Abstract
This study reports the intermediate-term results of four patients from a series eight patients who have had an insertion of a new complete distal radioulnar joint (DRUJ) prosthesis.
A retrospective review was performed for all patients who underwent DRUJ joint replacement with the STABILITY Sigmoid Notch Total DRUJ System between the years of 2003 and 2008. To be included in this report, all patients had to have more than 24 months of follow-up and hand examination by the senior author. From the eight patients with this procedure, four patients met the inclusion criteria. These included one patient with painful posttraumatic arthritis, two patients with failed hemiarthroplasty, and one patient with a failed Sauvé–Kapandji procedure. Mean age at the time of surgery was 42.5 years (range: 35 to 51 years) and mean follow-up was 46 months (range: 36 to 66 months). Preoperative and postoperative assessment included range of motion, grip strength, visual analog pain scale, patient satisfaction, and radiographic evaluation.
There was a successful replacement of the DRUJ in all four patients. Final range of motion showed mean pronation of 80 degrees (range: 60 to 90 degrees) and mean supination of 64 degrees (range: 45 to 90 degrees). Final grip strength on the operated extremity was 25.5 kg and averaged 73% of contralateral side. This was an improvement from preoperative grip strength of 14.5 kg visual analog pain scale decreased from 8 to 2.5 following surgery (scale: 1 to 10). Patient satisfaction was 100%. One patient returned to manual labor, one patient returned to office work, and two patients remained off work. Postoperative radiographs depict appropriate alignment of the DRUJ, and there have been no cases of subluxation or dislocation. Implant survival has been 100%.
Total DRUJ joint replacement with sigmoid notch resurfacing and distal ulna replacement is an alternative to ulnar head resection in cases of DRUJ arthritis. Total DRUJ arthroplasty with this resurfacing design may provide a means of decreasing pain and restoring DRUJ stability and motion following severe trauma, failed hemiarthroplasty, or failed Sauvé–Kapandji procedure. More experience is needed with this implant to confirm these initial encouraging results. The level of evidence for this study is IV (therapeutic, case series).
Keywords: arthroplasty, distal radioulnar joint, reconstruction, ulnar head, wrist
The distal radioulnar joint (DRUJ) and its supporting soft-tissue structures are responsible for maintaining normal kinematics of the forearm and wrist, especially during forearm rotation and axial loading.1,2,3,4,5,6,7 DRUJ dysfunction due to fracture or lack of soft-tissue support can lead to instability and eventual arthritis. Acute instability can be treated by reconstructing the supporting soft tissues and ligaments, and many studies have shown good intermediate-term results with acute repair.8,9 Chronic instability, with and without arthritis, poses a greater surgical challenge. Early treatment options focused on surgical excision of the distal ulna.10 Initial reports showed the Darrach procedure produced positive results in terms of improving pain and range of motion,11,12,13 but mounting evidence has shown that patients may develop painful ulnoradial impingement and poor function in the long term.14,15,16,17
Recognizing the importance of preserving, the DRUJ complex has led to several alternatives or supplements to the Darrach procedure. The Sauvé–Kapandji procedure fuses the DRUJ while creating a proximal pseudarthrosis.18 This procedure maintains the structure of the DRUJ and surrounding soft tissues and clinically has shown improved pain and range of motion.19,20,21,22,23,24,25,26,27 However, the instability of the ulnar stump including ulnoradial impingement following the Sauvé–Kapandji procedure is a concern,28,29 and some investigators recommend only Sauvé–Kapandji as a salvage procedure.19,21,29
