Abstract
Background
Although acupuncture is widely used for chronic pain, there remains considerable controversy as to its value. We aimed to determine the effect size of acupuncture for four chronic pain conditions: back and neck pain, osteoarthritis, chronic headache, and shoulder pain.
Methods
We conducted a systematic review to identify randomized trials of acupuncture for chronic pain where allocation concealment was determined unambiguously to be adequate. Individual patient data meta-analyses were conducted using data from 29 of 31 eligible trials, with a total of 17,922 patients analyzed.
Results
In the primary analysis including all eligible trials, acupuncture was superior to both sham and no acupuncture control for each pain condition (all p<0.001). After exclusion of an outlying set of trials that strongly favored acupuncture, the effect sizes were similar across pain conditions. Patients receiving acupuncture had less pain, with scores 0.23 (95% C.I. 0.13, 0.33), 0.16 (95% C.I. 0.07, 0.25) and 0.15 (95% C.I. 0.07, 0.24) standard deviations lower than sham controls for back and neck pain, osteoarthritis, and chronic headache respectively; the effect sizes in comparison to no acupuncture controls were 0.55 (95% C.I. 0.51, 0.58), 0.57 (95% C.I. 0.50, 0.64) and 0.42 (95% C.I. 0.37, 0.46). These results were robust to a variety of sensitivity analyses, including those related to publication bias.
Conclusions
Acupuncture is effective for the treatment of chronic pain and is therefore a reasonable referral option. Significant differences between true and sham acupuncture indicate that acupuncture is more than a placebo. However, these differences are relatively modest, suggesting that factors in addition to the specific effects of needling are important contributors to the therapeutic effects of acupuncture.
Introduction
Acupuncture is the insertion and stimulation of needles at specific points on the body to facilitate recovery of health. Although initially developed as part of traditional Chinese medicine, some contemporary acupuncturists, particularly those with medical qualifications, understand acupuncture in physiologic terms, without reference to pre-modern concepts1.
An estimated 3 million American adults receive acupuncture treatment each year2, and chronic pain is the most common presentation3. Acupuncture is known to have physiologic effects relevant to analgesia4, 5, but there is no accepted mechanism by which it could have persisting effects on chronic pain. This lack of biological plausibility, and its provenance in theories lying outside of biomedicine, makes acupuncture a highly controversial therapy.
A large number of randomized trials of acupuncture for chronic pain have been conducted. Most have been of low methodologic quality and, accordingly, meta-analyses based on these trials are of questionable interpretability and value6. Here we present an individual patient data meta-analysis of randomized trials of acupuncture for chronic pain, where only high quality trials were eligible for inclusion. Individual patient data meta-analysis is superior to the use of summary data in meta-analysis as it enhances data quality, enables different forms of outcome to be combined, and allows use of statistical techniques of increased precision.
Methods
The full protocol of the meta-analysis has been published.6 In brief, the study was conducted in three phases: identification of eligible trials; collection, checking and harmonization of raw data; individual patient data meta-analysis.
Data Sources and Searches
To identify papers, we searched MEDLINE, the Cochrane Collaboration Central Register of Controlled Trials and the citation lists of systematic reviews (full search strategy in Appendix). There were no language restrictions. The initial search, current to November 2008, was used to identify studies for the individual patient data meta-analysis; a second search was conducted in December 2010 for summary data to use in a sensitivity analysis.
Study Selection
Two reviewers applied inclusion criteria for potentially eligible papers separately, with disagreements about study inclusion resolved by consensus. Randomized trials were eligible for analysis if they included at least one group receiving acupuncture needling and one group receiving either sham (placebo) acupuncture or no acupuncture control. Trials must have accrued patients with one of four indications - non-specific back or neck pain, shoulder pain, chronic headache or osteoarthritis - with the additional criterion that the current episode of pain must be of at least four weeks duration for musculoskeletal disorders. There was no restriction on the type of outcome measure, although we specified that the primary endpoint must be measured more than four weeks after the initial acupuncture treatment.
It has been demonstrated that unconcealed allocation is the most important source of bias in randomized trials7 and, as such, we included only those trials where allocation concealment was determined unambiguously to be adequate (further detail in the review protocol6). Where necessary, we contacted authors for further information concerning the exact logistics of the randomization process. Trials were excluded if there was any ambiguity about allocation concealment.
Data Extraction and Quality Assessment
The principal investigator of eligible studies was contacted and asked to provide raw data from the trial. To ensure data accuracy, all results reported in the trial publication, including baseline characteristics and outcome data, were then replicated.
Reviewers assessed the quality of blinding for eligible trials with sham acupuncture control. Trials were graded as having a low likelihood of bias if either the adequacy of blinding was checked by direct questioning of patients (e.g. by use of a credibility questionnaire) and no important differences were found between groups, or the blinding method (e.g. the Streitberger sham device8) had previously been validated as able to maintain blinding. Trials with a high likelihood of bias from unblinding were excluded from the meta-analysis of acupuncture versus sham; a sensitivity analysis included only trials with a low risk of bias.
Data Synthesis and Analysis
Each trial was reanalyzed by analysis of covariance with the standardized principal endpoint (scores divided by pooled standard deviation) as the dependent variable, with the baseline measure of the principal endpoint and variables used to stratify randomization as covariates. This approach has been shown to have the greatest statistical power for trials with baseline and follow-up measures.9, 10 The effect size for acupuncture from each trial was then entered into a meta-analysis using the metan command in Stata 11 (Stata Corp., College Station, TX): the meta-analytic statistics were created by weighting each coefficient by the reciprocal of the variance, summing and dividing by the sum of the weights. Meta-analyses were conducted separately for comparisons of acupuncture with sham and no acupuncture control, and within each pain type. We pre-specified that the hypothesis test would be based on the fixed effects analysis as this constitutes a valid test of the null hypothesis of no treatment effect.
Results
Systematic review
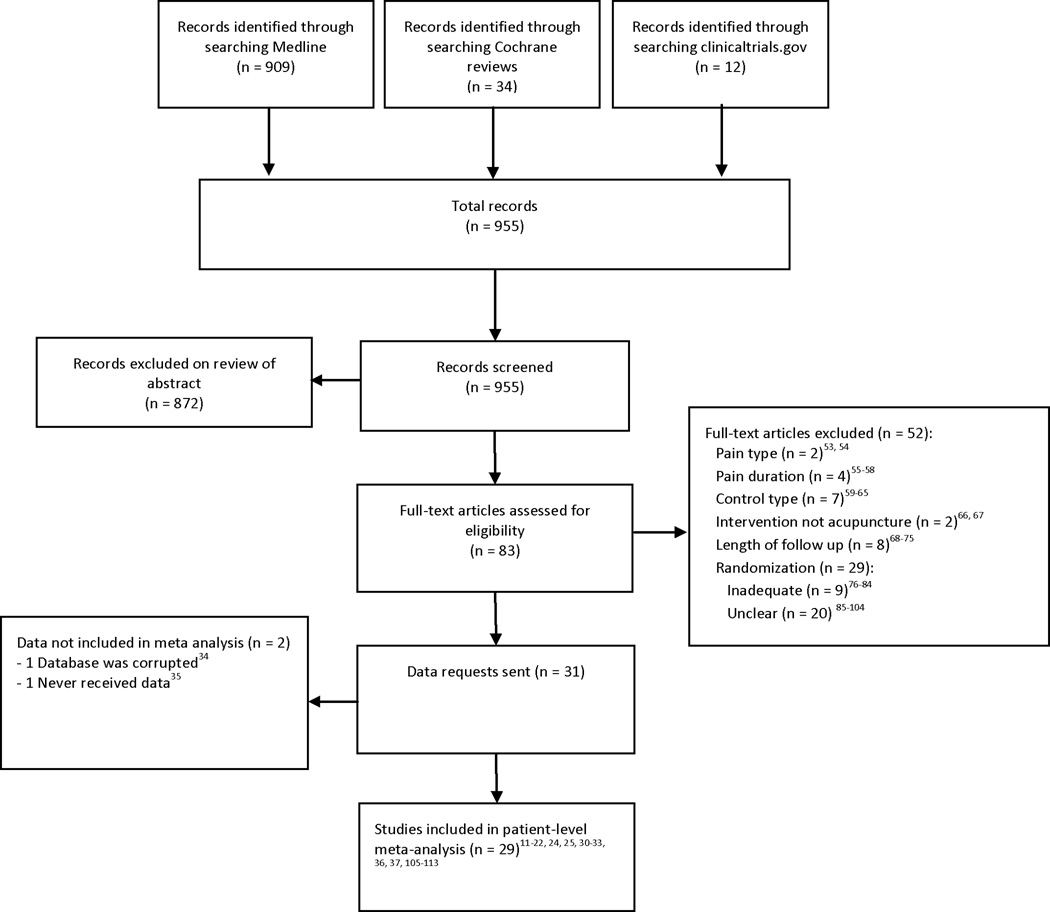
We identified 82 trials (see figure 1 for flowchart) of which 31 were eligible (Table 1 and Appendix online). Four of the studies were organized as part of the German Acupuncture Trials (GERAC) initiative11–14, 4 were part of the Acupuncture Randomized Trials (ART) group15–18; 4 were Acupuncture in Routine Care (ARC) studies19–22; 3 were UK National Health Service acupuncture trials23–25. Eleven studies were sham controlled, 10 had no acupuncture control and 10 were three-armed studies including both sham and no acupuncture control. The second search for subsequently published studies identified an additional four eligible studies26–29, with a total of 1,619 patients.
