched with effector memory phenotype CXCR3+CD62LlowCD4+ T cells. Second, the use of CD4 blocking Ab to prevent CD4 TCR-mediated activation without concomitant cell depletion has documented de novo CD4 T cell activation is not required for their function in liver IRI (37). Third, allo-Ag sensitized hosts were characterized by enhanced CD4 T cell-mediated liver immune response against IR (38). Fourth, RAG deficient TCR transgenic mice with fewer effector T cells suffered a less severe liver IR damage (39). Finally, our own studies using OT II system confirm higher potency of OVA-activated OT II T cells to promote liver immune response against IR, as compared with naïve counterparts (Zhai, unpublished data).
CD4 T cells can differentiate into multiple types of Th1, Th2, Th17 or Treg effectors. Our adaptive T cell transfer study indicates a more profound effect of Stat4-dependent Th cells in nude mice, consistent with the pathogenic role of Th1 cells in the mechanism of liver IRI (40). Putative role of Th17 or Treg cells, seen in other organ damage models (41–43), remains to be determined in liver IRI. It is also unknown as to how CD4 T cells may function in liver IRI. Our recent studies suggest a possible reverse CD154-CD40 costimulatory function between CD4 T cells and macrophages in the mechanism of IR-liver innate immune activation (37). Thus, livers are largely protected against IRI following CD154 blockade in WT mice or in nude mice reconstituted with CD154-deficient CD4 T cells. However, agonist anti-CD40 readily restored liver injury in CD4 KO mice. At the same time, IFN-γ does not seem critical in the early IRI phase, as no significant improvement in the liver function was observed in IFN-γ receptor-deficient mice, or following neutralization of IFN-γ in WT recipients. CD40 signaling has been shown to synergize with various TLR ligands to facilitate full “pro-inflammatory” activation phenotype in DC and macrophages, in particular, the elaboration of functional IL-12p70 complex (44). Interestingly, T cell - macrophage interactions may trigger multiple signaling pathways, and the engagement of PD-1 and PD-L1 has been shown to promote liver cytoprotection (27). Thus, different types of T cells or same T cells at different stages of the disease may regulate liver innate immune activation and IRI differently by distinctive pathways. Of note, most of these studies focused on the activation of liver immune response at the early reperfusion phase (0–6 h), and findings may not necessarily hold to the late phase of the disease, when different liver immune cell types dominate the process.
As in the case of TLR9 signaling in PMNs discussed above, NK and NKT cells may play phase-specific roles in the course of liver IRI. Although depletion of NK1.1 cells (NK and NKT) fails to affect the severity of reperfusion injury at the early time-points (37), it significantly reduces the hepatocellular damage in the later phase (45). By suppressing IL-10 production in synergy with TLR ligands, IFN-γ, produced mostly by NK and NKT cells, becomes critically important by 24 h of reperfusion. IR-triggered activation of NKT cells (comprise almost 50% of liver T cells) is mediated by CD1d, which is expressed by most liver cells and present glycolipid Ags, released possibly by necrotic cells, to NKT cell invariant TCRs. Interestingly, NKT cell function can be shut-down after adenosine (P1) A2A receptor engagement (45). Furthermore, NKT cells are heterogeneous, and analogous to T cells, different NKT cell subsets may play distinctive in vivo roles. Indeed, type II NKT cells prevented liver IRI when activated by their specific glycolipid ligand sulfatide (46). The activation of NK cells during IR is dependent on CD39, which is an ectonucleotidase to hydrolyze ADP to AMP. Thus, CD39 deficient livers were resistant to IRI, and IFN-γ production by their NK cells was diminished, possibly due to P2 receptor activation (47). This might be a cell-type or organ specific effect, as selective expression of CD39 on endothelial cells was protective in the kidney and cardiac IRI models (48, 49). Thus, T cells, NKT cells and NK cells are all involved, possibly at different stages of reperfusion, in liver IR innate immune activation by providing either costimulatory signaling via direct cell-cell interactions or via cytokine stimulation to KCs and/or DCs. This, in turn, promotes the pro-inflammatory phenotype of the liver immune response by augmenting IL-12 or inhibiting IL-10 production.