The attempts to treat the DRUJ arthrosis through partial or complete ulnar excision while attempting to preserve the triangular fibrocartilage complex attachment to the ulnar styloid have been proposed since the triangular fibrocartilage is the main stabilizer of the DRUJ. These ablative techniques include hemi-resection-interposition arthroplasty,30 matched distal ulna resection,31 and the complete excision or Darrach procedure. Hemi-resection-interposition showed improved functional and pain scores in select groups32,33,34 but poor radioulnar dynamics.35 The matched distal ulna resection procedure has shown adequate results in selected patient groups that include primarily rheumatoid31 and posttraumatic arthritis.36
Unfortunately, all of the earlier-described surgical options fail to restore normal DRUJ joint anatomy and kinematics. In an effort to correct these deficiencies, current basic and clinical research has focused on the development of an ulnar head prosthesis.37,38,39 In comparison with the Darrach procedure, ulnar head replacement has been shown to restore the normal axis of forearm rotation and resist compressive forced at the DRUJ.35,40 Recent reports examining ulnar head replacement have noted a high incidence of sigmoid notch erosion following ulnar head replacement.41,42 Although erosion alone has not been linked directly to pain, concerns remain regarding the overall impact that erosion has on clinical symptomatology and on long-term implant survival.41,42
Newer implant designs have focused on total joint replacement involving the sigmoid notch and the ulnar head. Presently available total joint replacements options include both constrained and semiconstrained designs. Although initial short-term results for the constrained Scheker prosthesis seem promising, long-term results are still unknown.43,44 There have been scant reports examining any other varieties of total DRUJ arthroplasties. Here, we report the preliminary intermediate outcomes of four patients who underwent total DRUJ reconstruction using an ulnar head prosthesis and a sigmoid notch resurfacing implant (STABILITY Sigmoid Notch Total DRUJ System, Small Bone Innovations, New York, NY), with specific focus on postoperative stability and forearm function.
Patients and Methods
A retrospective review was performed of all patients at our institution who had undergone placement of the STABILITY Sigmoid Notch Total DRUJ System (Small Bone Innovations, New York, NY) from 2003 to 2008 (Fig. 1). There were a total of eight patients. All but four patients were eliminated from the study related to exclusion criteria which included less than 2 years from time of surgery, inadequate radiographs, or the inability to return for postoperative evaluation by one of the senior authors. Patient records were reviewed for age, gender, injury, previous surgeries, chief presenting complaint, physical examination, and radiographs (Table 1). Postoperative assessment included range of motion, grip strength, pain, and radiographic evaluation.
Figure 1.
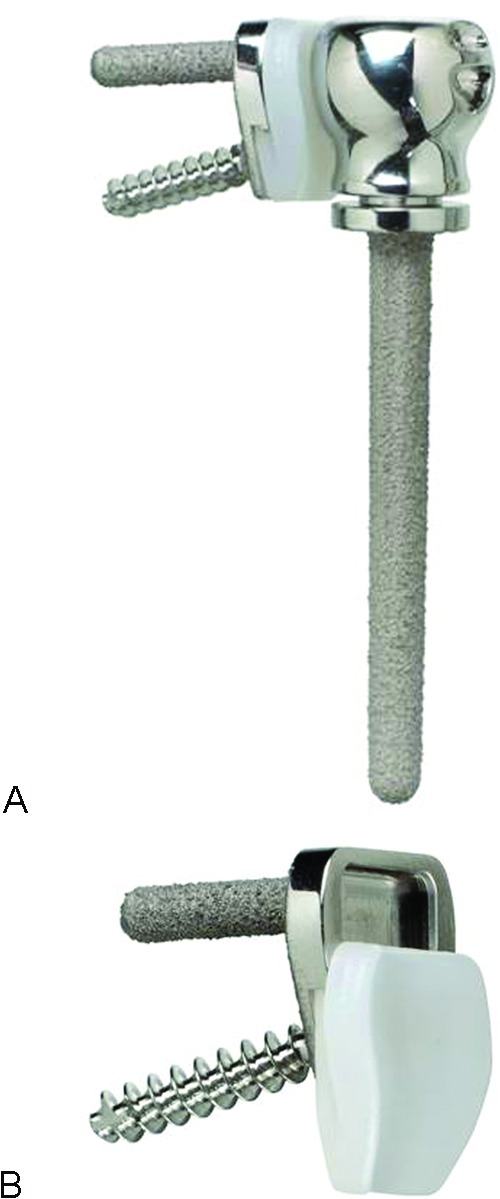
Semiconstrained Total distal radioulnar joint Implant System. (A) Sigmoid notch implant, standard-collar ulnar stem, and extended-collar ulnar stem. (B) Ulnar view of sigmoid notch implant and polyethylene tray, which slides up into the sigmoid notch implant.
