Abstract
Background:
Hip strength is associated with numerous orthopaedic and neuromuscular injuries and/or pathologies and may be assessed with a variety of anatomic testing positions and techniques. Isokinetic dynamometers are generally too cumbersome and intricate for efficient use in mass screenings (for prognostic studies of risk for injury) as well as with special populations. The reliability of isometric testing devices has demonstrated varied reliability, generally examining only 1 or 2 motions of the hip and reporting values of force, not torque. Consequently, there is a need for an efficient hip strength-testing device to quantify torque that tests subjects in 1 anatomic position, while evaluating multiple hip motions.
Hypothesis:
Evaluation of supine hip abduction, adduction, flexion, and extension torque using a new stabilized dynamometer system will produce good to excellent intra- and interexaminer reliability results.
Study Design:
A blinded, randomized, repeated-measures study design was used in this descriptive laboratory investigation.
Methods:
Supine isometric hip flexion, extension, abduction, and adduction torques were evaluated with a cage-stabilized dynamometer in 19 collegiate and professional-level ice hockey athletes by 2 investigators at 3 time intervals. Inter- and intrarater reliability was assessed.
Results:
Supine hip flexion, extension, abduction, and adduction torque was performed with good to excellent inter- and intrarater reliability (intraclass correlation coefficients ranging from 0.74 to 0.92 and 0.78 to 0.92, respectively) for all motions tested.
Conclusions:
We have developed an isometric hip strength-testing device that can be assembled around an examination table to efficiently and reliably evaluate torque developed for multiple motions of the hip.
Clinical Relevance:
This device and testing protocol may be used to efficiently evaluate hip strength in numerous settings; it allows decreased subject burden and increased comfort (which may be important following an injury in case-control investigations); and it may be well tolerated when testing athletes as well as special populations in the clinical setting.
Keywords: isometric, hip joint, strength testing, dynamometry, torque
Hip muscle strength has been implicated as a risk factor for musculoskeletal injuries, such as noncontact anterior cruciate ligament (ACL) disruption, iliotibial band syndrome, patellofemoral pain syndrome, groin strain, chronic ankle instability, and low back pain.§ In addition, hip strength has been associated with the assessment or progression of various neuromuscular and/or orthopaedic conditions, such as osteoarthritis, postpartum posterior pelvic pain, muscular dystrophy, cerebral palsy, hip fracture, and fall risk in the elderly.6,19,25,29,30,35,37
Currently, the evaluation of strength using computerized isokinetic dynamometry is considered the gold standard for the assessment of strength of the muscles about the hip.33 Isokinetic devices, however, are expensive, immobile, and time intensive (ie, requiring individualized setup and testing protocols for each motion tested), and they involve substantial examiner training and practice to become proficient in their use. These issues are particularly problematic when evaluating strength of the muscles about the hip in the setting of prognostic studies and/or during preseason risk factor screening sessions that require time-efficient evaluation of a large number of subjects.
In the clinical setting, functional muscular strength is traditionally evaluated on a 5-point grading scale with the use of manual muscle testing (MMT). This technique involves a subjective assessment of the strength of an involved limb compared to its contralateral limb.18 The reliability of subjective MMT with larger muscle groups, such as those that span the hip, has been shown to be problematic in healthy individuals.12,14,22,31
A more efficient means by which a clinician may quantify a patient’s muscular strength can be accomplished through isometric testing using a handheld dynamometer. These commercially available devices are appealing to clinicians and scientists alike, as they are relatively inexpensive and portable and do not require substantial examiner training for their use. Their intra- and interexaminer reliability, however, is reported to be quite variable and is largely dependent on the physical strength of the examiner (especially when the subject is able to produce greater amounts of force than what the examiner can physically resist).23,32,34,40 Moreover, isometric testing is often limited to the evaluation of force at the point of load applications, rather than the torque developed about the joint under examination. The latter is more desirable and clinically relevant when evaluating strength of hip musculature in individuals with varying lever arm lengths, and it allows more appropriate comparisons of strength between individuals of different statures while not being dependent on placement of the resistive device on the limb relative to the joint’s center of rotation. Furthermore, there does not appear to be a single agreed-on position in which to test hip muscle strength.
The aforementioned limitations of isokinetic and isometric strength testing have led to the utilization of stabilized dynamometry to evaluate hip strength. Stabilized dynamometry is a strength-testing technique that “fixes” or “stabilizes” a force measurement device (commonly a load sensor or a commercially available handheld dynamometer) with the use of a custom-made stabilization cage, thereby removing any confounding variables that could be introduced by the examiner (eg, strength, stabilization technique, and orientation of the sensor relative to the position of the limb). Previous studies examining stabilized dynamometer systems have demonstrated reliable strength measurements of various hip motions assessed with subjects in different testing positions.3,5,11,20,26,32,39 Unfortunately, the majority of studies investigating the reliability of these systems for the evaluation of hip strength generally examine only 1 to 2 primary muscle groups of the hip (making subsequent agonist:antagonist ratio evaluations challenging), often using different testing positions for each hip motion tested (ie, prone extension and side-lying abduction).