Conclusion
This review focuses on the mechanisms of liver innate immune activation during IR. We are aware that the effector mechanisms in the hepatocellular damage, local cytoprotective functions, and immune regulation of hepatic metabolic pathways, are all critically involved in the pathogenesis of liver IRI. Despite their distinctive roles in a variety of liver cells, these pathways may crosstalk with each other and function in synergistic or counteractive fashion. Our better appreciation of cellular interactions, as well as molecular signaling pathways that mediate these intricate cascades, should allow for the development of much needed novel therapeutic approaches aimed at ameliorating IRI and its adverse consequences in liver transplant recipients.
List of Abbreviations
- DAMP
damage-associated molecular pattern
- DC
dendritic cell
- HMGB1
high mobility group box-1
- IR
ischemia/reperfusion
- IRI
ischemia/reperfusion injury
- KC
Kupffer cell
- MyD88
Myeloid differentiation primary response gene (88)
- NPC
non-parenchymal cell
- OLT
orthotopic liver transplantation
- PAMP
pathogen-associated molecular pattern
- PC
parenchymal cell
- PD-1
Program death-1
- PMN
polymorphonuclear leukocyte
- SEC
sinusoidal endothelial cells
- RAGE
receptor for advanced glycation end products
- TLR
Toll-like receptor
Footnotes
Disclosure
The authors of this manuscript have no conflicts of interest to disclose, as described by the American Journal of Transplantation.
References
- 1.Fondevila C, Busuttil RW, Kupiec-Weglinski JW. Hepatic ischemia/reperfusion injury--a fresh look. Exp Mol Pathol. 2003;74(2):86–93. doi: 10.1016/s0014-4800(03)00008-x. [DOI] [PubMed] [Google Scholar]
- 2.Henderson JM. Liver transplantation and rejection: an overview. Hepato-Gastroenterol. 1999;46 (Suppl 2):1482–1484. [PubMed] [Google Scholar]
- 3.Howard TK, Klintmalm GB, Cofer JB, Husberg BS, Goldstein RM, Gonwa TA. The influence of preservation injury on rejection in the hepatic transplant recipient. Transplantation. 1990;49(1):103–107. doi: 10.1097/00007890-199001000-00023. [DOI] [PubMed] [Google Scholar]
- 4.Ikeda T, Yanaga K, Kishikawa K, Kakizoe S, Shimada M, Sugimachi K. Ischemic injury in liver transplantation: difference in injury sites between warm and cold ischemia in rats. Hepatology. 1992;16(2):454–461. doi: 10.1002/hep.1840160226. [DOI] [PubMed] [Google Scholar]
- 5.Huet PM, Nagaoka MR, Desbiens G, Tarrab E, Brault A, Bralet MP, et al. Sinusoidal endothelial cell and hepatocyte death following cold ischemia-warm reperfusion of the rat liver. Hepatology. 2004;39(4):1110–1119. doi: 10.1002/hep.20157. [DOI] [PubMed] [Google Scholar]
- 6.Shen XD, Gao F, Ke B, Zhai Y, Lassman CR, Tsuchihashi S, et al. Inflammatory responses in a new mouse model of prolonged hepatic cold ischemia followed by arterialized orthotopic liver transplantation. Liver Transpl. 2005;11(10):1273–1281. doi: 10.1002/lt.20489. [DOI] [PubMed] [Google Scholar]
- 7.Tsung A, Hoffman RA, Izuishi K, Critchlow ND, Nakao A, Chan MH, et al. Hepatic ischemia/reperfusion injury involves functional TLR4 signaling in nonparenchymal cells. J Immunol. 2005;175(11):7661–7668. doi: 10.4049/jimmunol.175.11.7661. [DOI] [PubMed] [Google Scholar]
- 8.Zhai Y, Shen XD, O’Connell R, Gao F, Lassman C, Busuttil RW, et al. Cutting edge: TLR4 activation mediates liver ischemia/reperfusion inflammatory response via IFN regulatory factor 3-dependent MyD88-independent pathway. J Immunol. 2004;173(12):7115–7119. doi: 10.4049/jimmunol.173.12.7115. [DOI] [PubMed] [Google Scholar]
