Abstract
Background:
Concussions represent 8.9% to 13.2% of all high school athletic injuries. How these injuries are managed is currently unknown.
Hypothesis:
There are differences in concussion management and awareness among boys football, boys ice hockey, and boys and girls soccer.
Study Design:
Descriptive epidemiologic study.
Methods:
High school athletic directors were contacted via e-mail and asked to complete, and request that their staff complete, an online survey with 4 sections aimed at athletic directors, head coaches, team physicians, and certified athletic trainers.
Results:
According to coaches, concussion awareness education was provided for football (97%), hockey (65%), and boys and girls soccer (57% and 47%, respectively) (P < 0.01). Use of sideline screening tools was significantly greater for football (P = 0.03). All participants agreed that a player who has suffered a concussion cannot return to play the same day.
Conclusion:
There is a difference in concussion management and awareness among the 4 sports. Concussion education is well promoted in football but should be expanded in soccer and hockey. Players are not allowed to return to play the same day, and the majority are referred to a physician.
Clinical Relevance:
Study results highlight the differences in concussion education among sports. Health care providers should address these gaps.
Keywords: concussion, return-to-play, concussion awareness, high school athletics
The US Centers for Disease Control and Prevention estimates that 1.6 to 3.8 million concussions occur during sport and recreational activity annually.10 A concussion is a complex pathophysiologic process affecting the brain induced by traumatic biomechanical forces.14 Each year, millions of adolescents participate in high school sports, over the course of which they are at risk for injuries, including concussions. Concussions represent 8.9%6 to 13.2%12 of all high school athletic injuries and 5.8%6 of all collegiate injuries. However, these rates may actually be higher, as concussions can be underreported.9,10,13
The rate of concussion among US high school athletes is estimated to be 300,000 per year.12 Studies have found that concussions tend to occur more frequently during competition.12 The breakdown by sport has been reported as 40%4 to 47%12 for football, 8.2%12 to 21%4 for girls soccer, and 15%4 for boys soccer. Concussions have represented a high proportion of total injuries in ice hockey12 and have been occurring at an increasing rate.5 For all athletes, concussion rates in high school athletics have increased by 16% annually from the 1997-1998 to 2007-2008 academic years, possibly resulting from an increase in injury or diagnosis.11 Because of increased participation in high school athletics, there is a responsibility of the school staff to properly promote concussion awareness, prevention, and management.17
To appropriately evaluate and treat concussions, an athletic program should have a clearly defined concussive injury policy produced by athletic directors, coaches, physicians, certified athletic trainers (ATCs), and other stakeholders. For the most effective management, all staff members must be well informed and prepared to take the proper steps within the school’s guidelines. A recent study examined high school football coaches’ understanding and management of concussions7 and found that the coaches had a greater understanding than the general public.7 Previous studies have examined the epidemiology of concussions and management of symptoms.6,8,18,22 However, few have focused on player education and whether schools are following return-to-play guidelines and the decision making involved. The purpose of this study was to explore concussion management and return-to-play policies in high schools by surveying athletic directors, head coaches (football, hockey, and boys and girls soccer), team physicians, and ATCs on their schools’ concussion policy and its execution. The hypothesis was that there would be differences in concussion management and awareness among boys football, soccer, and ice hockey and girls soccer.
Methods
Approval was obtained through the institution’s Institutional Review Board (no. 038711B3X) prior to initiation of any study-related procedures. High school athletic directors from the state of Michigan were contacted via e-mail and asked to have their staff complete an online survey with 4 sections, for athletic directors, head coaches, team physicians, and ATCs. The survey was intended to be completed by the athletic director and any head coach, physician, or ATC affiliated with boys football, boys soccer, boys ice hockey, or girls soccer teams, as these sports showed the highest concussion rates per exposure.6
A database was created of 579 high schools in 10 counties according to the Public School Review and Private School Review websites (http://publicschoolreview.com and http://privateschoolreview.com). Eligible programs were associated with currently operating schools participating in the Michigan High School Athletic Association. Public, private, and nonpublic charter schools were included, yielding 314 eligible schools.
