Abstract
Hearing loss is a major handicap in developing countries with paucity of trained audiologists and limited resources. In this pilot study trained community health workers were used to provide comprehensive hearing aid services in the community. One hundred and eleven patients were fitted with semi-digital hearing aid and were evaluated over a period of six months. They were assessed using self-report outcome measure APHAB. Results show that trained CHWs are effective in detecting disabling hearing loss and in providing HAs. APHAB can identify and pick up significant improvements in communication in daily activities and provides a realistic expectation of the benefits of a hearing aid. The model of using trained CHWs to provide rehabilitative services in audiology along with self-report outcome measures can be replicated in other developing countries.
1. Introduction
It is well recognized that hearing loss is the most common global disability [1]. As reported by Davis [2] (British MRC Institute of Hearing Research) the numbers with hearing impairment in developing countries is estimated to reach 500 million by the year 2015. In India, hearing loss is the third most common disability [3] and the prevalence of moderate to severe hearing loss is reported to be 6.3 percent by WHO [4]. The majority of India's population lives in rural areas with poor facilities and accesses for evaluation of hearing and treatment being seldom available. Also, due to the paucity of trained audiologists, [5] the burden of hearing handicap is magnified. The primary goal of the study was to determine the degree and nature of benefit that could be expected in the population by using trained community workers to fit semidigital hearing aids which can be programmed easily by trained workers and quantifying benefit using APHAB which was translated in to the local language.
Deafness is an expensive handicap, leading to loss of work and active participation in social activities of the community [6].
The measurement of outcomes in rehabilitative audiology has received more attention because of the need to demonstrate efficacy of treatment for consumers, carry out cost-benefit analyses. Traditionally, the outcomes of hearing aid intervention have been demonstrated using objective measures such as the functional gain [7] speech recognition [8] testing, and real ear responses [9]. An alternative to the use of objective hearing aid benefit measurements is the use of self-report methodology. In the 1980s and 1990s several other subjective measurement instruments were developed to assess hearing aid benefit [10, 11].
One of the most common subjective benefit measures in use today is the Abbreviated Profile of Hearing Aid Benefit (APHAB) developed by Cox and Alexander [12].
APHAB is a questionnaire which has 24 predetermined questions regarding various situations of hearing aid usage. It also gives the patient a realistic estimation of the use of a hearing aid. It is scored before and after fitting hearing aids (Table 3). The difference in scores with and without the use of hearing aid(s) is considered the measure of benefit. There are four categories in which benefit is calculated: ease of communication (EC), listening in background noise (BN), listening in reverberant conditions (RV), and aversiveness of sounds (AV).
Table 3.
Scores for each question.
| Unaided | Aided | Benefit | ||||
|---|---|---|---|---|---|---|
| Mean | Std. deviation | Mean | Std. deviation | Mean | Std. deviation | |
| BN 1 | 89.39 | 14.786 | 20.85 | 19.128 | 67.83 | 22.814 |
| BN 6 | 84.57 | 20.355 | 15.03 | 17.070 | 69.43 | 29.853 |
| BN 7 | 83.17 | 23.400 | 12.86 | 19.386 | 70.31 | 32.893 |
| BN 16 | 90.07 | 16.572 | 27.18 | 24.825 | 61.41 | 27.376 |
| BN 19 | 93.25 | 11.208 | 17.42 | 16.498 | 74.48 | 19.199 |
| BN 24 | 73.23 | 35.959 | 19.27 | 23.300 | 53.72 | 44.147 |
|
| ||||||
| EC 4 | 81.94 | 18.703 | 16.84 | 24.216 | 65.10 | 34.362 |
| EC 10 | 74.53 | 32.162 | 11.28 | 20.874 | 66.14 | 38.632 |
| EC 12 | 77.95 | 27.126 | 10.54 | 16.133 | 68.05 | 28.147 |
| EC 14 | 82.01 | 25.096 | 21.32 | 23.844 | 59.28 | 32.167 |
| EC 15 | 72.39 | 32.067 | 18.99 | 27.937 | 51.55 | 49.414 |
| EC 23 | 79.09 | 24.532 | 12.50 | 16.149 | 66.63 | 28.935 |
|
| ||||||
| RV 2 | 82.32 | 29.281 | 27.25 | 23.335 | 56.02 | 40.909 |
| RV 5 | 83.96 | 21.608 | 15.60 | 18.732 | 67.64 | 32.068 |
| RV 9 | 88.99 | 16.719 | 15.09 | 14.781 | 73.63 | 21.607 |
| RV 11 | 93.59 | 11.424 | 17.79 | 19.929 | 72.61 | 26.129 |
| RV 18 | 70.84 | 35.135 | 26.79 | 31.958 | 42.17 | 61.785 |
| RV 21 | 89.36 | 17.287 | 23.44 | 21.319 | 64.88 | 28.673 |
|
| ||||||
| AV 3 | 15.89 | 31.728 | 26.80 | 31.202 | −11.64 | 45.396 |
| AV 8 | 22.76 | 35.284 | 28.50 | 32.159 | −5.79 | 46.441 |
| AV 13 | 18.06 | 23.689 | 23.59 | 36.102 | −4.38 | 35.431 |
| AV 17 | 15.85 | 29.795 | 34.36 | 34.442 | −17.82 | 49.513 |
| AV 20 | 9.65 | 22.504 | 32.22 | 34.550 | −27.09 | 36.752 |
| AV 22 | 5.73 | 15.528 | 27.78 | 31.694 | −22.46 | 31.084 |
In a large developing country like India with significant rural population, the use of community health workers to identify hearing loss and provide hearing aids and associated services and evaluate the use and satisfaction of HAs by self-report measure APHAB and its stability was studied over a period of six months.