For optimal efficiency and accuracy across diverse populations, assessment of hip strength in all anatomic planes would ideally be performed with subjects in a supine testing position. Hip strength testing in this position allows for adequate stabilization of the pelvic girdle, decreases ancillary motions about limb segments not involved with the evaluation, provides standardization of body position, aids in subject comfort (ie, assessment of bilateral side-lying hip abduction may be difficult for some subjects following acute knee trauma), and mitigates the effects of gravity on weaker hip muscle groups (abduction/adduction). Testing in supine position exclusively also allows for testing of one or both hips in multiple anatomic planes without the need to reposition the subject between different strength tests (thus standardizing limb positions for the assessment of agonist:antagonist strength ratios).
To our knowledge, no previous investigations have evaluated the reliability of isometric torque measurements obtained via stabilized dynamometry in a healthy, athletic population using a single testing position that allows for strength assessment in multiple anatomic planes. Consequently, the purpose of this investigation was to design and develop a device that can be used to measure strength about the hip with subjects in a supine position—specifically in active athletes with strong hip musculature—and then evaluate its inter- and intrarater reliability.
Methods
An isometric muscle strength-testing device was developed that could be attached to a standard treatment table (found in most clinical settings) using supplies readily available at hardware and medical supply stores. A custom stabilization cage was fashioned and interfaced with a load sensor (Chatillon SLC-1000) and digital force gauge (Chatillon DFS-R, AMETEK TCI, Largo, Florida) in a manner that enabled the evaluation of hip strength with the subject in a supine position for all hip motions tested (Figures 1 and 2). The device allowed hip abduction/adduction position to be adjusted from 0° to 45°, and hip flexion/extension from 0° to 45° prior to testing. When the desired testing position was achieved, the device was locked in place, holding the limb in a fixed orientation. For the purpose of calculating torque, a standard clinical cloth measuring tape was used to measure the moment arm from the most prominent aspect of the ipsilateral anterior superior iliac spine (ASIS) to the center of the load cell–leg interface. The moment arm was multiplied by the maximal force produced by the subject during each testing repetition yielding the maximal torque generated about the hip joint. Stabilization of the subject’s pelvis was accomplished by firmly securing a wide strap that was centered over the subject’s bilateral ASIS to a stabilization platform secured to the table (Figure 1). The stabilization platform afforded the ability to adjust the proximal and distal position of the platform on the table to accommodate individuals of differing heights. The subject’s arms were crossed over the chest throughout the testing protocol.
Figure 1.
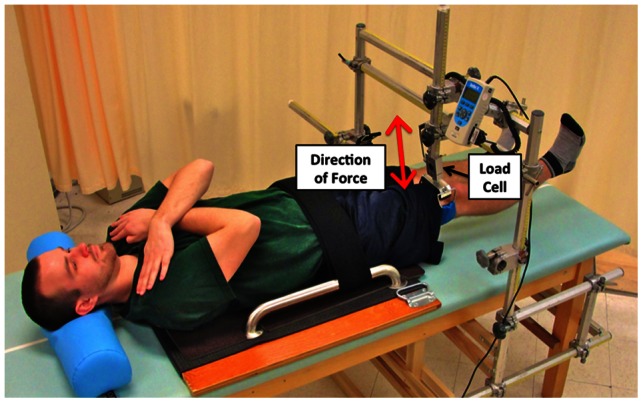
Supine isometric hip flexion/extension test position.
Figure 2.
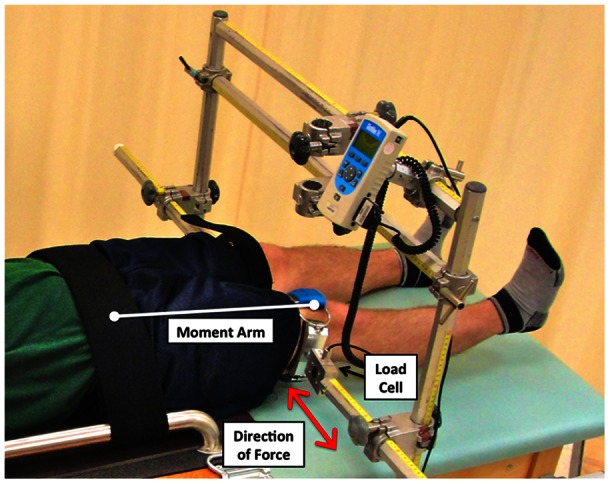
Hip abduction/adduction test position.
