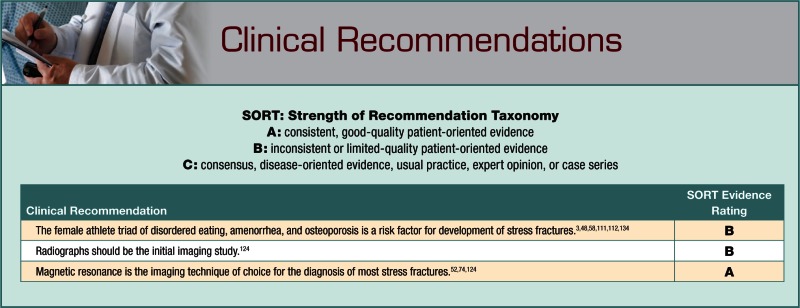
Abstract
Context:
Stress fractures are common injuries in athletes, often difficult to diagnose. A stress fracture is a fatigue-induced fracture of bone caused by repeated applications of stress over time.
Evidence Acquisition:
PubMed articles published from 1974 to January 2012.
Results:
Intrinsic and extrinsic factors may predict the risk of stress fractures in athletes, including bone health, training, nutrition, and biomechanical factors. Based on their location, stress fractures may be categorized as low- or high-risk, depending on the likelihood of the injury developing into a complete fracture. Treatment for these injuries varies substantially and must account for the risk level of the fractured bone, the stage of fracture development, and the needs of the patient. High-risk fractures include the anterior tibia, lateral femoral neck, patella, medial malleolus, and femoral head. Low-risk fractures include the posteromedial tibia, fibula, medial femoral shaft, and pelvis. Magnetic resonance is the imaging test of choice for diagnosis.
Conclusions:
These injuries can lead to substantial lost time from participation. Treatment will vary by fracture location, but most stress fractures will heal with rest and modified weightbearing. Some may require more aggressive intervention, such as prolonged nonweightbearing movement or surgery. Contributing factors should also be addressed prior to return to sports.
Keywords: stress fractures, athletes, lower extremity, treatment
Stress fractures were first reported in the metatarsals of Prussian soldiers in 1855,26 and Stechow found radiographic evidence of metatarsal stress fractures of military recruits in 1897.126 The earliest known diagnosis of a stress fracture on the femoral shaft in an athlete occurred in 1934.105 Devas published the first comprehensive study of incidence in a series of athletes with fibular stress fractures in 1956.43
Growing participation in athletic activity coupled with improving medical technology has resulted in a greater awareness of stress fractures. A comprehensive study of 320 cases in athletes describes the distribution of stress fractures based on bone location, associated activity, sex, and age.87 Stress fractures most commonly occur in the metatarsals, tibia, fibula, and tarsal navicular of track and field athletes, runners, and dancers.30 In one study, over a 2-year period, 34 of 914 varsity collegiate 1-AA athletes were diagnosed with a stress fracture.67 These fractures account for over 10% of all injuries in sports medicine clinics,125 and in running sports, they may account for up to 31% of all injuries.73
A stress fracture is a fatigue fracture of bone caused by repeated submaximal stress.20,52 The force required to generate a stress fracture is less than the maximum tolerated by bone, but its repetitive application causes a disruption in the bone homogeneity.101,135 During athletic activity, fatigued muscles subject the bone to increasing force, which may contribute to the overloading process.47,125 Over time, microfractures accumulate and a stress fracture may develop.68
“Stress fracture” is often used synonymously with stress reaction. A stress reaction is bone inflammation seen on a magnetic resonance imaging (MRI) or radionucleotide bone scan; it is possibly a microfracture of bone.68 A stress fracture is a true fracture with cortical disruption.11,55,87,122
In the competitive athlete, a stress fracture can be difficult to treat, with return to activity ranging from weeks43,92 to months132 depending on the location. A premature return to full activity may increase the risk of complications. If complete union is not obtained prior to a return to full activity, an athlete risks delayed union or nonunion.20 Therefore, early recognition and prompt treatment are important to the management of these injuries.36
Predisposing Factors
Training
Training habits, combined with biologic and biomechanical factors, contribute to stress fractures. A sudden increase in exercise intensity increases the risk of a stress fracture.58 When training is progressed rapidly, bones may sustain extra force due to muscle fatigue.14 This theory is supported by evidence that military recruits are most likely to endure a stress fracture during their first weeks of service.63 Additionally, in one study, elite male European soccer players with a shorter preseason were at a higher risk for developing stress fractures.48 The protective effect of physical training in preventing lower extremity stress injury has been demonstrated in recruits entering into the naval conditioning program.3,111
Several studies have correlated running mileage and risk of stress fractures.112,134 In a randomized study of 350 male army recruits in a standard running regimen or a weighted marching program, a reduction in running distance resulted in fewer injuries and lower injury severity.112 A surveyed cohort of 1680 runners correlated running mileage as well as year-round running with increased risk for injury, including stress fractures.134
Bone Health
From development to degradation, bone health is influenced by diet,9,16 hormone levels,9,16,133 and biomechanics.32,53,75,88 Bone of high mineral density may be less likely to endure a stress fracture because it can better withstand repetitive applications of force,15,119 although studies are contradictory.13,16,40,106 A prospective cohort of track and field athletes found statistically significant lower values for total body mineral content and lumbar spine and foot bone mineral density in female athletes sustaining stress fractures.16 A trend was noted for decreased bone density in men sustaining stress fractures, though this was not statistically significant.16
Diet may influence bone health and risk of stress fractures.65,86,106,123 A prospective cohort of competitive female distance runners showed that increased calcium, vitamin D, and protein intake correlated with increased bone mineral density and protection from stress fractures, while potassium was associated with increased bone mineral density alone.100 Protein likely improves calcium absorption or increases insulinlike growth factor 1 with subsequent skeletal benefit.71 Potassium is associated with higher fruit and vegetable intake,84 reduced bone turnover,99 and increased alkali load.108 An additional cup of skim milk consumed per day may reduce the incidence of stress fractures by 62%.100 A double-blind, placebo-controlled trial of female navy recruits showed a 20% lower incidence of stress fractures in those consuming 2000 mg of calcium and 800 international units of vitamin D daily.76 A small study of male recruits found no statistical difference in stress fractures with a supplemental 500 mg of calcium daily.118
The female athlete triad of disordered eating, amenorrhea, and osteoporosis significantly increases the risk of stress fracture because of the negative effect on bone health.9,16 Amenorrhea in athletes is multifactorial, resulting from energy deficit, decreased leptin levels,81 decreased gonadotropins,8 and/or stress from competition. The end result is a hypoestrogenemic state.49 Lower estrogen levels result in increased calcium resorption and decreased bone storage of calcium.49 A small case-control study of 19 female athletes showed direct correlations between the incidence of stress fractures and both current menstrual abnormalities and decreased bone mineral density.98 The relative risk of stress fracture in athletes with menstrual disturbances is 2 to 4 times that of eumenorrheic athletes.12
Biomechanics
Leg length discrepancy may predispose an athlete to a stress fracture.32,53,75 In army recruits, 73% with leg length inequalities sustained stress fractures in the longer leg, and a discrepancy greater than 5 mm increased the likelihood of fracture.53 In another study, stress fractures occurred more often in the shorter leg, with a mean leg length difference of 1.3 mm between controls and patients.75 Other studies demonstrate that stress fractures occur in both short and long legs.16,75
Athletes with tibial stress fractures have more knee joint stiffness during initial loading.93 Peak hip adduction and rearfoot eversion angles during the stance phase of running were increased in runners with previous tibial stress fractures.94 Biomechanical studies suggest that gait retraining to reduce tibial acceleration and loading may reduce stress fractures.41 A prospective clinical study of military recruits found that those with pes planus (flatfoot) have an increased risk of metatarsal stress fractures, and those with pes cavus (high arch) are prone to femoral and tibial stress fractures.123 Additionally, foot pronation may be a factor in the development of stress fractures, as biomechanical data in runners suggest that rotation helps distribute the impact throughout the tibia and lower extremity.88
Training Surface and Footwear
Hard surfaces usually pose a higher risk for stress fractures.66,90 Tibial strain and strain rates in runners were 48% to 285% higher when running over ground compared with treadmills.90 In a prospective cohort study of 582 habitual runners, females had a greater risk of injury when running on concrete surfaces.82 Worn running shoes may increase the risk for stress fracture because of decreased shock absorption,56 similar to combat boots.5 A meta-analysis of randomized controlled trials on insoles suggests a reduction in stress fractures in the military population.111
Diagnosis
Patient History
Stress fractures may be preceded by an increase in activity83 and present initially with discomfort only during activity.36 The pain usually progresses after activity, eventually leading to pain at rest.17 Female athletes are 1.5 to 3.5 times more likely to sustain a stress fracture than male athletes,32,138 and fewer risk factors are known for men.16,133 Low testosterone levels may increase risk for male athletes.15,33 African Americans are less prone to stress fractures, possibly due to increased bone mass, size, and geometry.77,114
Physical Examination
Clinical assessment begins with lower limb alignment (varus or valgus) and symmetry in the legs, ankles, and feet, as these may effect biomechanical forces.27,83 Pes planus or cavus may increase the risk of certain stress fractures.123 Local tenderness,29 swelling, and warmth may be present.87 Chronic cases may present with a palpable callus.137 If the suspected fracture is not readily palpable, such as the femoral neck, range of motion should be evaluated for pain.20 The fulcrum test (Figure 1) may help diagnose stress fractures.67
Figure 1.