Table 1. Preoperative Patient Characteristics.
| Patient | Gender | Age (y) | Hand Dominance | Side of Injury | Original Injury | Previous Surgeries to Wrist | Reason for Placement of STABILITY Implant |
|---|---|---|---|---|---|---|---|
| 1 | M | 35 | Right | Left | Open dorsal radiocarpal fracture-dislocation and ulnar styloid fracture | 1. Open reduction of distal radius, ulnar styloid pinning 2. Muscle flap coverage of wrist 3. Radioscapholunate fusion |
Ulnar wrist pain, loss of forearm rotation |
| 2 | F | 51 | Right | Right | Fall onto outstretched hand | 1. Distal radioulnar joint ligament repair × 2 2. Proximal row carpectomy 3. Wrist arthrodesis 4. U-head arthroplasty 5. U-head revision × 2 |
Chronic wrist pain, U-head erosion into radius |
| 3 | F | 47 | Right | Left | Car accident | 1. Darrach procedure 2. U-head arthroplasty |
Chronic ulnar-sided wrist pain, U-head erosion into radius |
| 4 | F | 37 | Right | Right | Triangular fibrocartilage complex tear following sports injury | 1. Radioscapholunate fusion 2. Nonunion revision 3. Excision of heterotopic ossification 4. Sauvé–Kapandji 5. Wrist arthrodesis |
Chronic wrist pain, ulnoradial impingement by ulnar stump |
Radiographs were specifically evaluated for signs of dorsal and volar instability using the criteria of Kakar et al.41 Dorsal and volar instability was judged through physical examination and by examining plain radiographs. True lateral radiographs, where there is an overlap of the distal one-third of the scaphoid on the pisiform, were examined for signs of joint subluxation. Subluxation was defined by drawing a longitudinally line through the center of the radius and the ulnar head and the distance between the two lines at the distal most aspect of the sigmoid notch was measured. A difference of 5 mm was defined as a sign of dorsal implant instability whereas a negative measurement greater than 5 mm indicated volar instability. Implants were evaluated for loosening, which was defined as greater than 2 mm of lucency around the ulnar prosthetic stem or greater than 2 mm of lucency around the screws of the sigmoid implant. Radiographs were also evaluated for osteolysis under the ulnar head and collar pedestal formation at the tip of the stem.41 Implant survival was defined as maintenance of the original implant. Charts were examined and the patients were questioned about any secondary surgical procedures following DRUJ arthroplasty.
The stability prosthesis is part of a modular system consisting of the, U-Head ulnar head prosthesis (Small Bone Innovations, Morristown, PA) and a polyethylene sigmoid notch resurfacing implant. The U-Head is a modular endoprosthesis that consists of a metal stem and ulnar head, connected via a tight-fit Morse-taper junction, and commercially pure titanium (CPTi) sprayed finish.45 Because the stem is also CPTi coated, the shaft can be either press fit or cemented into the distal ulnar medullary cavity. There are two neck designs, each with four stem diameters: a normal-length collar for primary procedures and an extended-length collar for secondary or revision procedures. The ulnar head is semispheric, made of cobalt-chrome alloy, and comes in four sizes. The ulnar head has suture sites to allow for soft-tissue attachment providing some stability during the initial healing phase, although any permanent soft tissue in growth is unlikely.
The Sigmoid Notch Implant comes in two sizes and consists of (1) cobalt chrome radial plate with CPTi finish, (2) cobalt chrome fixation screw (five sizes), and (3) ultrahigh molecular weight polyethylene insert (Fig. 1B). The insert slides onto the plate following plate fixation and secures via both peripheral and ramp lock snap fit. These implants are designed so that any size sigmoid notch can accommodate any size head.
