Abstract
Objectives:
To determine the immediate effects of Kinesio taping directed to the hip and manipulation directed to the lumbopelvic region in individuals with unilateral patellofemoral pain syndrome (PFPS).
Background:
PFPS affects up to 25% of the general population. Despite the high prevalence, this condition is not clearly understood, as evidenced by the numerous proposed causes and recommended treatments. Notwithstanding, recent evidence suggests that treatments directed at the hip or spine may lead to beneficial results.
Methods:
A convenience sample of 18 participants (12 men and 6 women, 19.5 ± 1.15 years old) with unilateral PFPS was recruited. Participants were randomized by sex to 1 of 3 groups: Kinesio taping, manipulation, and control taping. The main outcome measures included the Y-balance test, squatting range of motion (ROM), and the Lower Extremity Functional Scale.
Results:
Compared with the lumbopelvic manipulation and control groups, those in the Kinesio taping group performed significantly better on the Y-balance test (F = 5.59, P = 0.02) and with squatting ROM (F = 3.93, P = 0.04). The Kinesio taping and lumbopelvic groups were also significantly better than the control (sham) group with double-leg squatting ROM performance 3 days later.
Conclusion:
Kinesio taping may facilitate gluteus medius activation and improve postural stability and a double-leg squat.
Clinical Relevance:
The improvement in affected limb reach and double-leg squatting ROM highlights the potential for Kinesio taping to improve gluteus medius activation. Lumbopelvic manipulation may also immediately improve rehabilitation programs for PFPS.
Keywords: patellofemoral pain, Kinesio tape, lumbopelvic manipulation, Y-balance
Patellofemoral pain syndrome (PFPS) affects up to 25% of the general population.30 It is the most common overuse injury in runners12 and represents 25% to 40% of knee complaints in sports medicine clinics.3,10 Despite the high prevalence, this condition is not clearly understood, as evidenced by the many proposed causes and equally abundant number of recommended interventions.26 Because of this general lack of understanding, treatments and subsequent outcomes are highly inconsistent.26
Researchers have explored intrinsic versus extrinsic factors as well as distal versus proximal factors in regard to the etiology and treatment of PFPS; results have been limited or highly inconsistent.1-4,12,13,16,26,30,34,44 For example, impaired vastus medialis obliquus activation gained favor as a main contributor to PFPS; however, this theory lost support, as additional evidence demonstrated conflicting results.23,26,28,44 Patellar position and subsequent patellar taping showed promising early results,1,23,43,44 although subsequent research did not demonstrate the same positive effects.30,39
Recently, research has focused on the influence of proximal factors (hip and spine) that may contribute to this condition.2,4,12,13,27,31,34,36,38,44 Women with PFPS have increased peak hip internal rotation along with decreased hip muscle strength compared with healthy controls.34,37 Knee and hip strengthening significantly improved pain and function versus knee strengthening alone in women with PFPS.41 A preliminary clinical prediction rule has been proposed for the treatment of PFPS.27 Of the 5 factors that predicted a favorable response to treatment, hip internal rotation difference greater than 14° was 2 times more predictive than each of the 4 distal factors.
Kinesiology tape treatment can significantly reduce pain during shoulder motion.40 Additionally, Kinesio tape treatment reduced cervical pain and increased range of motion (ROM) 24 hours following whiplash injury.21 There are many studies on patellar taping, but they have not included proximal taping to facilitate hip musculature.18,24,25,42
The primary objective of this study was to determine the immediate effects of 2 proximal interventions (kinesiology taping directed to the hip and manipulation of the lumbopelvic region) on knee function and pain in individuals with unilateral PFPS.27 In addition, the clinical utility of the lumbopelvic prediction was assessed.
Methods
The Institutional Review Board at Keller Army Community Hospital granted approval for this study. A convenience sample of 18 participants (12 men and 6 women, 19.5 ± 1.15 years old) with unilateral PFPS was recruited from a walk-in sports medicine clinic at a small university. To be included, participants had to complain of diffuse unilateral anterior knee pain of at least 2 weeks and report 3 of the following 5 criteria: pain with running, stair climbing, squatting, sitting, and knee flexion.1,2,13 Exclusion criteria included knee tendinopathy, lower extremity fracture, knee or ankle ligamentous injury, and conditions affecting balance (eg, concussion), osteoarthritis, lower extremity or back surgery (including arthroscopy), patellar subluxtion/dislocation, or neurologic deficit. Each participant was given a verbal explanation of the study protocol and provided written informed consent prior to participation.