2. Methodology
2.1. Selecting the Health Workers
Community Hearing Workers (CHWs) were selected with educational qualification of graduate with preference for science subjects. They were given a six week training program on basic hearing health care, which included performing Pure tone audiometry (PTA) using a portable audiometer, impression taking, and ear mould making, performing hearing aid trial and hearing aid fitting, maintenance of hearing aids, minor repairs of hearing aids, and maintenance of ear moulds. They were also taught to counsel patients regarding hearing aid usage.
They were also trained to administer APHAB, translated into the local language (Tamil) and validated by the audiologist.
2.2. Recruiting of Patients
Camps were conducted with the help of the local government organization and nongovernmental agencies (NGOs), using local propaganda machine which included television broad casting and advertising in the regional language papers. Patients were screened by an ENT specialist and hearing assessment was done in the field using ARPHI-500 MKI dual channel portable audiometers programmed to ANSI standards in a quiet room. A three frequency (0.5 kHz, 1 kHz, 2 kHz) average was taken and hearing loss was classified as moderate, moderately severe, severe, and profound hearing loss. The PTA was later counter checked by the audiologist at the base hospital.
-
Inclusion criteria: age: 14–70 years.
-
Hearing loss—bilateral moderate to severe sensorineural hearing loss (41–90 dB).
-
Exclusion criteria:
- Hearing loss which can be surgically corrected.
- Children below 14 years and adults above 70 years.
- Mild hearing (<40 dB) loss and profound (>90 dB) hearing loss.
3. APHAB
The APHAB is a hearing aid outcome measure that reflects the impact of hearing loss and benefit of hearing aid in daily communication.
The APHAB comprises 24 items that are scored in 4 subscales. The subscales are as follows.
Ease of communication (EC): the strain of communicating under relatively favorable conditions.
Reverberation (RV): communication in reverberant rooms such as class rooms.
Background noise (BN): communication in settings with high background noise levels.
Aversiveness (AV): the unpleasantness of environmental sounds.
There are 24 items; each item contributes to only one subscale and there are six items for each subscale distributed randomly with in the inventory. Each item is answered for “without my hearing aid” and “with my hearing aid” so that each subscale produces a score for unaided listening and a score for aided listening. In addition, the difference between these two scores can be obtained to give a score for benefit. The complete APHAB generates 12 scores, three for each of four subscales.
The difference in the rating between the initial and the final visit is scored as the amount of benefit in each of four general categories.
The first three subscales, EC, RV, and BN, are known as the “speech communication” subscales. These subscale benefit scores are reported in the form of a positive percentage (i.e., 10%, 20%, 30%). The fourth subscale, aversiveness (AV), quantifies an individual's negative reaction to aversive environmental sounds. This subscale is reported in a negative percentage (i.e., −10%, −20%, −30%).