A blinded, randomized, repeated-measures study design approved by our institutional review board was employed to evaluate maximal isometric hip flexion, extension, abduction, and adduction torques in 19 athletes (10 men, 9 women) between 19 and 31 years of age. Entry criteria included the following: current participation in NCAA Division I or professional-level ice hockey; no previous lower extremity injury or substantial alteration of training status within 4 months of enrollment; no evidence of delayed-onset muscle soreness–related pain, stiffness, or decreased range of motion of the trunk or lower extremity musculature; and good overall health with no underlying medically diagnosed pathologies or conditions. Healthy, high-level ice hockey athletes were selected to provide a relatively homogeneous study sample group and so allowed for the development of a testing protocol that is robust to large torque production (as may be encountered in athletic injury screenings).
Following enrollment and acquisition of written informed consent to participate in the study, subjects reported to our research laboratory for testing. Positioning of each subject within the testing device was standardized in the following manner: Subjects were placed supine and centered on the testing table. For hip abduction/adduction testing, both hips were positioned in 15° abduction from the centerline of the body through use of a telescoping long arm-goniometer (Lafayette Instrument Company, Lafayette, Indiana) using the subject’s umbilicus as a reference point. For flexion/extension tests, hips were positioned in 10° abduction and 10° flexion. Flexion angle position was established with the use of a digital inclinometer (M-D Building Products, Oklahoma City, Oklahoma). Subjects were instructed to keep their knees fully extended and toes pointed up toward the ceiling to minimize hip rotation during all trials. During abduction/adduction testing, the load sensor interface (utilized on the test limb) and an identical “support” (attached to the contralateral limb) were strapped to the distal aspect of the subject’s thighs approximately 8 cm proximal to the superior pole of the patella and oriented perpendicular to the long axis of the femur. To prevent the potential bias that may have been produced by a leg dominance effect, the limb testing order was determined with a random-number generator and assigned to each subject number prior to enrollment of any participants. All subjects received standardized instructions regarding the execution of each motion tested prior to the onset of testing for that motion. Following appropriate positioning within the device, subjects performed a series of 3 submaximal practice repetitions (at 25%, 50%, and 75% of their perceived maximal effort) with 30 seconds of rest between repetitions. After completion of practice repetitions and a 1-minute rest period, 3 maximal test repetitions were performed with 30 seconds rest between efforts. Each abduction and adduction effort was measured in consecutive order (abduction effort, 30 seconds rest, adduction effort, 30 seconds rest, repeat). Flexion and extension torque were measured in a similar fashion. Each effort was performed for 5 seconds with increasing effort over the first 3 seconds. Subjects were instructed to produce a “ramping up” effort to create maximal force production and prevent impulsive loading (and the potential for artificially inflated measures). The maximal level of effort was provided over the remaining 2 seconds of each effort, and the peak force output was recorded. Additional maximal trials were added if one or more of the repetitions were not performed correctly. Strong verbal encouragement was provided to all subjects during testing bouts using consistent words and phrases. The highest “peak” force value generated during the 3 maximal test repetitions was used for the calculation of torque for each hip motion tested.
Isometric hip strength testing was performed on all subjects at 3 time intervals (baseline, 1 week, and 3 weeks) by 2 trained examiners during each test session interval. The order in which each examiner tested a subject was determined a priori by randomization. All data were collected and maintained by an independent assistant throughout the trial. Examiners were blinded to one another’s results and were not provided access to the data during the 3-week test/retest interval. Reliability was evaluated by concurrently estimating intra- and interexaminer intraclass correlation coefficients (ICC) and 95% confidence intervals, using the method described by Eliasziw et al.9
Results
Descriptive data for male and female subjects are provided in Table 1. Information regarding means ± standard deviations and variability between subjects, examiners, and repeated trials of force (N) and torque (Nm) for each measurement are provided in Table 2. Our analyses revealed that the majority of variability was attributed to “between subject” variability, which ranged from 74% to 91% for all modes of torque measurement. The between-trial variability, however, was 8% to 21%, with very little between-examiner variability, which ranged from 0% to 2%. For most measurements, no variability was attributed to an examiner-by-subject interaction, indicating that differences between examiners were consistent across subjects. However, 1.84% and 1.95% of the variability in hip extension force and torque strength, respectively, were due to examiner-by-subject interaction.
Table 1.
Subjects’ anthropometric information: Mean ± SD.
| Subjects | n | Age, y | Height, cm | Weight, kg | Body Mass Index |
|---|---|---|---|---|---|
| Females | 9 | 20 ± 0.71 | 166.83 ± 5.47 | 65.9 ± 3.62 | 23.72 ± 1.66 |
| Males | 10 | 23.1 ± 3.11 | 178.37 ± 10.08 | 85.53 ± 10.78 | 26.17 ± 1.52 |
Table 2.