Treatments
A certified Kinesio taping practitioner administered all treatments. The lumbopelvic manipulation was performed as previously described on the symptomatic side (Figure 1).5,6,19,20,27
Figure 1.

Lumbopelvic manipulation set up with the thrust applied through the hand on the hip.
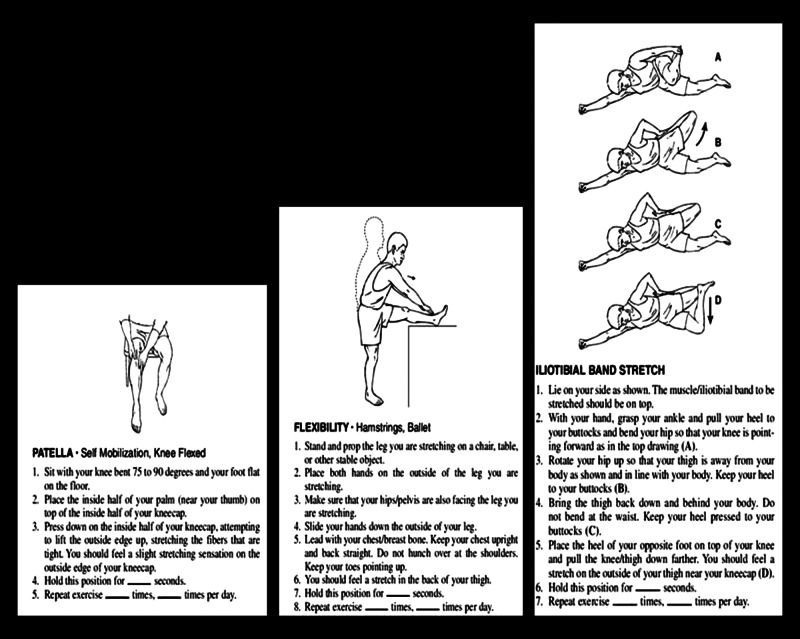
The kinesiology tape (Kinesio Tex Tape, Albuquerque, New Mexico) was applied to the lateral hip of the affected side to facilitate gluteus medius muscle activation while the participant was lying down with the affected hip up.29 The first third of one I-strip began at the posterior iliac crest without tension to provide an anchor that did not cross the target tissue. The participant actively flexed the adducted hip to allow application of the middle third of the tape with approximately 50% tension (able to visualize the wave pattern in the tape). Subsequently, with the leg in the original position, the remainder of the tape was applied without tension, ending approximately at the greater trochanter. Afterward, the second I-strip was applied in the same manner starting at the anterior iliac crest (Figure 2). Participants were instructed to leave the tape in place until the follow-up visit.
Figure 2.
Kinesio tape of the affected limb hip for facilitation of gluteus medius.
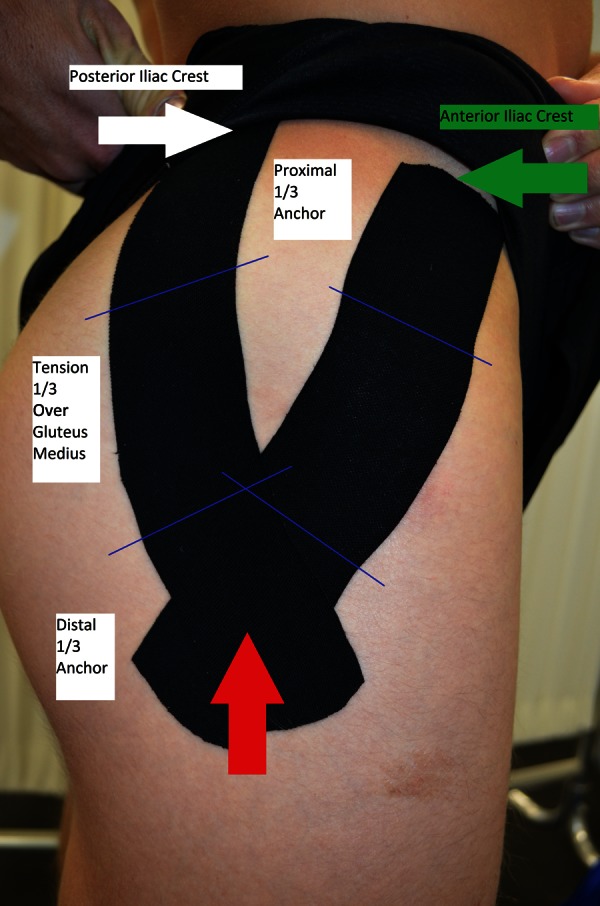
The control group (sham tape application) received a single strip of Kinesio tape across the lateral affected hip without tension in the tape or muscle stretch (Figure 3). Participants were instructed to leave the tape in place until the follow-up. Additionally, all were instructed to perform 3 standard lower extremity flexibility exercises (Figure 4).