Surgical technique for placement of the ulnar head component has been described previously.45 The approach to the DRUJ is made using an extended dorsal ulnar approach as previously described by Garcia-Elias and Hagert.46 The sigmoid notch component was placed after preparation of the ulnar shaft for ulnar head replacement. A trial head-and-saddle tool is placed onto the ulnar stem prior to placement of the final ulnar head prosthesis. This trial head and saddle tool is cannulated allowing the surgeon to drill a guidewire into the sigmoid notch. The position of the guidewire is then verified with posteroanterior and lateral fluoroscopy. Once position has been confirmed, the trial head is then removed, and a cannulated drill is passed over the guidewire to create a pilot hole for the sigmoid implant. The implant is then pressed into position and a cancellous bone screw is then placed into the sigmoid component firmly fixing it to the distal radius. The polyethylene insert is then placed onto the sigmoid component. The final ulnar head stem and prosthesis are then inserted into the ulnar shaft. The joint is reduced and the capsule is closed. Capsular closure is performed with several permanent sutures to ensure stability. It is important to note in revision cases of previous ulna head implant that an osteotome or special tool from the manufacturer is needed to loosen the ulna head component from the stem because the latter is locked in place with the Morris taper stem.
Following surgical intervention, the forearm and wrist were placed into a sugar tong splint for 2 weeks followed by a Muenster cast or long arm cast in full forearm supination for 4 additional weeks. Range-of-motion exercises were initiated at 6 weeks postoperatively, with a supportive ulnar gutter clam shell splint worn for an additional 4 weeks. Patients were allowed to return to regular activities at 12 weeks.
Results
Four patients fit inclusion criteria for the study. The mean age at time of surgery was 42.5 years (range: 35 to 51). Mean follow-up was 46 months (range: 36 to 66 months). The chief presenting complaint was ulnar-sided wrist pain. All patients had an average of four (range: two to seven) prior operative procedures before receiving a total DRUJ replacement. Successful implant of the total DRUJ was achieved in each patient.
Postoperatively, pain reduced in all patients. Average preoperative VAS pain score (scale: 1 to 10) was 8 points and averaged 2.5 on final follow-up. An average VAS decrease of 5 points was seen amongst the four patients. Preoperative grip strength averaged 7.5 kg (range: 4 to 12 kg) and improved postoperatively to an average of 25.5 kg (range: 10 to 32 kg). Grip strength was 73% of the contralateral side on final follow-up. Forearm rotation remained stable or improved in all patients. Mean final pronation and supination was 80 degrees (range: 60 to 90 degrees) and 64 degrees (range: 45 to 90 degrees), respectively. There was no clinical evidence of instability noted in any of the forearms. Patient satisfaction was 100% with all patients stating they would have the operation again. One patient was able to return to manual labor without restrictions, one patient returned to a desk job, and two patients remained off work. At time of most recent follow-up, there have been no secondary procedures performed following implant placement and implant survival at an average of 46 months is 100%.
Postoperative radiographs showed appropriate alignment of the DRUJ, with well-seated implants. There was no evidence of ulnar stem or sigmoid notch loosening (Figs. 2 and 3). Using the criteria of Kakar et al, there was no evidence of dorsal or volar instability.41 There was also no evidence for polyethylene wear or particular synovitis. All ulnar shafts showed evidence of tapering and two of the four had evidence of pedestal formation (Figs. 2 and 3).
Figure 2.

(A and B) Preoperative PA and lateral radiograph of the wrist of Patient 3. The patient had undergone a previous ulnar head replacement for (A) primary distal radioulnar joint arthritis. Note erosion of the ulnar head into the sigmoid notch with overlying shelf of bone, which was felt to limit pronation. (C and D) Final postoperative PA and lateral radiographs showing a well-seated implant with no evidence of dorsal subluxation. Tapering of the ulnar shaft can be seen in the PA radiograph. PA, posterior to anterior.
Figure 3.

(A and B) Preoperative PA and lateral radiograph of patient 4. The patient had undergone a previous radioscapholunate fusion and Sauvé–Kapandji procedure for wrist pain. At the time of initial evaluation, she had painful impingement of the proximal ulnar stump. (C and D) Final follow-up radiographs showing a well-seated implant. An extended collar was used to allow the sigmoid notch to be placed in position of the previously fused ulnar head. Note tapering of ulnar shaft on the PA radiograph. Lateral radiographs show good alignment. PA, posterior to anterior.