Percentage of variability due to different sources.
| Between b | |||||
|---|---|---|---|---|---|
| Motion a | Mean | SD | Subjects | Examiners | Sessions |
| Flexion | |||||
| Force | 462.73 | 150.00 | 87.85 | 1.09 | 11.05 |
| Torque | 174.07 | 66.88 | 91.34 | 0.00 | 8.66 |
| Extension | |||||
| Force | 390.19 | 126.77 | 71.39 | 0.00 | 26.77 |
| Torque | 146.74 | 56.67 | 73.95 | 2.38 | 21.75 |
| Abduction | |||||
| Force | 404.61 | 115.59 | 84.75 | 2.11 | 13.09 |
| Torque | 155.72 | 51.44 | 91.07 | 0.07 | 8.86 |
| Adduction | |||||
| Force | 408.42 | 106.90 | 83.95 | 3.30 | 12.75 |
| Torque | 157.49 | 48.89 | 91.47 | 0.00 | 8.53 |
Force, N; torque, Nm.
In percentages.
Assessment of repeated-measures reliability of inter- and intrarater produced good to excellent results. Inter- and intrarater reliability results for force and torque measurements of each motion tested, as well as 95% confidence intervals, are presented in Table 3. Interrater reliability ICC of torque values for hip flexion and extension strength were 0.91 and 0.74, respectively. Hip abduction and adduction torque strength ICC were 0.91 and 0.92, respectively. The intrarater reliability ICC for hip flexion torque strength was 0.91, and 0.78 for hip extension torque, while abduction and adduction torque strength ICC were 0.91 and 0.92, respectively.
Table 3.
Peak force and torque reliability estimates by examiner. a
| Interexaminer | Intraexaminer | |||
|---|---|---|---|---|
| Motion | ICC | Lower 95% CI | ICC | Lower 95% CI |
| Flexion | ||||
| Force | 0.88 | 0.78 | 0.89 | 0.78 |
| Torque | 0.91 | 0.84 | 0.91 | 0.83 |
| Extension | ||||
| Force | 0.71 | 0.54 | 0.73 | 0.51 |
| Torque | 0.74 | 0.56 | 0.78 | 0.59 |
| Abduction | ||||
| Force | 0.85 | 0.72 | 0.87 | 0.74 |
| Torque | 0.91 | 0.83 | 0.91 | 0.83 |
| Adduction | ||||
| Force | 0.84 | 0.70 | 0.87 | 0.75 |
| Torque | 0.92 | 0.84 | 0.92 | 0.83 |
ICC, intraclass correlation coefficient; CI, confidence interval.
Discussion
We have developed a new device to measure torque generated about the hip during isometric strength testing and have demonstrated that it provides reliable measurements within and between examiners. The low within-subject variability observed relative to the between-subject variability in this relatively homogeneous group indicates the utility of this hip strength protocol as a potential predictive risk factor screening tool for injury in prognostic studies.
Our inter- and intrarater reliability results are comparable with findings from studies that examined hip muscle strength in healthy individuals using stabilized dynamometry.5,11,26,28,32,39 However, to our knowledge, this is the first study to quantify values of hip flexion, extension, abduction, and adduction strength concurrently during the same study using a measurement of torque while the subject was positioned in supine for all measures. Conversely, previous studies measure force of 2 or 3 hip motions in different testing positions for each motion (seated, side lying, supine, and/or prone), with the exception of the study reported by Ford-Smith et al,11 who evaluated the interrater reliability of measuring hip flexion and extension in a seated position in a healthy elderly population. Only one study28 quantified torque (of supine hip extension exclusively) while using a stabilized dynamometer in a subset of healthy subjects.
The interrater reliability of quantifying supine hip extension torque using a stabilized dynamometry system in a subset of healthy adults has been reported by Perry et al.28 The purpose of their investigation was to establish a supine hip extension strength-testing technique that was able to distinguish among at least 4 levels of MMT grades (evaluated by 2 separate examiners), which were performed in the more traditional prone position. Although the authors did not provide specific interrater reliability results (or evaluate intrarater reliability) for their substudy of healthy subjects, they did report significant differences of supine hip torque measured with their chain-stabilized dynamometry system (a tensiometer connected to the ceiling by a chain) and subjects graded as 4 or 5 with MMT techniques (no “healthy” subjects had less than grade 4 MMT). Their results support the clinical utility of their supine hip extension strength assessment performed with a stabilized dynamometer. The reported mean torque values for supine hip extension in their MMT grade 5 group were considerably higher (211.9 Nm) than those reported in the present study (146.7 Nm). Differences between this investigation and ours were numerous. Although not specifically stated, it can be inferred from a figure within the article that moment arm distances were calculated from the greater trochanter to the center of the resistance cuff (fastened to the ankle with knee fully extended). Our moment arm was measured from the ASIS to the center of the resistance cuff, which was placed in a standardized location on the distal aspect of the thigh. Without access to specific force and lever arm length data, it is not possible to compare torque values between healthy subjects in the prior study with those measured in our investigation. Since exact calculation of lever arm length through radiographic measures was beyond the scope of both these studies, a standardized proximal reference point needed to be established a priori. We chose the most prominent aspect of the ASIS, as we feel identification of the greater trochanter can be problematic with an athletic individual lying supine with legs extended due to the increased size of the lateral thigh musculature, as well as with other populations that present with increased adipose in the lateral hip/thigh.