Hearing aids (Siemens 213) were dispensed based on the formula
| (1) |
4. Procedure
After identifying suitable individuals, a detailed session of counseling was done and APHAB questionnaire was filled up prior to HA fitting by the CHWs. Hearing assessment was done and ear mould impression was taken for selected patients. In the second visit, a semidigital, trimmer programmable hearing aid, Siemens Phoenix 213, which is a mini-BTE, suitable for moderate to severe hearing loss, was fitted for all the patients. The HAs were programmed to NAL (National Acoustic Laboratory) prescription standards [13]. Adjusting the HA for optimal use and its maintenance was taught. APHAB followup was done for 2 weeks, one month, three months, and six months. Modern telecommunication facilities were used and mobile phone was used by the patients to communicate with the health workers and minor problems of moulds and hearing aid fitting and trimmer adjustments were done in the field. The hearing health care service was provided free of health care costs to the patients at their doorstep by the CHWs.
5. Results
This study was done to evaluate a model of using trained Community hearing workers to provide rehabilitative audiological services in the community and to asses the use of Hearing Aids and their benefit in the community by using self reported benefit questionnaire APHAB translated in to local language.
A total of 111 patients with 48 females and 63 males, having moderately severe to severe ((41–90 dB) sensori-neural hearing loss (Table 1) were rehabilitated with hearing aids from March 2009 to September 2009. All were first time users with no prior hearing aid experience. 57% were males and 72.9% were above the age of 40 years (Table 2) (Figure 1). The whole process from the identification of patients to fitting hearing aids and followup over six months was done in the community.
Table 1.
Gender versus degree of hearing loss.
| Moderately severe | Severe | Profound | ||
|---|---|---|---|---|
| Sex | ||||
| F | 16 | 30 | 2 | 48 |
| M | 20 | 42 | 1 | 63 |
|
| ||||
| Total | 36 | 72 | 3 | 111 |
Table 2.
Age versus degree of hearing loss.
| Moderately severe | Severe | Profound | ||
|---|---|---|---|---|
| Age_1 | ||||
| 14–25 | 6 | 11 | 0 | 17 |
| 26–60 | 19 | 32 | 2 | 53 |
| 61–70 | 11 | 29 | 1 | 41 |
|
| ||||
| Total | 36 | 72 | 3 | 111 |
Figure 1.
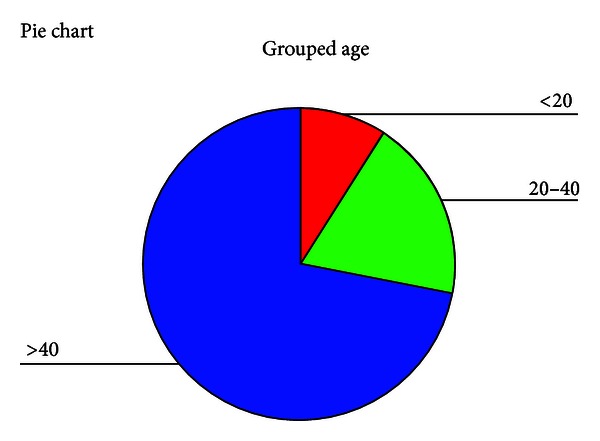
Distribution of age.
105 (94.5%) patients came for followup to six months. Six (5.4%) patients did not come for regular followup.
Of the six patients (5.4%) who failed to come for regular followup, one was later found to have auditory neuropathy. Two patients complained of excessive noise, and two did not have benefit from the HA.
88 patients (80%) were using their hearing aid regularly for more than 4 hours, whereas 20% were using it for less than 4 hours, due to their profession, which involved working as laborers, where sweating of face and dirt on hands were constraints for continuous usage.
It took approximately 25 minutes to administer APHAB.
The questionnaire when administered before HA fitting (unaided), 108 (97%) answered all the questions with respect to ease of communication (EC), background noise (BN), and aversiveness (AV). However, 14% did not respond to all the questions which assess reverberation (RV). There was no significant difference in the response pattern with respect to gender in both unaided and aided scores. It took time to administer as patients were semiliterate/illiterate in addition to being hearing challenged.
It was found that clients experienced more problems in personal communication (EC) even with little or no background noise with greatest difficulty faced when talking with family and friends. Communication in crowded places /shop (BN) experienced greatest benefit with most people being able to participate in community actively. They were able to participate in the social activities of the community (RV) and also enjoy recreational activities (movie) and also participate in religious activities (Figure 2).
Figure 2.