The survey determined concussion management and return-to-play guidelines among the staff involved. Each of the 4 surveys was tailored to the respondent’s position to avoid guessing or false reporting (see online appendix, available at http://sph.sagepub.com/content/suppl). Surveys included demographic questions about the size and classifications of the respondent’s school and his or her title, sport supported, and level of experience. Precautions taken by the team regarding concussion management were noted. The survey assessed the respondent’s level of familiarity with different concussion policies. Participants were asked to describe the concussion-screening tools that their school used, how they diagnose a concussion, and what steps they take when a concussion is diagnosed. They were also asked if athletes were educated on concussions prior to the start of the season.
A letter was mailed to the athletic directors informing them that they would be receiving an e-mail asking them to take an anonymous survey and to forward it to the necessary personnel. Two reminder e-mails were sent 3 and 6 weeks after the initial one asking them to complete the survey and follow-up with their staff. Although the survey was anonymous, participants were asked to enter a random de-identified code for their school so that the authors could determine how many schools had at least 1 participant.
Answers to all questions were compiled. To examine the differences in responses based on the sport played, a 4 × 2 chi-square analysis (sport × response, where sport meant football, ice hockey, boys soccer, or girls soccer) was performed with appropriate Yates continuity corrections (α = 0.05). Where P < 0.05, analyses were subdivided into a series of five 2 × 2 chi-square analyses (sport × response), where the sport categories were football versus all others, ice hockey versus all others, boys soccer versus all others, girls soccer versus all others, and soccer versus all others to determine whether there was a significant difference for a particular sport.
Results
Of the 314 high schools contacted, 5 had been permanently closed, and 6 chose to opt out of the survey. A total of 235 responses were received, including responses from 108 schools (response rate, 35%). Seventy-one athletic directors, 119 head coaches, and 45 ATCs responded; there were no responses from team physicians. Because the initial contact was made with the athletic directors, the authors cannot conclude the number of coaches, ATCs, or physicians that the survey was sent to. Of the 119 head coaches, 35 coached boys football; 21, boys ice hockey; 31, boys soccer; and 32, girls soccer. Forty-four ATCs worked with football; 27, ice hockey; 36, boys soccer; and 36, girls soccer.
The use of preseason concussion education and baseline cognitive testing was broken down by sport for both coaches and ATCs (Figure 1). According to coaches, concussion awareness education was provided for football players 97% of the time; hockey players, 65%; boys soccer, 57%; and girls soccer, 47%, χ2(3) = 19.42 (P < 0.01). Education of football players was significantly greater than all other groups (P < 0.01). Overall, soccer players were educated significantly less than ice hockey and football players (P < 0.01). Girl soccer players were educated significantly less overall (P = 0.04). Seventy-six percent of football ATCs responded that players were provided concussion education, compared with 56% and 48% for boys and girls soccer, respectively, and 70% for hockey, χ2(3) = 8.60 (P = 0.04). Football was significantly greater in this regard (P = 0.04), and soccer, significantly worse (P = 0.01). Seventy-two percent of athletic directors stated that their school had informational material available on concussion education.
Figure 1.