The inter- and intrarater reliability of isometric supine hip abduction strength testing using a stabilization device and 3 commercially available dynamometers has been evaluated by Click Fenter et al.5 Abduction strength was evaluated by 2 testers over the course of 3 days with a different dynamometer being tested on each day. The interrater ICC for each device ranged from 0.899 to 0.948, and intrarater reliability between the 3 devices ranged from 0.888 to 0.958. Limitations of this study include the lack of a torque calculation and absence of stabilization for the nontested limb. Although subjects were strapped to the table to help stabilize the pelvis and were allowed to brace themselves with their upper extremities during maximal efforts, we feel that it is important to also stabilize the contralateral lower extremity during abduction and adduction movements performed supine, as maximal force is generated via action against the opposing limb.
Widler et al39 evaluated the validity and intrarater reliability of stabilized dynamometry for assessment of isometric abduction strength in 3 anatomic positions (standing, side lying, and supine). Tests were performed during 2 sessions, separated by 48 and 72 hours. To assess validity, electromyographic activity of each subject’s bilateral gluteus medius muscles was measured during each unilateral strength test in each of the 3 testing positions. The rationale for assigning the most “valid” testing position, or the one demonstrating the highest construct validity, was based on the assumptions that the most valid position would be the one (1) producing the highest level of ipsilateral gluteus medius activation and lowest contralateral activation and (2) yielding the highest abduction force output. Their results demonstrated good to excellent ICC for intratester reliability for side-lying, supine, and standing testing positions (0.90, 0.83, and 0.88, respectively). Significantly higher strength and ipsilateral gluteus medius electromyographic activity and lower contralateral electromyographic activity were observed in the side-lying position, leading the authors to conclude this is the most “valid” position to use for measurement of hip abduction strength. As with the procedure described and discussed above by Click Fenter and colleagues,5 during the supine hip abduction test, the contralateral limb was not stabilized as in the side-lying and standing tests (ie, the table stabilized the contralateral lower extremity during side-lying, and a wall was used as support during the standing position test). In addition, the dynamometer was aligned perpendicular to the examination table (during side lying), the support wall (during standing), or midline of the body (during supine); however, the hip was tested in 10° of abduction for each motion. Failing to align the measurement axis of the load sensor perpendicular to the long axis of the thigh may result in unaccounted load components, such as shear, and may substantially influence results. In our examination, an offset was built into each thigh support bar, which permitted perpendicular alignment of the dynamometer with the long axis of the thigh. Complete stabilization of the subject during strength testing and proper alignment of the dynamometer with the long axis of the thigh are important considerations associated with strength measurement. These parameters have a direct effect on the force that is measured and torque calculated about the hip and so affect the validity and reliability of the findings described.
Ford-Smith et al11 examined the intrarater reliability of a single evaluator at measuring hip strength using a stabilized dynamometer in community-dwelling healthy older adults. In their investigation, 25 healthy older adults (aged 70-87 years) performed maximal isometric hip flexion and extension efforts on each leg while in the seated position during 2 test sessions separated by 1 week. The intrarater ICCs for right and left hip extension and flexion strength were 0.74 and 0.91, respectively. Using a seated testing position, although practical in the healthy elderly population, was not desirable in our study, as we felt that standardization of body position and firm stabilization of the pelvis and contralateral limb were more easily accomplished with subjects supine. In addition, we desired to test hip strength in positions that more closely resembled the anatomic positions in which subjects typically sustain noncontact lower extremity injuries, such as ACL sprain, which occur in a more extended lower extremity position, not 90° of hip flexion and 90° of knee flexion.13,16,21
The intrarater reliability of stabilized dynamometry for side-lying hip abduction and prone extension strength has been evaluated in healthy adults by Nadler et al.26 The calculated ICCs reported for peak strength measurement intrarater reliability were excellent (0.94 for extension and 0.95 for abduction). Contrasting results were found, however, in a follow-up investigation32 evaluating the inter- and intrarater reliability of side-lying hip abduction, prone hip extension, as well as seated hip extension using the same stabilized dynamometry system. In this study by Scott and colleagues,32 2 examiners compared peak isometric strength obtained with a handheld dynamometer with those obtained using their dynamometer anchoring station at 2 time points separated by 1 week. Interrater ICCs for peak isometric hip extension strength using the stabilized dynamometry system ranged from 0.56 to 0.80, abduction strength ranged from 0.69 to 0.88, and 0.84 to 0.92 for hip flexion strength. Intrarater ICCs ranged from 0.59 to 0.89 and 0.72 to 0.89, respectively, for each examiner across all strength tests when using the stabilized dynamometer. The addition of a second examiner and interrater reliability assessment (as well as a third strength test) in this study compared to the original single-examiner test-retest study performed by Nadler et al26 emphasizes the variability that may be introduced when performing multiple tests in different testing positions, as well as between examiners. The method described in the present study provides efficient evaluation of peak isometric torque generated in 4 of the primary anatomic planes of the hip, and its ease of use and lack of repeated subject repositioning aid in subject comprehension and procedural standardization of all testing bouts. This is beneficial for the subject as well as for examiners. The characteristics of our testing device and procedures are likely reflected in our good to excellent inter- and intrarater reliability measures.