Figure 3.

Sham taping of the affected limb hip.
Figure 4.
Standard lower extremity stretching that each participant was trained to perform. Instructions were issued in handout version.
Procedures
Baseline measures and randomization
Participants completed a demographic and injury information questionnaire, the Lower Extremity Functional Scale (LEFS), and the visual analog scale (VAS) for pain at rest. They completed a VAS immediately after performing a double-leg squat and a step-up and step-down maneuver. Additional measurements included knee ROM while squatting (average of 2 measurements recorded based on an 18-in goniometer on the affected limb), limb length from inferior portion of the anterior superior iliac spine to the distal medial malleolus, supine hip internal rotation, prone dorsiflexion with the knee flexed, and the standing navicular drop. A blinded second investigator assessed the Y-balance tests.
For the Y-balance test, the participants viewed an informational video (http://www.myinjuryrisk.com, Y-balance test group instruction video). Following a 5-minute warm-up on a stationary bicycle, standard instruction for the lower extremity Y-balance9 was given to emphasize proper execution. Four practice trials reaching in each direction were performed to minimize a potential testing effect.35 After the practice trials, the Y-balance testing was conducted with 3 correctly performed repetitions in each direction for each limb.9 For the composite Y-balance measures, normalization by limb length was calculated.9,32,33
Participants were then randomly assigned by sex distribution to 1 of 3 groups: Kinesio taping (n = 6), manipulation (n = 6), and control taping group (n = 6).
Intervention and immediate assessment
Following group assignment, the selected intervention was performed. Immediately following the intervention, squatting ROM measurements and the VAS for pain were repeated along with the retest. Reliability was evaluated by comparing measurements of the unaffected limb during baseline and the immediate follow-up assessment.
Three-day follow-up assessment
On this day, a second LEFS, pain at rest (VAS), squatting ROM, pain with squatting (VAS), and a third Y-balance testing were performed. Short-term reliability was assessed with the unaffected Y-balance distances reached at the 3-day follow-up compared with the baseline measurements.
Statistical Analysis
The independent variable was the interventions with 3 levels: manipulation, Kinesio tape, and control (sham) taping. Dependent variables analyzed included LEFS, squatting ROM, VAS pain with squatting, Y-balance normalized limb difference, and VAS pain with Y-balance. Differences in change from baseline for the dependent variables were examined with a 1-way analysis of variance. When applicable, post hoc testing in the form of the least significant difference was employed. Significance level for all statistical tests was set at P < 0.05. All statistical analyses were performed using SPSS 11.5 (IBM, Armonk, New York). For the clinical utility, the manipulation rule (3 of 5 characteristics) was used to determine success with treatment.
Results
All 18 participants (4 men and 2 women per group) completed the study; the mean follow-up time was 3.11 ± 0.65 days. Demographic characteristics were similar among groups; however, knee pain with the Y-balance test during the initial evaluation was significantly greater in the manipulation group compared with the control group (Table 1).
Table 1.
