Abstract
Context:
Injuries to the tendons of the elbow occur frequently in the overhead athlete, creating a significant loss of function and dilemma to sports medicine professionals. A detailed review of the anatomy, etiology, and pathophysiology of tendon injury coupled with comprehensive evaluation and treatment information is needed for clinicians to optimally design treatment programs for rehabilitation and prevention.
Evidence Acquisitions:
The PubMed database was searched in January 2012 for English-language articles pertaining to elbow tendon injury.
Results:
Detailed information on tendon pathophysiology was found along with incidence of elbow injury in overhead athletes. Several evidence-based reviews were identified, providing a thorough review of the recommended rehabilitation for elbow tendon injury.
Conclusions:
Humeral epicondylitis is an extra-articular tendon injury that is common in athletes subjected to repetitive upper extremity loading. Research is limited on the identification of treatment modalities that can reduce pain and restore function to the elbow. Eccentric exercise has been studied in several investigations and, when coupled with a complete upper extremity strengthening program, can produce positive results in patients with elbow tendon injury. Further research is needed in high-level study to delineate optimal treatment methods.
Keywords: humeral epicondylitis, rehabilitation, elbow tendon injury
Tendon injuries to the human elbow occur frequently, especially in the overhead athlete due to the repetitive loads and forceful muscular activations inherent in throwing, hitting, serving, and spiking.26,63 The most common injuries in the athletic elbow include humeral epicondylitis, valgus extension overload, and ulnar collateral ligament injury.21,52 The initial upper extremity evaluation, including baseline radiographs and clinical testing of the entire upper extremity kinetic chain, forms the critical first step in early recognition and diagnosis of elbow injury and allows for the development of a comprehensive rehabilitation to restore function.
Etiology and Pathophysiology of Tendon Injury
One of the most common tendon injuries of the elbow is humeral epicondylitis,53,55 referred to as “tennis elbow,” “golfer’s elbow,” and “thrower’s elbow” by laypersons and the sports medicine literature. The repetitive overuse is particularly evident in the history of many athletic patients with elbow tendon injury. Classic epidemiological research on adult tennis players shows incidences ranging from 35% to 50%.12,32,35,36,38,59 This incidence is actually far greater than in elite-level junior tennis players (11%-12%).81
As early as 1873, Runge described humeral epicondylitis, or “tennis elbow,” as it is more popularly known.62 Cyriax and Cyriax in 1936, listed 26 causes of tennis elbow,14 while an extensive study by Goldie in 1964 reported hypervascularization of the extensor aponeurosis and increased free nerve endings in the subtendinous space.29 Leadbetter40 later described humeral epicondylitis as a degenerative time-dependent process including vascular, chemical, and cellular events that lead to a failure of the cell matrix healing response in human tendon. This description of tendon injury differs from earlier theories where an inflammatory response was considered a primary factor; hence, the term tendonitis was used, as opposed to the term recommended by Leadbetter40 and Nirschl and Sobel.53
Humeral epicondylitis is an extra-articular tendinous injury characterized by excessive vascular granulation and an impaired healing response in the tendon, “angiofibroblastic hyperplasia.”52,51,55 In a thorough histopathological analysis, specimens of injured tendon from areas of chronic overuse did not contain large numbers of lymphocytes, macrophages, and neutrophils.38 Instead, tendinosis is a degenerative process characterized by large populations of fibroblasts, disorganized collagen, and vascular hyperplasia.38 It is not clear why tendinosis is painful, lacks inflammatory cells, and does not mature. The primary tendon in lateral humeral epicondylitis is the extensor carpi radialis brevis.52-53,55 Approximately one-third of cases involve the tendon of the extensor communis.38 The extensor carpi radialis longus and extensor carpi ulnaris can be involved as well. The primary sites of medial humeral epicondylitis are the flexor carpi radialis, pronator teres, and flexor carpi ulnaris tendons.52-53,55 The incidence of lateral humeral epicondylitis is far greater than that of medial epicondylitis in recreational tennis players and in the leading arm (left arm in a right-handed golfer), while medial humeral epicondylitis is far more common in elite tennis players and throwing athletes due to the powerful loading of the flexor and pronator muscle tendon units during the valgus extension overload inherent in the acceleration phase of those overhead movement patterns.52-53,55 The trailing arm of the golfer (right arm in a right-handed golfer) is more likely to have medial symptoms than lateral.