Fulcrum test: Examiner applies downward pressure on the knee with the opposite arm under the patient’s thigh. A positive test result elicits thigh pain.
Sacral stress fractures may produce a positive FABER (Figure 2); and/or Flamingo test(s), pain with hip flexion, abduction, and external rotation, or pain when standing on the affected limb, respectively.24,39
Figure 2.

FABER test: Examiner applies downward pressure on the knee. A positive test result elicits pelvic or groin pain.
Imaging
Standard radiography
Standard radiographs are commonly used as the initial assessment of suspected stress fractures and can confirm the diagnosis.124 However, in the early stages, radiographs have a low sensitivity (10%) and are of limited utility.52
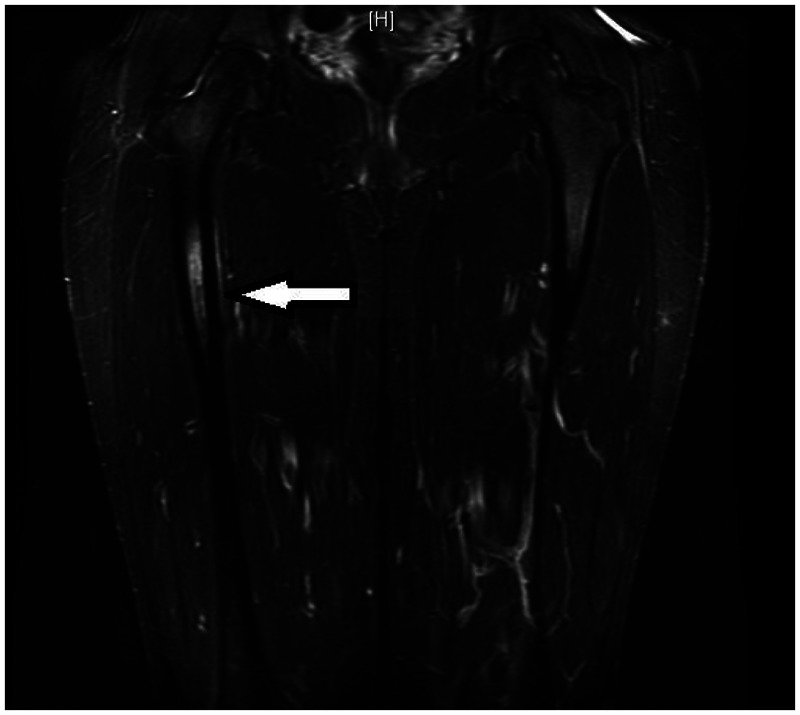
Magnetic resonance imaging
MRI is the most comprehensive method to evaluate a potential stress fracture4,50,52,74,124 because of a high level of both sensitivity (86%-100%) and specificity (100%). Recovery time may be predictable based on a 4-level grading system originally described in the tibia (Figure 3).4,17,20,55,74,121 This system can be applied to other bones (Table 1).4,78
Figure 3.
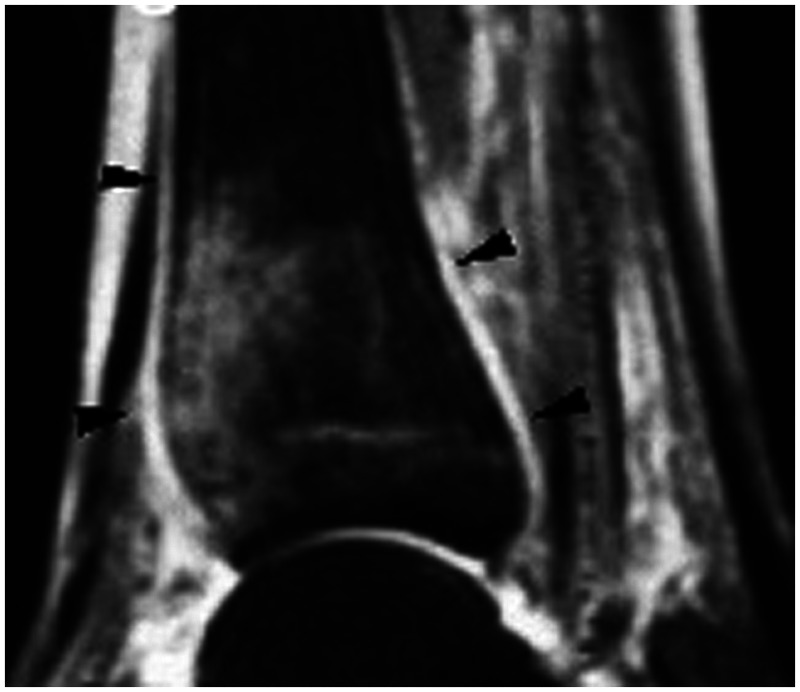
Sagittal fast STIR image of a 19-year-old female volleyball player with right tibial pain for 9 days. Arrows show edema in the distal diaphysis due to stress lesion.
Image reprinted from Gaeta et al55 with permission from the Radiological Society of North America.
Table 1.
Radiologic grading of stress fractures.
| Grade | Radiograph | Bone Scan | Magnetic Resonance Image |
|---|---|---|---|
| 0 | Normal | Normal | Normal |
| 1 | Normal | Mild uptake in one cortex | Positive STIR image |
| Poorly defined | |||
| 2 | Normal | Moderate activity | Positive STIR and T2 images |
| Larger lesion confined to one cortex | |||
| Poorly defined | |||
| 3 | Discrete line (?) | Sharply marginated increased focal or fusiform activity | Positive T1 and T2 images |
| Discrete periosteal reaction (?) | No definite cortical fracture (< 50% width) | Without definite cortical fracture | |
| 4 | Fracture | More intense fracture line | Positive T1 and T2 fracture line |
| Periosteal reaction | Bicortical uptake |
Note: This table was adapted from Arendt et al4 with permission from Clin Sports Med.
Computed tomography
Computed tomography is useful in detecting stress fractures in the pelvis and sacrum, which are not well visualized by MRI (sensitivity of 42% and specificity of 100%).17,55 Additionally, computed tomography can differentiate a stress fracture from a stress reaction and can be used for preoperative planning.60 Radiation exposure with computed tomography can be significant, but the effective dose of radiation decreases substantially with distance of the imaged extremity from the torso.18
91mTechnetium-methylene diphosphonate bone scintigraphy
Bone scanning is highly sensitive (74%-84%)11,55 but nonspecific (33%)11,55 for stress fractures. False positives can occur from increased bone metabolism in tumors or infections.86 Differentiating acute stress reactions and stress fractures can be difficult.95
Ultrasonography
Ultrasonography may be useful because it is noninvasive and simple to perform (operator dependent).7,50 In a pilot case-control study of 37 patients with metatarsal pain and normal radiographs, ultrasonography had a sensitivity of 83% and specificity of 76% compared with MRI in detecting metatarsal stress fractures.7 Also, sonograms may demonstrate fluid collections, soft tissue edema, periosteal thickening, and increased vasculature.22
High-Risk Versus Low-Risk Stress Fractures
Because of their tendency for nonunion or delayed union, certain stress fractures can be high-risk, requiring prompt treatment and careful monitoring to prevent complications (Table 2).17,20 For displaced fractures or those on the tension side of the femoral neck (Figure 4), one should consider surgery.21,95
Table 2.