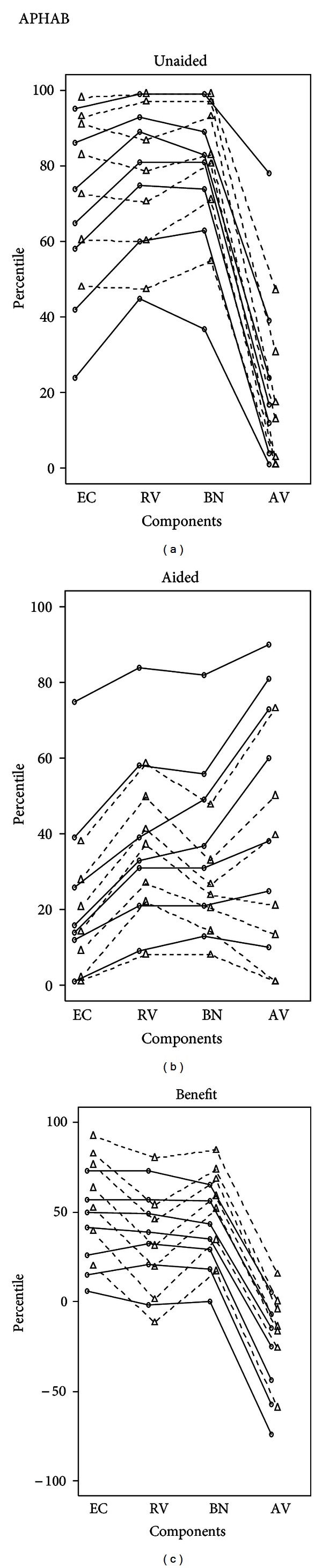
On comparing the percentiles of the present study with those of normative data [12].
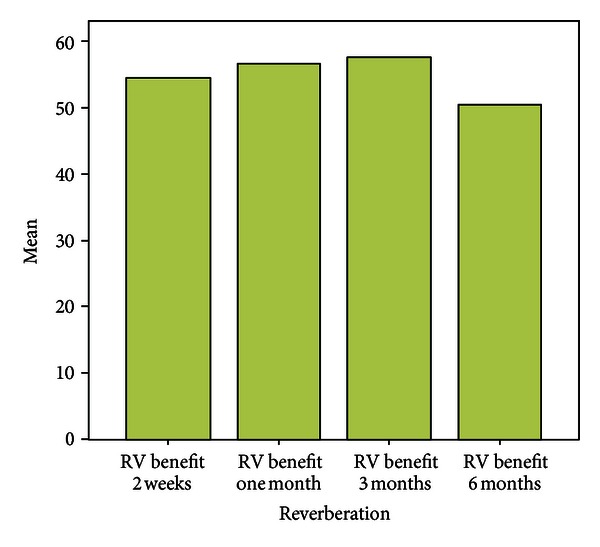
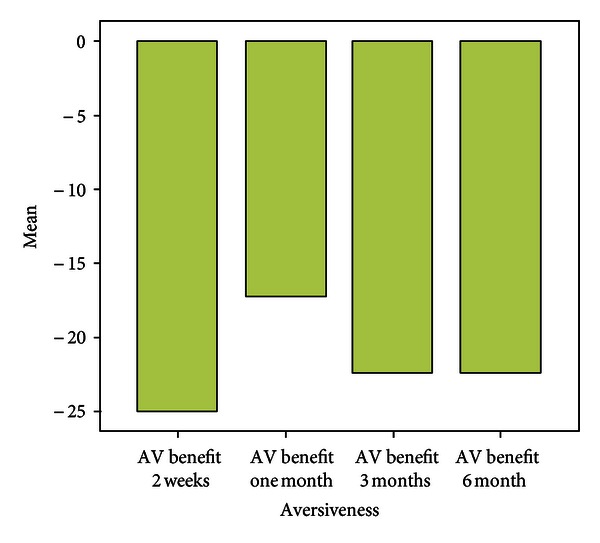
Over a period of six months the mean scores with respect to EC were almost similar to that assessed at the end of two weeks. Patients experienced fewer problems while communicating in background noise, whereas the mean scores with respect to communication in reverberant surroundings were more when compared with two weeks post fitting scores. Scores for Aversiveness increased in comparison to immediate post fitting scores.
Clients without hearing aid reported more than 35th percentile problems with respect to EC (85%), BN (79.2), RV (73%). 68.4% scored less than 50th percentile with respect to aversive sounds in the environment (AV).
Problems in the speech communication subscales (EC, BN, and RV) showed a significant decrease after using the hearing aid (Figures 3, 4, 5, and 6).
Figure 3.