Mechanical loading of tendon tissue is anabolic by upregulating collagen gene expression and increasing synthesis of collagen proteins peaking 24 hours after exercise and remaining elevated for up to 70 to 80 hours.33,48 However, exercise also degrades collagen proteins. This results in a net loss of collagen 24 to 36 hours after training, followed by a net gain in collagen.44 Thus, a restitution time interval between exercise bouts is critical for the tissue to adapt and avoid a net catabolic situation. The tissue’s adaptive factors are linked to tenocytes, extracellular matrix, and nerve receptors.44
Repetitive strain causes tenocytes to produce inflammatory molecules and engenders microrupture of collagen fibrils.78 Increased inflammatory mediators (eg, prostaglandin E2 [PGE2]) are found in tendons after repetitive mechanical loading.78 Intratendinous injections of PGE2 cause intense degenerative changes, and peritendinous injections of PGE1 result in a histological pattern of tendinopathy.36,70 Today, several studies confirm an inflammatory background in tendinopathy: granulation of capillary vessels and an inflammatory infiltrate of macrophages, mast cells, and B and T lymphocytes.46,66 Inflammatory cells activate a cascade of proinflammatory cytokines (eg, interleukin-18, -15, and -6) found in tendinopathy.47
Tendon cells and fibroblasts, subjected to repetitive mechanical stress in combination with proinflammatory cytokines and transforming growth factor β (TGF-β) stimulation can transform into myofibroblasts.72 Myofibroblasts are important for tendon healing, possibly for tissue adaptation.72 After healing is completed and the mechanical stress is released on the myofibroblasts, these cells undergo programmed cell death (apoptosis).72 If this mechanism fails, the myofibroblasts will propagate a hyperproliferative process: fibrosis—a prominent feature of tendinopathy.72
Another factor that may cause fibroblast hyperproliferation is hypoxia.27 This upregulates matrix metalloproteinases, which alters the material properties of tendon.60 Hypoxia upregulates vascular endothelial growth factor, increasing microvessel ingrowth (angiogenesis), a major finding in tendinopathy.60
Angiogenesis may cause pain since sclerotherapy relieves pain in tendinopathy.54 However, blood vessels per se are not painful, but ingrowth of sensory nerve fibers in tendinopathic patients may be.1,41,66 Healthy nonpainful tendons are almost aneuronal.1,41 Chronic painful tendons show ingrowth of sensory nerves from the paratenon with release of nociceptive substances.1,41,76 Restricting pathological nerve ingrowth by denervation (eg, mini-invasive surgery or release of the paratenon) can relieve pain.76
Sensory nerve ingrowth in the tendon may be a reaction to repetitive loading and a response to injury.45 In normal tendon repair, sensory nerve ingrowth correlates with increased nociception, followed by autonomic nerve ingrowth, coinciding with decreased nociception and subsequent nerve retraction.1,2 In tendinopathy, the ingrown sensory nerves do not retract.41 Neuronal dysregulation, characterized by aberrant sensory nerve sprouting, may reflect a failed healing response, increased pain signaling, and the hyperproliferation of tendinopathy.41
In addition to pain transmission, peripheral nerve fibers react to mechanical stimuli and release several chemical substances in healing and homeostasis. During prolonged release, these cause fibrosis.2 Essential neuromediators are present in tendon.2,67 Tendinopathic tendons exhibit increased sensory neuropeptide substance P (SP), which plays a role in nociception and proinflammatory and trophic actions.2,3,41,66 SP regulates vasodilation, plasma extravasation, and release of cytokines by binding to neurokinin 1 in tendon and is upregulated by loading.2,6,11,34,42,65 SP stimulates proliferation of fibroblasts and endothelial cells and may transform fibroblasts into myofibroblasts by increasing the production of TGF-β in fibroblasts.2,34 Upregulation of SP may contribute to tendinosis—that is, fibrosis (tenocyte transformation, hypercellularity, and hypervascularization).
The neurotransmitter glutamate and its receptor, NMDAR1, are in morphologically transformed tenocytes, endothelial and adventitial layers of neovessel walls, and sprouting nerve fibers.4,49,64
Anatomic Adaptations of the Throwing Athlete’s Elbow with Ramifications for Rehabilitation
Adaptation occurs in the overhead athlete’s elbow in range of motion, laxity, and muscular compensation. Comparison to the contralateral nondominant extremity is often complicated by these asymmetric anatomic developments.
Range of Motion Adaptations
Fifty percent of pitchers have a flexion contracture of the dominant elbow, with 30% demonstrating a cubitus valgus deformity.37 Elbow flexion contractures averaging 5° were common in 40 healthy professional baseball pitchers.22 Directly related to elbow function was wrist flexibility, which was 3° less on the dominant arm for extension and 3° greater on the dominant side for flexion compared with the nondominant extremity.22 In 33 throwing athletes prior to the competitive season, the average loss of elbow extension was 7°, and the average loss of flexion was 5.5°.82
Several studies have shown consistent alterations of shoulder rotation in the overhead athlete, with statistically greater dominant shoulder external rotation and less internal rotation in professional baseball pitchers.24,68,80 Despite these differences in internal and external rotation, the total rotation (internal + external) between extremities remained equal such that any increases in external rotation were matched by decreases in internal rotation in this uninjured population. Elite-level tennis players had significantly less internal rotation and no significant difference in external rotation on the dominant arm, as well as an overall decrease in total rotation range of motion on the dominant arm of approximately 10°.24 Careful monitoring of glenohumeral range of motion is recommended for the athlete with an elbow injury. Decreases in dominant arm internal rotation (glenohumeral internal rotation deficits) often occur in throwing athletes with ulnar collateral ligament injury.16 The comprehensive evaluation of the throwing athlete must include measurement of shoulder internal and external rotation with 90° of abduction, scapular stabilization, and management of internal rotation range of motion loss.24
Ligamentous Laxity
Manual examination of the elbow for medial and lateral laxity can be challenging; humeral rotation and small increases in joint opening are often present with ulnar collateral ligament injury. A critical-level increase of 0.5 mm in medial elbow joint opening in elbows with ulnar collateral ligament injury has been suggested with stress radiography.61 Increases in medial joint laxity can increase stress to the medial muscle tendon units to compensate for medial ligamentous laxity.5
Muscular Adaptations: Wrist and Forearm Strength Profiles in Elite Throwing Athletes
Professional throwing athletes have significantly greater wrist flexion and forearm pronation strength on the dominant arm (15%-35%) compared with the nondominant extremity with no difference in wrist extension or forearm supination strength between extremities.21 In professional baseball pitchers, there is 10% to 20% greater elbow flexion strength on the dominant arm, as well as 5% to 15% greater elbow extension strength.79
Clinical Evaluation of the Athlete’s Elbow
A thorough evaluation of the athlete’s elbow is necessary to rule out other concomitant injured structures and, most important, to identify the underlying cause of the tendon injury. Evaluation of the entire upper extremity kinetic chain with a particular focus on shoulder and scapular strength, motion, and stabilization, coupled with diagnostic imaging and clinical tests for the distal upper extremity, is needed (Figure 1). Overuse injuries in the elbow often occur with shoulder or scapular dysfunction.18,21,43,50,52,55
Figure 1.

