Abstract
Context:
A wire-reinforced silicone tube (LMA-Fastrach™ endotracheal tube) is specially designed for tracheal intubation using intubating laryngeal mask airway (ILMA). However, conventional polyvinyl chloride (PVC) tracheal tubes have also been used with ILMA to achieve tracheal intubation successfully.
Aim:
To evaluate the success of tracheal intubation using the LMA-Fastrach™ tracheal tube versus conventional PVC tracheal tube through ILMA.
Settings and Design:
Two hundred adult ASA physical status I/II patients, scheduled to undergo elective surgery under general anaesthesia requiring intubation, were randomly allocated into two groups.
Methods:
The number of attempts, time taken, and manoeuvres employed to accomplish tracheal intubation were compared using conventional PVC tubes (group I) and LMA-Fastrach™ wire-reinforced silicone tubes (group II). Intraoperative haemodynamic changes and evidence of trauma and postoperative incidence of sore throat and hoarseness, were compared between the groups.
Statistical Analysis:
The data was analyzed using two Student's t test and Chi-square test for demographics and haemodynamic parameters. Mann Whitney U test was used for comparison of time taken for endotracheal tube insertion. Fisher's exact test was used to compare postoperative complications.
Results:
Rate of successful tracheal intubation and haemodynamic variables were comparable between the groups. Time taken for tracheal intubation and manoeuvres required to accomplish successful endotracheal intubation, however, were significantly greater in group I than group II (14.71±6.21 s and 10.04±4.49 s, respectively (P<0.001), and 28% in group I and 3% in group II, respectively (P<0.05)).
Conclusion:
Conventional PVC tube can be safely used for tracheal intubation through the ILMA.
Keywords: Fastrach, intubating laryngeal mask airway, polyvinyl chloride, tracheal intubation
INTRODUCTION
A dedicated wire-reinforced silicone (WRS) endotracheal tube (ETT) is advocated for intubation through the LMA-Fastrach™.[1] The unique characteristics of this tube are the straight alignment, wire reinforcement, and presence of a conical Touhy-like tip made of silicone, which is less traumatic than conventional ETT. However, the low volume, high-pressure cuff of this tube makes it less suitable for prolonged use. Also, it is very expensive and not so easily available. Moreover, wire reinforcement may be disadvantageous, as ventilation may be hampered due to distortion of the lumen if the patient bites on the tube. A conventional PVC ETT besides being disposable is cheaper, easily available, and has high volume low pressure cuff, which is more suitable for prolonged ventilation.
However, with PVC ETT, there are concerns of decreased chances of entry into the glottis and airway trauma, due to its relative stiffness and also because the tip points anteriorly on emergence from the ILMA.
Despite these concerns, the conventional PVC tube has been used successfully for tracheal intubation through the ILMA.[2–9] In most of these studies, the PVC tube has been inserted either with the reverse curve anteriorly, pre-warmed or under fiberoptic guidance. None of these studies (except Lu et al.) compared the haemodynamic variables between the PVC and silicone tube groups.[7]
The present study was designed to compare the ease of insertion through the ILMA of LMA-Fastrach™ ETT with the conventional PVC tube to evaluate the feasibility of using PVC tube through the ILMA. The ease of insertion was evaluated by comparing the number of attempts, time taken, and manoeuvres employed to accomplish tracheal intubation using conventional PVC tubes (group I) versus LMA-Fastrach™ wire-reinforced silicone tubes (group II) (primary outcome). Haemodynamic changes, incidence of sore throat, hoarseness, and evidence of trauma were also compared between the groups (secondary outcome).