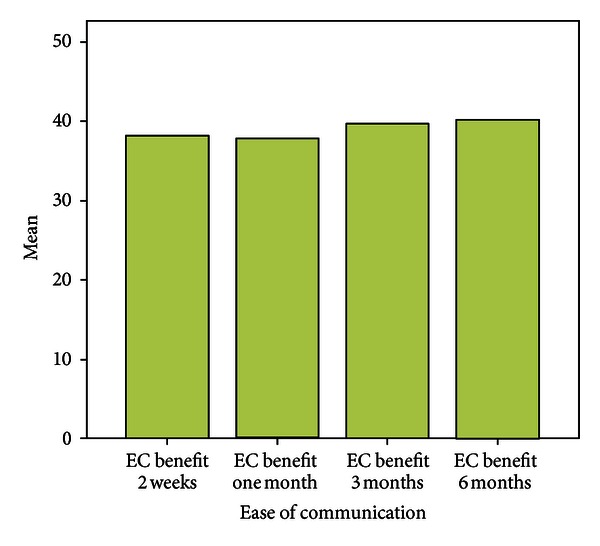
Benefit over six months.
Figure 4.
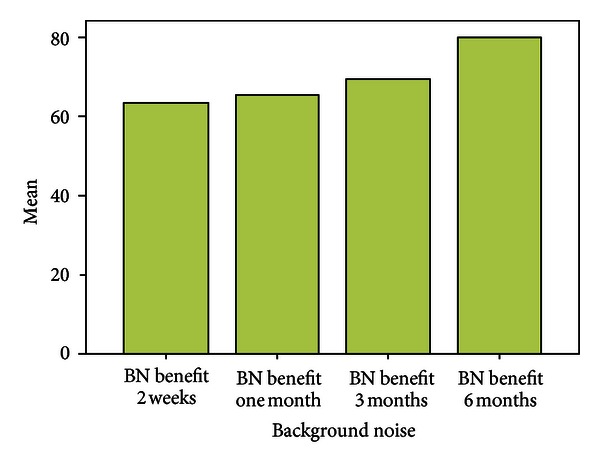
Benefit over six months.
Figure 5.
Benefit over six months.
Figure 6.
Benefit over six months.
There was significant benefit >25 in all the three speech subscales (Figure 7).
Figure 7.
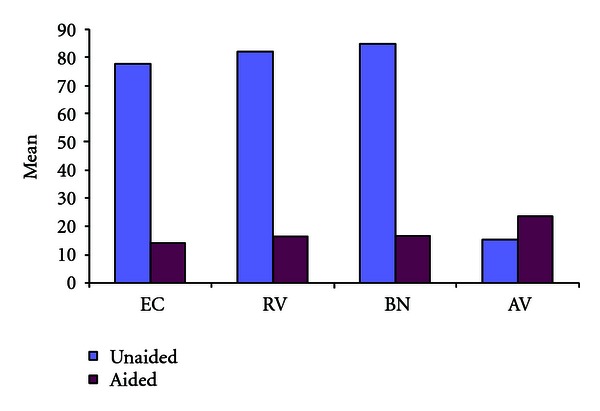
Mean scores.
6. Discussion
The main purpose of this study was using trained community workers to provide hearing aids in the community and to assess the self-report measure APHAB in the community and its stability over a period of six months.
It was found that most hearing aid users were above the age of 40, which was similar to the other studies. Hearing aids were fitted for patients with moderate to severe hearing loss which had a high acceptance level (98%).
Most of the recruited patients were from cluster of surrounding villages. Thus during followup patients were called together in the village and they could discuss the problems they faced and how to resolve them. The issues regarding usage of hearing aid and the stigma of not being able to hear were sorted out among themselves. A feeling of community helped them to overcome the shyness of using a hearing aid and thus it led to increased acceptance and the despondency of being a deaf person was overcome which led many other people with similar problem to seek help for their problem. In APHAB, in contrast to the report by Hojan et al., there was no significant difference in responses between male and female HA users [14].
There was a significant benefit in all the three communication subscales. The missing responses to BN and AV scales could be explained from the fact that the mentioned situations were not encountered immediately after hearing aid fitting and may have been due to rural living, which did not expose them to situations where background noise and aversive sounds were present.
The AV subscale score is typically higher at post-fitting. This likely reflects the increased audibility of certain environmental sounds that even individuals with normal hearing may find aversive. The small, statistically nonsignificant change in the AV scores indicates that the hearing aid provided acceptable listening comfort and sound quality for most of the participants.
There was correlation between the aided condition and PTA thresholds as reported by Cox et al. [15] which confirms that while fitting hearing aids in the community, clients with moderately severe and severe hearing loss suffer more problems which can be alleviated with provision of hearing aids suited for that range that is, the hearing aid has to be compatible or provide significant gain with respect to speech communication subscales (EC, RV, BN).