Example of scapular pathology seen in an elite junior tennis player with medial elbow pain on clinical examination.
Nonoperative Treatment Concepts
Based on the healing response of the human tendon, several specific phases can be followed during nonoperative treatment of elbow tendinosis: protected function, total arm strength, and return to activity. Each plays a critical part in the comprehensive treatment of elbow tendinosis.
Protected Function
During this first phase, care is taken to protect the injured muscle tendon unit from stress but not from function. Often, all sport activity must cease temporarily to allow the muscle tendon unit time to heal and to allow formal rehabilitation to progress. Immobilization can atrophy the musculature and negatively affect the upper extremity kinetic chain.51,55 Cessation of throwing and serving for medial-based humeral symptoms is indicated. Allowing batting and fielding activities in baseball or hitting double-handed backhands in tennis continues activity while minimizing stress to the injured area. Continued work or sports may slow the progression of resistive exercise and physical therapy.
Modalities are very helpful during this period; however, agreement on a superior modality does not exist.10,39,74 A meta-analysis of 185 studies on treatment of humeral epicondylitis showed glaring deficits in the scientific quality of the investigations, with no superior treatment approach.39 In a comprehensive review of the treatment for humeral epicondylitis, no significant difference was found with low-energy lasers, acupuncture, extracorporeal shockwave therapy, or steroid injection.10
Cortisone injection has been used during the pain-reduction phase of recalcitrant conditions. Traditional physical therapy and cortisone injection were compared in 70 patients with humeral epicondylitis.15 The cortisone injection produced initial relief in 91% of patients compared to 47% undergoing physical therapy. After 3 months, 51% of the cortisone injection group and only 5% in the physical therapy group had a return of primary symptoms. Similar findings were reported with Mills manipulation and cross-friction massage and corticosteroid injection in a prospective randomized controlled clinical trial in 106 patients with humeral epicondylitis.77 At 1 year, there were no differences between treatment groups.
In a double-blind randomized controlled trial of autologous platelet-rich plasma in patients with humeral epicondylitis, 49% had a successful response (25% reduction in visual analog score and Disabilities of the Arm, Shoulder and Hand score) in the cortisone group compared with 73% in the platelet-rich plasma group.56
In 199 patients with humeral epicondylitis treated with iontophoresis with dexamethasone, 52% improved, with only 33% of the placebo group reporting improvement after 2 days.52 There was no statistical difference in the overall improvement 1 month following treatment. Greater pain relief was seen with 6 treatments in a 10-day period.
In a multicenter prospective randomized control study, extracorporeal shockwave therapy was ineffective in 272 patients with humeral epicondylitis.31 Similarly, low-intensity Nd:YAG laser irradiation at 7 points along the forearm, 3 times a week for 4 weeks, was ineffective.8
A standardized modality or modality sequence has not been identified that is statistically more effective. Cryotherapy following increases in daily activity is recommended.51,55 Therapeutic modalities and cortisone injection can only be one part of the treatment sequence; increasing evidence favors progressive resistive exercise.13,28,57,71,75
Thirty-eight patients with lateral humeral epicondylitis were randomly assigned to a contract-relax stretching or eccentric exercise treatment group.71 Seventy-one percent reported full recovery in the eccentric exercise group, with 39% in the contract-relax stretching group. Eccentric exercise produced a significant reduction in pain and eliminated strength deficits in the wrist extensors and forearm supinators.13
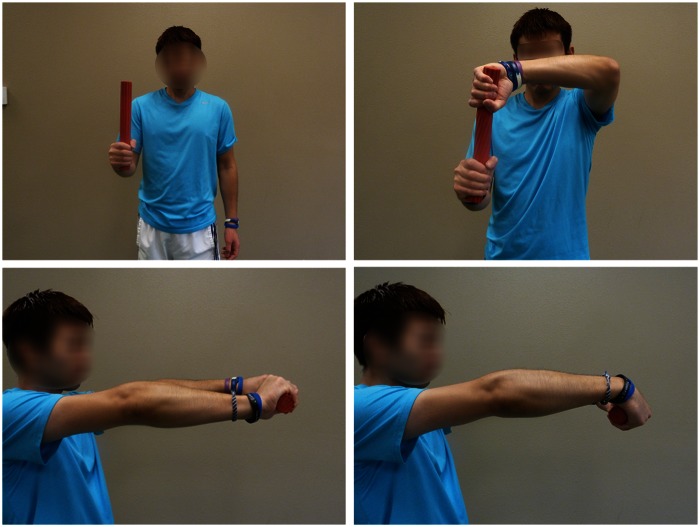
Elastic flexible bar (Thera-Band FlexBar, Hygenic Corp, Akron, Ohio) produces an eccentric overload to wrist and forearm musculature in patients with lateral humeral epicondylitis. A twisting exercise to eccentrically load the elbow extensor musculature showed superior results to traditional rehabilitation (Figure 2).75 Adaptation to medial humeral epicondylitis is also possible (Figure 3). The FlexBar preloads the wrist and finger musculature, followed by a slow eccentric contraction. Multiple sets of 15 repetitions are recommended75 with discomfort (visual analog scale levels 3-4).71
Figure 2.