Discussion
The attempts to reconstruct the DRUJ were first investigated by Swanson in the 1970s, using a silicone endoprosthesis.47 Long-term results showed effective pain relief; however, concerns over bone resorption, prosthesis tilting and fracture, and the development of silicone synovitis limited its use.48,49,50 In response to the difficulties encountered with the use of silicone, Herbert and coworkers developed an ulnar head replacement that used a titanium stem and a modular, spherical ceramic head.37,51 Multiple sizes of stems and heads combined with soft-tissue repair provide improved joint stability. Herbert and van Schoonhoven felt that compressive loads across the DRUJ were low enough to avoid the need for a separate sigmoid notch arthroplasty.37 Short-term and intermediate-term results, including pain, patient satisfaction, motion, and grip strength, have been promising.37,51,52
In 2007, Sauder and King reported on the E-Centrix ulnar head replacement.53 This prosthesis attempted to more exactly mimic the anatomic features of the ulnar head, including offsetting the ulnar head from the distal ulnar shaft and using an aspherical design. Clinical results have yet to be reported.
Garcia-Elias reported on the Eclypse partial ulnar head endoprosthesis in 2007.54 It is a pyrocarbon spacer that attempts to substitute the articular portion of the distal ulna while allowing the remaining portion of the distal ulna, specifically the fovea, to remain in the hopes of improving soft-tissue stability. Short-term outcomes in three patients showed promising results with good range of motion under 4-kg load.54
The longest published follow-up for ulnar head replacement involves the use of the U-Head endoprosthesis. Willis et al reported on the preliminary results of the U-head in 2007.45 The initial series of 19 wrists showed improvement in pain scores, satisfaction scores, and grip strength, but no change in forearm rotation from preoperative values. Longer-term results have shown that problems with this implant can occur in up to 30% of patients and these can include DRUJ instability, continued pain, and implant loosening.41 Six-year implant survival rate from the recent study by Kakar et al was 83%; 34% of implants had evidence of radiographic dorsal displacement of the implant with respect to the sigmoid fossa, although they were not correlated with clinical instability.41 In addition, 57% of implants showed evidence of ulnar head erosion into the sigmoid notch. Although a direct clinical correlation could not be identified with sigmoid erosion in the study by Kakar et al, it should be noted that two patients in this study had significant ulnar-sided pain and evidence of sigmoid notch erosion.41 This pain, in our study, was relieved following sigmoid notch replacement.
The need for sigmoid notch replacement can stem from various reasons, but in this study, primary osteoarthritis (posttraumatic arthritis), failed ulnar head arthroplasty, and a failed Sauvé-Kapandji procedure were the reasons for our decision to replace the sigmoid notch. Each patient had had multiple prior surgeries in and around the DRUJ. As such, this procedure was an attempt to improve pain and motion in cases of altered sigmoid notch anatomy. In this regard, the STABILITY system produced good results and better than one would expect if these cases had simply been converted to a Darrach procedure.14,15,16,17 Each patient was satisfied with the procedure, and strength improved as compared with preoperative status. One case study has previously reported the use of this implant in a failed Sauvé–Kapandji, with good results at 1 year.55
The STABILITY system is the only total DRUJ surface replacement arthroplasty prosthesis that exists today. The advantages of this system include maintenance of DRUJ stability, restoration of the anatomic forearm rotation, and avoidance of excessive hardware seen in constrained and semiconstrained designs. The implant also provides the option of additional salvage surgery should an ulnar head prosthesis alone fail due to long-term sigmoid notch erosion.
The concerns with a semiconstrained design, using a polyethylene component, are primarily centered on the development of wear debris. Such wear debris has been noted in total wrist placement as well as in lower extremity joint replacement.56,57 Although this study failed to find any evidence of polyethylene wear at close to 4-year follow-up, patient monitoring with clinical examination and radiographs is planned. Gross instability with this implant, as evident by dorsal subluxation in the lateral radiographs, should be a sign of concern as significant instability could result in expedited polyethylene edge wear. In such cases, we would recommend attempts at soft-tissue stabilization or conversion to a constrained implant.