As shown in Table 3, our ability to obtain similar measures across 3 testing sessions over the course of 3 weeks was excellent when evaluating hip flexion, abduction, and adduction (ICC = 0.91, 0.91, and 0.92, respectively, for inter- and intrarater reliability alike). Our assessment of hip extension torque reliability, however, was lower (ICC = 0.74 for interrater and 0.78 for intrarater). The reason that this measurement was more variable than our other assessments is likely multifactorial. Subjects were instructed to maintain an extended knee position during each testing bout. To perform maximal hip extension with the knee also extended requires contraction of the quadriceps (for knee extension) as well as the gluteus maximus and biceps femoris (for hip extension). This may have caused some degree of reciprocal inhibition7,8 between antagonistic muscle groups or at least varying degrees of inhibition between sessions depending on how much effort was utilized to maintain knee extension during each session. Also, stabilization of the distal thigh requires strapping of the load cell interface around substantial soft tissue. When designing our stabilization system, we wanted to apply resistance to all isometric forces above the knee, thus allowing easier use for future case-control studies that evaluate muscle strength after injury to the knee or ankle has occurred, as well as aiding in the clinical utility of the device during orthopaedic assessment or rehabilitation. Depending on how firmly straps are secured around the soft tissues surrounding the distal thigh, more or less hip extension movement will undoubtedly occur. As noted by Waters et al,38 hip extension strength is highly dependent on hip flexion angle and hamstring length, especially as the hip joint is moved into full extension. Although considerable care was taken to standardize all testing procedures and minimize unwanted limb movements during evaluation, it is certainly possible that thigh position may have varied due to soft tissue deformation during hip extension efforts.
Torque measurement reliability ICCs in our examination were better than the values calculated for corresponding force measurement reliability (Table 3). We feel this demonstrates the need to calculate torque values when assessing isometric muscular strength using a stabilized dynamometer. Evaluating torque allows strength values to be more appropriately compared between individuals of different statures and limb lengths, which is important when performing prognostic, diagnostic, and treatment studies. In addition, the evaluation of torque also removes a large amount of variability that may be introduced by dynamometer placement. Very subtle changes in placement of the dynamometer proximally or distally relative to the long axis of the limb segment will produce different force values secondary to the mechanical advantage created by the lever arm. However, accounting for lever arm length allows the dynamometer to be placed on the limb in different locations while yielding similar torque values.
In light of the investigations discussed above, the findings of this study have numerous implications for utilization in research- and clinic-based settings. We found that evaluation of hip flexion/extension and abduction/adduction strength with subjects tested in a supine position with the use of a stabilized dynamometer system provides efficient and reliable measurements (an important concern for prospective study designs that may require the screening of large groups of subjects to determine the risk factors associated with injury to the hip and lower extremity). This measurement system is particularly useful when subjects are unable to be positioned comfortably in side-lying and prone positions following injury to the contralateral limb, as may be required by case-control study designs. In addition, this system may be promising for use in clinical settings when evaluating orthopaedic patients. The measurement of a moment arm to calculate hip internal and external rotation torque was beyond the scope of this project. Recommendations for future research in this area include the incorporation of a torque sensor in the device and a foot plate attachment that can be used to measure supine hip internal and external rotation torque, as well as evaluation in additional study populations and settings.