Tyler twist for lateral humeral epicondylitis includes eccentric loading of the wrist extensors moving from a position of wrist extension to wrist flexion.
Figure 3.
Tyler twist for medial humeral epicondylitis includes eccentric loading of the wrist flexors moving from a position of wrist flexion to wrist extension.
Eighty-one patients with a 3-month history or greater (mean duration, 107 weeks) of chronic lateral elbow pain were randomly allocated to a concentric and eccentric exercise or control group for a 3-month period.58 Starting with a water container (1 kg for women; 2 kg for men), wrist flexion and extension were increased by one-tenth when subjects performed 45 repetitions (3 sets of 15 repetitions). After 3 months of training, 72% of the exercise group had a 30% reduction of pain with the maximal voluntary muscle provocation test, as compared with 44% in the control group.
Specific Applications of Exercise for Elbow Tendon Rehabilitation: Total Arm Strength Rehabilitation Approach
Resistive exercise for humeral epicondylitis focuses on the principle that “proximal stability is needed to promote distal mobility.”69 Initially, focus is on the rotator cuff and scapular musculature (Table 1).7,9,17-19,23,73 A low-resistance, high-repetition exercise format (ie, 3 sets of 15-20 repetitions) is followed to improve strength and local muscular endurance.25 Cuff weights allow rotator cuff and scapular exercises to be performed with the weight proximal to the elbow to minimize overload at the elbow and forearm.
Table 1.
Proximal exercises used in rehabilitation of elbow tendon injury.
| Side-lying external rotation |
| Prone extension with external humeral rotation (thumb-out position) |
| Prone horizontal abduction with external humeral rotation (thumb-out position) |
| Prone external rotation with scapular retraction |
| Scaption (scapular plane elevation with thumb-up position) |
| External rotation with scapular retraction (standing with elastic resistance) |
| Supine serratus punch |
Distal Upper Extremity Exercise
Initially (for lateral elbow tendon injury) exercise of the distal extremity stresses the injured muscle-tendon unit last: wrist flexion and forearm pronation. Gradual addition of wrist extension and forearm supination, as well as radial and ulnar deviation exercises, are added as signs and symptoms allow. Initially, most patients tolerate the exercises better in slight elbow flexion with light weights. Eccentric exercise may have a greater benefit than the concentric portion.13,71 Multiple sets of 15 to 20 repetitions are recommended to promote muscular endurance.
Once the patient tolerates the most basic series of distal exercises, simultaneous contraction of the wrist and forearm musculature is added during elbow flexion/extension (ball dribbling [Bodyblade, Hymanson, Texas]; FlexBar oscillation [Thera-Band]; seated rowing). Additionally, closed kinetic chain exercises (quadruped rhythmic stabilization) are added to promote cocontraction and mimic functional positions with joint approximation.20 Gentle passive stretching and supine combined stretches are indicated to optimize the muscle tendon unit length to elongate the biarticular muscle tendon units of the elbow, forearm, and wrist using a combination of shoulder, elbow, wrist, and forearm positions.21
When the patient tolerates the distal isotonic exercise progression pain-free (3-5 lb or medium elastic tubing or bands) and oscillatory-type exercises, he or she progresses to isokinetic and plyometric exercise (Figure 4). Contractile velocities ranging between 180° and 300° per second with 5 or 6 sets of 15 to 20 repetitions are used to foster local muscular endurance25 in athletic patients with slower contractile velocities (120° to 210° per second). Plyometric wrist snaps (Figure 5) and wrist flips (Figure 6) train the active elbow for functional and sport-specific demands.79
Figure 4.

Isokinetic wrist extension/flexion exercise setup used during rehabilitation of humeral epicondylitis.
Figure 5.

Wrist snaps using a plyo ball to improve wrist and forearm strength.
Figure 6.

Wrist flips using a plyo ball to improve wrist and forearm strength.
Return to Activity
The return-to-activity phase is frequently ignored or cut short, resulting in serious consequences or reinjury (Table 2). Objective criteria for this stage are strength equal to the contralateral extremity and a pain-free range of motion.
Table 2.
Nirschl tendonosis pain phases.
| Phase 1: Mild pain after exercise activity, resolves within 24 hours |
| Phase 2: Pain after exercise activity, exceeds 48 hours, resolves with warm-up |
| Phase 3: Pain with exercise activity that does not alter activity |
| Phase 4: Pain with exercise activity that alters activity |
| Phase 5: Pain caused by heavy activities of daily living |
| Phase 6: Intermittent pain at rest that does not disturb sleep, pain caused by light activities of daily living |
| Phase 7: Constant rest pain (dull aching) and pain that disturbs sleep |
Interval sport return programs utilize alternate days, gradual progressions of intensity, and repetitions of sport activities. For the interval tennis program, low-compression tennis balls decrease impact stress and increase the tolerance of activity (Figure 7). Supervision of the interval program allows for biomechanical evaluation and guards against overzealous intensity levels, a common mistake in well-intentioned, motivated patients. The alternate-day return program, with rest between sessions, enhances recovery and decreases reinjury.21,23,79
Figure 7.