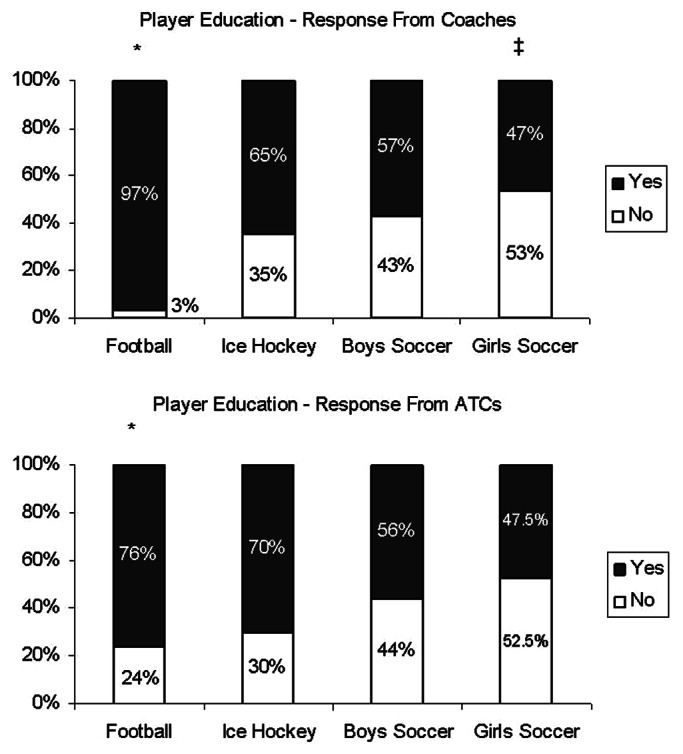
Percentage of players educated at the beginning of the season.
*Significantly more yes responses than other groups. ‡Significantly more no responses than other groups.
Athletic directors and coaches were more familiar with the state’s athletic association concussion guidelines than any of the other guidelines examined. Ninety-five percent of coaches reported being very or somewhat familiar with the state guidelines,15 and only 31%, very or somewhat familiar with the consensus statement.14 ATCs had the most familiarity with the state concussion guidelines15 (93%) and the National Athletic Trainers’ Association’s statement8 (98%). ATCs were also relatively familiar with all other major concussion guidelines (Figure 2).
Figure 2.
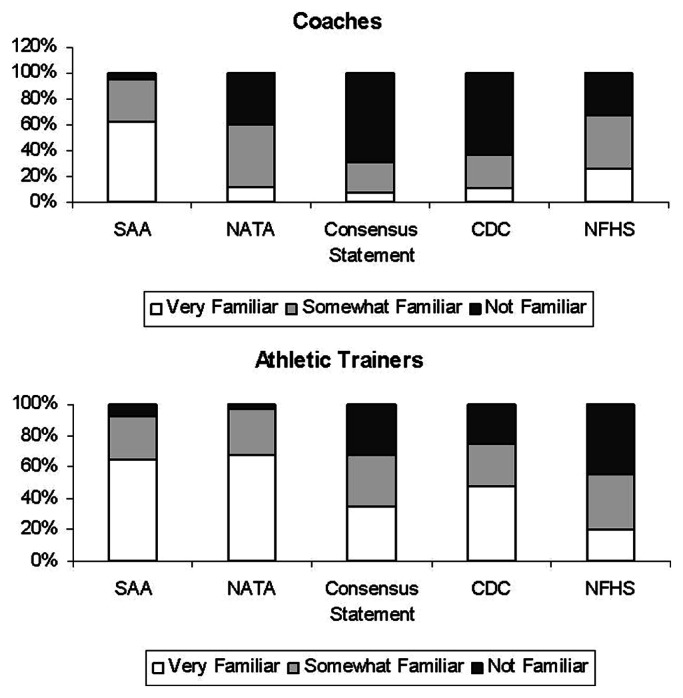
Familiarity with National Athletic Trainers’ Association’s (NATA’s) position statement on management of sport-related concussion,8 the consensus statement on concussion in sport from the Third International Conference on Concussion in Sport,14 “Heads Up” concussion kit from the Centers for Disease Control and Prevention (CDC),20 state athletic association (SAA) protocol for implementation of National Federation sports playing rules for concussions,15 and the National Federation of State High School Associations (NFHS) online course on concussions in sport.16
When asked whether their school had a written policy in place to manage concussions, 50% of athletic directors, 62% of coaches, and 53% of ATCs said yes. When these answers were compared within the school, there were 18 incidents where respondents indicated a different answer compared with their colleagues. When asked what the policy was based on, most respondents said the state-issued guidelines (Figure 3).
Figure 3.
