Abstract
Context:
Intra-articular injections into the glenohumeral joint are commonly performed by musculoskeletal providers, including orthopaedic surgeons, family medicine physicians, rheumatologists, and physician assistants. Despite their frequent use, there is little guidance for injectable treatments to the glenohumeral joint for conditions such as osteoarthritis, adhesive capsulitis, and rheumatoid arthritis.
Evidence Acquisition:
We performed a comprehensive review of the available literature on glenohumeral injections to help clarify the current evidence-based practice and identify deficits in our understanding. We searched MEDLINE (1948 to December 2011 [week 1]) and EMBASE (1980 to 2011 [week 49]) using various permutations of intra-articular injections AND (corticosteroid OR hyaluronic acid) and (adhesive capsulitis OR arthritis).
Results:
We identified 1 and 7 studies that investigated intra-articular corticosteroid injections for the treatment of osteoarthritis and adhesive capsulitis, respectively. Two and 3 studies investigated the use of hyaluronic acid in osteoarthritis and adhesive capsulitis, respectively. One study compared corticosteroids and hyaluronic acid injections in the treatment of osteoarthritis, and another discussed adhesive capsulitis.
Conclusion:
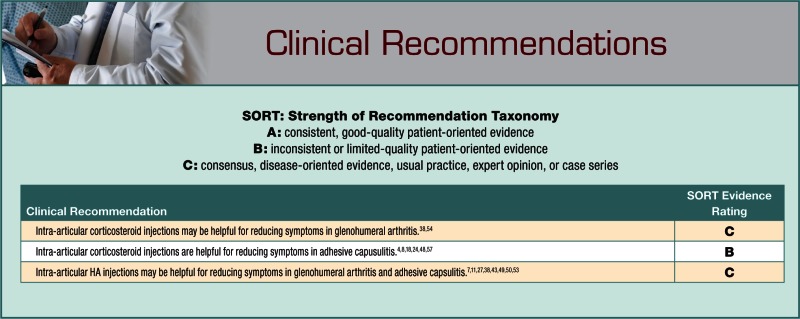
Based on existing studies and their level of evidence, there is only expert opinion to guide corticosteroid injection for osteoarthritis as well as hyaluronic acid injection for osteoarthritis and adhesive capsulitis.
Keywords: glenohumeral, arthritis, injection, corticosteroid, hyaluronic acid
Shoulder disorders are a cause for significant morbidity, with a prevalence of 6.9% to 34% in the general population and up to 21% in those over 70 years old.15 These debilitating disorders present a challenge to the treating clinician; conservative treatment options are finite before surgery is indicated. Current modalities include physical therapy, corticosteroid injection, viscosupplementation with hyaluronic acid (HA), nonsteroidal anti-inflammatory drugs (NSAIDs), and glucosamine and chondroitin sulfate. The success of these therapies may in part be based on the self-limiting nature of conditions such as adhesive capsulitis.
Shoulder injections of corticosteroids and HA are not limited to the glenohumeral joint. Rather, they are used in conditions of the subacromial space, acromioclavicular joint, bicipital tendon sheath, sternoclavicular joint, and the subcoracoid bursa.51 Though the use of HA is approved by the Food and Drug Administration for intra-articular injections in the knee, it remains an off-label use in the shoulder and its surrounding spaces. In this review, intra-articular injections to the pathologies affecting the glenohumeral joint are addressed with focus on corticosteroids and viscosupplementation.