Examples of low-compression tennis balls that can be used to decrease impact shock during the interval tennis program. These balls are available commercially.
Inspection and modification of the patient’s tennis racquet or golf clubs is important. Lowering the string tension and a softer string (coreless multifilament synthetic string or gut) are widely recommended for patients with upper extremity injuries.18,51,53,55 Grip size is also very important, as muscular activity changes can alter handle or grip size.3 Proper grip size should correspond to the distance measured with a tape from the distal tip of the ring finger, along the radial border of the finger, to the proximal palmar crease or allow for the width of the contralateral fifth finger to be placed between the thenar eminence and the longest finger while gripping the racquet21,51,53,55 (Figure 8). A counterforce brace can decrease stress on the insertion of the flexor and extensor tendons during work or sport activity.30
Figure 8.

Use of the contralateral fifth digit to gauge proper grip size. The width of the fifth digit should fit between the longest finger and the thenar eminence in an optimally sized tennis racquet grip.
The biological goals of nonoperative physiotherapy are neovascular enhancement and mature collagen production with associated improvement in muscular strength, endurance, and flexibility. Failure of a quality program may warrant surgical intervention. Most patients with elbow tendinosis respond to the nonoperative program.
Surgical Concepts
The principles of surgical intervention are total excision of the unhealthy pain producing angiofibroblastic tendinosis tissue, enhancement of vascular access to the surgical site, and preservation of normal tissue.51 Techniques that fail to identify and excise tendinosis tissue and release normal tendons are not recommended. Failed surgery is almost always related to inadequate excision of tendinosis tissue with or without excessive release of normal tissue (eg, lateral epicondyle, extensor digitorum communis, and lateral ligaments).51,54 The mini-open techniques have reported success rates of 95% and 97% for medial and lateral tissue, respectively.55 The key pathological tissues are in the extensor carpi radialis brevis and extensor digitorum communis lateral, pronator teres and flexor carpi radialis medial, triceps posterior, and distal biceps anterior.51,55
Ulnar nerve neurapraxia is often associated (50%) with medial elbow tendinosis and may require decompression of the cubital tunnel.51,55
Summary
Identifying the specific tendon pathology and understanding the healing mechanism will help clinicians guide patients through the rehabilitation process.
Footnotes
The following authors declared potential conflicts of interest: Todd S. Ellenbecker, DPT, MS, SCS, OCS, CSCS, is a consultant for the Theraband Research Advisory Committee and is an employee of the Physiotherapy Associates Scottsdale Sports Clinic and the ATP World Tour; Robert Nirschl, MD, is a corporate officer at Medical Sports Inc., a stock holder at Tenex Corp., and received grants from Smith & Nephew; Per Renstrom, MD, PhD, received payments and royalties for published work and university lectures.
References
- 1. Ackermann PW, Li J, Lundeberg T, Kreicbergs A. Neuronal plasticity in relation to nociception and healing of rat achilles tendon. J Orthop Res. 2003;21(3):432-441 [DOI] [PubMed] [Google Scholar]
- 2. Ackermann PW, Salo PT, Hart DA. Neuronal pathways in tendon healing. Front Biosci. 2009;14:5165-5187 [DOI] [PubMed] [Google Scholar]
- 3. Adelsberg S. An EMG analysis of selected muscles with rackets of increasing grip size. Am J Sports Med. 1986;14:139-142 [DOI] [PubMed] [Google Scholar]
- 4. Alfredson H, Forsgren S, Thorsen K, Fahlstrom M, Johansson H, Lorentzon R. Glutamate NMDAR1 receptors localised to nerves in human Achilles tendons: implications for treatment? Knee Surg Sports Traumatol Arthrosc. 2001;9(2):123-126 [DOI] [PubMed] [Google Scholar]
- 5. An KN, Hui FC, Morrey BF, Linscheid RL, Chao EY. Muscles across the elbow joint: a biomechanical analysis. J Biomech. 1981;14:659-669 [DOI] [PubMed] [Google Scholar]
- 6. Andersson G, Danielson P, Alfredson H, Forsgren S. Presence of substance P and the neurokinin-1 receptor in tenocytes of the human Achilles tendon. Regul Pept. 2008;150(1-3):81-87 [DOI] [PubMed] [Google Scholar]
- 7. Ballentyne BT, O’Hare SJ, Paschall JL, et al. Electromyographic activity of selected shoulder muscles in commonly used therapeutic exercises. Phys Ther. 1993;73:668-682 [DOI] [PubMed] [Google Scholar]
- 8. Basford JR, Sheffield CG, Cieslak KR. Laser therapy: a randomized, controlled trial of the effects of low intensity Nd:YAG laser irradiation on lateral epicondylitis. Arch Phys Med Rehabil. 2000;81:1504-1510 [DOI] [PubMed] [Google Scholar]