Stress fracture risk for delayed union.
| High-Risk20,44,52 | Low-Risk21,44,52 |
|---|---|
| Anterior tibial diaphysis | Posteromedial tibial |
| Lateral femoral neck | Metatarsals |
| Patella | Calcaneus |
| Medial malleolus | Cuboid |
| Navicular | Cuneiform |
| Fifth metatarsal base | Fibula |
| Proximal second metatarsal | Medial femoral neck |
| Sesamoids (great toe tibial) | Femoral shaft |
| Talus | Pelvis |
| Femoral head |
Figure 4.
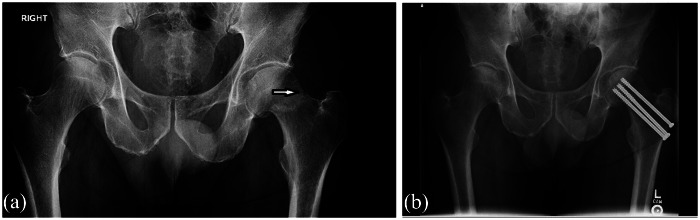
(a) Radiograph of a 51-year-old avid hiker with hip pain. Tension-side stress fracture can be seen (arrow). (b) Surgical fixation of the fracture.
Specific Stress Fractures
Tibia
The tibia accounts for 25.9% to 49.1% of all stress fractures, particularly in long-distance runners.31,62,65,87,116 These fractures may occur along the diaphysis and are typically transverse, although longitudinal fractures do occur and are at a higher risk for delayed union or nonunion.38,117 All running and high-impact activities should cease until the patient is asymptomatic with walking.52 In some low-risk fractures, when a period of relative rest does not allow the patient to return to a level of full functionality, immobilization may be required to promote healing before a gradual return to activity.44
A randomized controlled trial of pneumatic leg bracing versus traditional relative rest in athletes showed that bracing reduced the time to light activity from 21 to 7 days and to unrestricted activity from 77 to 21 days.129 In military recruits, however, pneumatic bracing had no significant benefit in time to pain-free hop test or 1-mile run.1
In the high-risk anterior tibia, radiography can reveal the “dreaded black line” (Figure 5).102 These stress fractures often take longer to heal and can result in nonunion. In one study, pneumatic bracing for 21 weeks avoided surgical intervention in delayed unions of the anterior tibia, with all patients returning to full activity at 12 months, radiographic evidence of healing in 75% of fractures.10 Tibial intramedullary nailing with a reamed intramedullary nail and locking screws (Figure 6) is an effective treatment.31,35,69 Radiographic union of the fracture can be expected at 3 months postoperatively, with return to competition at 4 months.132
Figure 5.
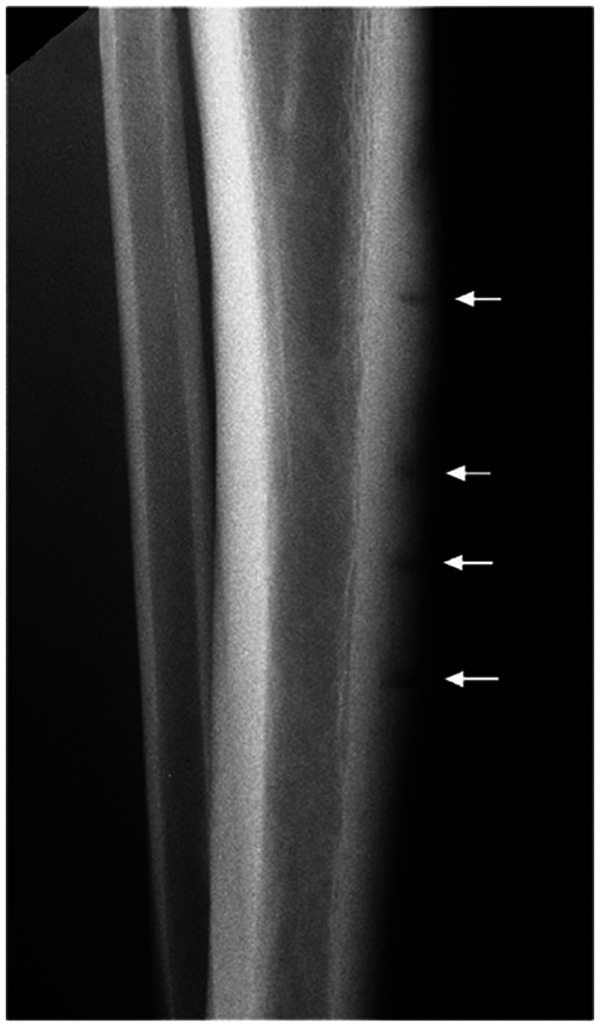
Lateral radiograph of a 21-year-old male football player with intermittent worsening bilateral anterior shin pain. Black lines indicate stress fractures of the anterior tibial cortex.
Image reprinted from Fredericson et al52 with permission from Lippincott, Williams, and Wilkins, Inc.
Figure 6.
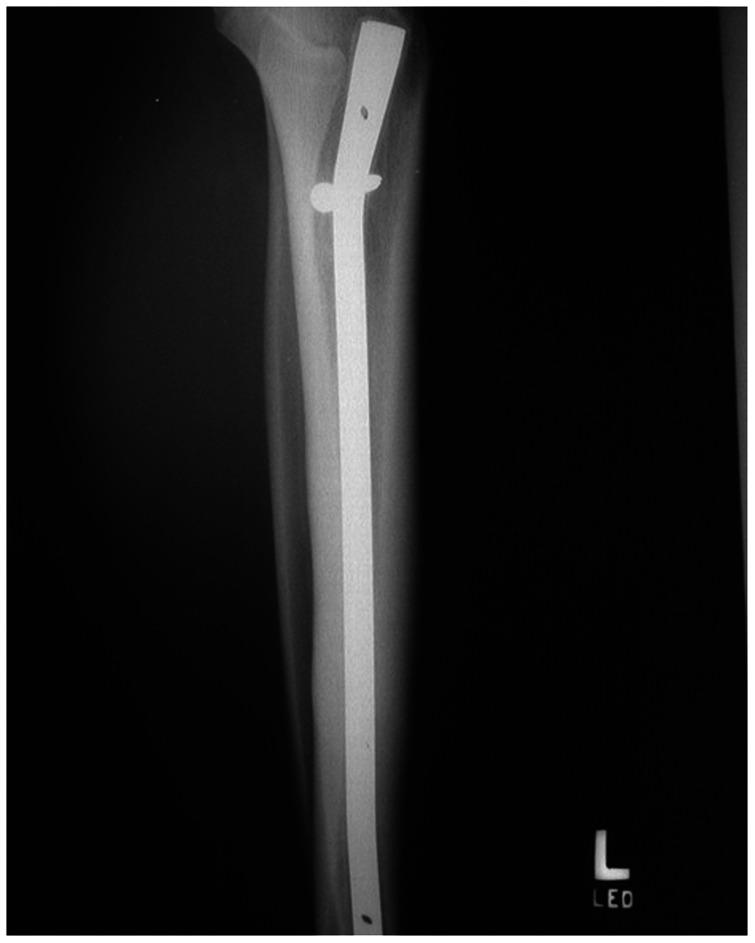
Lateral radiograph of a tibial intramedullary nail in a 20-year-old patient with a chronic anterior tibial stress fracture.
Image reprinted from Varner et al132 with permission from SAGE Publications.