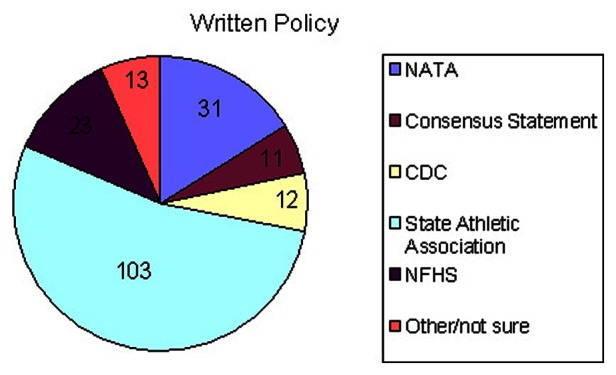
Answers regarding the basis for the written policy in place to manage sport-related concussions. NATA, National Athletic Trainers’ Association; CDC, Centers for Disease Control and Prevention; NFHS, National Federation of State High School Associations.
There was no significant difference among sports when coaches and ATCs were asked whether they conducted baseline cognitive evaluations for their athletes. Overall, 20% of coaches responded that these evaluations were conducted, and 37% of ATCs reported using them.
Participants were asked to list the signs and symptoms used when a concussion is suspected, and the majority of responses were commonly perceived factors, such as loss of consciousness, confusion, disorientation, lack of concentration, headaches, nausea, vomiting, dizziness, memory loss, dilated pupils, blurred vision, and loss of balance or coordination. Coaches and ATCs were also asked whether on-field or sideline screening tools were used. ATCs reported using them approximately 75% of the time, which was not significantly different among the sports. According to coaches, sideline screening tools were used for football players 55% of the time; hockey players, 50%; boys soccer, 30%; and girls soccer, 17%, χ2(3) = 11.64 (P = 0.01). Use of sideline screening tools was significantly higher for football (P = 0.03) and significantly less for soccer (P < 0.01). Sideline screening tool use was significantly less for girls soccer compared with all other groups (P = 0.04) (Figure 4).
Figure 4.
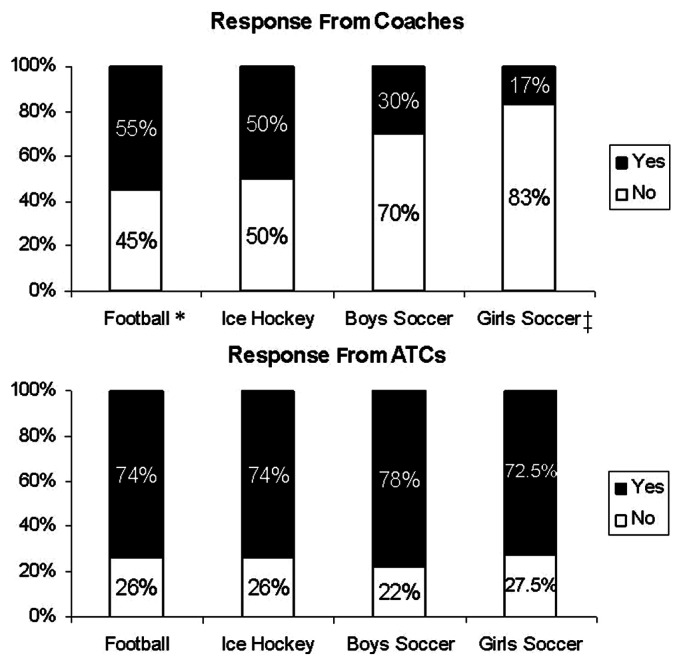
Use of sideline screening tools.
*Sideline tools used significantly more. ‡Sideline tools used significantly less.
All participants agreed that a player who suffered a concussion cannot return to play the same day. Parents are also notified when a player suffers a concussion. Thirty-five percent of athletic directors, 49% of coaches, and 18% of ATCs said they report concussions to the state athletic association. The survey also asked if players were referred to a physician after concussion, which was done 98%, 90%, and 93% of the time by athletic directors, coaches, and ATCs, respectively. Physician clearance before return to play was required by 95%, 89%, and 90% of athletic directors, coaches, and ATCs, respectively.