Figure 1.
PRISMA Flow Diagram
Table 1. Characteristics of included studies (Trial level information is provided in the Appendix).
The table includes the 31 trials identified in the initial search plus the four recently identified trials for which summary data were used.
| Indication n=35 | Pain Type | Control group | Primary Outcome Measure | Time point |
|---|---|---|---|---|
| Chronic headache n=7 | Migraine n=213, 18 Tension-type headache n=314, 16, 34 Both n=221, 53 |
Sham n=413, 14, 16, 18 No acupuncture control n=6 Ancillary care* n=134 Usual care^ n=416, 18, 21, 53 Guidelined care# n=113 |
Severity score n=234, 53 Days with headache n=114 Migraine days n=313, 16, 21 Days with moderate to severe pain n=118 |
1 month n=134 3 months n=316, 18, 21 6 months n=213, 14 12 months n=153 |
| Non-specific Musculoskeletal Pain (back and neck) n=15 | Back n=1012, 15, 19, 24, 28, 35–37, 54, 55 Neck n=520, 31, 32, 56, 57 |
Sham n=1012, 15, 28, 31, 32, 35–37, 54, 57 No acupuncture control n=9 Ancillary care* n=135 Usual care^ n=615, 19, 20, 24, 28, 56 Non specific advice§ n=155 Guidelined care# n=112 |
VAS n=715, 31, 32, 35–37, 57 Roland Morris Disability Questionnaire n=328, 54, 55 Neck Pain and Disability n=120 Hannover Functional Questionnaire n=119 Northwick Park Neck Pain Questionnaire n=156 Von Korff pain score n=112 SF36 Bodily pain n=124 |
1 month n=431, 32, 36, 57 2 months n=315, 28, 55 3 months n=519, 20, 26, 29, 35, 54, 56 6 months n=212, 37 24 months n=124 |
| Osteoarthritis n=9 | Sham n=611, 17, 25, 26, 33, 58 No acupuncture control n=8 Ancillary care* n=211, 25, 26 Usual care^ n=417, 22, 29 Non specific advice§ n=233, 59 |
Oxford Knee Score questionnaire n=159 Western Ontario and McMaster Universities Arthritis Index (WOMAC) n=217, 22 WOMAC pain subscore n=611, 25, 26, 29, 33, 58 |
2 months n=217, 59 3 months n=422, 26, 29, 58 6 months n=311, 25, 33 |
|
| Shoulder pain n=4 | Sham n=427, 30, 60, 61 No acupuncture control n=1 Usual care^ n=127 |
Constant-Murley-score n=230, 61 VAS n=227, 60 |
1 month n=230, 61 6 months n=227, 60 |
Ancillary care: Program of care received by both acupuncture and non acupuncture groups (e.g. trial comparing physiotherapy plus acupuncture to physiotherapy alone)
Usual care: Protocol did not specify treatments received in control group (e.g. trials with `waiting list control’)
Non specific advice: Patients in control group receive general advice and support (‘attention control’).
Guidelined care: Patients in control group received care according to national guidelines
An important source of clinical heterogeneity between studies concerns the control groups. In the sham controlled trials, the type of sham included acupuncture needles inserted superficially13, sham acupuncture devices with needles that retract into the handle rather than penetrate the skin30 and non-needle approaches such as deactivated electrical stimulation31 or detuned laser32. Moreover, co-interventions varied, with no additional treatment other than analgesics in some trials15, whereas in other trials, both acupuncture and sham groups received a course of additional treatment, such as exercise led by physical therapists25. Similarly, the no acupuncture control groups varied between usual care, such as a trial in which control group patients were merely advised to “avoid acupuncture”23; attention control, such as group education sessions33; and guidelined care, where patients were given advice as to specific drugs and doses13.
Data extraction and quality assessment
Usable raw data were obtained from 29 of the 31 eligible trials, including a total of 17,922 patients from the US, UK, Germany, Spain and Sweden. For one trial, the study database had become corrupted34; in another case, the statisticians involved in the trial failed to respond to repeated enquiries despite approval for data sharing being obtained from the principal investigator35.
The 29 trials comprised 18 comparisons with 14,597 patients of acupuncture with no acupuncture group and 20 comparisons with 5,230 patients of acupuncture and sham acupuncture. Patients in all trials had access to analgesics and other standard treatments for pain. Four sham-controlled trials were determined to have an intermediate likelihood of bias from unblinding13, 32, 36, 37; the 16 remaining sham-controlled trials were graded as having a low risk of bias from unblinding. On average, drop-out rates were low (weighted mean 10%). Drop-out rates were only above 25% for four trials: Molsberger 200235 and 201027 (33% and 27%, but raw data not received and neither trial included in main analysis); Carlsson 200137 (46%, trial excluded in a sensitivity analysis for blinding) and Berman 200433 (31%). This had a high drop-out rate amongst no acupuncture controls (43%); drop-out rates were close to 25% in the acupuncture and sham groups. The Kerr trial had a large difference in drop-out rates between groups (acupuncture 13%, control 33%) but was excluded in the sensitivity analysis for blinding36.
Meta-analysis
Forest plots for acupuncture against sham acupuncture and against no acupuncture control are shown separately for each of the four pain conditions in figures 2 and 3. Meta-analytic statistics are shown in table 2. Acupuncture was statistically superior to control for all analyses (p<0.001). Effect sizes are larger for the comparison between acupuncture and no acupuncture control than for the comparison between acupuncture and sham: 0.37, 0.26 and 0.15 in comparison with sham versus 0.55, 0.57 and 0.42 in comparison with no acupuncture control for musculoskeletal pain, osteoarthritis and chronic headache respectively.
Figure 2.
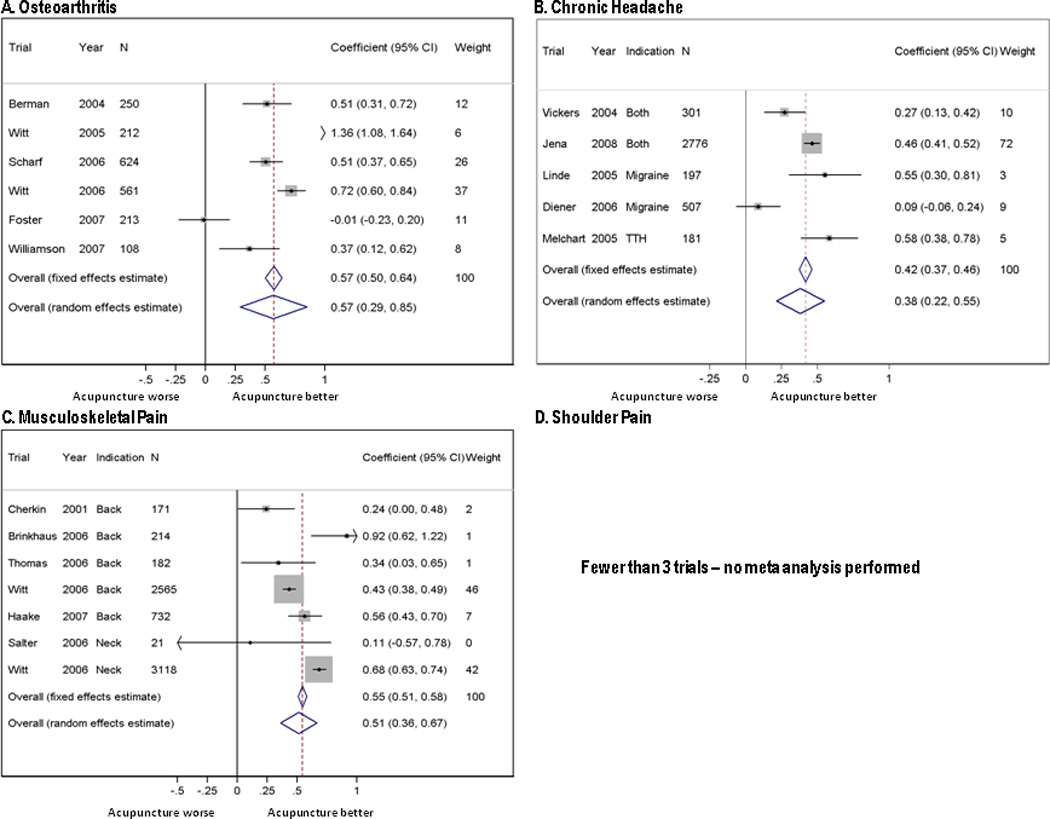
Forest plots for the comparison of acupuncture with no acupuncture control.
Figure 3.