Medial malleolus stress fractures are rare in young athletes but are seen in the elderly.17,61 These fractures are well managed with nonsurgical treatment: modified rest and cessation of running and jumping for 3 to 8 weeks.52 Delayed union or nonunion following conservative treatment may require operative initiative.110 Oblique drilling of the medial malleolus may promote fracture healing, with a recovery time of 5 months.103
Fibula
Fibular stress fractures account for 5.1% to 9.3% of all stress fractures.65,87,116 Most commonly occurring in the distal third,19,130 they are frequently seen in runners training on hard surfaces.43 They may be caused by muscle traction and torsional forces, as opposed to weightbearing compression.36 These fractures are low-risk, and can be managed with cessation of activity until point tenderness resolves.52
Femur
Stress fractures of the femur occur most often in the femoral neck and represent 1.0% to 7.2% of all stress fracture injuries.65,87,116 They are relatively rare, associated with coxa vara (decrease in femoral neck-shaft angle),34 and range from low- to high-risk.120 High-risk fractures result from tension on the lateral aspect of the femoral neck. They are inherently unstable and prone to displacement (Figure 7).54 Nondisplaced fractures can be treated with strict adherence to nonweightbearing movements until callus is seen radiographically.6,28 However, percutaneous screw fixation with 6.5- to 7.3-mm cannulated screws is often used in these high-risk fractures.21,95
Figure 7.
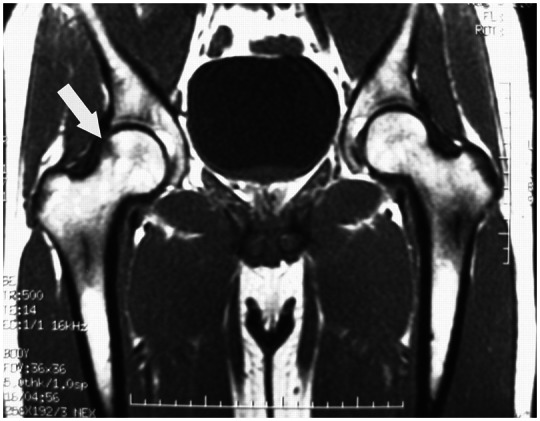
Coronal T1 image demonstrating a right tension-sided femoral neck stress fracture in a 27-year-old military recruit. Image reprinted from Provencher et al107 with permission from SAGE Publications.
Medial femoral neck fractures result from compressive forces and are low-risk (Figure 8).54 If a fracture line is not visible on radiography, it may be safely treated with a nonweightbearing regimen.42 Swimming or cycling can be permitted.69
Figure 8.
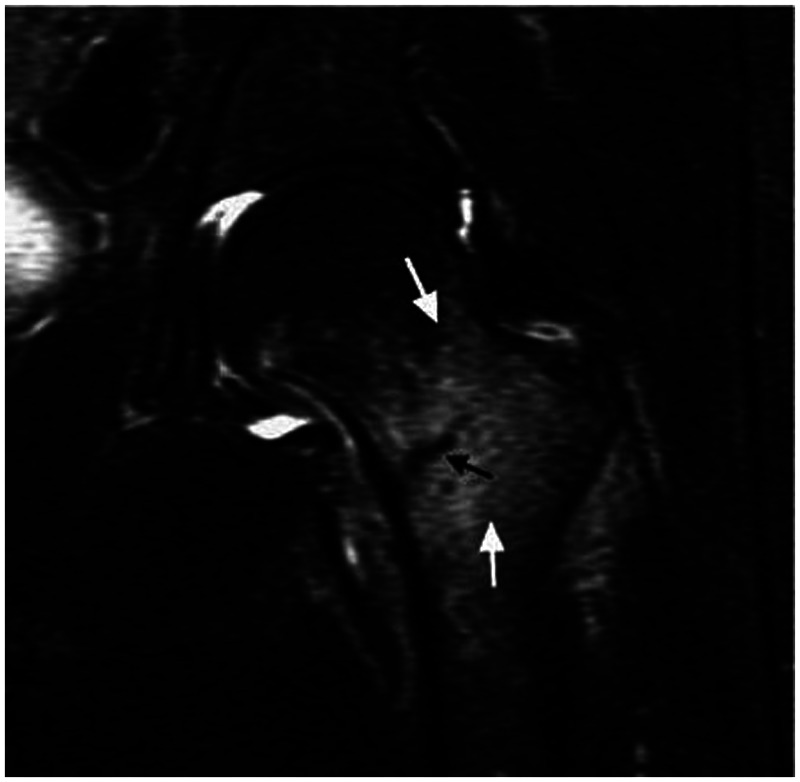
Medial femoral neck fracture on coronal T1 image of a 20-year-old female basketball player. White arrows indicate marrow edema and black arrow points to the fracture line.
Image reprinted from Fredericson et al52 with permission from Lippincott, Williams, and Wilkins, Inc.
Insufficiency or fatigue stress fractures in the femoral head are high-risk in otherwise healthy patients.72 If not recognized early, delayed union, nonunion, displacement, or avascular necrosis may ensue.17 Suspicion should arise with exercise-induced pain in the groin, hip, or proximal thigh that is relieved by rest.
Nondisplaced stress fractures of the femoral shaft can sometimes be managed with limited weightbearing28,51 (Figure 9). Surgical intervention should be considered with displaced, delayed union, and nonunited fractures.51
Figure 9.
Sagittal STIR image of a femoral shaft stress fracture (arrow) in a 21-year-old college basketball player.
Patella
Patellar stress fractures (Figure 10) are rare, representing 0.9% of all stress fractures,65,87 and are high-risk if left untreated.18 For transverse patella fractures, immobilization may be successful.85 Open reduction and internal fixation with tension band wiring and adjunctive iliotibial band release may be a better option for quicker return to activity, with reported recovery of 6 to 12 weeks.70,85 Nondisplaced longitudinal fractures can be treated conservatively with bracing.64
Figure 10.

Lateral radiograph of a 20-year-old basketball player with a transverse stress fracture of the inferior third if the patella. Image reprinted from Keeley et al70 with permission from BioMed Central.
Pelvis
Pelvic stress fractures are rare (1.6% to 7.1% of all stress fractures)65,87,116 (Figure 11). They may be difficult to detect.52 Pubic rami fractures are more common in women, with pain in the inguinal, perineal, or adductor region.91
Figure 11.

Pelvic stress fracture (arrow) in a 40-year-old distance runner.
Adjunctive Treatment
An athlete recovering from any stress fracture must comply with a gradual return to activity to allow for bone healing and remodeling.42,69 An athlete who rushes return to play risks further injury, possibly more serious than the initial insult.58 Animal studies of nonsteroidal anti-inflammatory treatment show delayed stress fracture healing, likely due to prostaglandin synthesis disruption.2,80 However, a meta-analysis did not find a significant risk of nonunion with nonsteroidal anti-inflammatory exposure.46
The use of bisphosphonates is not supported by randomized clinical trials.89,127 However, a case study of 5 collegiate female runners with stress fractures on bone scan showed recovery within 1 week of treatment with intravenous pamidronate.127 Bisphosphonates have not been shown to be effective prophylaxis in young military recruits at risk.89 Concerns exist regarding bisphosphonate use in women of childbearing age. Animal studies show that these drugs may cross the placenta and disrupt fetal osseous development.59,104 However, a review of 51 cases45 and a prospective cohort study79 of pregnancy or prepregnancy exposure to bisphosphonates did not demonstrate a relationship with congenital abnormalities. A recent review highlighted the emergence of atypical subtrochanteric stress fractures of the femur57 from oversuppression of bone turnover, a finding only observed to date in elderly patients.97 Side effects of bisphosphonates depend on the route of administration, and may include nephrotoxicity and osteonecrosis of the jaw.23,136
Bone stimulation
Both low-intensity pulsed ultrasound and electrical stimulation may increase the rate of bone healing in acute fractures.37,115 However, the efficacy of stimulation for stress fractures is unknown.109 In a prospective, randomized, double-blinded study, 26 patients were treated daily with either pulsed ultrasound or placebo until asymptomatic, and ultrasound did not significantly reduce the healing time of tibial stress fractures.113
Low-intensity ultrasound promoted an early return to athletic competition in an uncontrolled study of 8 patients with tibial stress fractures (7 posteromedial and 1 anterior).25 Patients continued competitive sports during treatment.