Inherent stability provided by the implant itself is most likely no more than in the anatomic setting, where it has been shown that 20% of DRUJ constraint is provided by articular contact.58 Capsular stability and soft-tissue stability are still necessary in these patients for good clinical outcomes. In all cases, with the exception of patient 4, stout capsular closure was possible following exposure of the DRUJ as described by Garcia-Elias and Hagert.46 It should be noted that in patient 4, who underwent a salvage of a failed Sauvé–Kapandji procedure, capsular reconstruction was necessary prior to closure because the native capsule was not present. In this case, a tenodesis was preformed, using the extensor carpi ulnaris tendon, to stabilize the ulnar head within the sigmoid notch. Until further data are available, the use of this implant is not encouraged in cases of gross ligamentous instability and concomitant interosseous membrane injuries. In such cases, where soft-tissue stabilization is not possible, we would recommend the use of a constrained implant. Further research is needed to validate this assumption.
Finally, it should be noted that three of four patients within this study had some form of carpal fusion (Table 1). Carpal fusion has been an area of concern in the past for ulnar head replacement because this could lead to increased force through the sigmoid notch leading to accelerated osteolysis. Although we are unable to verify such concerns in this study, we did find that good results were obtained in all patients despite previous wrist fusion procedures.
The limitations of this study include its retrospective nature, its small sample size, and the lack of standardized selection process for implant placement. Overall, results were promising with no major complications and 100% implant survival at close to 4-year follow-up. Given these preliminary results, further use and study of this total DRUJ arthroplasty is warranted.
References
- 1.Shaaban H, Giakas G, Bolton M. et al. The load-bearing characteristics of the forearm: pattern of axial and bending force transmitted through ulna and radius. J Hand Surg [Br] 2006;31(3):274–279. doi: 10.1016/j.jhsb.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 2.Markolf K L, Lamey D, Yang S, Meals R, Hotchkiss R. Radioulnar load-sharing in the forearm. A study in cadavera. J Bone Joint Surg Am. 1998;80(6):879–888. doi: 10.2106/00004623-199806000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Elias M. Soft-tissue anatomy and relationships about the distal ulna. Hand Clin. 1998;14(2):165–176. [PubMed] [Google Scholar]
- 4.Linscheid R L. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1992;(275):46–55. [PubMed] [Google Scholar]
- 5.Kauer J M. The distal radioulnar joint. Anatomic and functional considerations. Clin Orthop Relat Res. 1992;(275):37–45. [PubMed] [Google Scholar]
- 6.Hagert C G. The distal radioulnar joint in relation to the whole forearm. Clin Orthop Relat Res. 1992;(275):56–64. [PubMed] [Google Scholar]
- 7.Palmer A K, Werner F W. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1984;(187):26–35. [PubMed] [Google Scholar]
- 8.Adams B D, Berger R A. An anatomic reconstruction of the distal radioulnar ligaments for posttraumatic distal radioulnar joint instability. J Hand Surg Am. 2002;27(2):243–251. doi: 10.1053/jhsu.2002.31731. [DOI] [PubMed] [Google Scholar]
- 9.Scheker L R, Belliappa P P, Acosta R, German D S. Reconstruction of the dorsal ligament of the triangular fibrocartilage complex. J Hand Surg [Br] 1994;19(3):310–318. doi: 10.1016/0266-7681(94)90079-5. [DOI] [PubMed] [Google Scholar]