- 9. Blackburn TA, McLeod WD, White B, et al. EMG analysis of posterior rotator cuff exercises. J Athl Train. 1990;25:40-45 [Google Scholar]
- 10. Boyer MI, Hastings H. Lateral tennis elbow: is there any science out there? J Shoulder Elbow Surg. 1999;8:481-491 [DOI] [PubMed] [Google Scholar]
- 11. Bring DKI, Reno C, Renstrom P, Salo P, Hart DA, Ackermann PW. Joint immobilization reduces the expression of sensory neuropeptide receptors and impairs healing after tendon rupture in a rat model. J Orthop Res. 2009;27(2):274-280 [DOI] [PubMed] [Google Scholar]
- 12. Carroll R. Tennis elbow: incidence in local league players. Br J Sports Med. 1981;15:250-255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Croisier JL, Foidart-Dessalle M, Tinant F, et al. An isokinetic eccentric programme for the management of chronic lateral epicondylar tendinopathy. Br J Sports Med. 2007;41:269-275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cyriax JH, Cyriax PJ. Illustrated Manual of Orthopaedic Medicine. London, UK: Butterworth; 1983 [Google Scholar]
- 15. Dijs H, Mortier G, Driessens M, DeRidder A, Willems J, Devroey T. A retrospective study of the conservative treatment of tennis elbow. Medica Physica. 1990;13:73-77 [PubMed] [Google Scholar]
- 16. Dines JS, Frank JB, Akerman M, et al. Glenohumeral internal rotation deficits in baseball players with ulnar collateral ligament deficiency. Am J Sports Med. 2009;37(3):566-570 [DOI] [PubMed] [Google Scholar]
- 17. Ekstrom RA, Donatelli RA, Soderberg GL. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J Orthop Sports Phys Ther. 2003;33(5):247-258 [DOI] [PubMed] [Google Scholar]
- 18. Ellenbecker TS. Rehabilitation of shoulder and elbow injuries in tennis players. Clin Sports Med. 1995;14:87. [PubMed] [Google Scholar]
- 19. Ellenbecker TS, Cools A. Rehabilitation of shoulder impingement syndrome and rotator cuff injuries: an evidence based review. Br J Sports Med. 2010;44:319-327 [DOI] [PubMed] [Google Scholar]
- 20. Ellenbecker TS, Davies GJ. Closed Kinetic Chain Exercise: A Comprehensive Guide to Multiple Joint Exercises. Champaign, IL: Human Kinetics; 2001 [Google Scholar]
- 21. Ellenbecker TS, Mattalino AJ. The Elbow in Sport. Champaign, IL: Human Kinetics; 1997 [Google Scholar]
- 22. Ellenbecker TS, Mattalino AJ, Elam EA, et al. Medial elbow laxity in professional baseball pitchers: a bilateral comparison using stress radiography. Am J Sports Med. 1998;26(3):420-424 [DOI] [PubMed] [Google Scholar]
- 23. Ellenbecker TS, Reinold MM, Nelson CO. Clinical concepts for treatment of the elbow in the adolescent overhead athlete. Clin Sports Med. 2010;29(4):705-724 [DOI] [PubMed] [Google Scholar]
- 24. Ellenbecker TS, Roetert EP, Bailie DS, Davies GJ, Brown SW. Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Med Sci Sports Exerc. 2002;34(12):2052-2056 [DOI] [PubMed] [Google Scholar]
- 25. Fleck S, Kraemer W. Designing Resistance Training Programs. Champaign, IL: Human Kinetics; 2004 [Google Scholar]
- 26. Fleisig GS, Andrews JR, Dillman CJ, et al. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233. [DOI] [PubMed] [Google Scholar]
- 27. Freeman TA, Parvizi J, Dela Valle CJ, Steinbeck MJ. Mast cells and hypoxia drive tissue metaplasia and heterotopic ossification in idiopathic arthrofibrosis after total knee arthroplasty. Fibrogenesis Tissue Repair. 2010;3:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gam AN, Warming S, Larsen LH, et al. Treatment of myofascial trigger points with ultrasound combined with massage and exercise: a randomized controlled trial. Pain. 1998;77(1):73-79 [DOI] [PubMed] [Google Scholar]
- 29. Goldie I. Epicondylitis lateralis humeri. Acta Chir Scand Suppl. 1964;339:1. [PubMed] [Google Scholar]
- 30. Groppel JL, Nirschl RP. A biomechanical and electromyographical analysis of the effects of counter force braces on the tennis player. Am J Sports Med. 1986;14:195-200 [DOI] [PubMed] [Google Scholar]
- 31. Haake M, Konig IR, Decker T, et al. Extracorporeal shock wave therapy in the treatment of lateral epicondylitis: a randomized multi-center study. J Bone Joint Surgery Am. 2002;84:1982-1991 [DOI] [PubMed] [Google Scholar]
- 32. Hang YS, Peng SM. An epidemiological study of upper extremity injury in tennis players with particular reference to tennis elbow. J Formos Med Assoc. 1984;83:307-316 [PubMed] [Google Scholar]
- 33. Heinemeier KM, Olesen JL, Haddad F, et al. Expression of collagen and related growth factors in rat tendon and skeletal muscle in response to specific contraction types. J Physiol. 2007;582(pt 3):1303-1316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hoffmann P, Hoeck K, Deters S, Werner-Martini I, Schmidt WE. Substance P and calcitonin gene related peptide induce TGF-alpha expression in epithelial cells via mast cells and fibroblasts. Regul Pept. 2010;161(1-3):33-37 [DOI] [PubMed] [Google Scholar]