- 9.Tsung A, Klune JR, Zhang X, Jeyabalan G, Cao Z, Peng X, et al. HMGB1 release induced by liver ischemia involves Toll-like receptor 4 dependent reactive oxygen species production and calcium-mediated signaling. J Exp Med. 2007;204(12):2913–2923. doi: 10.1084/jem.20070247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hui W, Jinxiang Z, Heshui W, Zhuoya L, Qichang Z. Bone marrow and non-bone marrow TLR4 regulates hepatic ischemia/reperfusion injury. Biochemical and biophysical research communications. 2009;389(2):328–332. doi: 10.1016/j.bbrc.2009.08.149. [DOI] [PubMed] [Google Scholar]
- 11.Hreggvidsdottir HS, Ostberg T, Wahamaa H, Schierbeck H, Aveberger AC, Klevenvall L, et al. The alarmin HMGB1 acts in synergy with endogenous and exogenous danger signals to promote inflammation. J Leukoc Biol. 2009;86(3):655–662. doi: 10.1189/jlb.0908548. [DOI] [PubMed] [Google Scholar]
- 12.Qin YH, Dai SM, Tang GS, Zhang J, Ren D, Wang ZW, et al. HMGB1 enhances the proinflammatory activity of lipopolysaccharide by promoting the phosphorylation of MAPK p38 through receptor for advanced glycation end products. J Immunol. 2009;183(10):6244–6250. doi: 10.4049/jimmunol.0900390. [DOI] [PubMed] [Google Scholar]
- 13.Zeng S, Dun H, Ippagunta N, Rosario R, Zhang QY, Lefkowitch J, et al. Receptor for advanced glycation end product (RAGE)-dependent modulation of early growth response-1 in hepatic ischemia/reperfusion injury. J Hepatol. 2009;50(5):929–936. doi: 10.1016/j.jhep.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 14.Zeng S, Feirt N, Goldstein M, Guarrera J, Ippagunta N, Ekong U, et al. Blockade of receptor for advanced glycation end product (RAGE) attenuates ischemia and reperfusion injury to the liver in mice. Hepatology. 2004;39(2):422–432. doi: 10.1002/hep.20045. [DOI] [PubMed] [Google Scholar]
- 15.Bamboat ZM, Balachandran VP, Ocuin LM, Obaid H, Plitas G, DeMatteo RP. Toll-like receptor 9 inhibition confers protection from liver ischemia-reperfusion injury. Hepatology. 2010;51(2):621–632. doi: 10.1002/hep.23365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cavassani KA, Ishii M, Wen H, Schaller MA, Lincoln PM, Lukacs NW, et al. TLR3 is an endogenous sensor of tissue necrosis during acute inflammatory events. J Exp Med. 2008;205(11):2609–2621. doi: 10.1084/jem.20081370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crispe IN. The liver as a lymphoid organ. Annual Review of Immunology. 2009;27:147–163. doi: 10.1146/annurev.immunol.021908.132629. [DOI] [PubMed] [Google Scholar]
- 18.Gao B, Jeong WI, Tian Z. Liver: An organ with predominant innate immunity. Hepatology. 2008;47(2):729–736. doi: 10.1002/hep.22034. [DOI] [PubMed] [Google Scholar]
- 19.West XZ, Malinin NL, Merkulova AA, Tischenko M, Kerr BA, Borden EC, et al. Oxidative stress induces angiogenesis by activating TLR2 with novel endogenous ligands. Nature. 2010;467(7318):972–976. doi: 10.1038/nature09421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khandoga A, Hanschen M, Kessler JS, Krombach F. CD4+ T cells contribute to postischemic liver injury in mice by interacting with sinusoidal endothelium and platelets. Hepatology. 2006;43(2):306–315. doi: 10.1002/hep.21017. [DOI] [PubMed] [Google Scholar]
- 21.Schrage A, Wechsung K, Neumann K, Schumann M, Schulzke JD, Engelhardt B, et al. Enhanced T cell transmigration across the murine liver sinusoidal endothelium is mediated by transcytosis and surface presentation of chemokines. Hepatology. 2008;48(4):1262–1272. doi: 10.1002/hep.22443. [DOI] [PubMed] [Google Scholar]
- 22.McDonald B, Pittman K, Menezes GB, Hirota SA, Slaba I, Waterhouse CC, et al. Intravascular danger signals guide neutrophils to sites of sterile inflammation. Science. 2010;330(6002):362–366. doi: 10.1126/science.1195491. [DOI] [PubMed] [Google Scholar]