Footnotes
References
- 1. Baker RL, Souza RB, Fredericson M. Iliotibial band syndrome: soft tissue and biomechanical factors in evaluation and treatment. PM R. 2011;3(6):550-561 [DOI] [PubMed] [Google Scholar]
- 2. Boling MC, Padua DA, Alexander Creighton R. Concentric and eccentric torque of the hip musculature in individuals with and without patellofemoral pain. J Athl Train. 2009;44(1):7-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brinkmann JR. Comparison of a hand-held and fixed dynamometer in measuring strength of patients with neuromuscular disease. J Orthop Sports Phys Ther. 1994;19(2):100-104 [DOI] [PubMed] [Google Scholar]
- 4. Bullock-Saxton JE. Local sensation changes and altered hip muscle function following severe ankle sprain. Phys Ther. 1994;74(1):17-28 [DOI] [PubMed] [Google Scholar]
- 5. Click Fenter P, Bellew JW, Pitts TA, Kay RE. Reliability of stabilised commercial dynamometers for measuring hip abduction strength: a pilot study. Br J Sports Med. 2003;37(4):331-334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dekker J, van Dijk GM, Veenhof C. Risk factors for functional decline in osteoarthritis of the hip or knee. Curr Opin Rheumatol. 2009;21(5):520-524 [DOI] [PubMed] [Google Scholar]
- 7. Eccles JC, Fatt P, Landgren S. Central pathway for direct inhibitory action of impulses in largest afferent nerve fibres to muscle. J Neurophysiol. 1956;19(1):75-98 [DOI] [PubMed] [Google Scholar]
- 8. Eccles RM, Lundberg A. Integrative pattern of Ia synaptic actions on motoneurones of hip and knee muscles. J Physiol. 1958;144(2):271-298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Eliasziw M, Young SL, Woodbury MG, Fryday-Field K. Statistical methodology for the concurrent assessment of interrater and intrarater reliability: using goniometric measurements as an example. Phys Ther. 1994;74(8):777-788 [DOI] [PubMed] [Google Scholar]
- 10. Emery CA, Maitland ME, Meeuwisse WH. Test-retest reliabilty of isokinetic hip adductor and flexor muscle strength. Clin J Sport Med. 1999;9(2):79-85 [DOI] [PubMed] [Google Scholar]
- 11. Ford-Smith CD, Wyman JF, Elswick RK, Fernandez T. Reliability of stationary dynamometer muscle strength testing in community-dwelling older adults. Arch Phys Med Rehabil. 2001;82(8):1128-1132 [DOI] [PubMed] [Google Scholar]
- 12. Frese E, Brown M, Norton BJ. Clinical reliability of manual muscle testing: middle trapezius and gluteus medius muscles. Phys Ther. 1987;67(7):1072-1076 [DOI] [PubMed] [Google Scholar]
- 13. Hashemi J, Breighner R, Chandrashekar N, et al. Hip extension, knee flexion paradox: a new mechanism for non-contact ACL injury. J Biomech. 2011;44(4):577-585 [DOI] [PubMed] [Google Scholar]
- 14. Hayes KW, Falconer J. Reliability of hand-held dynamometry and its relationship with manual muscle testing in patients with osteoarthritis in the knee. J Orthop Sports Phys Ther. 1992;16(3):145-149 [DOI] [PubMed] [Google Scholar]
- 15. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492-501 [DOI] [PubMed] [Google Scholar]
- 16. Homyk A, Orsi A, Wibby S, Yang N, Nayeb-Hashemi H, Canavan PK. Failure locus of the anterior cruciate ligament: 3D finite element analysis. Comput Methods Biomech Biomed Engin. 2012;15(8):865-74 [DOI] [PubMed] [Google Scholar]
- 17. Hrysomallis C. Hip adductors’ strength, flexibility, and injury risk. J Strength Cond Res. 2009;23(5):1514-1517 [DOI] [PubMed] [Google Scholar]
- 18. Kendall FP. Muscles: Testing and Function With Posture and Pain. 5th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2005 [Google Scholar]
- 19. Korpelainen R, Keinanen-Kiukaanniemi S, Nieminen P, Heikkinen J, Vaananen K, Korpelainen J. Long-term outcomes of exercise: follow-up of a randomized trial in older women with osteopenia. Arch Intern Med. 2010;170(17):1548-1556 [DOI] [PubMed] [Google Scholar]
- 20. Krause DA, Schlagel SJ, Stember BM, Zoetewey JE, Hollman JH. Influence of lever arm and stabilization on measures of hip abduction and adduction torque obtained by hand-held dynamometry. Arch Phys Med Rehabil. 2007;88(1):37-42 [DOI] [PubMed] [Google Scholar]
- 21. Krosshaug T, Slauterbeck JR, Engebretsen L, Bahr R. Biomechanical analysis of anterior cruciate ligament injury mechanisms: three-dimensional motion reconstruction from video sequences. Scand J Med Sci Sports. 2007;17(5):508-519 [DOI] [PubMed] [Google Scholar]