- 35. Kamien M. A rational management of tennis elbow. Sports Med. 1990;9:173-191 [DOI] [PubMed] [Google Scholar]
- 36. Khan MH, Li Z, Wang JH. Repeated exposure of tendon to prostaglandin-E2 leads to localized tendon degeneration. Clin J Sport Med. 2005;15(1):27-33 [DOI] [PubMed] [Google Scholar]
- 37. King JW, Brelsford HJ, Tullos HS. Analysis of the pitching arm of the professional baseball pitcher. Clin Orthop Relat Res. 1969;67:116-123 [PubMed] [Google Scholar]
- 38. Kraushaar BS, Nirschl RP. Tendinosis of the elbow (tennis elbow). Clinical features and findings of histopathological, immunohistochemical and electron microscopy studies. J Bone Joint Surg Am. 1999;81:259-278 [PubMed] [Google Scholar]
- 39. Labelle H, Guibert R, Joncas J, Newman N, Fallaha M, Rivard CH. Lack of scientific evidence for the treatment of lateral epicondylitis of the elbow. J Bone Joint Surg Br. 1992;74:646-651 [DOI] [PubMed] [Google Scholar]
- 40. Leadbetter WB. Cell matrix response in tendon injury. Clin Sports Med. 1992;11:533-579 [PubMed] [Google Scholar]
- 41. Lian O, Dahl J, Ackermann PW, Frihagen F, Engebretsen L, Bahr R. Pronociceptive and antinociceptive neuromediators in patellar tendinopathy. Am J Sports Med. 2006;34(11):1801-1808 [DOI] [PubMed] [Google Scholar]
- 42. Ljung BO, Alfredson H, Forsgren S. Neurokinin 1-receptors and sensory neuropeptides in tendon insertions at the medial and lateral epicondyles of the humerus: studies on tennis elbow and medial epicondylalgia. J Orthop Res. 2004;22(2):321-327 [DOI] [PubMed] [Google Scholar]
- 43. Magee DJ. Orthopedic Physical Assessment. 3rd ed. Philadelphia, PA: Saunders; 1997 [Google Scholar]
- 44. Magnusson SP, Langberg H, Kjaer M. The pathogenesis of tendinopathy: balancing the response to loading. Nat Rev Rheumatol. 2010;6(5):262-268 [DOI] [PubMed] [Google Scholar]
- 45. Messner K, Wei Y, Andersson B, Gillquist J, Rasanen T. Rat model of Achilles tendon disorder: a pilot study. Cells Tissues Organs. 1999;165(1):30-39 [DOI] [PubMed] [Google Scholar]
- 46. Millar NL, Hueber AJ, Reilly JH, et al. Inflammation is present in early human tendinopathy. Am J Sports Med. 2010;38(10):2085-2091 [DOI] [PubMed] [Google Scholar]
- 47. Millar NL, Wei AQ, Molloy TJ, Bonar F, Murrell GA. Cytokines and apoptosis in supraspinatus tendinopathy. J Bone Joint Surg Br. 2009;91(3):417-424 [DOI] [PubMed] [Google Scholar]
- 48. Miller BF, Olesen JL, Hansen M, et al. Coordinated collagen and muscle protein synthesis in human patella tendon and quadriceps muscle after exercise. J Physiol. 2005;567(pt 3):1021-1033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Molloy TJ, Kemp MW, Wang Y, Murrell GA. Microarray analysis of the tendinopathic rat supraspinatus tendon: glutamate signaling and its potential role in tendon degeneration. J Appl Physiol. 2006;101(6):1702-1709 [DOI] [PubMed] [Google Scholar]
- 50. Morrey BF. The Elbow and Its Disorders. 2nd ed. Philadelphia, PA: Saunders; 1993 [Google Scholar]
- 51. Nirschl RP, Ashman ES. Tennis elbow tendinosis (epicondylitis). Instr Course Lect. 2004;53:587-598 [PubMed] [Google Scholar]
- 52. Nirschl RP, Rodin DM, Ochiai DH, et al. Iontophoretic administration of dexamethasone sodium phosphate for acute epicondylitis: a randomized, double blind, placebo controlled study. Am J Sports Med. 2003;31(2):189-195 [DOI] [PubMed] [Google Scholar]
- 53. Nirschl R, Sobel J. Conservative treatment of tennis elbow. Phys Sportsmed. 1981;9:43-54 [DOI] [PubMed] [Google Scholar]
- 54. Ohberg L, Alfredson H. Ultrasound guided sclerosis of neovessels in painful chronic Achilles tendinosis: pilot study of a new treatment. Br J Sports Med. 2002;36(3):173-175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ollivierre CO, Nirschl RP. Tennis elbow: current concepts of treatment and rehabilitation. Sports Med. 1996;22(2):133-139 [DOI] [PubMed] [Google Scholar]
- 56. Peerbooms JC, Sluimer J, Bruijn DJ, Gosens T. Positive effect of an autologous platelet concentrate in lateral epicondylitis in a double blind randomized controlled trial. Am J Sports Med. 2010;38(2):255-262 [DOI] [PubMed] [Google Scholar]
- 57. Penimaki T, Karinen P, Kemila T, Koivukangas P, Vanharanta H. Long term follow-up of conservatively treated chronic tennis elbow patients: a prospective and retrospective analysis. Scan J Rehabil Med. 1998;30(3):159-166 [DOI] [PubMed] [Google Scholar]
- 58. Peterson M, Butler S, Eriksson M, Svardsudd K. A randomized controlled trial of exercise versus wait-list in chronic tennis elbow (lateral epicondylosis). Ups J Med Sci. 2011;116(4):269-279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Priest JD, Jones HH, Tichenor CJC, et al. Arm and elbow changes in expert tennis players. Minn Med. 1977;60:399-404 [PubMed] [Google Scholar]