Baseline characteristics between the groups assessed by 1-way analysis of variance test
| Characteristic | Mean ± SD | F | P |
|---|---|---|---|
| Age, y | 19.5 ± 1.15 | 0.349 | 0.71 |
| Height, cm | 173.78 ± 9.10 | 0.109 | 0.98 |
| Weight, kg | 71.67 ± 9.81 | 0.576 | 0.57 |
| Lower Extremity Functional Scale | 60.89 ± 8.98 | 2.643 | 0.10 |
| Limb length uninvolved, cm | 90.41 ± 6.22 | 0.336 | 0.72 |
| Limb length involved, cm | 90.50 ± 6.13 | 0.297 | 0.74 |
| Squat range of motion, deg | 101.25 ± 22.07 | 0.590 | 0.57 |
| Squat pain, visual analog scale | 31.67 ± 18.92 | 2.097 | 0.16 |
| Y-balance composite involved, cm | 91.08 ± 9.47 | 2.803 | 0.09 |
| Y-balance composite uninvolved, cm | 94.84 ± 10.16 | 2.716 | 0.10 |
| Y-balance limb difference, cm | 3.77 ± 4.79 | 1.83 | 0.19 |
| Pain with Y-balance, visual analog scale | 28.06 ± 17.98 a | 4.526 b | 0.03 b |
Control, 16.5 ± 15.31; manipulation, 42.33 ± 17.52; and Kinesio, 25.33 ± 11.99.
The manipulation group was significantly different from the control group.
Immediate Assessment
A significant treatment effect was observed (F = 6.13, P = 0.01) for Y-balance performance during the immediate assessment. The change in performance on the affected lower extremity was significantly greater in the Kinesio taping group (4.4 ± 2.4 cm) compared with the manipulation group (1.6 ± 1.3 cm) and the control group (0.7 ± 1.9 cm). A significant treatment effect was also observed (F = 3.93, P = 0.04) for double-leg squatting ROM. The change in performance was significantly greater in the Kinesio taping group (10.2° ± 6.1°) compared with the manipulation group (4.8° ± 5.0°) or the control group (1.1° ± 4.1°). During the immediate intervention assessment, no significant differences were observed between groups for VAS pain with squatting (F = 0.74, P = 0.494) or VAS pain with the Y-balance (F = 0.684, P = 0.519).
Three-Day Follow-up Assessment
A significant treatment effect was observed (F = 4.88, P = 0.02) for double-leg squatting ROM during the short-term assessment. The change in performance was significantly greater in the Kinesio taping group (15.2° ± 5.6°) compared with the control group (0.7 ± 1.9°). No short-term differences (P = 0.12) were observed between the Kinesio taping group and the manipulation group during the short-term follow-up. During the short-term assessment, no significant differences were observed between groups for Y-balance performance (F = 1.56, P = 0.24), VAS pain with squatting (F = 2.99, P = 0.09), VAS pain with the Y-balance (F = 1.67, P = 0.22), or with the LEFS (F = 1.91, P = 0.18). Mean change in VAS pain from baseline to 3 days later was 1.8 and 2.2 cm for the Kinesio tape and manipulation groups, respectively. Mean change in the LEFS score was 5 (Kinesio tape), 3 (manipulation), and 1 (sham group).
Lumbopelvic Manipulation Prediction Rule
Three individuals in the manipulation group met the prediction rule, and 2 experienced success with manipulative treatment.
Discussion
The results of this randomized controlled trial suggest that Kinesio taping focused on gluteus medius activation may be superior to lumbopelvic manipulation and control (sham) taping in regard to change in lower extremity function as measured by Y-balance performance and squatting ROM immediately following intervention. Kinesio taping may also be superior to control taping up to 3 days later.
A growing body of evidence suggests that interventions directed at the hip are beneficial for many who have PFPS.8,15,22,26,38,41 Further evidence suggests that Kinesio tape can decrease immediate and short-term musculoskeletal symptoms.21,25,40,42,45 The improved immediate functional results with Kinesio tape support previous research.21,25,40,42,45
The positive results could be from the contributions of kinesthesia cutaneous receptors, proprioception, and hip motor control and not necessarily just pain modulation.7,17,25,40,45 Cutaneous receptors may augment and override the muscle spindle feedback.7,17 When muscle spindles and cutaneous receptors are activated together, larger responses in kinesthesia and proprioception can be seen at multiple joints compared with skin stretch or muscle spindle activation alone.7 Increased proprioception and kinesthesia may contribute to greater motor control.