METHODS
This study was conducted on 200 adult ASA I and II patients of either sex, scheduled for elective surgery requiring general anaesthesia, with endotracheal intubation between April 2007 and October 2008 at tertiary care hospital. After approval by the institutional ethics committee, patients with Mallampati grade I and II and interdental distance more than 2 cm on pre-anesthetic assessment were included in the study. Written informed consent was obtained from all the patients. Exclusion criteria included patients with loose dentures, hypertrophied tonsils (grade 3 and 4), thyroid enlargement, morbid obesity, respiratory tract pathology, previous upper gastrointestinal (GI) surgery, or pathology. All patients were kept fasting overnight and were pre-medicated with tablet alprazolam 0.25 mg and tablet ranitidine 150 mg with sips of water, night before and on the morning of surgery.
In the operating room, an intravenous infusion was started with normal saline, and patients were randomly allocated to one of the two groups: Group I (n = 100): Cuffed PVC tube (Portex Inc. Keene, USA) and group II (n = 100): LMA Fastrach™ WRS ETT (The Laryngeal Mask Company, UK) by sealed envelope method. Standard monitors were applied, and baseline parameters like heart rate (HR), arterial oxygen saturation (SpO2), and non-invasive blood pressure (NIBP) were recorded. Patients were pre-oxygenated for 3 minutes, and anaesthesia was induced with fentanyl 2 μg.kg-1 and propofol 2 mg.kg-1 intravenously (IV). Muscle relaxation was facilitated with vecuronium 0.1 mg.kg-1 IV. When patient was fully relaxed, with the head in neutral position, an appropriate-sized ILMA was inserted with cuff deflated, after which the cuff was inflated with air as per recommendations.[10] Correct placement was confirmed by the ability to ventilate without leak at an airway pressure of ≤20 cm of H2O and a square-wave capnograph tracing during gentle manual ventilation. To ensure optimal positioning, ILMA adjustments like extension of ILMA handle/up and down movement/optimization manoeuvre/head-neck maneuver, rotation in the sagittal plane, or lifting away from the posterior pharyngeal wall (Chandy maneuver) were allowed. Thereafter, a well-lubricated size 7.0 or 7.5 mm ID cuffed PVC or WRS ETT, according to the group assignment, was passed through the metal tube of the ILMA. The tube was inserted till 16 cm depth (the distance to the epiglottis elevating bar). It was then gently advanced into the trachea without applying undue force, the cuff was inflated, and the circuit connected. Correct tube placement was confirmed by capnography and the presence of bilateral breath sounds. The ILMA was then deflated and removed using the designated stabilizing rod to maintain the tube in place, which was then reconnected to the breathing circuit.
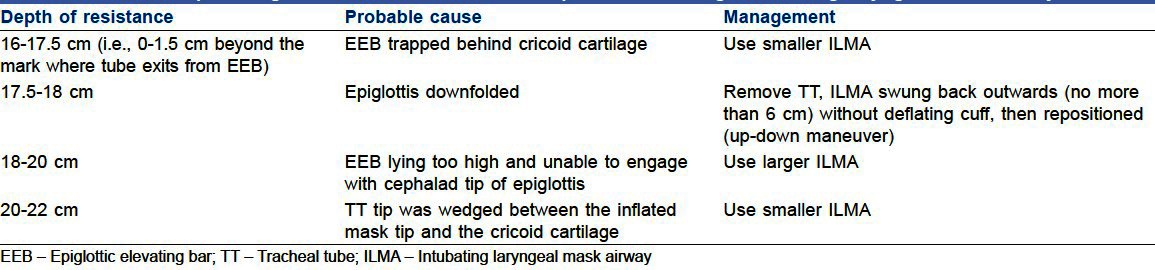
However, if the tracheal tube placement was unsuccessful, then an optimizing maneuver was employed with each attempt according to the level, at which resistance was felt [Table 1]. A maximum of 3 attempts were allowed. In case of failure after 3 attempts, alternative method of securing the airway using direct laryngoscopy was used. Tracheal intubation was considered to have failed if it was not accomplished in 3 attempted adjustment manoeuvres. All ILMA placements and tracheal intubations were performed by the same anesthesiologist. After intubation, anaesthesia was maintained with end-tidal isoflurane 0.5-1% and 66% N2O in oxygen using closed circuit with controlled ventilation.