Discussion
The results support the hypothesis that there would be a difference in concussion management and awareness among the 4 sports. Concussion education is well promoted in football but should be reevalutated in soccer and hockey, as the rates of preseason concussion education provided for these sports were significantly lower than for football. Sarmiento et al20 published reports evaluating the use of the Centers for Disease Control and Prevention’s “Heads Up” tool kit by high school coaches. Eighty-four percent of coaches who ordered the kit provided concussion education to their athletes; 90% of respondents reported using at least 1 of the materials from the kit.20 Because of this kit, half of the coaches changed their views on the seriousness of concussions, and 38% made changes in their prevention and management strategies.20 There are specific kits available for each sport, and it is possible that promoting this kit to soccer and ice hockey coaches could improve concussion education strategies for non-football-playing student athletes.
Athletes are more likely to sustain a concussion during a game than practice.4,12 ATCs were present at more than two-thirds of games but less than one-quarter of soccer and hockey practices. This means that coaches are responsible for potential recognition of a concussion the majority of the time. Approximately half of football and hockey coaches reported using some type of sideline screening tool to determine if a player had sustained a concussion; the proportion of soccer coaches using sideline screening was significantly lower. Many coaches stated that they always defer concussion screening to their ATC. A study by Valovich-McLeod et al21 found that coaches who attended a coaching course or workshop were more likely to correctly report signs and symptoms of concussion, supporting increased education for coaches.
Currently, 40 states and Washington, DC, have some sort of legislation regarding concussions. At the time that this study was conducted, Michigan did not have legislation requiring all athletes to be educated/trained about concussions and players with a suspected concussion to be immediately removed from play, with written clearance required from a qualified licensed health care professional before return to play.19 It is possible that this new, recently signed law could affect the results from this study.19 A follow-up study could examine whether this law helps to increase concussion education among sports other than football.
The Michigan High School Athletic Association recently revised its concussion management policy to align with the rules of the National Federation of State High School Associations.15 The new policy states, “Any athlete who exhibits sign, symptoms, or behaviors consistent with a concussion shall be immediately removed from the contest and shall not return to play until cleared by an appropriate health care professional.”15 Compliance with graduated return-to-play guidelines has been reported to be poor among high school students, as Yard and Comstock22 found that almost half of students were not compliant with return-to-play guidelines and 1 in 6 athletes returned prematurely under the previous Prague return-to-play guidelines.
In addition to potential prolongation of concussion symptoms, students returning to play before full recovery of symptoms may be at risk of further injury.1 The majority of respondents stated that players were required to be cleared by a physician or neuropsychologist prior to returning to play. However, without a written policy, this is difficult to enforce. Continuing efforts need to be made to educate coaches, parents, athletes, and policy makers on the consequences of returning athletes to play prematurely after concussive injuries.7
The most education about head injuries and concussions is available for sports at the highest risk for concussion, such as football. Girls soccer had especially low rates of concussion education. It is important to ensure that female players are provided with a concussion education program as they have proven to be more likely to sustain a concussion than male players participating in the same sport.2-4,10
There were limitations to this study. As with many survey-based studies, the response rate was low. Overall, 35% of schools originally sent the survey responded. However, the number of responses from coaches in each individual sport was low. An exact response rate for coaches or ATCs cannot be determined, as it is unknown how many total ATCs or coaches were possible. Also, no physicians returned the survey.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this manuscript.