- 22. Lawson A, Calderon L. Interexaminer agreement for applied kinesiology manual muscle testing. Percept Mot Skills. 1997;84(2):539-546 [DOI] [PubMed] [Google Scholar]
- 23. Lu TW, Hsu HC, Chang LY, Chen HL. Enhancing the examiner’s resisting force improves the reliability of manual muscle strength measurements: comparison of a new device with hand-held dynamometry. J Rehabil Med. 2007;39(9):679-684 [DOI] [PubMed] [Google Scholar]
- 24. Malliaras P, Hogan A, Nawrocki A, Crossley K, Schache A. Hip flexibility and strength measures: reliability and association with athletic groin pain. Br J Sports Med. 2009;43(10):739-744 [DOI] [PubMed] [Google Scholar]
- 25. Mens JM, Vleeming A, Snijders CJ, Ronchetti I, Stam HJ. Reliability and validity of hip adduction strength to measure disease severity in posterior pelvic pain since pregnancy. Spine (Phila Pa 1976). 2002;27(15):1674-1679 [DOI] [PubMed] [Google Scholar]
- 26. Nadler SF, DePrince ML, Hauesien N, Malanga GA, Stitik TP, Price E. Portable dynamometer anchoring station for measuring strength of the hip extensors and abductors. Arch Phys Med Rehabil. 2000;81(8): 1072-1076 [DOI] [PubMed] [Google Scholar]
- 27. Nadler SF, Malanga GA, Feinberg JH, Prybicien M, Stitik TP, DePrince M. Relationship between hip muscle imbalance and occurrence of low back pain in collegiate athletes: a prospective study. Am J Phys Med Rehabil. 2001;80(8):572-577 [DOI] [PubMed] [Google Scholar]
- 28. Perry J, Weiss WB, Burnfield JM, Gronley JK. The supine hip extensor manual muscle test: a reliability and validity study. Arch Phys Med Rehabil. 2004;85(8):1345-1350 [DOI] [PubMed] [Google Scholar]
- 29. Pizzigalli L, Filippini A, Ahmaidi S, Jullien H, Rainoldi A. Prevention of falling risk in elderly people: the relevance of muscular strength and symmetry of lower limbs in postural stability. J Strength Cond Res. 2011;25(2):567-574 [DOI] [PubMed] [Google Scholar]
- 30. Roy MA, Doherty TJ. Reliability of hand-held dynamometry in assessment of knee extensor strength after hip fracture. Am J Phys Med Rehabil. 2004;83(11):813-818 [DOI] [PubMed] [Google Scholar]
- 31. Schmitt WH, Cuthbert SC. Common errors and clinical guidelines for manual muscle testing: “the arm test” and other inaccurate procedures. Chiropr Osteopat. 2008;16:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Scott DA, Bond EQ, Sisto SA, Nadler SF. The intra- and interrater reliability of hip muscle strength assessments using a handheld versus a portable dynamometer anchoring station. Arch Phys Med Rehabil. 2004;85(4):598-603 [DOI] [PubMed] [Google Scholar]
- 33. Stark T, Walker B, Phillips JK, Fejer R, Beck R. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM R. 2011;3(5):472-479 [DOI] [PubMed] [Google Scholar]
- 34. Stratford PW, Balsor BE. A comparison of make and break tests using a hand-held dynamometer and the Kin-Com. J Orthop Sports Phys Ther. 1994;19(1):28-32 [DOI] [PubMed] [Google Scholar]
- 35. Stuberg WA, Metcalf WK. Reliability of quantitative muscle testing in healthy children and in children with Duchenne muscular dystrophy using a hand-held dynamometer. Phys Ther. 1988;68(6):977-982 [DOI] [PubMed] [Google Scholar]
- 36. Tyler TF, Nicholas SJ, Campbell RJ, McHugh MP. The association of hip strength and flexibility with the incidence of adductor muscle strains in professional ice hockey players. Am J Sports Med. 2001;29(2):124-128 [DOI] [PubMed] [Google Scholar]
- 37. van der Linden ML, Aitchison AM, Hazlewood ME, Hillman SJ, Robb JE. Test-retest repeatability of gluteus maximus strength testing using a fixed digital dynamometer in children with cerebral palsy. Arch Phys Med Rehabil. 2004;85(12):2058-2063 [DOI] [PubMed] [Google Scholar]
- 38. Waters RL, Perry J, McDaniels JM, House K. The relative strength of the hamstrings during hip extension. J Bone Joint Surg Am. 1974;56(8):1592-1597 [PubMed] [Google Scholar]
- 39. Widler KS, Glatthorn JF, Bizzini M, et al. Assessment of hip abductor muscle strength: a validity and reliability study. J Bone Joint Surg Am. 2009;91(11):2666-2672 [DOI] [PubMed] [Google Scholar]
- 40. Wikholm JB, Bohannon RW. Hand-held dynamometer measurements: tester strength makes a difference. J Orthop Sports Phys Ther. 1991;13(4):191-198 [DOI] [PubMed] [Google Scholar]