Mediation and facilitation of neural excitability via spinal/lumbopelvic manipulation could affect quadriceps activation and spinal reflex excitability immediately after intervention.14,22,38 In the current study, the change in squatting ROM between the immediate assessment and 3-day follow-up was highest in the lumbopelvic manipulation group.
Previous research on the reliability and responsiveness of VAS scores in individuals with PFPS identified a minimal clinically important difference of 1.5 to 2.0 cm.11 In the present study, both the Kinesio taping group and the manipulation group experienced a mean decrease in VAS scores of 1.8 and 2.2 cm with squatting from baseline to 3 days later. Therefore, while there was not a statistically significant difference in VAS change, there was arguably a short-term clinically meaningful decrease in pain with both interventions.
The improvement in affected limb reach and meaningful pain decrease in this study highlights the potential of Kinesio taping for gluteus medius activation and lumbopelvic manipulation as adjuncts to rehabilitation programs immediately.
The obvious limitations were the small sample size and short follow-up. An a priori power analysis of 80% with a moderate effect size indicated that a group of 10 participants was sufficient; however, only 6 participants per group could be recruited. While the concern for a small sample size is important, sufficient power to detect differences in Y-balance performance and squatting ROM existed. Additionally, the narrow age range of the participants restricts the generalizability of the results. Finally, the assessment of the prediction rule had a severe limitation owing to the sample size of only 6 participants.
Conclusion
For the treatment of PFPS, Kinesio taping directed at facilitating gluteus medius activation may increase the immediate postural stability as measured by the Y-balance test. The double-leg squat may also increase with the gluteus medius Kinesio taping procedure. Lumbopelvic manipulation also provided benefits. The improvement in affected limb reach, double-leg squatting ROM, and meaningful pain decrease highlights the potential benefit of gluteus medius Kinesio taping for young active individuals diagnosed with PFPS.
Footnotes
The author(s) of this article are U.S. government employees and created the article within the scope of their employment. As a work of the U.S. federal government, the content of the article is in the public domain.
The authors report no potential conflicts of interest in the development and publication of this manuscript.
References
- 1. Aminaka N, Gribble PA. Patellar taping, patellofemoral pain syndrome, lower extremity kinematics, and dynamic postural control. J Athl Tr. 2008;43:21-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barton CJ, Bonanno D, Levinger P, Menz HB. Foot and ankle characteristics in patellofemoral pain syndrome: a case control and reliability study. J Orthop Sports Phys Ther. 2010;40:286-296 [DOI] [PubMed] [Google Scholar]
- 3. Bizzini M, Childs JD, Piva SR, Delitto A. Systematic review of the quality of randomized controlled trials for patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2003;33:4-20 [DOI] [PubMed] [Google Scholar]
- 4. Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome. Am J Sports Med. 2009;37:2108-2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Childs JD, Flynn TW. Spinal manipulation for low back pain. Ann Intern Med. 2004;140:665. [DOI] [PubMed] [Google Scholar]
- 6. Childs JD, Fritz JM, Flynn TW, et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med. 2004;141:920-928 [DOI] [PubMed] [Google Scholar]
- 7. Collins DF, Refshauge KM, Todd G, Gandevia SC. Cutaneous receptors contribute to kinesthesia at the index finger, elbow, and knee. J Neurophysiol. 2005;94:1699-1706 [DOI] [PubMed] [Google Scholar]
- 8. Connell T. Concepts for assessment and treatment of anterior knee pain related to altered spinal and pelvic biomechanics: a case report. Man Ther. 2008;13:560-563 [DOI] [PubMed] [Google Scholar]