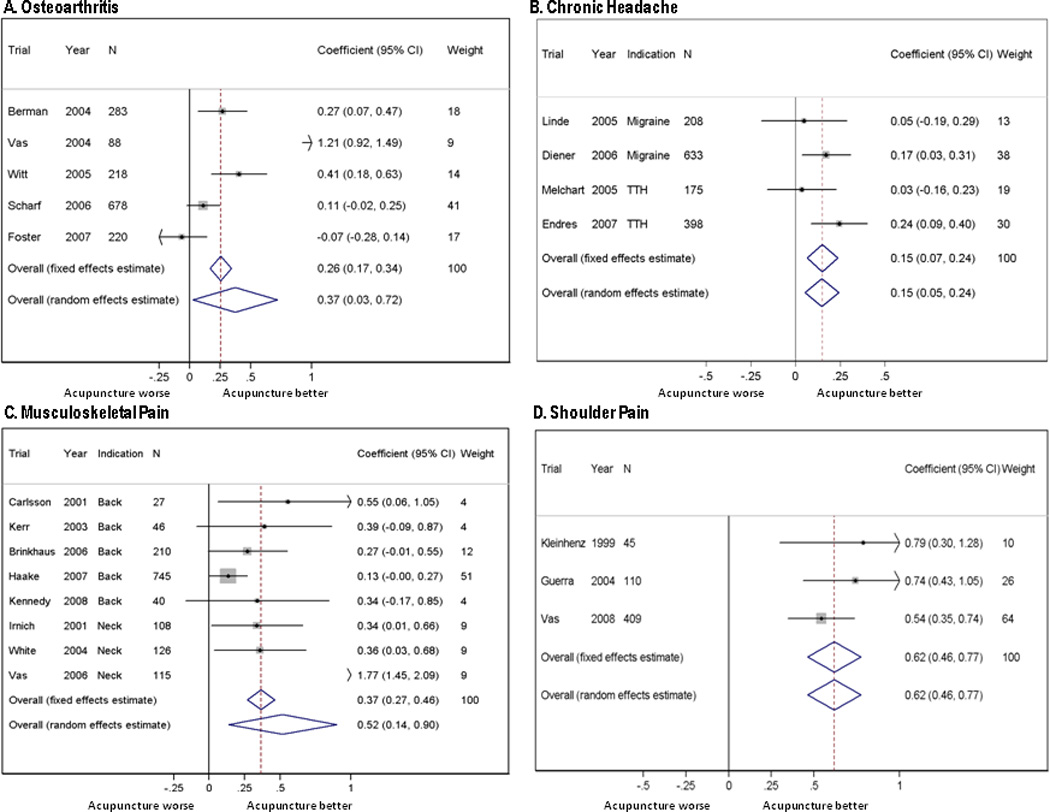
Forest plots for the comparison of true and sham acupuncture.
Table 2. Primary analyses.
Effect sizes are standardized differences.
| Acupuncture vs. Sham acupuncture | Acupuncture vs. no acupuncture control | |||||||
|---|---|---|---|---|---|---|---|---|
| N | Fixed effects (95%CI) |
Random effects (95%CI) |
P value for overall effect |
N | Fixed effects (95%CI) | Random effects (95%CI) |
P value for overall effect |
|
| Non-specific musculoskeletal pain (back and neck) | 8 | 0.37 (0.27, 0.46) Heterogeneity: p<0.001 |
0.52 (0.14, 0.90) | p<0.001 | 7 | 0.55(0.51, 0.58) Heterogeneity: p<0.001 |
0.51 (0.36, 0.67) | p<0.001 |
| Osteoarthritis | 5 | 0.26 (0.17, 0.34) Heterogeneity p<0.001 |
0.37 (0.03, 0.72) | p<0.001 | 6 | 0.57 (0.50, 0.64) Heterogeneity: p<0.001 |
0.57 (0.29, 0.85) | p<0.001 |
| Chronic headache | 4 | 0.15 (0.07, 0.24) Heterogeneity: p=0.3 |
0.15 (0.05, 0.24) | p<0.001 | 5 | 0.42 (0.37, 0.46) Heterogeneity: p<0.001 |
0.38 (0.22, 0.55) | p<0.001 |
| Shoulder pain | 3 | 0.62 (0.46, 0.77) Heterogeneity: p=0.4 |
0.62 (0.46, 0.77) | p<0.001 | 0 | No trials | ||
For five of the seven analyses, the test for heterogeneity was statistically significant. In the case of comparisons with sham acupuncture, the trials by Vas et al are clear outliers. For example, the effect size of the Vas trial for neck pain is about 5 times greater than meta-analytic estimate. One effect of excluding these trials in a sensitivity analysis (table 3) is that there is no significant heterogeneity in the comparisons between acupuncture and sham. Moreover, the effect size for acupuncture becomes relatively similar for the different pain conditions: 0.23, 0.16 and 0.15 against sham, and 0.55, 0.57 and 0.42 against no acupuncture control for back and neck pain, osteoarthritis, and chronic headache respectively (fixed effects; results similar for the random effects analysis).
Table 3. Sensitivity analyses.
Effect sizes are standardized differences.
| Indication | Acupuncture vs. Sham acupuncture | Acupuncture vs. no acupuncture control | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Fixed effects (95%CI) | Random effects (95%CI) |
P value for overall effect |
N | Fixed effects (95%CI) | Random effects (95%CI) |
P value for overall effect |
||
| Exclusion of Vas trials | Non-specific musculoskeletal pain | 7 | 0.23 (0.13, 0.33) Heterogeneity: p=0.5 |
0.23 (0.13, 0.33) | p<0.001 | Not applicable | |||
| Osteoarthritis | 4 | 0.16 (0.07, 0.25) Heterogeneity: p=0.15 |
0.17 (0.00, 0.35) | p<0.001 | |||||
| Shoulder pain | Fewer than 3 trials | ||||||||
| Separate pain types | Back pain | 5 | 0.20 (0.09, 0.31) Heterogeneity: p=0.4 |
0.20 (0.09, 0.32) | p<0.001 | 5 | 0.46 (0.40, 0.51) Heterogeneity: p=0.004 |
0.49 (0.33, 0.64) | p<0.001 |
| Neck Pain | 3 | 0.83 (0.64, 1.01) Heterogeneity: p<0.001 |
0.82 (−0.11, 1.75) | p<0.001 | No trials | ||||
| Inclusion of trials for which raw data not obtained | Non-specific musculoskeletal pain | 10 | 0.30 (.21, 0.38) Heterogeneity: p<0.001 |
0.48 (0.14, 0.81) | p<0.001 | 9 | 0.55 (0.51, 0.58) Heterogeneity: p<0.001 |
0.57 (0.42, 0.71) | p<0.001 |
| Osteoarthritis | 6 | 0.22 (0.14, 0.30) Heterogeneity p<0.001 |
0.31 (0.02, 0.60) | p<0.001 | 8 | 0.58 (0.51, 0.64) Heterogeneity: p<0.001 |
0.57 (0.33, 0.80) | p<0.001 | |
| Chronic headache | No trials | 6 | 0.42 (0.38, 0.47) Heterogeneity: p<0.001 |
0.41 (0.25, 0.56) | p<0.001 | ||||
| Shoulder pain | 4 | 0.57 (0.44, 0.69) Heterogeneity: p= 0.4 |
0.57 (0.44, 0.69) | <0.001 | 1 | Fewer than 3 trials | |||
| Only trials with low likelihood of bias for blinding | Non-specific musculoskeletal pain | 5 | 0.36 (0.25,0.46) Heterogeneity: p<0.001 |
0.57 (0.00, 1.14) | p<0.001 | Not applicable | |||
| Osteoarthritis | As for table 2: all trials have a low likelihood of bias for blinding | ||||||||
| Chronic headache | 3 | 0.14 (0.03, 0.25) Heterogeneity: p=0.18 |
0.12 (−0.02, 0.27) | p=0.013 | |||||
| Shoulder pain | As for table 2: all trials have a low likelihood of bias for blinding | ||||||||
| Multiple imputation for missing data | Non-specific musculoskeletal pain | 8 | 0.36 (0.27, 0.46) Heterogeneity: p<0.001 |
0.52 (0.15, 0.88) | p<0.001 | 7 | 0.55 (0.51, 0.58) Heterogeneity: p<0.001 |
0.51 (0.36, 0.66) | p<0.001 |
| Osteoarthritis | 5 | 0.25 (0.16, 0.33) Heterogeneity: p<0.001 |
0.37 (0.03, 0.71) | p<0.001 | 6 | 0.57 (0.50, 0.64) Heterogeneity: p<0.001 |
0.57 (0.29, 0.85) | p<0.001 | |
| Chronic headache | 4 | 0.16 (0.07, 0.25) Heterogeneity: p=0.4 |
0.16 (0.07, 0.25) | p<0.001 | 5 | 0.42 (0.38, 0.46) Heterogeneity: p<0.001 |
0.38 (0.22, 0.55) | p<0.001 | |
| Shoulder pain | 3 | 0.62 (0.46, 0. 78) Heterogeneity: p=0.4 |
0.62 (0.46, 0.78) | p<0.001 | No trials | ||||
To give an example of what these effect sizes mean in real terms, baseline pain score on a 0 – 100 scale for a typical trial might be 60. Given a standard deviation of 25, follow-up scores might be 43 in a no acupuncture group, 35 in sham acupuncture and 30 in patients receiving true acupuncture. If response were defined in terms of a pain reduction of 50% or more, response rates would be approximately 30%, 42.5% and 50%, respectively.