Electric field stimulation may hasten recovery in acute tibial stress fractures.12 A randomized control trial of 44 patients with posteromedial stress fractures did not demonstrate an overall benefit from the treatment.12 However, fractures graded more severe based on radiologic criteria4 healed quicker when treated with electric field stimulation, suggesting that the device may be helpful in these severe injuries.12
In 5 chronic stress fractures, extracorporeal shock wave therapy showed bony union at a mean of 3 months, and return to athletics between 3 and 6 months.131 A recent retrospective study of male soccer players with fifth metatarsal and tibial fractures treated with 3 sessions of extracorporeal shock wave therapy every 47 hours reported fracture healing in 6 to 14 weeks, and return to competition between 3 and 10 months posttreatment.96
Conclusions
To prevent stress fractures, athletes should progress activity levels gradually (no more than a 10% increase in load per week) to strengthen leg muscles, avoiding sudden increases in activity and running mileage.6,7,9,13,15,16,30,56,128 Training surface,66,82,90 footwear, and the female athlete triad may predispose some to stress fractures.3,14,47,48,58,108,111,112,125,134 MRI provides the highest sensitivity and specificity, making it the test of choice for diagnosing these injuries.52,74,124 High-risk stress fractures include the femoral neck, patella, anterior tibial diaphysis, and the medial malleolus.17 The role of bisphosphonates89,127 and bone stimulation12,96,131 remain unclear.
References
- 1. Allen CS, Flynn TW, Kardouni JR, et al. The use of a pneumatic leg brace in soldiers with tibial stress fractures: a randomized clinical trial. Mil Med. 2004;169(11):880-884 [DOI] [PubMed] [Google Scholar]
- 2. Allen HL, Wase A, Bear WT. Indomethacin and aspirin: effect of nonsteroidal anti-inflammatory agents on the rate of fracture repair in the rat. Acta Orthop Scand. 1980;51(4):595-600 [DOI] [PubMed] [Google Scholar]
- 3. Andrish JT, Bergfeld JA, Walheim J. A prospective study on the management of shin splints. J Bone Joint Surg Am. 1974;56(8):1697-1700 [PubMed] [Google Scholar]
- 4. Arendt EA, Griffiths HJ. The use of MR imaging in the assessment and clinical management of stress reactions of bone in high-performance athletes. Clin Sports Med. 1997;16(2):291-306 [DOI] [PubMed] [Google Scholar]
- 5. Arndt A, Westblad P, Ekenman I, Lundberg A. A comparison of external plantar loading and in vivo local metatarsal deformation wearing two different military boots. Gait Posture. 2003;18(2):20-26 [DOI] [PubMed] [Google Scholar]
- 6. Aro H, Dahlstrom S. Conservative management of distraction-type stress fractures of the femoral neck. J Bone Joint Surg Br. 1986;68(1): 65-67 [DOI] [PubMed] [Google Scholar]
- 7. Banal F, Gandjbakhch F, Foltz V, et al. Sensitivity and specificity of ultrasonography in early diagnosis of metatarsal bone stress fractures: a pilot study of 37 patients. J Rheumatol. 2009;36(8):1715-1719 [DOI] [PubMed] [Google Scholar]
- 8. Barash IA, Cheung CC, Weigle DS, et al. Leptin is a metabolic signal to the reproductive system. Endocrinology. 1996;137(7):3144-3147 [DOI] [PubMed] [Google Scholar]
- 9. Barrow GW, Saha S. Menstrual irregularity and stress fractures in collegiate female distance runners. Am J Sports Med. 1988;16(3):209-216 [DOI] [PubMed] [Google Scholar]
- 10. Batt ME, Kemp S, Kerslake R. Delayed union stress fractures of the anterior tibia: conservative management. Br J Sports Med. 2001;35(1):74-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Batt ME, Ugalde V, Anderson MW, Shelton DK. A prospective controlled study of diagnostic imaging for acute shin splints. Med Sci Sports Exerc. 1998;30(11):1564-1571 [DOI] [PubMed] [Google Scholar]
- 12. Beck BR, Matheson GO, Bergman G, et al. Do capacitively coupled electric fields accelerate tibial stress fracture healing? A randomized controlled trial. Am J Sports Med. 2008;36(3):545-553 [DOI] [PubMed] [Google Scholar]
- 13. Beck TJ, Ruff CB, Mourtada FA, et al. Dual-energy X-ray absorptiometry derived structural geometry for stress fracture prediction in male US Marine Corps recruits. J Bone Miner Res. 1996;11(5):645-653 [DOI] [PubMed] [Google Scholar]
- 14. Beck TJ, Ruff CB, Shaffer RA, Betsinger K, Trone DW, Brodine SK. Stress fracture in military recruits: gender differences in muscle and bone susceptibility factors. Bone. 2000;27(3):437-444 [DOI] [PubMed] [Google Scholar]
- 15. Bennell K, Matheson G, Meeuwisse W, Brukner P. Risk factors for stress fractures. Sports Med. 1999;28(2):91-122 [DOI] [PubMed] [Google Scholar]
- 16. Bennell KL, Malcolm SA, Thomas SA, et al. Risk factors for stress fractures in track and field athletes: a twelve-month prospective study. Am J Sports Med. 1996;24(6):810-818 [DOI] [PubMed] [Google Scholar]
- 17. Berger FH, de Jonge MC, Maas M. Stress fractures in the lower extremity: the importance of increasing awareness amongst radiologists. Eur J Radiol. 2007;62(1):16-26 [DOI] [PubMed] [Google Scholar]
- 18. Biswas D, Bible JE, Bohan M, Simpson AK, Whang PG, Grauer JN. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am. 2009;91(8):1882-1889 [DOI] [PubMed] [Google Scholar]
- 19. Blair WF, Hanley SR. Stress fracture of the proximal fibula. Am J Sports Med. 1980;8(3):212-213 [DOI] [PubMed] [Google Scholar]
- 20. Boden BP, Osbahr DC. High-risk stress fractures: evaluation and treatment. J Am Acad Orthop Surg. 2000;8(6):344-353 [DOI] [PubMed] [Google Scholar]
- 21. Boden BP, Osbahr DC, Jimenez C. Low-risk stress fractures. Am J Sports Med. 2001;29(1):100-111 [DOI] [PubMed] [Google Scholar]
- 22. Bodner G, Stockl B, Fierlinger A, Schocke M, Bernathova M. Sonographic findings in stress fractures of the lower limb: preliminary findings. Eur Radiol. 2005;15(2):356-359 [DOI] [PubMed] [Google Scholar]
- 23. Body JJ. Bisphosphonates in metastatic bone disease: renal safety matters. Oncologist. 2005;10(suppl 1):1-2 [DOI] [PubMed] [Google Scholar]
- 24. Bono CM. Low-back pain in athletes. J Bone Joint Surg Am. 2004;86(2): 382-396 [DOI] [PubMed] [Google Scholar]
- 25. Brand JC, Brindle T, Nyland J, Caborn DN, Johnson DL. Does pulsed low intensity ultrasound allow early return to normal activities when treating stress fractures? A review of one tarsal navicular and eight tibial stress fractures. Iowa Orthop J. 1999;19:26-30 [PMC free article] [PubMed] [Google Scholar]
- 26. Breithaupt MB. Zur Pathologie des Menschlichen Fusses. Med Z. 1855;4:169-177 [Google Scholar]
- 27. Brockwell J, Yeung Y, Griffith JF. Stress fractures of the foot and ankle. Sports Med Arthrosc. 2009;17(3):149-159 [DOI] [PubMed] [Google Scholar]
- 28. Brukner P. Stress fractures in runners. J Back Musculoskel Rehabil. 1995(5):341-351 [DOI] [PubMed] [Google Scholar]