The accuracy of injection delivery to the glenohumeral joint proper has been unreliable.55 Tobola et al55 examined the accuracy of intra-articular injection utilizing anterior, supraclavicular, and posterior approaches. Differences among these approaches were not significant; the anterior approach had a reliability of 64.7%, compared with 45.7% and 45.5% for supraclavicular and posterior approaches, respectively. However, anatomic delivery of injectable medications into the glenohumeral joint may not be relevant.26 Hegedus et al found that relief of shoulder pain with injectables did not correlate with clinician experience, injection intra- or extracapsularly, and duration of symptoms.26
Corticosteroids
Injectable steroids have been in use for decades to treat various disorders of the glenohumeral joint.3 Much of the evidence supporting the use of corticosteroids is anecdotal. Indeed, level 1 and 2 evidence supporting the use of intra-articular corticosteroids is lacking. Confounding variables such as physiotherapy, analgesics, and NSAIDs also make it difficult to arrive at definitive conclusions or recommendations.3
Properties
The pharmacologic properties of corticosteroids have been well documented.10,23 They act locally and are much like the anti-inflammatory effects of systemic steroids10,23 In the knee, local lymphocytes, macrophages, mast cells, and overall edema of the joint after injection with Depo-Medrol occurs.45 Local corticosteroid injection also decreases the erythrocyte-sedimentation rate and C-reactive protein in patients with rheumatoid arthritis.16
The injectable formulations vary by molecular size, crystal structure, serum half-life, solubility, fluorination, and duration of action.16 Water-soluble steroids (dexamethasone) rapidly dissipate from the joint and exert many systemic side effects.16 These are primarily helpful with extra-articular uses such as carpal tunnel. Conversely, formulations with lower solubility maintain longer synovial levels with decreased systemic effects.16 The length of action for each steroid varies widely among different corticosteroids (Table 1).5,10,23 While decreased solubility maintains longevity within the synovium, solubility is not correlated to duration of action.46 The chemical structure of the steroid also affects activity: fluorinated compounds (Decadron, Kenalog, Aristospan, Celestone) have increased activity and systemic absorption42 and a higher rate of side effects. Moore suggests that the use of fluorinated compounds be limited to intra-articular injections because of the higher rate of tendon rupture and subcutaneous collagen atrophy.39 Flocculation (colloids out of solution) can also occur with the mixture of corticosteroids and local anesthetic agents and may inhibit the local effects of the steroid.
Table 1.
Injectable corticosteroid properties.
| Generic Name: Trade Name | Dose, mg17 | Solubility, % wt/vol20 | Mean Duration of Action, d5,23 | Fluorinated |
|---|---|---|---|---|
| Methylprednisolone diacetate: Depo-Medrol | 40-60 | .001 | 7-84 | No |
| Prednisolone tebutate: Hydeltra-TBA | 5-50 | .001 | 10-15 | No |
| Triamcinolone acetonide: Kenalog | 5-40 | .004 | 11 | Yes |
| Triamcinolone hexetidine: Aristospan | 5-40 | .0002 | 3 | Yes |
| Betamethasone sodium phosphate, betamethasone acetate: Celestone Soluspan | 1.5-6 | NA | 9 | Yes |
The most effective dosage and specific type of corticosteroid are not known (Table 1). Recommendations for the frequency of intra-articular injection are empirically based on the recommendations of the American College of Rheumatology.25 Generally, a steroid should not be injected into the same joint more than every 3 months.25 Aspirating synovial fluid at the time of injection and resting the joint may decrease painful relapses.13,19
Side Effects and Complications
The complication rate of intra-articular corticosteroid injections is relatively low (1%-15%).25 One of the most common complications is transient pain during injection and/or postinjection (6.7%). Flare-up pain usually lasts 24 to 48 hours and most likely results from a transient reactive synovitis in response to the steroid crystals. Facial flushing may occur in up to 15% of patients, with a greater number of women affected. The effects are transient, lingering for no more than 3 days.33 Skin or subcutaneous fat atrophy may occur after corticosteroid injection and may persist longer than 6 months (.35%).32 Septic arthritis is the greatest concern, occurring from 1:3000 to 1:50 000.14 Hyaline cartilage damage has been reported in animal models but not in humans.16 Contraindications to intra-articular corticosteroid injection include a prosthetic joint, septic arthritis, and joint fracture.32
The hypothalamic pituitary-adrenal axis may be suppressed with corticosteroids injected locally. A single intra-articular injection of methylprednisone acetate showed an average 21.5% reduction in serum cortisol 24 hours after injection normalizing in 3 days.34
Glenohumeral Arthritis
The glenohumeral joint is the third-most-common large joint affected by degenerative joint disease.37 It is usually diagnosed at much later stages of disease and less frequently than knees or hips. Conservative management for glenohumeral arthritis includes activity modification, physical therapy to promote strength and flexibility, nonnarcotic medications to reduce pain, intra-articular corticosteroid injections to reduce local inflammation, viscosupplementation, and general health maintenance.44
There is currently no level 1 or 2 studies on intra-articular corticosteroid injections as a treatment modality for glenohumeral arthritis.29 While literature suggests that injectable corticosteroid therapy is a treatment modality for shoulder arthritis, not one lists shoulder-specific evidence. According to the most recent guidelines54 for the treatment of glenohumeral arthritis, by the American Academy of Orthopaedic Surgeons, the use of injectable corticosteroids is inconclusive. Unfortunately, the organization is unable to recommend for or against glenohumeral corticosteroid injections.54 One study does address corticosteroids in comparison to HA in treating shoulder osteoarthritis.38 This is discussed in the HA section (Table 2).
Table 2.