- 10.Darrach W. Partial excision of lower shaft of ulna for deformity following Colles' fracture. Ann Surg. 1913;57:764–765. [PubMed] [Google Scholar]
- 11.Hartz C R, Beckenbaugh R D. Long-term results of resection of the distal ulna for post-traumatic conditions. J Trauma. 1979;19(4):219–226. doi: 10.1097/00005373-197904000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Dingman P VC. Resection of the distal end of the ulna (Darrach operation); an end result study of twenty four cases. J Bone Joint Surg Am. 1952;34A(4):893–900. [PubMed] [Google Scholar]
- 13.McKee M D, Richards R R. Dynamic radio-ulnar convergence after the Darrach procedure. J Bone Joint Surg Br. 1996;78(3):413–418. [PubMed] [Google Scholar]
- 14.Field J, Majkowski R J, Leslie I J. Poor results of Darrach's procedure after wrist injuries. J Bone Joint Surg Br. 1993;75(1):53–57. doi: 10.1302/0301-620X.75B1.8421034. [DOI] [PubMed] [Google Scholar]
- 15.Bieber E J, Linscheid R L, Dobyns J H, Beckenbaugh R D. Failed distal ulna resections. J Hand Surg Am. 1988;13(2):193–200. doi: 10.1016/s0363-5023(88)80047-9. [DOI] [PubMed] [Google Scholar]
- 16.Bell M J, Hill R J, McMurtry R Y. Ulnar impingement syndrome. J Bone Joint Surg Br. 1985;67(1):126–129. doi: 10.1302/0301-620X.67B1.3968131. [DOI] [PubMed] [Google Scholar]
- 17.Garcia-Elias M. Failed ulnar head resection: prevention and treatment. J Hand Surg [Br] 2002;27(5):470–480. doi: 10.1054/jhsb.2002.0815. [DOI] [PubMed] [Google Scholar]
- 18.Sauve L, Kapandji M. Nouvelle technique des traitement chirurgical des luxations redidivantes isolees de l'extremite intericubitus. J Chir (Paris) 1936;47:589–594. [Google Scholar]
- 19.Jacobsen T W, Leicht P. The Sauvé-Kapandji procedure for posttraumatic disorders of the distal radioulnar joint. Acta Orthop Belg. 2004;70(3):226–230. [PubMed] [Google Scholar]
- 20.Low C K, Chew W YC. Results of Sauve-kapandji procedure. Singapore Med J. 2002;43(3):135–137. [PubMed] [Google Scholar]
- 21.Lamey D M, Fernandez D L. Results of the modified Sauvé-Kapandji procedure in the treatment of chronic posttraumatic derangement of the distal radioulnar joint. J Bone Joint Surg Am. 1998;80(12):1758–1769. doi: 10.2106/00004623-199812000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Rothwell A G, O'Neill L, Cragg K. Sauvé-Kapandji procedure for disorders of the distal radioulnar joint: a simplified technique. J Hand Surg Am. 1996;21(5):771–777. doi: 10.1016/S0363-5023(96)80190-0. [DOI] [PubMed] [Google Scholar]
- 23.Minami A, Suzuki K, Suenaga N, Ishikawa J. The Sauvé-Kapandji procedure for osteoarthritis of the distal radioulnar joint. J Hand Surg Am. 1995;20(4):602–608. doi: 10.1016/s0363-5023(05)80276-x. [DOI] [PubMed] [Google Scholar]
- 24.Vincent K A, Szabo R M, Agee J M. The Sauve-Kapandji procedure for reconstruction of the rheumatoid distal radioulnar joint. J Hand Surg Am. 1993;18(6):978–983. doi: 10.1016/0363-5023(93)90386-H. [DOI] [PubMed] [Google Scholar]
- 25.Mikkelsen S S, Lindblad B E, Sommer J. Sauvè-Kapandji operation for disorders of the distal radioulnar joint. Contemp Orthop. 1993;26(2):151–155. [PubMed] [Google Scholar]
- 26.Millroy P, Coleman S, Ivers R. The Sauvé-Kapandji operation. Technique and results. J Hand Surg [Br] 1992;17(4):411–414. doi: 10.1016/s0266-7681(05)80264-5. [DOI] [PubMed] [Google Scholar]
- 27.Sanders R A, Frederick H A, Hontas R B. The Sauvé-Kapandji procedure: a salvage operation for the distal radioulnar joint. J Hand Surg Am. 1991;16(6):1125–1129. doi: 10.1016/s0363-5023(10)80078-4. [DOI] [PubMed] [Google Scholar]