- 60. Pufe T, Petersen WJ, Mentlein R, Tillmann BN. The role of vasculature and angiogenesis for the pathogenesis of degenerative tendons disease. Scand J Med Sci Sports. 2005;15(4):211-222 [DOI] [PubMed] [Google Scholar]
- 61. Rijke AM, Goitz HT, McCue FC. Stress radiography of the medial elbow ligaments. Radiology 1994;191:213-216 [DOI] [PubMed] [Google Scholar]
- 62. Runge F. Zur genese unt behand lung bes schreibekramp fes. Berl Klin Woschenschr. 1873;10:245 [Google Scholar]
- 63. Ryu KN, McCormick J, Jobe FW, et al. An electromyographic analysis of shoulder function in tennis players. Am J Sports Med. 1988;16:481-485 [DOI] [PubMed] [Google Scholar]
- 64. Schizas L, Frihagen E, Bahr A. Coexistence of up-regulated NMDA receptor 1 and glutamate on nerves, vessels and transformed tenocytes in tendinopathy. Scand J Med Sci Sports. 2010;20(2):208-215 [DOI] [PubMed] [Google Scholar]
- 65. Schizas N, Andersson T, Fahlgren A, Aspenberg P, Ahmed M, Ackermann P. Compression therapy promotes proliferative repair during rat Achilles tendon immobilization. J Orthop Res. 2010;28(7):852-858 [DOI] [PubMed] [Google Scholar]
- 66. Schubert TE, Weidler C, Lerch K, Hofstadter F, Straub RH. Achilles tendinosis is associated with sprouting of substance P positive nerve fibres. Ann Rheum Dis. 2005;64(7):1083-1086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Scott A, Bahr R. Neuropeptides in tendinopathy. Front Biosci. 2009;14:2203-2211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Shanley E, Rauh MJ, Michener LA, Ellenbecker TS, Garrison JC, Thigpen CA. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. Am J Sports Med. 2011;39:1997-2006 [DOI] [PubMed] [Google Scholar]
- 69. Sullivan PE, Markos PD, Minor MD. An Integrated Approach to Therapeutic Exercise: Theory and Clinical Application. Reston, VA: Reston Publishing Co; 1982 [Google Scholar]
- 70. Sullo A, Maffulli N, Capasso G, Testa V. The effects of prolonged peritendinous administration of PGE1 to the rat Achilles tendon: a possible animal model of chronic Achilles tendinopathy. J Orthop Sci. 2001;6(4):349-357 [DOI] [PubMed] [Google Scholar]
- 71. Svernl AB, Adolfsson L. Non-operative treatment regime including eccentric training for lateral humeral epicondylalgia. Scand J Med Sci Sports. 2001;11(6):328-334 [DOI] [PubMed] [Google Scholar]
- 72. Tomasek JJ, Gabbiani G, Hinz B, Chaponnier C, Brown RA. Myofibroblasts and mechano-regulation of connective tissue remodelling. Nat Rev Mol Cell Biol. 2002;3(5):349-363 [DOI] [PubMed] [Google Scholar]
- 73. Townsend H, Jobe FW, Pink M, et al. Electromyographic analysis of the glenohumeral muscles during a baseball rehabilitation program. Am J Sports Med. 1992;19:264-272 [DOI] [PubMed] [Google Scholar]
- 74. Trudel D, Duley J, Zastrow I, Kerr EW, Davidson R, MacDermid JC. Rehabilitation for patients with lateral epicondylitis: a systematic review. J Hand Ther. 2004;17(2):243-266 [DOI] [PubMed] [Google Scholar]
- 75. Tyler TF, Thomas GC, Nicholas SJ, McHugh MP. Addition of isolated wrist extensor eccentric exercise to standard treatment for chronic lateral epicondylosis: a prospective randomized trial. J Shoulder Elbow Surg. 2010;19(6):917-922 [DOI] [PubMed] [Google Scholar]
- 76. van Sterkenburg MN, van Dijk CN. Mid-portion Achilles tendinopathy: why painful? An evidence-based philosophy. Knee Surg Sports Traumatol Arthrosc. 2011;19(8):1367-1375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Verhaar JAN, Walenkamp GHIM, Kester ADM, Linden AJVD. Local corticosteroid injection versus Cyriax-type physiotherapy for tennis elbow. J Bone Joint Surgery Br. 1995;77:128-132 [PubMed] [Google Scholar]
- 78. Wang JH, Jia F, Yang G, et al. Cyclic mechanical stretching of human tendon fibroblasts increases the production of prostaglandin E2 and levels of cyclooxygenase expression: a novel in vitro model study. Connect Tissue Res. 2003;44(3-4):128-133 [DOI] [PubMed] [Google Scholar]
- 79. Wilk KE, Arrigo CA, Andrews JR. Rehabilitation of the elbow in the throwing athlete. J Orthop Sports Phys Ther. 1993;17:305-317 [DOI] [PubMed] [Google Scholar]
- 80. Wilk KE, Macrina LC, Fleisig GS, et al. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am J Sports Med. 2011;39:329-335 [DOI] [PubMed] [Google Scholar]
- 81. Winge S, Jorgensen U, Nielsen AL. Epidemiology of injuries in Danish championship tennis. Int J Sports Med. 1989;10:368-371 [DOI] [PubMed] [Google Scholar]
- 82. Wright RW, Steeger May K, Wasserlauf BI, et al. Elbow range of motion in professional baseball pitchers. Am J Sports Med. 2006;34(2):190-193 [DOI] [PubMed] [Google Scholar]