Study characteristics of hyaluronic acid and corticosteroid use for arthritis.
| Study | Type | Patients, n | Follow-up, wk | Treatment Arm | Control Arm | Outcomes Measures |
|---|---|---|---|---|---|---|
| Merolla38 | Retrospective controlled | 84 | 26 | Hylan G-F 20 | Methylprednisolone acetate | Constant-Murley, Shoulder Pain and Disability Index, satisfaction |
The use of corticosteroids in glenohumeral arthritis is based on its effects on the synovium and surrounding tissue, as well as its clinical efficacy in other arthrodial joints, especially the knee.6 Triamcinolone hexetidine injection in knee osteoarthritis19 showed improved visual analog pain scale at 1 week compared to placebo. An intra-articular injection of methylprednisolone acetate demonstrated a significant reduction in pain at 3 weeks.30 However, at 6 to 8 weeks, no appreciable difference was seen in either steroid. A more successful response was seen in patients with an intra-articular effusion and aspiration of synovial fluid at the time of injection.30 A 24-month randomized trial with triamcinolone acetate injection of symptomatic knees every 3 months noted improvement in range of motion and slightly improved pain at 1 year.47 Patients in the steroid group had improved knee pain and stiffness and no difference in joint space at the end of 2 years.
Adhesive Capsulitis
Adhesive capsulitis (frozen shoulder) affects 2% to 5% of the adult population.41 It may be idiopathic or present after shoulder immobilization, trauma, or surgery.56 It may be intrinsic (tightening of the joint capsule) or extrinsic (scarring of the rotator interval or external rotators). It is usually self-limiting and has 3 phases: freezing, frozen, and thawing.56 In the first stage, capsular inflammation occurs8; consequently, intra-articular corticosteroid injections are thought to be best during this initial phase. In a systematic review of corticosteroid injections compared with physical therapy in the treatment of adhesive capsulitis, greater improvements in shoulder pain and function in the short term are reported with glenohumeral joint corticosteroid injections versus physical therapy (Table 3).8 Greater efficacy of glenohumeral corticosteroid injections compared with physical therapy57 persisted at 1 year and were more beneficial than physical therapy and NSAIDs combined.4
Table 3.
Study characteristics of corticosteroid treatment of adhesive capsulitis. a
| Study | Type | Patients, n | Follow-up, wk | Treatment Arm | Control Arm | Outcomes Measures |
|---|---|---|---|---|---|---|
| Arlsan4 | RCT | 20 | 2, 12 | 40 mg, methylprednisolone | NSAIDs, PT | VAS, ROM |
| Blanchard8 | SR | 362 | Up to 52 | Triamcinolone or methylprednisolone | PT | VAS, ROM, SPADI, SF-36 |
| de Jong18 | RCT | 25 | 1,3,6 | 40 mg, triamcinolone | 10 mg, triamcinolone | Pain, sleep disturbance |
| Griesser24 | SR | 409 | Up to 52 | Triamcinolone or methylprednisolone | PT, oral steroid, manipulation, ice pack, no treatment | SPADI, VAS, SF-36, ROM |
| Rizk48 | RCT | 48 | 3 | 40 mg, methylprednisolone | Lidocaine, PT | Pain, ROM |
| van der Windt57 | RCT | 109 | 3, 7, 13, 26, 52 | 40 mg, triamcinolone (no more than 3 injections) | 12 sessions of PT | VAS day and night, passive lateral rotation and abduction |
RCT, randomized controlled trial; SR, systematic review; NSAIDs, nonsteroidal anti-inflammatory drugs; PT, physical therapy; VAS, visual analog scale; ROM, range of motion; SPADI, Shoulder Pain and Disability Index.