- 29. Brukner P, Bennell K, Gordon M. Stress Fractures. Malden, MA: Blackwell Science; 1999 [Google Scholar]
- 30. Brukner P, Bradshaw C, Khan KM, White S, Crossley K. Stress fractures: a review of 180 cases. Clin J Sport Med. 1996;6(2):85-89 [PubMed] [Google Scholar]
- 31. Brukner P, Fanton G, Bergman AG, Beaulieu C, Matheson GO. Bilateral stress fractures of the anterior part of the tibial cortex: a case report. J Bone Joint Surg Am. 2000;82(2):213-218 [DOI] [PubMed] [Google Scholar]
- 32. Brunet ME, Cook SD, Brinker MR, Dickinson JA. A survey of running injuries in 1505 competitive and recreational runners. J Sports Med Phys Fitness. 1990;30(3):307-315 [PubMed] [Google Scholar]
- 33. Burge MR, Lanzi RA, Skarda ST, Eaton RP. Idiopathic hypogonadotropic hypogonadism in a male runner is reversed by clomiphene citrate. Fertil Steril. 1997;67(4):783-785 [DOI] [PubMed] [Google Scholar]
- 34. Carpintero P, Leon F, Zafra M, Serrano-Trenas JA, Roman M. Stress fractures of the femoral neck and coxa vara. Arch Orthop Trauma Surg. 2003;123(6):273-277 [DOI] [PubMed] [Google Scholar]
- 35. Chang PS, Harris RM. Intramedullary nailing for chronic tibial stress fractures: a review of five cases. Am J Sports Med. 1996;24(5):688-692 [DOI] [PubMed] [Google Scholar]
- 36. Choi L. Overuse injuries. In: DeLee JC, Drez D, Miller MD, eds. DeLee and Drez’s Orthopaedic Sports Medicine: Principles and Practice. 3rd ed. Philadephia, PA: Saunders; 2010 [Google Scholar]
- 37. Ciombor DM, Aaron RK. The role of electrical stimulation in bone repair. Foot Ankle Clin. 2005;10(4):579-593 [DOI] [PubMed] [Google Scholar]
- 38. Clayer M, Krishnan J, Lee WK, Tamblyn P. Longitudinal stress fracture of the tibia: two cases. Clin Radiol. 1992;46(6):401-404 [DOI] [PubMed] [Google Scholar]
- 39. Clement DB, Ammann W, Taunton JE, et al. Exercise-induced stress injuries to the femur. Int J Sports Med. 1993;14(6):347-352 [DOI] [PubMed] [Google Scholar]
- 40. Crossley K, Bennell KL, Wrigley T, Oakes BW. Ground reaction forces, bone characteristics, and tibial stress fracture in male runners. Med Sci Sports Exerc. 1999;31(8):1088-1093 [DOI] [PubMed] [Google Scholar]
- 41. Crowell HP, Davis IS. Gait retraining to reduce lower extremity loading in runners. Clin Biomech (Bristol, Avon). 2011;26(1):78-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. DeFranco MJ, Recht M, Schils J, Parker RD. Stress fractures of the femur in athletes. Clin Sports Med. 2006;25(1):89-103 [DOI] [PubMed] [Google Scholar]
- 43. Devas MB. Stress fractures of the fibula: a review of fifty cases in athletes. J Bone Joint Surg Br. 1956;38:818-829 [DOI] [PubMed] [Google Scholar]
- 44. Diehl JJ, Best TM, Kaeding CC. Classification and return-to-play considerations for stress fractures. Clin Sports Med. 2006;25(1):17-28 [DOI] [PubMed] [Google Scholar]
- 45. Djokanovic N, Klieger-Grossmann C, Koren G. Does treatment with bisphosphonates endanger the human pregnancy? J Obstet Gynaecol Can. 2008;30(12):1146-1148 [DOI] [PubMed] [Google Scholar]
- 46. Dodwell ER, Latorre JG, Parisini E, et al. NSAID exposure and risk of nonunion: a meta-analysis of case-control and cohort studies. Calcif Tissue Int. 2010;87(3):193-202 [DOI] [PubMed] [Google Scholar]
- 47. Egol KA, Koval KJ, Kummer F, Frankel VH. Stress fractures of the femoral neck. Clin Orthop Relat Res. 1998;348:72-78 [PubMed] [Google Scholar]
- 48. Ekstrand J, Torstveit MK. Stress fractures in elite male football players. Scand J Med Sci Sports. 2012;22(3):341-346 [DOI] [PubMed] [Google Scholar]
- 49. Feingold D, Hame SL. Female athlete triad and stress fractures. Orthop Clin North Am. 2006;37(4):575-583 [DOI] [PubMed] [Google Scholar]
- 50. Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners: correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23(4):472-481 [DOI] [PubMed] [Google Scholar]
- 51. Fredericson M, Jang K, Bergman G, Gold G. Femoral diaphyseal stress fractures: results of a systematic bone scan and magnetic resonance imaging evaluation in 25 runners. Phys Ther Sport. 2004;5(4):188-193 [Google Scholar]
- 52. Fredericson M, Jennings F, Beaulieu C, Matheson GO. Stress fractures in athletes. Top Magn Reson Imaging. 2006;17(5):309-325 [DOI] [PubMed] [Google Scholar]
- 53. Friberg O. Leg length asymmetry in stress fractures: clinical and radiological study. J Sports Med Phys Fitness. 1982;22(4):485-488 [PubMed] [Google Scholar]
- 54. Fullerton LR, Snowdy HA. Femoral neck stress fractures. Am J Sports Med. 1988;16(4):365-377 [DOI] [PubMed] [Google Scholar]
- 55. Gaeta M, Minutoli F, Scribano E, et al. CT and MR imaging findings in athletes with early tibial stress injuries: comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology. 2005;235(2):553-561 [DOI] [PubMed] [Google Scholar]
- 56. Gardner LI, Dziados JE, Jones BH, et al. Prevention of lower extremity stress fractures: a controlled trial of a shock absorbent insole. Am J Public Health. 1988;78(12):1563-1567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Goh SK, Yang KY, Koh JS, et al. Subtrochanteric insufficiency fractures in patients on alendronate therapy: a caution. J Bone Joint Surg Br. 2007;89(3):349-353 [DOI] [PubMed] [Google Scholar]
- 58. Goldberg B, Pecora C. Stress fractures: a risk of increased training in freshman. Phys Sports Med. 1994;22:68-78 [DOI] [PubMed] [Google Scholar]
- 59. Graepel P, Bentley P, Fritz H, Miyamoto M, Slater SR. Reproduction toxicity studies with pamidronate. Arzneimittelforschung. 1992;42(5):654-667 [PubMed] [Google Scholar]
- 60. Groves AM, Cheow HK, Balan KK, Housden BA, Bearcroft PW, Dixon AK. 16-Detector multislice CT in the detection of stress fractures: a comparison with skeletal scintigraphy. Clin Radiol. 2005;60(10):1100-1105 [DOI] [PubMed] [Google Scholar]
- 61. Harrast MA, Colonno D. Stress fractures in runners. Clin Sports Med. 2010;29(3):399-416 [DOI] [PubMed] [Google Scholar]
- 62. Heaslet MW, Kanda-Mehtani SL. Return-to-activity levels in 96 athletes with stress fractures of the foot, ankle, and leg: a retrospective analysis. J Am Podiatr Med Assoc. 2007;97(1):81-84 [DOI] [PubMed] [Google Scholar]
- 63. Henningsen A, Hinz P, Ludde R, Ekkernkamp A, Rosenbaum D. [Retrospective analysis of march fractures in the german armed forces in the years 1998 to 2000]. Z Orthop Ihre Grenzgeb. 2006;144(5):502-506 [DOI] [PubMed] [Google Scholar]
- 64. Hershman EB, Mailly T. Stress fractures. Clin Sports Med. 1990;9(1):183-214 [PubMed] [Google Scholar]
- 65. Iwamoto J, Takeda T. Stress fractures in athletes: review of 196 cases. J Orthop Sci. 2003;8(3):273-278 [DOI] [PubMed] [Google Scholar]
- 66. Johanson MA. Contributing factors in microtrauma injuries of the lower extremity. J Back Musculoskelet Rehabil. 1992;2:12-25 [DOI] [PubMed] [Google Scholar]