Table 1.
Optimizing maneuvers for tracheal tube placement through Intubating laryngeal mask airway
HR, SpO2, NIBP, and EtCO2 were monitored continuously during the procedure. These parameters were recorded at 1-minute interval after successful tracheal intubation for 5 consecutive minutes. Thereafter, they were recorded every 5 minutes till 15 minutes after successful tracheal intubation. After extubation, all patients were evaluated for sore throat and hoarseness of voice during the first 24 hours on a descriptive scale (none, mild, moderate, or severe). The observer was blinded to the group allocation, and the observations were made at 1, 2, 4, 12, and 24 hours post-extubation.
The number of attempts to achieve successful tracheal insertion, time consumed, and the adjustment manoeuvres employed for successful intubation were compared between the two groups. Time taken for intubation was defined as the time from disconnection of breathing circuit from the ILMA to the time to successful tracheal intubation as confirmed by capnography and the presence of bilateral breath sounds. The minimum value of arterial oxygen saturation levels during the procedure and any adverse intra-operative events were also noted. Haemodynamic and ventilatory parameters were recorded and compared between the two groups at 5, 10, and 15 minutes after intubation. The data were analyzed using Student's ‘t’ test and chi square test to compare demographic data, haemodynamic parameters (HR, systolic blood pressure (SBP), diastolic blood pressure (DBP)), SpO2, and EtCO2. For comparison of time taken for ETT insertion, Mann Whitney U test was used. Fisher's exact test was used to compare incidence and degree of sore throat and hoarseness. For a confidence interval of 95%, a sample size of 100 patients in each group was calculated to detect a power of more than 90%. This was derived based on difference in success rate, and the estimation was done on the basis of a pilot study. For all analyses, P<0.05 was considered statistically significant.
RESULTS
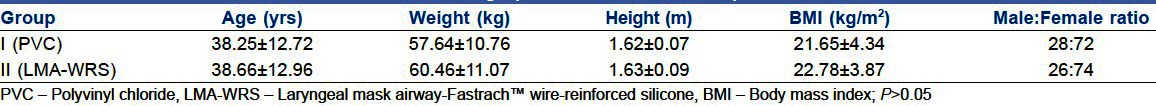
The age, weight, gender distribution, and body mass index (BMI) were comparable in both the groups [Table 2].
Table 2.
Demographic characteristics of patients
In group I, 96% patients were successfully intubated (90% in the 1st attempt, 5% in the 2nd attempt, and 1% in the 3rd attempt). In group II, the success rate was 97% (95% in 1st attempt and 2% in 2nd attempt) [Table 3]. The difference between the two groups was clinically and statistically insignificant. The mean time for successful tracheal intubation was significantly higher in group I than in group II (14.71 s and 10.04 s, respectively, [Table 4]. Adjustment manoeuvres were significantly higher in group I (28%) than in group II (3%) [Table 4] HR, NIBP, SpO2, and EtCO2 between the two groups were comparable at all times [Figure 1]. The lowest SpO2 was comparable in the two groups, and at no time, the SpO2 fell below 95% for any patient in either group. Three patients in each group had trauma to the airway as evidenced by blood on ILMA cuff. Esophageal intubation during attempt to tracheal intubation through the ILMA occurred in 2 patients in group I and 3 patients in group II. The difference in the incidence of trauma and esophageal intubation between the two groups was insignificant. Although the incidence and degree of sore throat and hoarseness was higher in group I (10%) than in group II (4%), it was statistically insignificant.
Table 3.
Successful endotracheal tube insertion through Intubating laryngeal mask airway-number of attempts
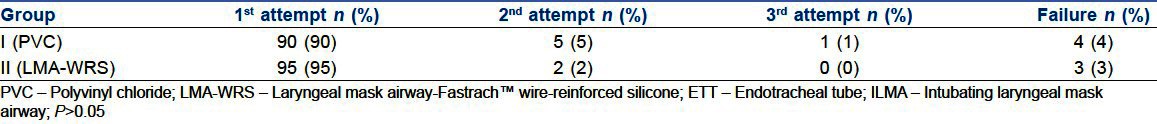
Table 4.