The dose of steroid affects the outcome of adhesive capsulitis. Glenohumeral injection of 40 mg triamcinolone acetonide (vs 10 mg)18 relieved more pain at 6 weeks. Arm function and glenohumeral range of motion improved, while sleep disturbances were unchanged.61
The data for corticosteroid treatment versus placebos or traditional oral medication are sparse. Studies comparing corticosteroid injection to lidocaine injection48 have mixed results. In a double-blind intention-to-treat analysis at 6 months, there were no differences in range of motion or pain in the corticosteroid or lidocaine injection group.48 In an unblinded study comparing steroid injection to NSAID therapy, glenohumeral injection reduced pain more than analgesia alone at 6 weeks.35,48 Interestingly, the location of injection was not a determinant of clinical effect; a steroid injection into the bicipital tendon sheath also provided pain relief. A systematic review of existing level 1 and 2 evidence comparing injectable steroids and no treatment, ice pack, or low volume of intra-articular saline solution showed that the corticosteroid group provided earlier return of shoulder motion and improvement in Shoulder Pain and Disability Index scores, but at 52 weeks, there was no difference between the groups.24
Hyaluronic Acid
Hyaluronic acid is a high–molecular weight glycosaminoglycan composed of repeating disaccharide units of glucuronic acid and N-acetyl-glucosamine.9,52 The viscoelastic properties of HA play a critical role in joint mechanics in synovial fluid.9,50,52,59 Exogenous HA has anti-inflammatory, anabolic, analgesic, and chondroprotective effects.28,40
Properties
In animal models, HA preparations with high molecular weight have increased efficacy.27 Though proven to have anti-inflammatory and analgesic effects, the precise mechanism for pain relief is not known, given that it has a short half-life in the joint.21,40 The temporary improvement of normal viscoelastic joint properties likely contributes to pain relief, but it is unclear if HA anti-inflammatory effects contribute to viscosupplementation long-term relief. HA may coat the articular cartilage and prevent loss of essential chondrocyte matrix molecules, such as prostaglandins.40 Exogenous HA may facilitate the de novo synthesis of HA.2,40 The interplay between mechanical and biological effects likely contributes to the difficulty in assessing the therapeutic effect for viscosupplementation. While the use of viscosupplementation in joints other than the knee has not yet been approved by the Food and Drug Administration, recent clinical studies have begun to address its potential use in the hip, ankle, and, more recently, the shoulder.50,52
Side Effects and Complications
The side effect profile of viscosupplementation includes acute local reactions (pain and swelling in the joint within 72 hours), flare-up of pseudogout, and pseudosepsis (acute systemic inflammatory reactions).22,36,60 In a series of 4253 injections, acute local reactions occurred at a rate of 2.4%31; another study reported adverse reactions in 1.2% per injection or 5.2% per patient in a series of 1489 injections.58 Higher molecular weight HA preparations have been shown to be safer with a decreased infection rate, since lower weight preparations require more frequent treatment to achieve the same clinical result.1 Preparations that include HA derived from rooster combs may have increased immunogenicity and may account for the few cases of pseudosepsis in patients.60
Several publications conflict on whether rates of adverse reactions are increased in patients with repeat injections of HA.36,58,60 While some studies report an eightfold increase in adverse reactions in subsequent injections, others show adverse reaction rates less than those from the first series of injections.36,60 Another series reports the incidence of treatment-related adverse reactions to be 0.8% (3.4% of patients) in the first series, 4.3% (13.1%) in the second, and 5.4% (17.3%) in the third.58
Glenohumeral Osteoarthritis
Patients with glenohumeral osteoarthritis treated with HA had a significant decrease in pain and significant improvements in activities of daily living, based on visual analog scale, University of California–Los Angeles, and Simple Shoulder Test scores (Table 4).50 More patients slept comfortably after treatment (56%) than before (15%). However, the authors were unable to conclude which patients would benefit from HA therapy. Another prospective trial showed that at 3 months, the visual analog scale significantly decreased from 61.2 to 37.1 after 1 or 2 injections of HA.43
Table 4.
Study design for intra-articular injections of hyaluronic acid for osteoarthritis. a
| Study | Type | Patients, n | Follow-up, wk | Treatment Arm | Control Arm | Outcomes Measures |
|---|---|---|---|---|---|---|
| Noel43 | Prospective | 39 | 26 | Hylan G-F 20 | None | VAS |
| Silverstein50 | Prospective | 30 | 26 | 3 injections of Hylan G-F 20 | None | VAS, UCLA, SST |
| Blaine7 | RCT | 456 | 26 | Sodium hyaluronate | Saline | VAS |
| Merolla38 | Retrospective controlled | 84 | 26 | Hylan G-F 20 | Methylprednisolone acetate | Constant-Murley, SPADI, satisfaction |
RCT, randomized controlled trial; VAS, visual analog scale; UCLA, University of California–Los Angeles; SST, Simple Shoulder Test; SPADI, Shoulder Pain and Disability Index.
In a multicenter, randomized, double-blind, controlled trial,7 the efficacy and safety of intra-articular injections of sodium hyaluronate (molecular weight, 500 to 730 kDa) for persistent shoulder pain and limited function, including glenohumeral joint arthritis, torn rotator cuff, and/or adhesive capsulitis, were studied. Patients with osteoarthritis showed significant pain and visual analog scale score improvement with both 3 and 5 glenohumeral injection regimens at both 7 and 26 weeks. However, this improvement was not maintained for every intermediary time point, and results are similar to previous studies investigating 3- and 5-injection regimens in the knee.12
One study evaluated the efficacy of HA versus methylprednisolone acetate in arthritis in 84 patients at 1-, 3-, and 6-month intervals.38 The HA group showed a significant pain reduction, improvement in Constant-Murley and Shoulder Pain and Disability Index scores, and satisfaction at all 3 follow-up times. In the corticosteroid group, improvements in pain, functional outcomes, and satisfaction were present only at 1 month. Outcomes were relative to the degree of arthritis and the presence of rotator cuff tears.