- 9. Cook G, Burton L, Kiesel K, Rose G, Bryant MF. Movement: Functional Movement Systems. Screening, Assessment, Corrective Strategies. Aptos, CA: On Target Publications; 2010:367-369 [Google Scholar]
- 10. Coppack RJ, Etherington J, Wills AK. The effects of exercise for the prevention of overuse anterior knee pain: a randomized controlled trial. Am J Sports Med. 2011;39:940-948 [DOI] [PubMed] [Google Scholar]
- 11. Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil. 2004;85:815-822 [DOI] [PubMed] [Google Scholar]
- 12. Dierks TA, Manal KT, Hamill J, Davis I. Lower extremity kinematics in runners with patellofemoral pain during a prolonged run. Med Sci Sports Exerc. 2011;43:693-700 [DOI] [PubMed] [Google Scholar]
- 13. Dierks TA, Manal KT, Hamill J, Davis IS. Proximal and distal influences on hip and knee kinematics in runners with patellofemoral pain during a prolonged run. J Orthop Sports Phys Ther. 2008;38:448-456 [DOI] [PubMed] [Google Scholar]
- 14. Dishman JD, Burke J. Spinal reflex excitability changes after cervical and lumbar spinal manipulation: a comparative study. Spine J. 2003;3:204-212 [DOI] [PubMed] [Google Scholar]
- 15. Dolak KL, Silkman C, Medina McKeon J, Hosey RG, Lattermann C, Uhl TL. Hip strengthening prior to functional exercises reduces pain sooner than quadriceps strengthening in females with patellofemoral pain syndrome: a randomized clinical trial. J Orthop Sports Phys Ther. 2011;41:560-570 [DOI] [PubMed] [Google Scholar]
- 16. Draper CE, Souza RB, Fredericson M, Powers CM. Femur rotation and patellofemoral joint kinematics: a weight-bearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther. 2010;40:277-285 [DOI] [PubMed] [Google Scholar]
- 17. Edin BB. Quantitative analyses of dynamic strain sensitivity in human skin mechanoreceptors. J Neurophysiol. 2004;92:3233-3243 [DOI] [PubMed] [Google Scholar]
- 18. Firth BL, Dingley P, Davies ER, Lewis JS, Alexander CM. The effect of kinesiotape on function, pain, and motoneuronal excitability in healthy people and people with Achilles tendinopathy. Clin J Sport Med. 2010;20:416-421 [DOI] [PubMed] [Google Scholar]
- 19. Flynn T, Fritz J, Whitman J, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine (Phila Pa 1976). 2002;27:2835-2843 [DOI] [PubMed] [Google Scholar]
- 20. Fritz JM, Childs JD, Flynn TW. Pragmatic application of a clinical prediction rule in primary care to identify patients with low back pain with a good prognosis following a brief spinal manipulation intervention. BMC Fam Pract. 2005;6:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. González-Iglesias J, Fernández-de-Las-Peñas C, Cleland JA, Huijbregts P, Del Rosario Gutiérrez-Vega M. Short-term effects of cervical Kinesio taping on pain and cervical range of motion in patients with acute whiplash injury: a randomized clinical trial. J Orthop Sports Phys Ther. 2009;39:515-521 [DOI] [PubMed] [Google Scholar]
- 22. Grindstaff TL, Hertel J, Beazell JR, Magrum EM, Ingersoll CD. Effects of lumbopelvic joint manipulation on quadriceps activation and strength in healthy individuals. Man Ther. 2009;14:415-420 [DOI] [PubMed] [Google Scholar]
- 23. Herrington L. The difference in a clinical measure of patella lateral position between individuals with patellofemoral pain and matched controls. J Orthop Sports Phys Ther. 2008;38:59-62 [DOI] [PubMed] [Google Scholar]
- 24. Herrington L, Hatcher J, Hatcher A, McNicholas M. A comparison of Star Excursion Balance Test reach distances between ACL deficient patients and asymptomatic controls. Knee. 2009;16:149-152 [DOI] [PubMed] [Google Scholar]
- 25. Hsu YH, Chen WY, Lin HC, Wang WT, Shih YF. The effects of taping on scapular kinematics and muscle performance in baseball players with shoulder impingement syndrome. J Electromyogr Kinesiol. 2009;19:1092-1099 [DOI] [PubMed] [Google Scholar]