- 67. Johnson AW, Weiss CB, Wheeler DL. Stress fractures of the femoral shaft in athletes: more common than expected. A new clinical test. Am J Sports Med. 1994;22(2):248-256 [DOI] [PubMed] [Google Scholar]
- 68. Kaeding CC, Najarian RG. Stress fractures: classification and management. Phys Sportsmed. 2010;38(3):45-54 [DOI] [PubMed] [Google Scholar]
- 69. Kaeding CC, Yu JR, Wright R, Amendola A, Spindler KP. Management and return to play of stress fractures. Clin J Sport Med. 2005;15(6):442-447 [DOI] [PubMed] [Google Scholar]
- 70. Keeley A, Bloomfield P, Cairns P, Molnar R. Iliotibial band release as an adjunct to the surgical management of patellar stress fracture in the athlete: a case report and review of the literature. Sports Med Arthrosc Rehabil Ther Technol. 2009;1(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Kerstetter JE, O’Brien KO, Insogna KL. Low protein intake: the impact on calcium and bone homeostasis in humans. J Nutr. 2003;133(3):855S-861S [DOI] [PubMed] [Google Scholar]
- 72. Kim JW, Yoo JJ, Min BW, Hong SH, Kim HJ. Subchondral fracture of the femoral head in healthy adults. Clin Orthop Relat Res. 2007;464:196-204 [DOI] [PubMed] [Google Scholar]
- 73. Kiuru MJ, Niva M, Reponen A, Pihlajamaki HK. Bone stress injuries in asymptomatic elite recruits: a clinical and magnetic resonance imaging study. Am J Sports Med. 2005;33(2):272-276 [DOI] [PubMed] [Google Scholar]
- 74. Kiuru MJ, Pihlajamaki HK, Hietanen HJ, Ahovuo JA. MR imaging, bone scintigraphy, and radiography in bone stress injuries of the pelvis and the lower extremity. Acta Radiol. 2002;43(2):207-212 [DOI] [PubMed] [Google Scholar]
- 75. Korpelainen R, Orava S, Karpakka J, Siira P, Hulkko A. Risk factors for recurrent stress fractures in athletes. Am J Sports Med. 2001;29(3):304-310 [DOI] [PubMed] [Google Scholar]
- 76. Lappe J, Cullen D, Haynatzki G, Recker R, Ahlf R, Thompson K. Calcium and vitamin D supplementation decreases incidence of stress fractures in female navy recruits. J Bone Miner Res. 2008;23(5):741-749 [DOI] [PubMed] [Google Scholar]
- 77. Lappe JM, Stegman MR, Recker RR. The impact of lifestyle factors on stress fractures in female Army recruits. Osteoporos Int. 2001;12(1):35-42 [DOI] [PubMed] [Google Scholar]
- 78. Lee JK, Yao L. Stress fractures: MR imaging. Radiology. 1988;169(1):217-220 [DOI] [PubMed] [Google Scholar]
- 79. Levy S, Fayez I, Taguchi N, et al. Pregnancy outcome following in utero exposure to bisphosphonates. Bone. 2009;44(3):428-430 [DOI] [PubMed] [Google Scholar]
- 80. Li J, Waugh LJ, Hui SL, Burr DB, Warden SJ. Low-intensity pulsed ultrasound and nonsteroidal anti-inflammatory drugs have opposing effects during stress fracture repair. J Orthop Res. 2007;25(12):1559-1567 [DOI] [PubMed] [Google Scholar]
- 81. Loucks AB. Energy availability, not body fatness, regulates reproductive function in women. Exerc Sport Sci Rev. 2003;31(3):144-148 [DOI] [PubMed] [Google Scholar]
- 82. Macera CA, Pate RR, Powell KE, Jackson KL, Kendrick JS, Craven TE. Predicting lower-extremity injuries among habitual runners. Arch Intern Med. 1989;149(11):2565-2568 [PubMed] [Google Scholar]
- 83. Maitra RS, Johnson DL. Stress fractures: clinical history and physical examination. Clin Sports Med. 1997;16(2):259-274 [DOI] [PubMed] [Google Scholar]
- 84. Massey LK. Caffeine and the elderly. Drugs Aging. 1998;13(1):43-50 [DOI] [PubMed] [Google Scholar]
- 85. Mata SG, Grande MM, Ovejero AH. Transverse stress fracture of the patella: a case report. Clin J Sport Med. 1996;6(4):259-261 [DOI] [PubMed] [Google Scholar]
- 86. Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, Macintyre JG. Scintigraphic uptake of 99mTc at non-painful sites in athletes with stress fractures: the concept of bone strain. Sports Med. 1987;4(1):65-75 [DOI] [PubMed] [Google Scholar]
- 87. Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Stress fractures in athletes: a study of 320 cases. Am J Sports Med. 1987;15(1):46-58 [DOI] [PubMed] [Google Scholar]
- 88. Messier SP, Pittala KA. Etiologic factors associated with selected running injuries. Med Sci Sports Exerc. 1988;20(5):501-505 [PubMed] [Google Scholar]
- 89. Milgrom C, Finestone A, Novack V, et al. The effect of prophylactic treatment with risedronate on stress fracture incidence among infantry recruits. Bone. 2004;35(2):418-424 [DOI] [PubMed] [Google Scholar]
- 90. Milgrom C, Finestone A, Segev S, Olin C, Arndt T, Ekenman I. Are overground or treadmill runners more likely to sustain tibial stress fracture? Br J Sports Med. 2003;37(2):160-163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Miller C, Major N, Toth A. Pelvic stress injuries in the athlete: management and prevention. Sports Med. 2003;33(13):1003-1012 [DOI] [PubMed] [Google Scholar]
- 92. Miller MD, Marks PH, Fu FH. Bilateral stress fractures of the distal fibula in a 35-year-old woman. Foot Ankle Int. 1994;15(8):450-453 [DOI] [PubMed] [Google Scholar]
- 93. Milner CE, Hamill J, Davis I. Are knee mechanics during early stance related to tibial stress fracture in runners? Clin Biomech (Bristol, Avon). 2007;22(6):697-703 [DOI] [PubMed] [Google Scholar]
- 94. Milner CE, Hamill J, Davis IS. Distinct hip and rearfoot kinematics in female runners with a history of tibial stress fracture. J Orthop Sports Phys Ther. 2010;40(2):59-66 [DOI] [PubMed] [Google Scholar]
- 95. Monteleone GP. Stress fractures in the athlete. Orthop Clin North Am. 1995;26(3):423-432 [PubMed] [Google Scholar]
- 96. Moretti B, Notarnicola A, Garofalo R, et al. Shock waves in the treatment of stress fractures. Ultrasound Med Biol. 2009;35(6):1042-1049 [DOI] [PubMed] [Google Scholar]
- 97. Murphy CG, O’Flanagan S, Keogh P, Kenny P. Subtrochanteric stress fractures in patients on oral bisphosphonate therapy: an emerging problem. Acta Orthop Belg. 2011;77(5):632-637 [PubMed] [Google Scholar]
- 98. Myburgh KH, Hutchins J, Fataar AB, Hough SF, Noakes TD. Low bone density is an etiologic factor for stress fractures in athletes. Ann Intern Med. 1990;113(10):754-759 [DOI] [PubMed] [Google Scholar]
- 99. New SA, Robins SP, Campbell MK, et al. Dietary influences on bone mass and bone metabolism: further evidence of a positive link between fruit and vegetable consumption and bone health? Am J Clin Nutr. 2000;71(1):142-151 [DOI] [PubMed] [Google Scholar]
- 100. Nieves JW, Melsop K, Curtis M, et al. Nutritional factors that influence change in bone density and stress fracture risk among young female cross-country runners. PM R. 2010;2(8):740-750 [DOI] [PubMed] [Google Scholar]
- 101. Orava S. Stress fractures. Br J Sports Med. 1980;14(1):40-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Orava S, Hulkko A. Stress fracture of the mid-tibial shaft. Acta Orthop Scand. 1984;55(1):35-37 [DOI] [PubMed] [Google Scholar]