Adhesive Capsulitis
In a clinical study of viscosupplementation for adhesive capsulitis,27 sodium hyaluronate was injected into the glenohumeral joint of 70 patients once per week over the course of 5 weeks. A global improvement rating demonstrated that 51 of 62 patients (82.3%) were slightly improved or better and that 32 of 62 patients (51.6%) were moderately improved or better (Table 5). Pain at rest, motion, pressure, activities of daily living, and range of motion improved.27
Table 5.
Study design of hyaluronic acid injection for adhesive capsulitis. a
| Study | Type | Patients, n | Follow-up, wk | Treatment Arm | Control Arm | Outcomes measures |
|---|---|---|---|---|---|---|
| Itokazu27 | Prospective | 62 | 8 | Sodium hyaluronate 25 mg (1/wk × 5) | None | ROM; pain at rest, motion, pressure |
| Calis11 | RCT | 95 | 12 | Sodium hyaluronate | Triamcinolone acetate vs PT vs no treatment | Pain severity with passive ROM, functional considerations |
| Rovetta49 | RCT | 30 | 26 | Sodium hyaluronate + triamcinolone | Triamcinolone + PT | ROM, pain |
| Tamai53 | Prospective | 11 | 6 | Sodium hyaluronate | None | Coefficient of enhancement of synovium on MRI, JOA score |
RCT, randomized controlled trial; ROM, range of motion; PT, physical therapy; MRI, magnetic resonance imaging; JOA, Japanese Orthopaedic Association shoulder score.
In a study of HA injection, triamcinolone acetonide, or physical therapy modalities,11 significant improvement was observed in pain, passive range of motion, and function on the 15th day after treatment and the third month for both HA treatment and steroid injections. Physical therapy alone demonstrated better pain reduction, passive range of motion, and function compared with both corticosteroid and HA injection.11 While adhesive capsulitis can be treated with physical therapy, a combined HA and corticosteroids injection may offer a suitable alternative; patients that received both injections fared better functionally than those receiving corticosteroids only.49 Researchers do not know why HA injections improve adhesive capsulitis outcomes. One study suggests that clinical improvement may be related to a decrease in synovial inflammation or decreased synovial perfusion in the glenohumeral joint53; another hypothesizes that the HA may decrease shoulder soft tissue retraction by influencing the volume of synovial fluid or regulating joint osmotic pressure.49
Conclusions
There is little scientific support in the literature for the use of intra-articular corticosteroid injections to treat glenohumeral arthritis.38,54 The use of intra-articular corticosteroids for adhesive capsulitis has inconsistent patient-oriented evidence but better literature support than for glenohumeral arthritis.4,8,18,24,48,57 Intra-articular HA injections for osteoarthritis and adhesive capsulitis show promise but lack any well-designed prospective trials to fully evaluate their effectiveness.7,11,27,38,43,49,50,53 While the use of corticosteroids and HA in the conservative management of osteoarthritis and adhesive capsulitis is widespread, its basis rests on limited evidence.