- 23.Zhu P, Duan L, Chen J, Xiong A, Xu Q, Zhang H, et al. Gene Silencing of NALP3 Protects Against Liver Ischemia-Reperfusion Injury in Mice. Hum Gene Ther. 2011 doi: 10.1089/hum.2010.145. [DOI] [PubMed] [Google Scholar]
- 24.Kato A, Okaya T, Lentsch AB. Endogenous IL-13 protects hepatocytes and vascular endothelial cells during ischemia/reperfusion injury. Hepatology. 2003;37(2):304–312. doi: 10.1053/jhep.2003.50075. [DOI] [PubMed] [Google Scholar]
- 25.Kato A, Yoshidome H, Edwards MJ, Lentsch AB. Reduced hepatic ischemia/reperfusion injury by IL-4: potential anti-inflammatory role of STAT6. Inflamm Res. 2000;49(6):275–279. doi: 10.1007/PL00000207. [DOI] [PubMed] [Google Scholar]
- 26.Yoshidome H, Kato A, Miyazaki M, Edwards MJ, Lentsch AB. IL-13 activates STAT6 and inhibits liver injury induced by ischemia/reperfusion. Am J Pathol. 1999;155(4):1059–1064. doi: 10.1016/S0002-9440(10)65208-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ji H, Shen X, Gao F, Ke B, Freitas MC, Uchida Y, et al. Programmed death-1/B7-H1 negative costimulation protects mouse liver against ischemia and reperfusion injury. Hepatology. 2010;52(4):1380–1389. doi: 10.1002/hep.23843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhai Y, Shen XD, Gao F, Zhao A, Freitas MC, Lassman C, et al. CXCL10 regulates liver innate immune response against ischemia and reperfusion injury. Hepatology. 2008;47(1):207–214. doi: 10.1002/hep.21986. [DOI] [PubMed] [Google Scholar]
- 29.Saraiva M, O’Garra A. The regulation of IL-10 production by immune cells. Nat Rev Immunol. 2010;10(3):170–181. doi: 10.1038/nri2711. [DOI] [PubMed] [Google Scholar]
- 30.Zhang X, Majlessi L, Deriaud E, Leclerc C, Lo-Man R. Coactivation of Syk kinase and MyD88 adaptor protein pathways by bacteria promotes regulatory properties of neutrophils. Immunity. 2009;31(5):761–771. doi: 10.1016/j.immuni.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 31.Ellett JD, Atkinson C, Evans ZP, Amani Z, Balish E, Schmidt MG, et al. Murine Kupffer cells are protective in total hepatic ischemia/reperfusion injury with bowel congestion through IL-10. J Immunol. 2010;184(10):5849–5858. doi: 10.4049/jimmunol.0902024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Knolle P, Schlaak J, Uhrig A, Kempf P, Meyer zum Buschenfelde KH, Gerken G. Human Kupffer cells secrete IL-10 in response to lipopolysaccharide (LPS) challenge. J Hepatol. 1995;22(2):226–229. doi: 10.1016/0168-8278(95)80433-1. [DOI] [PubMed] [Google Scholar]
- 33.Bamboat ZM, Ocuin LM, Balachandran VP, Obaid H, Plitas G, DeMatteo RP. Conventional DCs reduce liver ischemia/reperfusion injury in mice via IL-10 secretion. J Clin Invest. 2010;120(2):559–569. doi: 10.1172/JCI40008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsung A, Zheng N, Jeyabalan G, Izuishi K, Klune JR, Geller DA, et al. Increasing numbers of hepatic dendritic cells promote HMGB1-mediated ischemia-reperfusion injury. J Leukoc Biol. 2007;81(1):119–128. doi: 10.1189/jlb.0706468. [DOI] [PubMed] [Google Scholar]
- 35.Caldwell CC, Tschoep J, Lentsch AB. Lymphocyte function during hepatic ischemia/reperfusion injury. J Leukoc Biol. 2007 doi: 10.1189/jlb.0107062. [DOI] [PubMed] [Google Scholar]