- 103. Orava S, Karpakka J, Taimela S, Hulkko A, Permi J, Kujala U. Stress fracture of the medial malleolus. J Bone Joint Surg Am. 1995;77(3):362-365 [DOI] [PubMed] [Google Scholar]
- 104. Patlas N, Golomb G, Yaffe P, Pinto T, Breuer E, Ornoy A. Transplacental effects of bisphosphonates on fetal skeletal ossification and mineralization in rats. Teratology. 1999;60(2):68-73 [DOI] [PubMed] [Google Scholar]
- 105. Pirker H. Bruch der Oberschenkeldiaphyse durch Muskelzug. Arch Klin Chir. 1934;175:155-168 [Google Scholar]
- 106. Pouilles JM, Bernard J, Tremollieres F, Louvet JP, Ribot C. Femoral bone density in young male adults with stress fractures. Bone. 1989;10(2):105-108 [DOI] [PubMed] [Google Scholar]
- 107. Provencher MT, Baldwin AJ, Gorman JD, Gould MT, Shin AY. Atypical tensile-sided femoral neck stress fractures: the value of magnetic resonance imaging. Am J Sports Med. 2004;32(6):1528-1534 [DOI] [PubMed] [Google Scholar]
- 108. Prynne CJ, Ginty F, Paul AA, et al. Dietary acid-base balance and intake of bone-related nutrients in Cambridge teenagers. Eur J Clin Nutr. 2004;58(11):1462-1471 [DOI] [PubMed] [Google Scholar]
- 109. Raasch WG, Hergan DJ. Treatment of stress fractures: the fundamentals. Clin Sports Med. 2006;25(1):29-36, vii [DOI] [PubMed] [Google Scholar]
- 110. Reider B, Falconiero R, Yurkofsky J. Nonunion of a medial malleolus stress fracture: a case report. Am J Sports Med. 1993;21(3):478-481 [DOI] [PubMed] [Google Scholar]
- 111. Rome K, Handoll HH, Ashford R. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst Rev. 2005;(2):CD000450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Rudzki SJ. Injuries in Australian Army recruits: part I. Decreased incidence and severity of injury seen with reduced running distance. Mil Med. 1997;162(7):472-476 [PubMed] [Google Scholar]
- 113. Rue JP, Armstrong DW 3rd, Frassica FJ, Deafenbaugh M, Wilckens JH. The effect of pulsed ultrasound in the treatment of tibial stress fractures. Orthopedics. 2004;27(11):1192-1195 [DOI] [PubMed] [Google Scholar]
- 114. Ruffing J, Cosman F, Zion M, et al. Determinants of bone mass and bone size in a large cohort of physically active young adult men. Nutr Metab (Lond). 2006;3:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Rutten S, Nolte PA, Guit GL, Bouman DE, Albers GH. Use of low-intensity pulsed ultrasound for posttraumatic nonunions of the tibia: a review of patients treated in the Netherlands. J Trauma. 2007;62(4):902-908 [DOI] [PubMed] [Google Scholar]
- 116. Sakai N. Diagnoses and treatment of stress fractures in athletes. J Jpn Soc Clin Sports Med. 1999;7:32-39 [Google Scholar]
- 117. Schraml FV, Riego De, Dios RL, Flemming DJ. Exercise-related longitudinal tibial stress fracture in a young person. Ann Nucl Med. 2006;20(6):441-444 [DOI] [PubMed] [Google Scholar]
- 118. Schwellnus MP, Jordaan G. Does calcium supplementation prevent bone stress injuries? A clinical trial. Int J Sport Nutr. 1992;2(2):165-174 [DOI] [PubMed] [Google Scholar]
- 119. Seeman E. The structural and biomechanical basis of the gain and loss of bone strength in women and men. Endocrinol Metab Clin North Am. 2003;32(1):25-38 [DOI] [PubMed] [Google Scholar]
- 120. Shin AY, Gillingham BL. Fatigue fractures of the femoral neck in athletes. J Am Acad Orthop Surg. 1997;5(6):293-302 [DOI] [PubMed] [Google Scholar]
- 121. Shin AY, Morin WD, Gorman JD, Jones SB, Lapinsky AS. The superiority of magnetic resonance imaging in differentiating the cause of hip pain in endurance athletes. Am J Sports Med. 1996;24(2):168-176 [DOI] [PubMed] [Google Scholar]
- 122. Sijbrandij ES, van Gils AP, de Lange EE. Overuse and sports-related injuries of the ankle and hind foot: MR imaging findings. Eur J Radiol. 2002;43(1):45-56 [DOI] [PubMed] [Google Scholar]
- 123. Simkin A, Leichter I, Giladi M, Stein M, Milgrom C. Combined effect of foot arch structure and an orthotic device on stress fractures. Foot Ankle. 1989;10(1):25-29 [DOI] [PubMed] [Google Scholar]
- 124. Sofka CM. Imaging of stress fractures. Clin Sports Med. 2006;25(1):53-62 [DOI] [PubMed] [Google Scholar]
- 125. Spitz DJ, Newberg AH. Imaging of stress fractures in the athlete. Radiol Clin North Am. 2002;40(2):313-331 [DOI] [PubMed] [Google Scholar]
- 126. Stechow AW. Fussoedem und Roentgenstrahlen. Dtsch Mil Aerztl. 1897;26:465-471 [Google Scholar]
- 127. Stewart GW, Brunet ME, Manning MR, Davis FA. Treatment of stress fractures in athletes with intravenous pamidronate. Clin J Sport Med. 2005;15(2):92-94 [DOI] [PubMed] [Google Scholar]
- 128. Sundgot-Borgen J, Torstveit MK. The female football player, disordered eating, menstrual function and bone health. Br J Sports Med. 2007;41(suppl 1):i68-i72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Swenson EJ, DeHaven KE, Sebastianelli WJ, Hanks G, Kalenak A, Lynch JM. The effect of a pneumatic leg brace on return to play in athletes with tibial stress fractures. Am J Sports Med. 1997;25(3):322-328 [DOI] [PubMed] [Google Scholar]
- 130. Symeonides PP. High stress fractures of the fibula. J Bone Joint Surg Br. 1980;62(2):192-193 [DOI] [PubMed] [Google Scholar]
- 131. Taki M, Iwata O, Shiono M, Kimura M, Takagishi K. Extracorporeal shock wave therapy for resistant stress fracture in athletes: a report of 5 cases. Am J Sports Med. 2007;35(7):1188-1192 [DOI] [PubMed] [Google Scholar]
- 132. Varner KE, Younas SA, Lintner DM, Marymont JV. Chronic anterior midtibial stress fractures in athletes treated with reamed intramedullary nailing. Am J Sports Med. 2005;33(7):1071-1076 [DOI] [PubMed] [Google Scholar]
- 133. Voss LA, Fadale PD, Hulstyn MJ. Exercise-induced loss of bone density in athletes. J Am Acad Orthop Surg. 1998;6(6):349-357 [DOI] [PubMed] [Google Scholar]
- 134. Walter SD, Hart LE, McIntosh JM, Sutton JR. The Ontario cohort study of running-related injuries. Arch Intern Med. 1989;149(11):2561-2564 [PubMed] [Google Scholar]
- 135. Warden SJ, Creaby MW, Bryant AL, Crossley KM. Stress fracture risk factors in female football players and their clinical implications. Br J Sports Med. 2007;41(suppl 1):i38-i43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Watts NB, Harris ST, McClung MR, Bilezikian JP, Greenspan SL, Luckey MM. Bisphosphonates and osteonecrosis of the jaw. Ann Intern Med. 2006;145(10):791-792 [DOI] [PubMed] [Google Scholar]
- 137. Young AJ, McAllister DR. Evaluation and treatment of tibial stress fractures. Clin Sports Med. 2006;25(1):117-128 [DOI] [PubMed] [Google Scholar]
- 138. Zeni AI, Street CC, Dempsey RL, Staton M. Stress injury to the bone among women athletes. Phys Med Rehabil Clin N Am. 2000;11(4):929-947 [PubMed] [Google Scholar]