References
- 1. Adams ME, Lussier AJ, Peyron JG. A risk-benefit assessment of injections of hyaluronan and its derivatives in the treatment of osteoarthritis of the knee. Drug Safety. 2000;23:115-130 [DOI] [PubMed] [Google Scholar]
- 2. Altman RD. Osteoarthritis: differentiation from rheumatoid arthritis, causes of pain, treatment. Postgrad Med. 1990;87:66-72 [DOI] [PubMed] [Google Scholar]
- 3. Arroll B, Goodyear-Smith F. Corticosteroid injections for painful shoulder: a meta-analysis. Br J Gen Pract. 2005;55:224-228 [PMC free article] [PubMed] [Google Scholar]
- 4. Arslan S, Celiker R. Comparison of the efficacy of local corticosteroid injection and physical therapy for the treatment of adhesive capsulitis. Rheumatol Int. 2001;21:20-23 [DOI] [PubMed] [Google Scholar]
- 5. Bain LS, Balch HW, Wetherly JM, Yeadon A. Intraarticular triamcinolone hexacetonide: double-blind comparison with methylprednisolone. Br J Clin Pract. 1972;26:559-561 [PubMed] [Google Scholar]
- 6. Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G. Intraarticular corticosteroid for treatment of osteoarthritis of the knee. Cochrane Database Syst Rev. 2006;CD005328. [DOI] [PubMed] [Google Scholar]
- 7. Blaine T, Moskowitz R, Udell J, et al. Treatment of persistent shoulder pain with sodium hyaluronate: a randomized, controlled trial. A multicenter study. J Bone Joint Surg Am. 2008;90:970-979 [DOI] [PubMed] [Google Scholar]
- 8. Blanchard V, Barr S, Cerisola FL. The effectiveness of corticosteroid injections compared with physiotherapeutic interventions for adhesive capsulitis: a systematic review. Physiotherapy. 2010;96:95-107 [DOI] [PubMed] [Google Scholar]
- 9. Brockmeier SF, Shaffer BS. Viscosupplementation therapy for osteoarthritis. Sports Med Arthrosc. 2006;14:155-162 [DOI] [PubMed] [Google Scholar]
- 10. Caldwell JR. Intra-articular corticosteroids: guide to selection and indications for use. Drugs. 1996;52:507-514 [DOI] [PubMed] [Google Scholar]
- 11. Calis MDH, Ulker S, Kirnap M, Duygulu F, Calis HT. Is intraarticular sodium hyaluronate injection an alternative treatment in patients with adhesive capsulitis? Rheumatol Int. 2006;26:536-540 [DOI] [PubMed] [Google Scholar]
- 12. Carrabba M, Paresce E, Angelini M, Galanti A, Marini MG, Cigarini P. A comparison of the local tolerability, safety and efficacy of meloxicam and piroxicam suppositories in patients with osteoarthritis: a single-blind, randomized, multicentre study. Curr Med Res Opin. 1995;13:343-355 [DOI] [PubMed] [Google Scholar]
- 13. Chakravarty K, Pharoah PD, Scott DG. A randomized controlled study of post-injection rest following intra-articular steroid therapy for knee synovitis. Br J Rheumatol. 1994;33:464-468 [DOI] [PubMed] [Google Scholar]
- 14. Charalambous CP, Tryfonidis M, Sadiq S, Hirst P, Paul A. Septic arthritis following intra-articular steroid injection of the knee: a survey of current practice regarding antiseptic technique used during intra-articular steroid injection of the knee. Clin Rheumatol. 2003;22:386-390 [DOI] [PubMed] [Google Scholar]
- 15. Chard MD, Hazleman R, Hazleman BL, King RH, Reiss BB. Shoulder disorders in the elderly: a community survey. Arthritis Rheum. 1991;34:766-769 [DOI] [PubMed] [Google Scholar]
- 16. Cole BJ, Schumacher HR. Injectable corticosteroids in modern practice. J Am Acad Orthop Surg. 2005;13:37-46 [DOI] [PubMed] [Google Scholar]
- 17. Cush JKA. Synovial fluid analysis, arthrocentesis, and joint injection techniques. In: Cush JKA, ed. Rheumatology: Diagnosis and Therapeutics. Philadelphia, PA: Lippincott Williams & Wilkins; 2000:61-73 [Google Scholar]
- 18. de Jong BA, Dahmen R, Hogeweg JA, Marti RK. Intra-articular triamcinolone acetonide injection in patients with capsulitis of the shoulder: a comparative study of two dose regimens. Clin Rehabil. 1998;12:211-215 [DOI] [PubMed] [Google Scholar]
- 19. Gaffney K, Ledingham J, Perry JD. Intra-articular triamcinolone hexacetonide in knee osteoarthritis: factors influencing the clinical response. Ann Rheum Dis. 1995;54:379-381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Genovese MC. Joint and soft-tissue injection: a useful adjuvant to systemic and local treatment. Postgrad Med. 1998;103:125-134 [DOI] [PubMed] [Google Scholar]