- 36.Geginat J, Sallusto F, Lanzavecchia A. Cytokine-driven proliferation and differentiation of human naive, central memory, and effector memory CD4(+) T cells. The Journal of experimental medicine. 2001;194(12):1711–1719. doi: 10.1084/jem.194.12.1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shen X, Wang Y, Gao F, Ren F, Busuttil RW, Kupiec-Weglinski JW, et al. CD4 T cells promote tissue inflammation via CD40 signaling without de novo activation in a murine model of liver ischemia/reperfusion injury. Hepatology. 2009;50(5):1537–1546. doi: 10.1002/hep.23153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shen X, Reng F, Gao F, Uchida Y, Busuttil RW, Kupiec-Weglinski JW, et al. Alloimmune activation enhances innate tissue inflammation/injury in a mouse model of liver ischemia/reperfusion injury. Am J Transplant. 2010;10(8):1729–1737. doi: 10.1111/j.1600-6143.2010.03205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kuboki S, Sakai N, Tschop J, Edwards MJ, Lentsch AB, Caldwell CC. Distinct contributions of CD4+ T cell subsets in hepatic ischemia/reperfusion injury. Am J Physiol Gastrointest Liver Physiol. 2009;296(5):G1054–1059. doi: 10.1152/ajpgi.90464.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shen XD, Ke B, Zhai Y, Gao F, Anselmo D, Lassman CR, et al. Stat4 and Stat6 signaling in hepatic ischemia/reperfusion injury in mice: HO-1 dependence of Stat4 disruption-mediated cytoprotection. Hepatology. 2003;37(2):296–303. doi: 10.1053/jhep.2003.50066. [DOI] [PubMed] [Google Scholar]
- 41.Gandolfo MT, Jang HR, Bagnasco SM, Ko GJ, Agreda P, Satpute SR, et al. Foxp3+ regulatory T cells participate in repair of ischemic acute kidney injury. Kidney Int. 2009;76(7):717–729. doi: 10.1038/ki.2009.259. [DOI] [PubMed] [Google Scholar]
- 42.Marks BR, Nowyhed HN, Choi JY, Poholek AC, Odegard JM, Flavell RA, et al. Thymic self-reactivity selects natural interleukin 17-producing T cells that can regulate peripheral inflammation. Nat Immunol. 2009;10(10):1125–1132. doi: 10.1038/ni.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zheng Y, Danilenko DM, Valdez P, Kasman I, Eastham-Anderson J, Wu J, et al. Interleukin-22, a T(H)17 cytokine, mediates IL-23-induced dermal inflammation and acanthosis. Nature. 2007;445(7128):648–651. doi: 10.1038/nature05505. [DOI] [PubMed] [Google Scholar]
- 44.Abdi K, Singh NJ. Antigen-activated T cells induce IL-12p75 production from dendritic cells in an IFN-gamma-independent manner. Scand J Immunol. 2010;72(6):511–521. doi: 10.1111/j.1365-3083.2010.02467.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lappas CM, Day YJ, Marshall MA, Engelhard VH, Linden J. Adenosine A2A receptor activation reduces hepatic ischemia reperfusion injury by inhibiting CD1d-dependent NKT cell activation. J Exp Med. 2006;203(12):2639–2648. doi: 10.1084/jem.20061097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Arrenberg P, Maricic I, Kumar V. Sulfatide-mediated activation of type II natural killer T cells prevents hepatic ischemic reperfusion injury in mice. Gastroenterology. 2011;140(2):646–655. doi: 10.1053/j.gastro.2010.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Beldi G, Banz Y, Kroemer A, Sun X, Wu Y, Graubardt N, et al. Deletion of CD39 on natural killer cells attenuates hepatic ischemia/reperfusion injury in mice. Hepatology. 2010;51(5):1702–1711. doi: 10.1002/hep.23510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Crikis S, Lu B, Murray-Segal LM, Selan C, Robson SC, D’Apice AJ, et al. Transgenic overexpression of CD39 protects against renal ischemia-reperfusion and transplant vascular injury. Am J Transplant. 2010;10(12):2586–2595. doi: 10.1111/j.1600-6143.2010.03257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kohler D, Eckle T, Faigle M, Grenz A, Mittelbronn M, Laucher S, et al. CD39/ectonucleoside triphosphate diphosphohydrolase 1 provides myocardial protection during cardiac ischemia/reperfusion injury. Circulation. 2007;116(16):1784–1794. doi: 10.1161/CIRCULATIONAHA.107.690180. [DOI] [PubMed] [Google Scholar]