Time taken and Adjustment maneuvers for endotracheal tube insertion through Intubating laryngeal mask airway
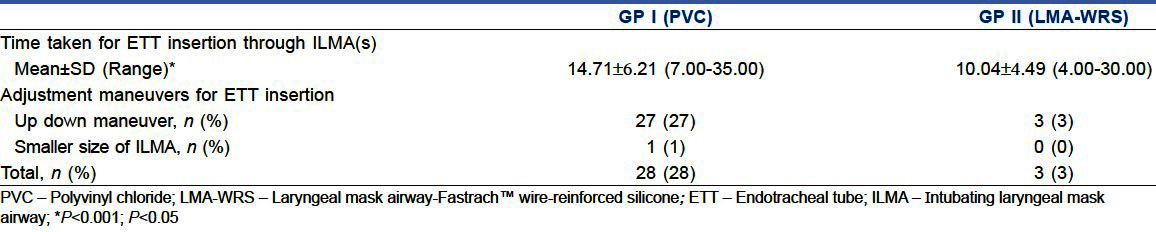
Figure 1.
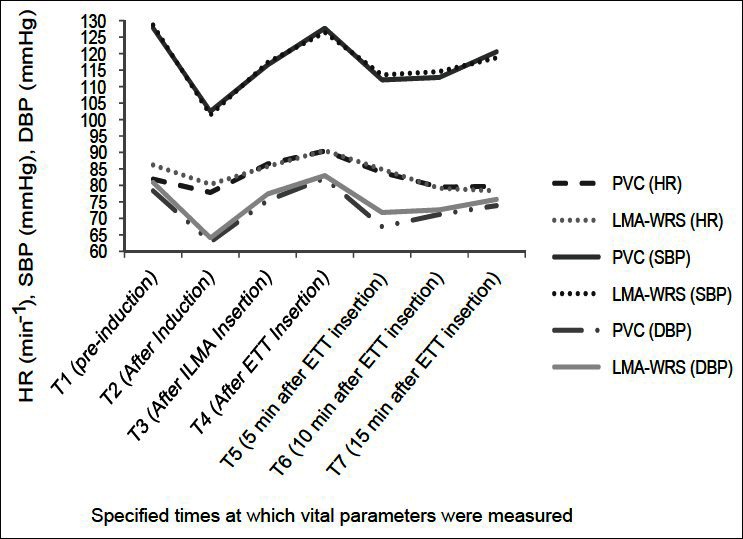
Heart rate, systolic BP, and diastolic BP at specified times
DISCUSSION
The WRS tube dedicated for tracheal intubation through ILMA has a low volume and high pressure cuff besides being more expensive than conventional PVC tube. Conventional disposable PVC tube with the advantages of high volume low pressure cuff and low cost has been used for intubation through ILMA with varied results.[2–9] The difficulties with conventional tube are probably due to more obtuse angle of the tip of tracheal tube, at which it emerges from the ILMA cuff compared to the silicone tube resulting in increased impingement of the tip of the PVC tube against the anterior part of larynx. This non-alignment of the axes of the trachea and the tube may be responsible for increased incidence of failed intubation and trauma.[1,3]
Our results are in contrast with those of Kanazi et al. who compared the ease of intubation using WRS tube, Parker tube, and PVC tube through the ILMA.[5] They reported a success rate of 90%, 54%, and 48%, respectively, for the 3 groups without the use of manipulations and 90%, 86%, and 57%, respectively, with manipulations. The difference could be attributed to limited clinical experience in using PVC tubes with ILMA and the small sample size in their study. Further, in their study, it has not been mentioned whether the same person performed all the intubations and no fixed criterion for ILMA size selection was followed.