References
- 1. Byard RW, Vink R. The second impact syndrome. Forensic Sci Med Pathol. 2009;5(1):36-38 [DOI] [PubMed] [Google Scholar]
- 2. Covassin T, Elbin RJ. The female athlete: the role of gender in the assessment and management of sport-related concussion. Clin Sports Med. 2011;30(1):125-131 [DOI] [PubMed] [Google Scholar]
- 3. Covassin T, Elbin R, Stiller-Ostrowski JL. Current sport-related concussion teaching and clinical practices of sports medicine professionals. J Athl Train. 2009;44(4):400-404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Daneshvar DH, Nowinski CJ, McKee AC, Cantu RC. The epidemiology of sport-related concussion. Clin Sports Med. 2011;30(1):1-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Deits J, Yard EE, Collins CL, Fields SK, Comstock RD. Patients with ice hockey injuries presenting to US emergency departments, 1990-2006. J Athl Train. 2010;45(5):467-474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gessel LM, Fields SK, Collins CL, Dick RW, Comstock RD. Concussions among United States high school and collegiate athletes. J Athl Train. 2007;42(4):495-503 [PMC free article] [PubMed] [Google Scholar]
- 7. Guilmette TJ, Malia LA, McQuiggan MD. Concussion understanding and management among New England high school football coaches. Brain Inj. 2007;21:1039-1047 [DOI] [PubMed] [Google Scholar]
- 8. Guskiewicz KM, Bruce SL, Cantu RC, et al. National Athletic Trainers’ Association position statement: management of sport-related concussion. J Athl Train. 2004;39(3):280-297 [PMC free article] [PubMed] [Google Scholar]
- 9. Kaut KP, DePompei R, Kerr J, Congeni J. Reports of head injury and symptom knowledge among college athletes: implications for assessment and educational intervention. Clin J Sport Med. 2003;13(4):213-221 [DOI] [PubMed] [Google Scholar]
- 10. Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375-378 [DOI] [PubMed] [Google Scholar]
- 11. Lincoln AE, Caswell SV, Almquist JL, Dunn RE, Norris JB, Hinton RY. Trends in concussion incidence in high school sports. Am J Sports Med. 2011;39(5):958-963 [DOI] [PubMed] [Google Scholar]
- 12. Marar M, McIlvain NM, Fields SK, Comstock RD. Epidemiology of concussions among United States high school athletes in 20 sports. Am J Sports Med. 2012;40(4):747-755 [DOI] [PubMed] [Google Scholar]
- 13. McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. Unreported concussion in high school football players: implications for prevention. Clin J Sport Med. 2004;14(1):13-17 [DOI] [PubMed] [Google Scholar]
- 14. McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport: the Third International Conference on Concussion in Sport held in Zurich, November 2008. Phys Sports Med 2009;37(2):141-159 [DOI] [PubMed] [Google Scholar]
- 15. Michigan High School Athletic Association Health and safety. http://www.mhsaa.com/Schools/HealthSafetyResources.aspx Accessed January 10, 2013
- 16. National Federation of State High School Associations Concussion in sports: what you need to know. http://www.nfhslearn.com/electiveDetail.aspx?courseID=38000 Accessed January 10, 2013
- 17. National Federation of State High School Associations High school sports participation continues upward climb. http://www.nfhs.org/content.aspx?id=5752 Accessed October 3, 2011
- 18. Powell JW, Barber-Foss KD. Traumatic brain injury in high school athletes. J Am Med Assoc. 1999;282(10):958-963 [DOI] [PubMed] [Google Scholar]
- 19. Proos J, Brandenburg J, Marleau J, Hansen G, Jones R. Youth athlete concussion. Senate Bill 1122 (S-1). 2012 [Google Scholar]
- 20. Sarmiento K, Mitchko J, Klein C, Wong S. Evaluation of the Centers for Disease Control and Prevention’s concussion initiative for high school coaches: “Heads up: concussion in high school sports.” J Sch Health. 2010;80(3):112-118 [DOI] [PubMed] [Google Scholar]
- 21. Valovich-McLeod TC, Schwartz C, Bay RC. Sport-related concussion misunderstanding among youth coaches. Clin J Sports Med. 2007;17(2):140-142 [DOI] [PubMed] [Google Scholar]
- 22. Yard EE, Comstock RD. Compliance with return to play guidelines following concussion in US high school athletes, 2005-2008. Brain Inj. 2009;23(11):888-898 [DOI] [PubMed] [Google Scholar]