The comparisons with no acupuncture control show evidence of heterogeneity. This appears largely explicable in terms of differences between the control groups used. In the case of osteoarthritis, the largest effect is for Witt 200517, where patients in the waiting list control received only rescue pain medication, and the smallest for Foster 200725, which involved a program of exercise and advice led by physical therapists. For the musculoskeletal analyses, heterogeneity is driven by two very large trials19, 20 (n=2565 and n=3118) for back and neck pain. If only back pain is considered (table 3), heterogeneity is dramatically reduced and is again driven by one trial, Brinkhaus 200615, with waiting list control. In the headache meta-analysis, Diener 200613 had much smaller differences between groups. This trial involved providing drug therapy according to national guidelines in the no acupuncture group, including initiation of beta-blockers as migraine prophylaxis. There was disagreement within the collaboration about whether this constituted active control. Excluding this trial reduced evidence of heterogeneity (p=0.04) but had little effect on the effect size (0.42 to 0.45).
Table 3 shows several pre-specified sensitivity analyses. Neither restricting the sham control trials to those with low likelihood of unblinding nor adjustment for missing data had any substantive effect on our main estimates. Inclusion of summary data from trials for which raw data were not obtained (2 trials) or which were published recently (4 trials) also had little impact on either the primary analysis (table 3) or the analysis with the outlying Vas trials excluded (data not shown).
To estimate the potential impact of publication bias, we entered all trials in to a single analysis and compared the effect sizes from small and large studies38. We saw some evidence that small studies had larger effect sizes for the comparison with sham (p=0.023) but not no acupuncture control (p=0.7). However, these analyses are influenced by the outlying Vas trials, which were smaller than average, and by indication, as the shoulder pain trials were small and had large effect sizes. Tests for asymmetry were non-significant when we excluded Vas and shoulder pain studies (n=15; p=0.065) and when small studies were also excluded(n<100, n=12; p=0.3). Nonetheless, we repeated our meta-analyses excluding trials with a sample size less than 100. This had essentially no effect on our results. As a further test of publication bias, we considered the possible effect on our analysis if we had failed to include high-quality, unpublished studies. Only if there were 47 unpublished trials with n=100 showing an advantage to sham of 0.25 standard deviations would the difference between acupuncture and sham lose significance.
A final sensitivity analysis examined the effect of pooling different endpoints measured at different periods of follow-up. We repeated our analyses including only pain endpoints measured at 2 – 3 months after randomization. There was no material effect on results: effect sizes increased by 0.05 to 0.09 SD for musculoskeletal and osteoarthritis trials and were stable otherwise.
As an exploratory analysis, we compared sham to no acupuncture control. In a meta-analysis of 9 trials11–13, 15–18, 25, 33, the effect size for sham was 0.33 (95% C.I. 0.27, 0.40) and 0.38 (95% C.I. 0.20, 0.56) for fixed and random effects models respectively (p<0.001 for tests of both effect and heterogeneity).
Comment
Overview of findings
In an analysis of patient-level data from 29 high quality randomized trials, including 17,922 patients, we found statistically significant differences between both acupuncture versus sham and acupuncture versus no acupuncture control for all pain types studied. After excluding an outlying set of studies, meta-analytic effect sizes were similar across pain conditions.
The effect size for individual trials comparing acupuncture to no acupuncture control did vary, an effect that appears at least partly explicable in terms of the type of control used. As might be expected, acupuncture had a smaller benefit in patients who received a program of ancillary care – such as physical therapist led exercise25 – than in patients who continued on usual care. Nonetheless, the average effect, as expressed in the meta-analytic estimate of approximately 0.5 standard deviations, is of clear clinical relevance whether considered either as a standardized difference39 or when converted back to a pain scale. The difference between acupuncture and sham is of lesser magnitude, 0.15 to 0.23 standard deviations.
Limitations
Neither study quality nor sample size appear to be a problem for this meta-analysis, on the grounds that only high quality studies were eligible and the total sample size is large. Moreover, we saw no evidence that publication bias, or failure to identify published eligible studies, could affect our conclusions.
As the comparisons between acupuncture and no acupuncture cannot be blinded, both performance and response bias are possible. Similarly, while we considered the risk of bias of unblinding low in most studies comparing acupuncture and sham acupuncture, providers obviously were aware of the treatment provided and, as such, a certain degree of bias of our effect estimate for specific effects cannot be entirely ruled out. However, it should be kept in mind that this problem applies to almost all studies on non-drug interventions. We would argue that the risk of bias in the comparison between acupuncture and sham acupuncture is low compared to other non-drug treatments for chronic pain, such as cognitive therapies, exercise or manipulation, which are rarely subject to placebo control.
Another possible critique is that the meta-analyses combined different endpoints, such as pain and function, measured at different times. However, results did not change when we restricted the analysis to pain endpoints measured at a specific follow-up time, 2 – 3 months after randomization.
Comparison with other studies
Many prior systematic reviews of acupuncture for chronic pain have had liberal eligibility criteria, accordingly included trials of low methodologic quality, and then came to the circular conclusion that weaknesses in the data did not allow conclusions to be drawn40, 41. Other reviews have not included meta-analyses, apparently due to variation in study endpoints42, 43. We have avoided both problems by including only high quality trials and obtaining raw data for individual patient data meta-analysis. Some more recent systematic reviews have published meta-analyses44–46 47 and reported findings that are broadly comparable to ours with clear differences between acupuncture and no treatment control and smaller differences between true and sham acupuncture. Our findings have greater precision: all prior reviews have analyzed summary data, an approach of reduced statistical precision when compared to individual patient data meta-analysis 6, 48. In particular, we have demonstrated a robust difference between acupuncture and sham control that can be distinguished from bias. This is a novel finding that moves beyond the prior literature.
Interpretation
We believe that our findings are both clinically and scientifically important. They suggest that the total effects of acupuncture, as experienced by the patient in routine clinical practice, are clinically relevant, but that an important part of these total effects is not due to issues considered to be crucial by most acupuncturists, such as the correct location of points and depth of needling. Several lines of argument suggest that acupuncture (whether real or sham) is associated with more potent placebo or context effects than other interventions49–52. Yet many clinicians would feel uncomfortable in providing or referring patients to acupuncture if it were merely a potent placebo. Similarly, it is questionable whether national or private health insurance should reimburse therapies that do not have specific effects. Our finding that acupuncture has effects over and above sham acupuncture is therefore of major importance for clinical practice. Even though on average these effects are small, the clinical decision made by doctors and patients is not between true and sham acupuncture, but between a referral to an acupuncturist or avoiding such a referral. The total effects of acupuncture, as experienced by the patient in routine practice, include both the specific effects associated with correct needle insertion according to acupuncture theory, non-specific physiologic effects of needling, and non-specific psychological (placebo) effects related to the patient’s belief that treatment will be effective.
Conclusion
We found acupuncture to be superior to both no acupuncture control and sham acupuncture for the treatment of chronic pain. Although the data indicate that acupuncture is more than a placebo, the differences between true and sham acupuncture are relatively modest, suggesting that factors in addition to the specific effects of needling are important contributors to therapeutic effects. Our results from individual patient data meta-analyses of nearly 18,000 randomized patients on high quality trials provide the most robust evidence to date that acupuncture is a reasonable referral option for patients with chronic pain.
Supplementary Material
Acknowledgments
Funding
The Acupuncture Trialists’ Collaboration is funded by an R21 (AT004189I from the National Center for Complementary and Alternative Medicine (NCCAM) at the National Institutes of Health (NIH) to Dr Vickers) and by a grant from the Samueli Institute. Dr MacPherson’s work has been supported in part by the UK National Institute for Health Research (NIHR) under its Programme Grants for Applied Research scheme (RP-PG-0707-10186). Eric Manheimer’s work on the Acupuncture Trialists’ Collaboration was supported by grant number R24 AT001293 from NCCAM The views expressed in this publication are those of the author(s) and not necessarily those of the NCCAM NHS, the NIHR or the Department of Health in England. No sponsor had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Appendix
The Acupuncture Trialists' Collaboration includes physicians, clinical trialists, biostatisticians, practicing acupuncturists and others. The list of collaborators is as follows.
Claire Allen is the consumer representative ('patient advocate'). Mrs Allen is the Deputy Administrator at the Cochrane Collaboration Secretariat.
Mac Beckner, MIS, is Vice President of the Information Technology and Data Management Center at the Samueli Institute.
Brian Berman, MD, is Professor of Family & Community Medicine at the University of Maryland School of Medicine and Director of the Center for Integrative Medicine.
Benno Brinkhaus, MD, is professor at the Institute for Social Medicine, Epidemiology and Health Economics, Charité - University Medical Center, Berlin, Germany.
Remy Coeytaux, MD, PhD, is Associate Professor, Community and Family Medicine, Duke University.
Angel M. Cronin, MS, is a biostatistician at the Dana-Farber Cancer Institute.
Hans-Christoph Diener, MD, PhD, is Professor of Neurology and Chairman of the Department of Neurology at the University of Duisburg-Essen, Germany.
Heinz G. Endres, MD, is a senior research assistant and lecturer at the Ruhr-University Bochum, Germany.
Nadine Foster, DPhil, BSc(Hons), is Professor of Musculoskeletal Health in Primary Care, Arthritis Research UK Primary Care Centre, Keele University, UK.