APHAB picked up significant improvements in communication especially in reverberant rooms and in settings with high background noise levels.
The limitation of this study was the lack of responses to questions, as in a rural community the provision of modern amenities is lacking when compared to an urban setting.
7. Conclusion
APHAB picked up significant improvements in communication especially in reverberant rooms and in settings with high background noise levels. Though the questionnaire is long the questions take into consideration most of the situations the patients face in their daily life. However in a rural community with lack of basic amenities some of the questions may not be assessed for a considerable time period till the patient comes into contact with such situations.
However it is the most comprehensive questionnaire and gives the patient a realistic expectation from a hearing aid. It can also be used at a later time when the patient upgrades his hearing aid and thus the benefits can be compared.
Acknowledgments
The authors wish to acknowledge Mr. Grant Preston, Dr. Andrew W Smith, Dr. Ron Brouillette, WWHearing, and CBM.
Abbreviations
- APHAB:
Abbreviated Profile of Hearing Aid Benefit
- PTA:
Pure tone audiometry
- HA:
Hearing aid
- CHW:
Community hearing worker
- MPO:
Maximum Power output
- FA:
Frequency average.
References
- 1.Disease incidence, prevalence and disability. http://www.who.int/entity/healthinfo/global, burden disease/GBD report, 2004.
- 2.Davis A. British MRC Institute of Hearing Research, http://www.hear-it.org/
- 3.Patel S. An empirical study of causes of disability in India. The Internet Journal of Epidemiology. 2009;6(2) [Google Scholar]
- 4.WHO. State of Hearing and Ear Care in the South East Asia Region. New Delhi, India: WHO; 2004. Prevention and causes of deafness and hearing impairment in the South East Asia region; pp. 9–10. [Google Scholar]
- 5.Suneela G, Shelly C, Sumit M, Agarwal AK. Deafness: Burden, prevention and control in India. National Medical Journal of India. 2009;22(2):79–81. [PubMed] [Google Scholar]
- 6.Mohr PE, Feldman JJ, Dunbar JL, et al. The societal costs of severe to profound hearing loss in the United States. International Journal of Technology Assessment in Health Care. 2000;16(4):1120–1135. doi: 10.1017/s0266462300103162. [DOI] [PubMed] [Google Scholar]
- 7.Kuk FK, Harper T, Doubek K. Preferred real-ear insertion gain on a commercial hearing aid at different speech and noise levels. Journal of the American Academy of Audiology. 1994;5(2):99–109. [PubMed] [Google Scholar]
- 8.Mason D, Popelka GR. Comparison of hearing-aid gain using functional, coupler, and probe-tube measurements. Journal of Speech and Hearing Research. 1986;29(2):218–226. doi: 10.1044/jshr.2902.218. [DOI] [PubMed] [Google Scholar]
- 9.Studebaker GA. Hearing aid selection: an overview. In: Studebaker GA, Bess FH, editors. The Vanderbilt Hearing-Aid Report. Upper Darby, Pa, USA: Monographs in Contemporary Audiology; 1982. pp. 147–155. [Google Scholar]
- 10.Demorest ME, Erdman SA. Development of the communication profile for the hearing impaired. Journal of Speech and Hearing Disorders. 1987;52(2):129–143. doi: 10.1044/jshd.5202.129. [DOI] [PubMed] [Google Scholar]
- 11.Cox RM, Gilmore C. Development of the profile of hearing aid performance (PHAP) Journal of Speech and Hearing Research. 1990;33(2):343–357. doi: 10.1044/jshr.3302.343. [DOI] [PubMed] [Google Scholar]
- 12.Cox RM, Alexander GC. The abbreviated profile of hearing aid benefit. Ear and Hearing. 1995;16(2):176–186. doi: 10.1097/00003446-199504000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I. Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models. Health Technology Assessment. 2007;11(42):1–294. doi: 10.3310/hta11420. [DOI] [PubMed] [Google Scholar]
- 14.Hojan E, Sworek K, Furmann A. Abbreviated profile of aid benefit (APHAB) Personality and Social Psychology Bulletin. 2000;11:31–38. [Google Scholar]
- 15.Cox RM, Alexander GC, Gray GA. Audiometric correlates of the unaided APHAB. Journal of the American Academy of Audiology. 2003;14(7):361–371. [PubMed] [Google Scholar]