Difference in tracheal insertion time between the two groups in our study was statistically significant but not clinically relevant (14.71 s and 10.04 s in group I and group II, respectively). No significant difference in the mean insertion time between the study groups was observed by Kundra et al.[3] Insertion time in their study was lesser in PVC group (11.8 s) than in silicone group (12.9 s), which can be attributed to pre-warming of the PVC tube before insertion.
Joo et al. reported longer intubation time of 23 s (median value) (18-35.8 s) in their ILMA blind intubation group.[2] This could be due to the PVC tube insertion with the reverse curvature facing forwards. Greater use of adjusting manoeuvres to facilitate intubation in our study may have contributed to lower insertion time.
We employed a combination of several adjustment manoeuvres described by various authors.[11–13] Adjustment manoeuvres as described by Kihara et al. Ferson et al. were employed to ensure optimal ILMA placement.[11,12] While Kihara et al. employed extension maneuver/up-down maneuver/optimization maneuver/head-neck maneuver in sequence at the time of ETT insertion, we employed these manoeuvres to ensure optimal ILMA placement even before attempting ETT insertion (along with Chandy maneuver).[11] Chandy maneuver consists of 2 sequential steps to aid correct positioning of ILMA and thus facilitate intubation. First step is slight rotation of ILMA in sagittal plane until least resistance to bag ventilation is achieved (important for optimization of ventilation). Second step is slight lift (not tilt) of the ILMA away from posterior pharyngeal wall just before attempting tracheal intubation.[12] When there was resistance to tracheal tube insertion, manoeuvres were employed according to the level, at which resistance was felt, as described by Brain et al.[13]
In the present study, HR, SBP, DBP, SpO2, and EtCO2 between the two groups were comparable at all times. Lowest value of SpO2 did not fall below 95% at any time in either group. Lu et al. also reported no significant haemodynamic changes in patients with ankylosing spondylitis intubated with PVC tube through ILMA.[7] To the best of our knowledge, this is the first study to evaluate haemodynamic variables in patients with normal airways, intubated using PVC tube and LMA-WRS tube through ILMA.
Incidence of esophageal intubation in both our groups was similar to that reported by Kundra et al. (1.8%) in their PVC group. However, the incidence of esophageal intubation in their WRS group was higher (7.4%). Also, the incidence of airway trauma reported by Kundra et al. is[3] much higher (8% and 14% patients in LMA-WRS and PVC groups, respectively) compared to our results where only 3% patients in each group had airway trauma. This may be because they used only the 1st step of Chandy's maneuver while we used as many as 6 manoeuvres to optimally place the ILMA. This could have resulted in better ILMA positioning, which was closer to ideal for ventilation as well as for intubation.
The incidence and degree of sore throat and hoarseness in the present study was more in the patients who required more number of attempts, which is consistent with the observations of Lu et al. and Kundra et al.[3,6] Higher incidence of sore throat reported by Zhu et al. (26% and 19% with normal and reverse curved PVC tubes)[4] may be due to lower success rate in their two groups (84% and 90%, respectively) that required more intubation attempts.
There are certain limitations in our study. First, the results of our study are applicable only to patients with normal airway. Secondly, a good mask-larynx relationship was ascertained only clinically and not with fiberscope. Furthermore, blinding was not possible during intra-operative period (observer bias in post-operative period was minimized, as post-operative complications were studied by a blinded observer).
CONCLUSION
The less expensive and readily available Portex PVC tube is a feasible option to the WRS tube for intubation through the ILMA in patients with normal airway. However, further studies are suggested to assess the feasibility of using a PVC tube through ILMA in patients with anticipated difficult airways.