Juan Antonio Guerra de Hoyos, MD, is director of the Andalusian Integral Plan for Pain Management, coordinator of Andalusian Health Service Project for Improving Primary Care Research.
Michael Haake, MD, PhD is an orthopedic surgeon who directs the Department of Orthopedics and Traumatology of the SLK-Hospitals in Heilbronn, Germany.
Richard Hammerschlag, PhD, is the Emeritus Dean of Research at the Oregon College of Oriental Medicine in Portland, Oregon.
Dominik Irnich, MD, is head of the Interdisciplinary Pain Centre at the University of Munich, Germany.
Wayne B. Jonas, MD, is the president and chief executive officer of the Samueli institute.
Kai Kronfeld, PhD, is a clinical trialist at the Interdisciplinary Centre for Clinical Trials (IZKS Mainz), University Medical Centre Mainz, Germany.
Lixing Lao, PhD, is professor at the University of Maryland, and director of Traditional Chinese Medicine Research at the Center for Integrative Medicine at that institution.
George Lewith, MD, FRCP, is a Professor of Health Research directing the Complementary and Integrated Medicine Research Unit at Southampton Medical School, UK.
Klaus Linde, MD, is research coordinator at the Institute of General Practice, Technische Universität München.
Hugh MacPherson, PhD, is a Senior Research Fellow who heads the Complementary Medicine Research Group at the University of York, UK.
Eric Manheimer, MS, is a research associate at the University of Maryland School of Medicine Center for Integrative Medicine.
Alexandra Maschino, BS, is a data analyst at Memorial Sloan-Kettering Cancer Center.
Dieter Melchart, MD, PhD, is a Professor directing the Centre for Complementary Medicine Research (Znf) at the Technische Universität München.
Albrecht Molsberger, MD, PhD, Prof. is an orthopedic surgeon, a practicing acupuncturist and the president of the German acupuncture research group.
Karen J. Sherman, PhD, MPH, is Senior Scientific Investigator at the Group Health Research Institute, Seattle WA.
Hans Trampisch, PhD, Chair of the department of Medical Statistics and Epidemiology at Ruhr-University Bochum, Germany.
Jorge Vas, MD, PhD, is the Chief Medical Officer of the Pain Treatment Unit, Dos Hermanas Primary Care Health Center (Andalusia Public Health System), Spain.
Andrew J. Vickers (collaboration chair), DPhil, is Assistant Attending Research Methodologist at Memorial Sloan-Kettering Cancer Center.
Norbert Victor, PhD, is Professor Emeritus at the University of Heidelberg, where he was previously Chair of Medical Biometry, and Director of the Institute for Medical Biometry and Informatics.
Peter White, PhD, is a lecturer in research methodology at the School of Health Sciences, University of Southampton, UK.
Lyn Williamson, MD, MA (Oxon), MRCGP, FRCP, is Consultant Rheumatologist at the Great Western Hospital, Swindon, UK and Honorary Senior Lecturer in Clinical Medicine at Oxford University.
Stefan N. Willich, MD, MPH, MBA, is Professor and Director of the Institute for Social Medicine, Epidemiology and Health Economics, Charité University Medical Center, Berlin, Germany.
Claudia M. Witt, MD, MBA, is Professor for Complementary Medicine at the University Medical Center Charité and Vice Director of the Institute for Social Medicine, Epidemiology and Health Economics, Berlin, Germany.
Footnotes
Ethics statement
An ethics statement was not required for this work.
Conflicts of Interest
The authors declare that they have no competing interests.
Authors’ contributions
The study was conceived by AV, GL, CW, and KL. AV was responsible for the overall study design with input from AC for the statistical analysis; AM for the systematic review; GL and HM with respect to acupuncture analyses; NV, CW, NF, KS and KL with respect to clinical trial methodology and meta-analysis. Statistical analyses were conducted by AV, AC and AM. The first draft of the manuscript was written by AV and AM. All authors gave comments on early drafts and approved the final version of the manuscript. AV had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Contributor Information
Andrew J. Vickers, Memorial Sloan-Kettering Cancer Center, New York, NY.
Angel M. Cronin, Memorial Sloan-Kettering Cancer Center, New York, NY now at Dana-Farber Cancer Center, Boston, MA.
Alexandra C. Maschino, Memorial Sloan-Kettering Cancer Center, New York, NY.
George Lewith, University of Southampton, UK.
Hugh MacPherson, University of York, UK.
Norbert Victor, University of Heidelberg, Germany.
Nadine E. Foster, Keele University, UK.
Karen J. Sherman, Group Health Research Institute, Seattle, WA.
Claudia M. Witt, Charité Universitätsmedizin, Berlin Germany.
Klaus Linde, Technische Universität München, Germany.
References
- 1.White A. Western medical acupuncture: a definition. Acupunct Med. 2009;27(1):33–35. doi: 10.1136/aim.2008.000372. [DOI] [PubMed] [Google Scholar]
- 2.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008 Dec 10;(12):1–23. [PubMed] [Google Scholar]
- 3.Sherman KJ, Cherkin DC, Eisenberg DM, Erro J, Hrbek A, Deyo RA. The practice of acupuncture: who are the providers and what do they do? Ann Fam Med. 2005 Mar-Apr;3(2):151–158. doi: 10.1370/afm.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peets JM, Pomeranz B. CXBK mice deficient in opiate receptors show poor electroacupuncture analgesia. Nature. 1978 Jun 22;273(5664):675–676. doi: 10.1038/273675a0. [DOI] [PubMed] [Google Scholar]
- 5.Zhang WT, Jin Z, Luo F, Zhang L, Zeng YW, Han JS. Evidence from brain imaging with fMRI supporting functional specificity of acupoints in humans. Neurosci Lett. 2004 Jan 2;354(1):50–53. doi: 10.1016/j.neulet.2003.09.080. [DOI] [PubMed] [Google Scholar]
- 6.Vickers AJ, Cronin AM, Maschino AC, et al. Individual patient data meta-analysis of acupuncture for chronic pain: protocol of the Acupuncture Trialists' Collaboration. Trials. 2010;11:90. doi: 10.1186/1745-6215-11-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. Jama. 1995 Feb 1;273(5):408–412. doi: 10.1001/jama.273.5.408. [DOI] [PubMed] [Google Scholar]
- 8.Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998 Aug 1;352(9125):364–365. doi: 10.1016/S0140-6736(97)10471-8. [DOI] [PubMed] [Google Scholar]
- 9.Frison L, Pocock SJ. Repeated measures in clinical trials: analysis using mean summary statistics and its implications for design. Stat Med. 1992 Sep 30;11(13):1685–1704. doi: 10.1002/sim.4780111304. [DOI] [PubMed] [Google Scholar]
- 10.Vickers AJ. Statistical reanalysis of four recent randomized trials of acupuncture for pain using analysis of covariance. Clin J Pain. 2004 Sep-Oct;20(5):319–323. doi: 10.1097/00002508-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Scharf HP, Mansmann U, Streitberger K, et al. Acupuncture and knee osteoarthritis: a three-armed randomized trial. Ann Intern Med. 2006 Jul 4;145(1):12–20. doi: 10.7326/0003-4819-145-1-200607040-00005. [DOI] [PubMed] [Google Scholar]
- 12.Haake M, Muller HH, Schade-Brittinger C, et al. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007 Sep 24;167(17):1892–1898. doi: 10.1001/archinte.167.17.1892. [DOI] [PubMed] [Google Scholar]
- 13.Diener HC, Kronfeld K, Boewing G, et al. Efficacy of acupuncture for the prophylaxis of migraine: a multicentre randomised controlled clinical trial. Lancet Neurol. 2006 Apr;5(4):310–316. doi: 10.1016/S1474-4422(06)70382-9. [DOI] [PubMed] [Google Scholar]
- 14.Endres HG, Bowing G, Diener HC, et al. Acupuncture for tension-type headache: a multicentre, sham-controlled, patient-and observer-blinded, randomised trial. J Headache Pain. 2007 Oct;8(5):306–314. doi: 10.1007/s10194-007-0416-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brinkhaus B, Witt CM, Jena S, et al. Acupuncture in patients with chronic low back pain: a randomized controlled trial. Arch Intern Med. 2006 Feb 27;166(4):450–457. doi: 10.1001/archinte.166.4.450. [DOI] [PubMed] [Google Scholar]
- 16.Melchart D, Streng A, Hoppe A, et al. Acupuncture in patients with tension-type headache: randomised controlled trial. Bmj. 2005 Aug 13;331(7513):376–382. doi: 10.1136/bmj.38512.405440.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Witt C, Brinkhaus B, Jena S, et al. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet. 2005 Jul 9–15;366(9480):136–143. doi: 10.1016/S0140-6736(05)66871-7. [DOI] [PubMed] [Google Scholar]