- 21. Gigante A, Callegari L. The role of intra-articular hyaluronan (Sinovial) in the treatment of osteoarthritis. Rheumatol Int. 2011;31:427-444 [DOI] [PubMed] [Google Scholar]
- 22. Goldberg VM, Coutts RD. Pseudoseptic reactions to hylan viscosupplementation: diagnosis and treatment. Clin Orthop Relat Res. 2004:419:130-137 [DOI] [PubMed] [Google Scholar]
- 23. Gray RG, Gottlieb NL. Intra-articular corticosteroids: an updated assessment. Clin Orthop Relat Res. 1983:177:235-263 [PubMed] [Google Scholar]
- 24. Griesser MJ, Harris JD, Campbell JE, Jones GL. Adhesive capsulitis of the shoulder: a systematic review of the effectiveness of intra-articular corticosteroid injections. J Bone Joint Surg Am. 2011;93:1727-1733 [DOI] [PubMed] [Google Scholar]
- 25. Guidelines ACoRSoRA: Guidelines for the management of rheumatoid arthritis: 2002 update Arthritis Rheum. 2002;46:328-346 [DOI] [PubMed] [Google Scholar]
- 26. Hegedus EJ, Zavala J, Kissenberth M, et al. Positive outcomes with intra-articular glenohumeral injections are independent of accuracy. J Shoulder Elbow Surg. 2010;19:795-801 [DOI] [PubMed] [Google Scholar]
- 27. Itokazu M, Matsunaga T. Clinical evaluation of high-molecular-weight sodium hyaluronate for the treatment of patients with periarthritis of the shoulder. Clinical Ther. 1995;17:946-955 [DOI] [PubMed] [Google Scholar]
- 28. Iwata H. Pharmacologic and clinical aspects of intraarticular injection of hyaluronate. Clin Orthop Relat Res. 1993;289:285-291 [PubMed] [Google Scholar]
- 29. Izquierdo R, Voloshin I, Edwards S, et al. Treatment of glenohumeral osteoarthritis. J Am Acad Orthop Surg. 2010;18:375-382 [DOI] [PubMed] [Google Scholar]
- 30. Jones A, Doherty M. Intra-articular corticosteroids are effective in osteoarthritis but there are no clinical predictors of response. Ann Rheum Dis. 1996;55:829-832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kemper F, Gebhardt U, Meng T, Murray C. Tolerability and short-term effectiveness of hylan G-F 20 in 4253 patients with osteoarthritis of the knee in clinical practice. Curr Med Res Opin. 2005;21:1261-1269 [DOI] [PubMed] [Google Scholar]
- 32. Kumar N, Newman RJ. Complications of intra- and peri-articular steroid injections. Br J Gen Pract. 1999;49:465-466 [PMC free article] [PubMed] [Google Scholar]
- 33. Lanyon PDM. Intra-articular therapy. In: Firestein GSPG, Wollheim FA, eds. Rheumatoid Arthritis: Frontiers in Pathogenesis and Treatment. Oxford, UK: Oxford University Press; 2000:361-369 [Google Scholar]
- 34. Lazarevic MB, Skosey JL, Djordjevic-Denic G, Swedler WI, Zgradic I, Myones BL. Reduction of cortisol levels after single intra-articular and intramuscular steroid injection. Am J Med. 1995;99:370-373 [DOI] [PubMed] [Google Scholar]
- 35. Lee M, Haq AM, Wright V, Longton EB. Periarthritis of the shoulder: a controlled trial of physiotherapy. Physiotherapy. 1973;59:312-315 [PubMed] [Google Scholar]
- 36. Leopold SS, Warme WJ, Pettis PD, Shott S. Increased frequency of acute local reaction to intra-articular hylan GF-20 (synvisc) in patients receiving more than one course of treatment. J Bone Joint Surg Am. 2002;84:1619-1623 [DOI] [PubMed] [Google Scholar]
- 37. Matsen FA, Rockwood CA, Wirth MA, Lippitt SB, Moby P. Glenohumeral arthritis and its management. In: The Shoulder . 3rd ed Philadelphia, PA: Saunders; 2004:879-1009 [Google Scholar]
- 38. Merolla G, Sperling JW, Paladini P, Porcellini G. Efficacy of Hylan G-F 20 versus 6-methylprednisolone acetate in painful shoulder osteoarthritis: a retrospective controlled trial. Musculoskelet Surg. 2011;95:215-224 [DOI] [PubMed] [Google Scholar]
- 39. Moore G. Arthrocentesis technique and intraarticular therapy. In: Koopman WJ, ed. Arthritis and Allied Conditions: A Textbook of Rheumatology. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:848-859 [Google Scholar]
- 40. Moreland LW. Intra-articular hyaluronan (hyaluronic acid) and hylans for the treatment of osteoarthritis: mechanisms of action. Arthritis Res Ther. 2003;5:54-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Neer CSSC, Dalsey RM. On the value of the coracohumeral ligament release. Orthopedic Trans. 1989;13:235-236 [Google Scholar]