Footnotes
Source of Support: Institutional (Government Medical College and Hospital, Chandigarh, India)
Conflict of Interest: None declared
REFERENCES
- 1.Brain AI, Verghese C, Addy EV, Kapila A. The intubating laryngeal mask I: Development of a new device for intubation of the trachea. Br J Anaesth. 1997;79:699–703. doi: 10.1093/bja/79.6.699. [DOI] [PubMed] [Google Scholar]
- 2.Joo HS, Rose DK. The intubating laryngeal mask airway with and without fibreoptic guidance. Anesth Analg. 1999;88:662–6. doi: 10.1097/00000539-199903000-00036. [DOI] [PubMed] [Google Scholar]
- 3.Kundra P, Sujata N, Ravishankar M. Conventional tracheal tubes for intubation through the intubating laryngeal mask airway. Anesth Analg. 2005;100:284–8. doi: 10.1213/01.ANE.0000139348.00435.33. [DOI] [PubMed] [Google Scholar]
- 4.Zhu T. Conventional endotracheal tubes for intubation through intubating laryngeal mask airway. Anesth Analg. 2007;104:213. doi: 10.1213/01.ane.0000249790.89467.af. [DOI] [PubMed] [Google Scholar]
- 5.Kanazi GE, El-Khatib M, Nasr VG, Kaddoum R, Al-Alami A, Baraka AS, et al. A comparison of a silicone wire-reinforced tube with the Parker and polyvinyl chloride tubes for tracheal intubation through an intubating laryngeal mask airway in patients with normal airways undergoing general anaesthesia. Anesth Analg. 2008;107:994–7. doi: 10.1213/ane.0b013e31817ef110. [DOI] [PubMed] [Google Scholar]
- 6.Lu PP, Yang CH, Ho AC, Shyr MH. The intubating LMA: A comparison of insertion techniques with conventional tracheal tubes. Can J Anesth. 2000;47:849–53. doi: 10.1007/BF03019663. [DOI] [PubMed] [Google Scholar]
- 7.Lu PP, Brimacombe J, Ho AC, Shyr MH, Liu HP. The intubating laryngeal mask airway in severe ankylosing spondylitis. Can J Anaesth. 2001;48:1015–9. doi: 10.1007/BF03016593. [DOI] [PubMed] [Google Scholar]
- 8.Ye L, Liu J, Wong DT, Zhu T. Effects of tracheal tube orientation on the success of intubation through an intubating laryngeal mask airway: Study in Mallampati class 3 or 4 patients. Br J Anaesth. 2009;102:269–72. doi: 10.1093/bja/aen365. [DOI] [PubMed] [Google Scholar]
- 9.Somboon T, Duenpen H, Malinee W, Polpun B, Thitima C, Suthannee S. An experience with intubating laryngeal mask airway for difficult airway management: Report on 38 Cases. J Med Assoc Thai. 2004;87:1234–8. [PubMed] [Google Scholar]
- 10.Brimacombe JR. Intubating LMA for airway intubation. In: Brimacombe JR, editor. Laryngeal Mask Anesthesia: Principles and practice. 2nd ed. Philadelphia: Saunders; 2005. pp. 469–505. [Google Scholar]
- 11.Kihara S, Watanabe S, Taguchi N, Suga S, Brimacombe JR. Tracheal intubation with the Macintosh laryngoscope versus intubating laryngeal mask airway in adults with normal airways. Anaesth Intensive Care. 2000;28:281–6. doi: 10.1177/0310057X0002800305. [DOI] [PubMed] [Google Scholar]
- 12.Ferson DZ, Rosenblatt WH, Johansen MJ, Osborn I, Ovassapian A. Use of the intubating LMA-Fastrach™ in 254 patients with difficult-to-manage airways. Anesthesiology. 2001;95:1175–81. doi: 10.1097/00000542-200111000-00022. [DOI] [PubMed] [Google Scholar]
- 13.Brain AI, Verghese C, Addy EV, Kapila A, Brimacombe JR. The intubating laryngeal mask II: A preliminary clinical report of a new means of intubating the trachea. Br J Anaesth. 1997;79:704–9. doi: 10.1093/bja/79.6.704. [DOI] [PubMed] [Google Scholar]