- 18.Linde K, Streng A, Jurgens S, et al. Acupuncture for patients with migraine: a randomized controlled trial. Jama. 2005 May 4;293(17):2118–2125. doi: 10.1001/jama.293.17.2118. [DOI] [PubMed] [Google Scholar]
- 19.Witt CM, Jena S, Selim D, et al. Pragmatic Randomized Trial Evaluating the Clinical and Economic Effectiveness of Acupuncture for Chronic Low Back Pain. Am J Epidemiol. 2006 Jun 23;164(5):487–496. doi: 10.1093/aje/kwj224. [DOI] [PubMed] [Google Scholar]
- 20.Witt CM, Jena S, Brinkhaus B, Liecker B, Wegscheider K, Willich SN. Acupuncture for patients with chronic neck pain. Pain. 2006 Jun 13; doi: 10.1016/j.pain.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 21.Jena S, Witt CM, Brinkhaus B, Wegscheider K, Willich SN. Acupuncture in patients with headache. Cephalalgia. 2008 Sep;28(9):969–979. doi: 10.1111/j.1468-2982.2008.01640.x. [DOI] [PubMed] [Google Scholar]
- 22.Witt CM, Jena S, Brinkhaus B, Liecker B, Wegscheider K, Willich SN. Acupuncture in patients with osteoarthritis of the knee or hip: a randomized, controlled trial with an additional nonrandomized arm. Arthritis Rheum. 2006 Nov;54(11):3485–3493. doi: 10.1002/art.22154. [DOI] [PubMed] [Google Scholar]
- 23.Wonderling D, Vickers AJ, Grieve R, McCarney R. Cost effectiveness analysis of a randomised trial of acupuncture for chronic headache in primary care. Bmj. 2004 Mar 27;328(7442):747. doi: 10.1136/bmj.38033.896505.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thomas KJ, MacPherson H, Thorpe L, et al. Randomised controlled trial of a short course of traditional acupuncture compared with usual care for persistent non-specific low back pain. Bmj. 2006 Sep 23;333(7569):623. doi: 10.1136/bmj.38878.907361.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foster NE, Thomas E, Barlas P, et al. Acupuncture as an adjunct to exercise based physiotherapy for osteoarthritis of the knee: randomised controlled trial. Bmj. 2007 Sep 1;335(7617):436. doi: 10.1136/bmj.39280.509803.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suarez-Almazor ME, Looney C, Liu Y, et al. A randomized controlled trial of acupuncture for osteoarthritis of the knee: effects of patient-provider communication. Arthritis Care Res (Hoboken) 2010 Sep;62(9):1229–1236. doi: 10.1002/acr.20225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Molsberger AF, Schneider T, Gotthardt H, Drabik A. German Randomized Acupuncture Trial for chronic shoulder pain (GRASP) - a pragmatic, controlled, patient-blinded, multi-centre trial in an outpatient care environment. Pain. 2010 Oct;151(1):146–154. doi: 10.1016/j.pain.2010.06.036. [DOI] [PubMed] [Google Scholar]
- 28.Cherkin DC, Sherman KJ, Avins AL, et al. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009 May 11;169(9):858–866. doi: 10.1001/archinternmed.2009.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lansdown H, Howard K, Brealey S, MacPherson H. Acupuncture for pain and osteoarthritis of the knee: a pilot study for an open parallel-arm randomised controlled trial. BMC Musculoskelet Disord. 2009;10:130. doi: 10.1186/1471-2474-10-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kleinhenz J, Streitberger K, Windeler J, Gussbacher A, Mavridis G, Martin E. Randomised clinical trial comparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendinitis. Pain. 1999 Nov;83(2):235–241. doi: 10.1016/s0304-3959(99)00107-4. [DOI] [PubMed] [Google Scholar]
- 31.White P, Lewith G, Prescott P, Conway J. Acupuncture versus placebo for the treatment of chronic mechanical neck pain: a randomized, controlled trial. Ann Intern Med. 2004 Dec 21;141(12):911–919. doi: 10.7326/0003-4819-141-12-200412210-00007. [DOI] [PubMed] [Google Scholar]
- 32.Irnich D, Behrens N, Molzen H, et al. Randomised trial of acupuncture compared with conventional massage and "sham" laser acupuncture for treatment of chronic neck pain. Bmj. 2001 Jun 30;322(7302):1574–1578. doi: 10.1136/bmj.322.7302.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berman BM, Lao L, Langenberg P, Lee WL, Gilpin AM, Hochberg MC. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2004 Dec 21;141(12):901–910. doi: 10.7326/0003-4819-141-12-200412210-00006. [DOI] [PubMed] [Google Scholar]
- 34.Coeytaux RR, Kaufman JS, Kaptchuk TJ, et al. A randomized, controlled trial of acupuncture for chronic daily headache. Headache. 2005 Oct;45(9):1113–1123. doi: 10.1111/j.1526-4610.2005.00235.x. [DOI] [PubMed] [Google Scholar]
- 35.Molsberger AF, Mau J, Pawelec DB, Winkler J. Does acupuncture improve the orthopedic management of chronic low back pain--a randomized, blinded, controlled trial with 3 months follow up. Pain. 2002 Oct;99(3):579–587. doi: 10.1016/S0304-3959(02)00269-5. [DOI] [PubMed] [Google Scholar]
- 36.Kerr DP, Walsh DM, Baxter D. Acupuncture in the management of chronic low back pain: a blinded randomized controlled trial. Clin J Pain. 2003 Nov-Dec;19(6):364–370. doi: 10.1097/00002508-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 37.Carlsson CP, Sjolund BH. Acupuncture for chronic low back pain: a randomized placebo-controlled study with long-term follow-up. Clin J Pain. 2001 Dec;17(4):296–305. doi: 10.1097/00002508-200112000-00003. [DOI] [PubMed] [Google Scholar]
- 38.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997 Sep 13;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sloan J. Asking the obvious questions regarding patient burden. J Clin Oncol. 2002 Jan 1;20(1):4–6. doi: 10.1200/JCO.2002.20.1.4. [DOI] [PubMed] [Google Scholar]
- 40.Furlan AD, van Tulder MW, Cherkin DC, et al. Acupuncture and dry-needling for low back pain. Cochrane Database Syst Rev. 2005;(1):CD001351. doi: 10.1002/14651858.CD001351.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Green S, Buchbinder R, Hetrick S. Acupuncture for shoulder pain. Cochrane Database Syst Rev. 2005;(2):CD005319. doi: 10.1002/14651858.CD005319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.White AR, Ernst E. A systematic review of randomized controlled trials of acupuncture for neck pain. Rheumatology (Oxford) 1999 Feb;38(2):143–147. doi: 10.1093/rheumatology/38.2.143. [DOI] [PubMed] [Google Scholar]
- 43.Ezzo J, Hadhazy V, Birch S, et al. Acupuncture for osteoarthritis of the knee: a systematic review. Arthritis Rheum. 2001 Apr;44(4):819–825. doi: 10.1002/1529-0131(200104)44:4<819::AID-ANR138>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 44.Manheimer E, Cheng K, Linde K, et al. Acupuncture for peripheral joint osteoarthritis. Cochrane Database Syst Rev. 2010;(1):CD001977. doi: 10.1002/14651858.CD001977.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for tension-type headache. Cochrane Database Syst Rev. 2009;(1):CD007587. doi: 10.1002/14651858.CD007587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009;(1):CD001218. doi: 10.1002/14651858.CD001218.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Madsen MV, Gotzsche PC, Hrobjartsson A. Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups. Bmj. 2009;338:a3115. doi: 10.1136/bmj.a3115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Riley RD, Lambert PC, Abo-Zaid G. Meta-analysis of individual participant data: rationale, conduct, and reporting. Bmj. 2010;340:c221. doi: 10.1136/bmj.c221. [DOI] [PubMed] [Google Scholar]
- 49.Kaptchuk TJ, Stason WB, Davis RB, et al. Sham device v inert pill: randomised controlled trial of two placebo treatments. Bmj. 2006 Feb 18;332(7538):391–397. doi: 10.1136/bmj.38726.603310.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Linde K, Niemann K, Meissner K. Are sham acupuncture interventions more effective than (other) placebos? A re-analysis of data from the Cochrane review on placebo effects. Forsch Komplementmed. 2010 Oct;17(5):259–264. doi: 10.1159/000320374. [DOI] [PubMed] [Google Scholar]
- 51.Kaptchuk TJ. The placebo effect in alternative medicine: can the performance of a healing ritual have clinical significance? Ann Intern Med. 2002 Jun 4;136(11):817–825. doi: 10.7326/0003-4819-136-11-200206040-00011. [DOI] [PubMed] [Google Scholar]