- 42. Nesbitt LT. Minimizing complications from systemic glucocorticosteroid use. Dermatol Clin. 1995;13(4):925-939 [PubMed] [Google Scholar]
- 43. Noel E, Hardy P, Hagena FW, et al. Efficacy and safety of Hylan G-F 20 in shoulder osteoarthritis with an intact rotator cuff: open-label prospective multicenter study. Joint Bone Spine. 2009;76:670-673 [DOI] [PubMed] [Google Scholar]
- 44. Parsons IMT, Weldon EJ, Titelman RM, Smith KL. Glenohumeral arthritis and its management. Phys Med Rehabil Clin N Am. 2004;15:447-474 [DOI] [PubMed] [Google Scholar]
- 45. Pasquali Ronchetti I, Guerra D, Taparelli F, et al. Morphological analysis of knee synovial membrane biopsies from a randomized controlled clinical study comparing the effects of sodium hyaluronate (Hyalgan) and methylprednisolone acetate (Depomedrol) in osteoarthritis. Rheumatology (Oxford). 2001;40:158-169 [DOI] [PubMed] [Google Scholar]
- 46. Pyne D, Ioannou Y, Mootoo R, Bhanji A. Intra-articular steroids in knee osteoarthritis: a comparative study of triamcinolone hexacetonide and methylprednisolone acetate. Clin Rheumatol. 2004;23:116-120 [DOI] [PubMed] [Google Scholar]
- 47. Raynauld JP, Buckland-Wright C, Ward R, et al. Safety and efficacy of long-term intraarticular steroid injections in osteoarthritis of the knee: a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2003;48:370-377 [DOI] [PubMed] [Google Scholar]
- 48. Rizk TE, Pinals RS, Talaiver AS. Corticosteroid injections in adhesive capsulitis: investigation of their value and site. Arch Phys Med Rehabil. 1991;72:20-22 [PubMed] [Google Scholar]
- 49. Rovetta G, Monteforte P. Intraarticular injection of sodium hyaluronate plus steroid versus steroid in adhesive capsulitis of the shoulder. Int J Tissue React. 1998;20:125-130 [PubMed] [Google Scholar]
- 50. Silverstein E, Leger R, Shea KP. The use of intra-articular hylan G-F 20 in the treatment of symptomatic osteoarthritis of the shoulder: a preliminary study. Am J Sports Med. 2007;35:979-985 [DOI] [PubMed] [Google Scholar]
- 51. Stitik TP, Foye PM, Fossati J. Shoulder injections for osteoarthritis and other disorders. Phys Med Rehabil Clin N Am. 2004;15:407-446 [DOI] [PubMed] [Google Scholar]
- 52. Strauss EJ, Hart JA, Miller MD, Altman RD, Rosen JE. Hyaluronic acid viscosupplementation and osteoarthritis: current uses and future directions. Am J Sports Med. 2009;37:1636-1644 [DOI] [PubMed] [Google Scholar]
- 53. Tamai K, Mashitori H, Ohno W, Hamada J, Sakai H, Saotome K. Synovial response to intraarticular injections of hyaluronate in frozen shoulder: a quantitative assessment with dynamic magnetic resonance imaging. J Orthop Sci. 2004;9(3):230-234 [DOI] [PubMed] [Google Scholar]
- 54. The treatment of glenohumeral joint arthritis: guideline and evidence report. http://www.aaos.org/research/guidelines/gloguideline.pdf. Published 2008 Accessed May 5, 2012
- 55. Tobola A, Cook C, Cassas KJ, et al. Accuracy of glenohumeral joint injections: comparing approach and experience of provider. J Shoulder Elbow Surg. 2011;20(7):1147-1154 [DOI] [PubMed] [Google Scholar]
- 56. Tonino PM, Gerber C, Itoi E, Porcellini G, Sonnabend D, Walch G. Complex shoulder disorders: evaluation and treatment. J Am Acad Orthop Surg. 2009;17:125-136 [DOI] [PubMed] [Google Scholar]
- 57. van der Windt DA, Koes BW, Deville W, Boeke AJ, de Jong BA, Bouter LM. Effectiveness of corticosteroid injections versus physiotherapy for treatment of painful stiff shoulder in primary care: randomised trial. BMJ. 1998;317:1292-1296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Waddell DD, Bricker DC. Hylan G-F 20 tolerability with repeat treatment in a large orthopedic practice: a retrospective review. J Surg Orthop Adv. 2006;15(1):53-59 [PubMed] [Google Scholar]
- 59. Watterson JR, Esdaile JM. Viscosupplementation: therapeutic mechanisms and clinical potential in osteoarthritis of the knee. J Am Acad Orthop Surg. 2000;8:277-284 [DOI] [PubMed] [Google Scholar]
- 60. Webber TA, Webber AE, Matzkin E. Rate of adverse reactions to more than 1 series of viscosupplementation. Orthopedics. 2012;35:e514-e519 [DOI] [PubMed] [Google Scholar]
- 61. White A, Tuite JD. The accuracy and efficacy of shoulder injections in restrictive capsulitis. J Orthop Rheum. 1996;9:37-40 [Google Scholar]