- 26. Irene S, Davis CMP. Patellofemoral pain syndrome: proximal, distal, and local factors, an international retreat, April 30–May 2, 2009, Fells Point, Baltimore, MD. J Orthop Sports Phys Ther. 2009;40:A1-A48 [DOI] [PubMed] [Google Scholar]
- 27. Iverson CA, Sutlive TG, Crowell MS, et al. Lumbopelvic manipulation for the treatment of patients with patellofemoral pain syndrome: development of a clinical prediction rule. J Orthop Sports Phys Ther. 2008;38:297-312 [DOI] [PubMed] [Google Scholar]
- 28. Janwantanakul P, Gaogasigam C. Vastus lateralis and vastus medialis obliquus muscle activity during the application of inhibition and facilitation taping techniques. Clin Rehabil. 2005;19:12-19 [DOI] [PubMed] [Google Scholar]
- 29. Kase K. Clinical Therapeutic Applications of the Kinesio Taping Method. 2nd ed. Tokyo, Japan: Ken Ikai Co Ltd; 2003 [Google Scholar]
- 30. MacIntyre NJ, Hill NA, Fellows RA, Ellis RE, Wilson DR. Patellofemoral joint kinematics in individuals with and without patellofemoral pain syndrome. J Bone Joint Surg Am. 2006;88:2596-2605 [DOI] [PubMed] [Google Scholar]
- 31. Niemuth PE, Myers MJ, Thieman TJ. Hip muscle weakness and overuse injuries in recreational runners. Clin J Sports Med. 2005;15:14-21 [DOI] [PubMed] [Google Scholar]
- 32. Plisky PJ, Butler RJ, Kiesel KB, Underwood FB, Elkins B. The reliability of an instrumented device for measuring components of the Star Excursion Balance Test. N Am J Sports Phys Ther. 2009;4:92-99 [PMC free article] [PubMed] [Google Scholar]
- 33. Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36:911-919 [DOI] [PubMed] [Google Scholar]
- 34. Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39:12-19 [DOI] [PubMed] [Google Scholar]
- 35. Robinson RH. Support for a reduction in the number of trials needed for the Star Excursion Balance Test. Arch Phys Med Rehabil 2008;89:364-370 [DOI] [PubMed] [Google Scholar]
- 36. Rowe J, Shafer L, Kelley K, et al. Hip strength and knee pain in females. N Am J Sports Phys Ther. 2007;2:164-169 [PMC free article] [PubMed] [Google Scholar]
- 37. Souza RB, Powers CM. Predictors of hip internal rotation during running: an evaluation of hip strength and femoral structure in women with and without patellofemoral pain. Am J Sports Med. 2009;37:579-587 [DOI] [PubMed] [Google Scholar]
- 38. Suter E, McMorland G, Herzog W, Bray R. Decrease in quadriceps inhibition after sacroiliac joint manipulation in patients with anterior knee pain. J Manipulative Physiol Ther. 1999;22:149-153 [DOI] [PubMed] [Google Scholar]
- 39. Ota S, Nakashima T, Morisaka A, Ida K, Kawamura M. Comparison of patellar mobility in female adults with and without patellofemoral pain. J Orthop Sports Phys Ther. 2008;38:396-402 [DOI] [PubMed] [Google Scholar]
- 40. Thelen DJ, Stoneman PD. The clinical effcacy of Kinesio tape for shoulder pain: a randomized, double-blinded, clinical trial. J Orthop Sports Phys Ther. 2008;38:389-395 [DOI] [PubMed] [Google Scholar]
- 41. Thiago YF, Rossetto FM, Magalhães E, Bryk FF, Lucareli PR, de Almeida Aparecida Carvalho N. Short-term effects of hip abductors and lateral rotators strengthening in females with patellofemoral pain syndrome: a randomized controlled clinical trial. J Orthop Sports Phys Ther. 2010;40:736-742 [DOI] [PubMed] [Google Scholar]
- 42. Tieh-Cheng F, Wong AM, Pei YC, Wu KP, Chou SW, Lin YC. Effect of Kinesio taping on muscle strength in athletes: a pilot study. J Sci Med Sport. 2008;11:198-201 [DOI] [PubMed] [Google Scholar]
- 43. Tsung-Yu L, Ching-Chuan J, Chiang H. Immediate effect and predictors of effectiveness of taping for patellofemoral pain syndrome. Am J Sports Med. 2010;38:1626-1630 [DOI] [PubMed] [Google Scholar]
- 44. Waryasz GR, McDermott AY. Patellofemoral pain syndrome (PFPS): a systematic review of anatomy and potential risk factors. Dyn Med. 2008;7:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Yoshida A, Kahanov L. The effect of Kinesio taping on lower trunk range of motions. Res Sports Med. 2007;15:103-112 [DOI] [PubMed] [Google Scholar]