- 52.Liu T, Yu C-P. Placebo Analgesia, Acupuncture and Sham Surgery. eCAM. 2010:1–6. doi: 10.1093/ecam/neq030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vickers AJ, Rees RW, Zollman CE, et al. Acupuncture for chronic headache in primary care: large, pragmatic, randomised trial. Bmj. 2004 Mar 27;328(7442):744. doi: 10.1136/bmj.38029.421863.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kennedy S, Baxter GD, Kerr DP, Bradbury I, Park J, McDonough SM. Acupuncture for acute non-specific low back pain: a pilot randomised non-penetrating sham controlled trial. Complement Ther Med. 2008 Jun;16(3):139–146. doi: 10.1016/j.ctim.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 55.Cherkin DC, Eisenberg D, Sherman KJ, et al. Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self-care education for chronic low back pain. Arch Intern Med. 2001 Apr 23;161(8):1081–1088. doi: 10.1001/archinte.161.8.1081. [DOI] [PubMed] [Google Scholar]
- 56.Salter GC, Roman M, Bland MJ, MacPherson H. Acupuncture for chronic neck pain: a pilot for a randomised controlled trial. BMC Musculoskelet Disord. 2006;7:99. doi: 10.1186/1471-2474-7-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vas J, Perea-Milla E, Mendez C, et al. Efficacy and safety of acupuncture for chronic uncomplicated neck pain: a randomised controlled study. Pain. 2006 Dec 15;126(1–3):245–255. doi: 10.1016/j.pain.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 58.Vas J, Mendez C, Perea-Milla E, et al. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomised controlled trial. Bmj. 2004 Nov 20;329(7476):1216. doi: 10.1136/bmj.38238.601447.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Williamson L, Wyatt MR, Yein K, Melton JT. Severe knee osteoarthritis: a randomized controlled trial of acupuncture, physiotherapy (supervised exercise) and standard management for patients awaiting knee replacement. Rheumatology (Oxford) 2007 Sep;46(9):1445–1449. doi: 10.1093/rheumatology/kem119. [DOI] [PubMed] [Google Scholar]
- 60.Guerra de Hoyos JA, Andres Martin Mdel C, Bassas y Baena de Leon E, et al. Randomised trial of long term effect of acupuncture for shoulder pain. Pain. 2004 Dec;112(3):289–298. doi: 10.1016/j.pain.2004.08.030. [DOI] [PubMed] [Google Scholar]
- 61.Vas J, Ortega C, Olmo V, et al. Single-point acupuncture and physiotherapy for the treatment of painful shoulder: a multicentre randomized controlled trial. Rheumatology (Oxford) 2008 Jun;47(6):887–893. doi: 10.1093/rheumatology/ken040. [DOI] [PubMed] [Google Scholar]
- 62.Zheng Z, Guo RJ, Helme RD, Muir A, Da Costa C, Xue CC. The effect of electroacupuncture on opioid-like medication consumption by chronic pain patients: a pilot randomized controlled clinical trial. Eur J Pain. 2008 Jul;12(5):671–676. doi: 10.1016/j.ejpain.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 63.Coan RM, Wong G, Coan PL. The acupuncture treatment of neck pain: a randomized controlled study. Am J Chin Med. 1981 Winter;9(4):326–332. doi: 10.1142/s0192415x81000433. [DOI] [PubMed] [Google Scholar]
- 64.Franca DL, Senna-Fernandes V, Cortez CM, Jackson MN, Bernardo-Filho M, Guimaraes MA. Tension neck syndrome treated by acupuncture combined with physiotherapy: a comparative clinical trial (pilot study) Complement Ther Med. 2008 Oct;16(5):268–277. doi: 10.1016/j.ctim.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 65.Ezzo J, Vickers A, Richardson MA, et al. Acupuncture-point stimulation for chemotherapy-induced nausea and vomiting. J Clin Oncol. 2005 Oct 1;23(28):7188–7198. doi: 10.1200/JCO.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 66.He D, Veiersted KB, Hostmark AT, Medbo JI. Effect of acupuncture treatment on chronic neck and shoulder pain in sedentary female workers: a 6-month and 3-year follow-up study. Pain. 2004 Jun;109(3):299–307. doi: 10.1016/j.pain.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 67.Razavi M, Jansen GB. Effects of acupuncture and placebo TENS in addition to exercise in treatment of rotator cuff tendinitis. Clin Rehabil. 2004 Dec;18(8):872–878. doi: 10.1191/0269215504cr849oa. [DOI] [PubMed] [Google Scholar]
- 68.Grant DJ, Bishop-Miller J, Winchester DM, Anderson M, Faulkner S. A randomized comparative trial of acupuncture versus transcutaneous electrical nerve stimulation for chronic back pain in the elderly. Pain. 1999 Jul;82(1):9–13. doi: 10.1016/S0304-3959(99)00027-5. [DOI] [PubMed] [Google Scholar]
- 69.Itoh K, Katsumi Y, Kitakoji H. Trigger point acupuncture treatment of chronic low back pain in elderly patients--a blinded RCT. Acupunct Med. 2004 Dec;22(4):170–177. doi: 10.1136/aim.22.4.170. [DOI] [PubMed] [Google Scholar]
- 70.Johansson KM, Adolfsson LE, Foldevi MO. Effects of acupuncture versus ultrasound in patients with impingement syndrome: randomized clinical trial. Phys Ther. 2005 Jun;85(6):490–501. [PubMed] [Google Scholar]
- 71.Streng A, Linde K, Hoppe A, et al. Effectiveness and tolerability of acupuncture compared with metoprolol in migraine prophylaxis. Headache. 2006 Nov-Dec;46(10):1492–1502. doi: 10.1111/j.1526-4610.2006.00598.x. [DOI] [PubMed] [Google Scholar]
- 72.David J, Modi S, Aluko AA, Robertshaw C, Farebrother J. Chronic neck pain: a comparison of acupuncture treatment and physiotherapy. Br J Rheumatol. 1998 Oct;37(10):1118–1122. doi: 10.1093/rheumatology/37.10.1118. [DOI] [PubMed] [Google Scholar]
- 73.Ga H, Choi JH, Park CH, Yoon HJ. Acupuncture needling versus lidocaine injection of trigger points in myofascial pain syndrome in elderly patients--a randomised trial. Acupunct Med. 2007 Dec;25(4):130–136. doi: 10.1136/aim.25.4.130. [DOI] [PubMed] [Google Scholar]
- 74.Ng MM, Leung MC, Poon DM. The effects of electro-acupuncture and transcutaneous electrical nerve stimulation on patients with painful osteoarthritic knees: a randomized controlled trial with follow-up evaluation. J Altern Complement Med. 2003 Oct;9(5):641–649. doi: 10.1089/107555303322524490. [DOI] [PubMed] [Google Scholar]
- 75.Melchart D, Hager S, Hager U, Liao J, Weidenhammer W, Linde K. Treatment of patients with chronic headaches in a hospital for traditional Chinese medicine in Germany. A randomised, waiting list controlled trial. Complement Ther Med. 2004 Jun-Sep;12(2–3):71–78. doi: 10.1016/j.ctim.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 76.Weiner DK, Rudy TE, Morone N, Glick R, Kwoh CK. Efficacy of periosteal stimulation therapy for the treatment of osteoarthritis-associated chronic knee pain: an initial controlled clinical trial. J Am Geriatr Soc. 2007 Oct;55(10):1541–1547. doi: 10.1111/j.1532-5415.2007.01314.x. [DOI] [PubMed] [Google Scholar]
- 77.Inoue M, Kitakoji H, Ishizaki N, et al. Relief of low back pain immediately after acupuncture treatment--a randomised, placebo controlled trial. Acupunct Med. 2006 Sep;24(3):103–108. doi: 10.1136/aim.24.3.103. [DOI] [PubMed] [Google Scholar]
- 78.Nabeta T, Kawakita K. Relief of chronic neck and shoulder pain by manual acupuncture to tender points--a sham-controlled randomized trial. Complement Ther Med. 2002 Dec;10(4):217–222. doi: 10.1016/s0965-2299(02)00082-1. [DOI] [PubMed] [Google Scholar]
- 79.Berry H, Fernandes L, Bloom B, Clark RJ, Hamilton EB. Clinical study comparing acupuncture, physiotherapy, injection and oral anti-inflammatory therapy in shoulder-cuff lesions. Curr Med Res Opin. 1980;7(2):121–126. doi: 10.1185/03007998009112038. [DOI] [PubMed] [Google Scholar]
- 80.Fernandes L, Berry N, Clark RJ, Bloom B, Hamilton EB. Clinical study comparing acupuncture, physiotherapy, injection, and oral anti-inflammatory therapy in shoulder-cuff lesions. Lancet. 1980 Jan 26;1(8161):208–209. doi: 10.1016/s0140-6736(80)90696-0. [DOI] [PubMed] [Google Scholar]
- 81.Moore ME, Berk SN. Acupuncture for chronic shoulder pain. An experimental study with attention to the role of placebo and hypnotic susceptibility. Ann Intern Med. 1976 Apr;84(4):381–384. doi: 10.7326/0003-4819-84-4-381. [DOI] [PubMed] [Google Scholar]
- 82.Ma T, Kao MJ, Lin IH, et al. A study on the clinical effects of physical therapy and acupuncture to treat spontaneous frozen shoulder. Am J Chin Med. 2006;34(5):759–775. doi: 10.1142/S0192415X06004272. [DOI] [PubMed] [Google Scholar]
- 83.Giles LG, Muller R. Chronic spinal pain syndromes: a clinical pilot trial comparing acupuncture, a nonsteroidal anti-inflammatory drug, and spinal manipulation. J Manipulative Physiol Ther. 1999 Jul-Aug;22(6):376–381. doi: 10.1016/s0161-4754(99)70082-5. [DOI] [PubMed] [Google Scholar]
- 84.Melchart D, Thormaehlen J, Hager S, Liao J, Linde K, Weidenhammer W. Acupuncture versus placebo versus sumatriptan for early treatment of migraine attacks: a randomized controlled trial. J Intern Med. 2003 Feb;253(2):181–188. doi: 10.1046/j.1365-2796.2003.01081.x. [DOI] [PubMed] [Google Scholar]
- 85.Coan RM, Wong G, Ku SL, et al. The acupuncture treatment of low back pain: a randomized controlled study. Am J Chin Med. 1980 Spring-Summer;8(1–2):181–189. doi: 10.1142/s0192415x80000141. [DOI] [PubMed] [Google Scholar]
- 86.Christensen BV, Iuhl IU, Vilbek H, Bulow HH, Dreijer NC, Rasmussen HF. Acupuncture treatment of severe knee osteoarthrosis. A long-term study. Acta Anaesthesiol Scand. 1992 Aug;36(6):519–525. doi: 10.1111/j.1399-6576.1992.tb03511.x. [DOI] [PubMed] [Google Scholar]
- 87.Molsberger A, Bowing G, Jensen KU, Lorek M. Acupuncture treatment for the relief of gonarthrosis pain-a controlled clinical trial. Schmerz. 1994 Mar;8(1):37–42. doi: 10.1007/BF02527508. [DOI] [PubMed] [Google Scholar]
- 88.Linde M, Fjell A, Carlsson J, Dahlof C. Role of the needling per se in acupuncture as prophylaxis for menstrually related migraine: a randomized placebo-controlled study. Cephalalgia. 2005 Jan;25(1):41–47. doi: 10.1111/j.1468-2982.2004.00803.x. [DOI] [PubMed] [Google Scholar]
- 89.Muller R, Giles LG. Long-term follow-up of a randomized clinical trial assessing the efficacy of medication, acupuncture, and spinal manipulation for chronic mechanical spinal pain syndromes. J Manipulative Physiol Ther. 2005 Jan;28(1):3–11. doi: 10.1016/j.jmpt.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 90.Sator-Katzenschlager SM, Scharbert G, Kozek-Langenecker SA, et al. The short- and long-term benefit in chronic low back pain through adjuvant electrical versus manual auricular acupuncture. Anesth Analg. 2004 May;98(5):1359–1364. doi: 10.1213/01.ane.0000107941.16173.f7. table of contents. [DOI] [PubMed] [Google Scholar]
- 91.Karst M, Reinhard M, Thum P, Wiese B, Rollnik J, Fink M. Needle acupuncture in tension-type headache: a randomized, placebo-controlled study. Cephalalgia. 2001 Jul;21(6):637–642. doi: 10.1046/j.1468-2982.2001.00198.x. [DOI] [PubMed] [Google Scholar]
- 92.Ceccheerelli F, Bordin M, Gagliardi G, Caravello M. Comparison between superficial and deep acupuncture in the treatment of the shoulder's myofascial pain: a randomized and controlled study. Acupunct Electrother Res. 2001;26(4):229–238. doi: 10.3727/036012901816355938. [DOI] [PubMed] [Google Scholar]
- 93.Ceccherelli F, Rigoni MT, Gagliardi G, Ruzzante L. Comparison of superficial and deep acupuncture in the treatment of lumbar myofascial pain: a double-blind randomized controlled study. Clin J Pain. 2002 May-Jun;18(3):149–153. doi: 10.1097/00002508-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 94.Naprienko MV, Oknin V, Kremenchugskaia MR, Filatova EG. Use of acupuncture in the therapy of chronic daily headache. Zh Nevrol Psikhiatr Im S S Korsakova. 2003;103(10):40–44. [PubMed] [Google Scholar]
- 95.Leibing E, Leonhardt U, Koster G, et al. Acupuncture treatment of chronic low-back pain -- a randomized, blinded, placebo-controlled trial with 9-month follow-up. Pain. 2002 Mar;96(1–2):189–196. doi: 10.1016/s0304-3959(01)00444-4. [DOI] [PubMed] [Google Scholar]
- 96.Meng CF, Wang D, Ngeow J, Lao L, Peterson M, Paget S. Acupuncture for chronic low back pain in older patients: a randomized, controlled trial. Rheumatology (Oxford) 2003 Dec;42(12):1508–1517. doi: 10.1093/rheumatology/keg405. [DOI] [PubMed] [Google Scholar]
- 97.Berman BM, Singh BB, Lao L, et al. A randomized trial of acupuncture as an adjunctive therapy in osteoarthritis of the knee. Rheumatology (Oxford) 1999 Apr;38(4):346–354. doi: 10.1093/rheumatology/38.4.346. [DOI] [PubMed] [Google Scholar]
- 98.Takeda W, Wessel J. Acupuncture for the treatment of pain of osteoarthritic knees. Arthritis Care Res. 1994 Sep;7(3):118–122. doi: 10.1002/art.1790070304. [DOI] [PubMed] [Google Scholar]
- 99.Tukmachi E, Jubb R, Dempsey E, Jones P. The effect of acupuncture on the symptoms of knee osteoarthritis--an open randomised controlled study. Acupunct Med. 2004 Mar;22(1):14–22. doi: 10.1136/aim.22.1.14. [DOI] [PubMed] [Google Scholar]
- 100.Itoh K, Hirota S, Katsumi Y, Ochi H, Kitakoji H. A pilot study on using acupuncture and transcutaneous electrical nerve stimulation (TENS) to treat knee osteoarthritis (OA) Chin Med. 2008;3:2. doi: 10.1186/1749-8546-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Alecrim-Andrade J, Maciel-Junior JA, Carne X, Severino Vasconcelos GM, Correa-Filho HR. Acupuncture in migraine prevention: a randomized sham controlled study with 6-months posttreatment follow-up. Clin J Pain. 2008 Feb;24(2):98–105. doi: 10.1097/AJP.0b013e3181590d66. [DOI] [PubMed] [Google Scholar]
- 102.Alecrim-Andrade J, Maciel-Junior JA, Cladellas XC, Correa-Filho HR, Machado HC. Acupuncture in migraine prophylaxis: a randomized sham-controlled trial. Cephalalgia. 2006 May;26(5):520–529. doi: 10.1111/j.1468-2982.2006.01062.x. [DOI] [PubMed] [Google Scholar]
- 103.Giles LG, Muller R. Chronic spinal pain: a randomized clinical trial comparing medication, acupuncture, and spinal manipulation. Spine (Phila Pa 1976) 2003 Jul 15;28(14):1490–1502. doi: 10.1097/00007632-200307150-00003. discussion 1502-1493. [DOI] [PubMed] [Google Scholar]
- 104.Itoh K, Hirota S, Katsumi Y, Ochi H, Kitakoji H. Trigger point acupuncture for treatment of knee osteoarthritis--a preliminary RCT for a pragmatic trial. Acupunct Med. 2008 Mar;26(1):17–26. doi: 10.1136/aim.26.1.17. [DOI] [PubMed] [Google Scholar]
- 105.Itoh K, Katsumi Y, Hirota S, Kitakoji H. Effects of trigger point acupuncture on chronic low back pain in elderly patients--a sham-controlled randomised trial. Acupunct Med. 2006 Mar;24(1):5–12. doi: 10.1136/aim.24.1.5. [DOI] [PubMed] [Google Scholar]
- 106.Itoh K, Katsumi Y, Hirota S, Kitakoji H. Randomised trial of trigger point acupuncture compared with other acupuncture for treatment of chronic neck pain. Complement Ther Med. 2007 Sep;15(3):172–179. doi: 10.1016/j.ctim.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 107.Jubb RW, Tukmachi ES, Jones PW, Dempsey E, Waterhouse L, Brailsford S. A blinded randomised trial of acupuncture (manual and electroacupuncture) compared with a non-penetrating sham for the symptoms of osteoarthritis of the knee. Acupunct Med. 2008 Jun;26(2):69–78. doi: 10.1136/aim.26.2.69. [DOI] [PubMed] [Google Scholar]
- 108.Stener-Victorin E, Kruse-Smidje C, Jung K. Comparison between electro-acupuncture and hydrotherapy, both in combination with patient education and patient education alone, on the symptomatic treatment of osteoarthritis of the hip. Clin J Pain. 2004 May-Jun;20(3):179–185. doi: 10.1097/00002508-200405000-00008. [DOI] [PubMed] [Google Scholar]
- 109.Tsui ML, Cheing GL. The effectiveness of electroacupuncture versus electrical heat acupuncture in the management of chronic low-back pain. J Altern Complement Med. 2004 Oct;10(5):803–809. doi: 10.1089/acm.2004.10.803. [DOI] [PubMed] [Google Scholar]
- 110.Yeung CK, Leung MC, Chow DH. The use of electro-acupuncture in conjunction with exercise for the treatment of chronic low-back pain. J Altern Complement Med. 2003 Aug;9(4):479–490. doi: 10.1089/107555303322284767. [DOI] [PubMed] [Google Scholar]
- 111.Facco E, Liguori A, Petti F, et al. Traditional acupuncture in migraine: a controlled, randomized study. Headache. 2008 Mar;48(3):398–407. doi: 10.1111/j.1526-4610.2007.00916.x. [DOI] [PubMed] [Google Scholar]
- 112.White AR, Resch KL, Chan JC, et al. Acupuncture for episodic tension-type headache: a multicentre randomized controlled trial. Cephalalgia. 2000 Sep;20(7):632–637. doi: 10.1111/j.1468-2982.2000.00097.x. [DOI] [PubMed] [Google Scholar]
- 113.Sun KO, Chan KC, Lo SL, Fong DY. Acupuncture for frozen shoulder. Hong Kong Med J. 2001 Dec;7(4):381–391. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.