- 28.Nakamura R, Tsunoda K, Watanabe K, Horii E, Miura T. The Sauvé-Kapandji procedure for chronic dislocation of the distal radio-ulnar joint with destruction of the articular surface. J Hand Surg [Br] 1992;17(2):127–132. doi: 10.1016/0266-7681(92)90071-9. [DOI] [PubMed] [Google Scholar]
- 29.Taleisnik J. The Sauvé-Kapandji procedure. Clin Orthop Relat Res. 1992;(275):110–123. [PubMed] [Google Scholar]
- 30.Bowers W H. Distal radioulnar joint arthroplasty: the hemiresection-interposition technique. J Hand Surg Am. 1985;10(2):169–178. doi: 10.1016/s0363-5023(85)80100-3. [DOI] [PubMed] [Google Scholar]
- 31.Watson H K, Ryu J Y, Burgess R C. Matched distal ulnar resection. J Hand Surg Am. 1986;11(6):812–817. doi: 10.1016/s0363-5023(86)80228-3. [DOI] [PubMed] [Google Scholar]
- 32.Bain G I, Pugh D M, MacDermid J C, Roth J H. Matched hemiresection interposition arthroplasty of the distal radioulnar joint. J Hand Surg Am. 1995;20(6):944–950. doi: 10.1016/S0363-5023(05)80141-8. [DOI] [PubMed] [Google Scholar]
- 33.Imbriglia J E, Matthews D. Treatment of chronic post-traumatic dorsal subluxation of the distal ulna by hemiresection-interposition arthroplasty. J Hand Surg Am. 1993;18(5):899–907. doi: 10.1016/0363-5023(93)90064-A. [DOI] [PubMed] [Google Scholar]
- 34.Minami A, Kaneda K, Itoga H. Hemiresection-interposition arthroplasty of the distal radioulnar joint associated with repair of triangular fibrocartilage complex lesions. J Hand Surg Am. 1991;16(6):1120–1125. doi: 10.1016/s0363-5023(10)80077-2. [DOI] [PubMed] [Google Scholar]
- 35.Sauerbier M, Fujita M, Hahn M E, Neale P G, Berger R A. The dynamic radioulnar convergence of the Darrach procedure and the ulnar head hemiresection interposition arthroplasty: a biomechanical study. J Hand Surg [Br] 2002;27(4):307–316. doi: 10.1054/jhsb.2002.0763. [DOI] [PubMed] [Google Scholar]
- 36.Watson H K, Gabuzda G M. Matched distal ulna resection for posttraumatic disorders of the distal radioulnar joint. J Hand Surg Am. 1992;17(4):724–730. doi: 10.1016/0363-5023(92)90324-i. [DOI] [PubMed] [Google Scholar]
- 37.Herbert T J, van Schoonhoven J. Ulnar head replacement. Tech Hand Up Extrem Surg. 2007;11(1):98–108. doi: 10.1097/bth.0b013e318033738a. [DOI] [PubMed] [Google Scholar]
- 38.Kopylov P, Tägil M. Distal radioulnar joint replacement. Tech Hand Up Extrem Surg. 2007;11(1):109–114. doi: 10.1097/bth.0b013e3180337dd9. [DOI] [PubMed] [Google Scholar]
- 39.Conaway D A, Kuhl T L, Adams B D. Comparison of the native ulnar head and a partial ulnar head resurfacing implant. J Hand Surg Am. 2009;34(6):1056–1062. doi: 10.1016/j.jhsa.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 40.Gordon K D, Dunning C E, Johnson J A, King G JW. Kinematics of ulnar head arthroplasty. J Hand Surg [Br] 2003;28(6):551–558. doi: 10.1016/s0266-7681(03)00150-5. [DOI] [PubMed] [Google Scholar]
- 41.Kakar S, Swann R P, Perry K I, Wood-Wentz C M, Shin A Y, Moran S L. Functional and radiogrpahic outcomes following distal ulna implant arthroplasty. J Hand Surg Am. 2012;37:1364–1371. doi: 10.1016/j.jhsa.2012.03.026. [DOI] [PubMed] [Google Scholar]
- 42.Herzberg G. Periprosthetic bone resorption and sigmoid notch erosion around ulnar head implants: a concern? Hand Clin. 2010;26(4):573–577. doi: 10.1016/j.hcl.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 43.Scheker L R. Implant arthroplasty for the distal radioulnar joint. J Hand Surg Am. 2008;33(9):1639–1644. doi: 10.1016/j.jhsa.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 44.Scheker L R, Babb B A, Killion P E. Distal ulnar prosthetic replacement. Orthop Clin North Am. 2001;32(2):365–376. doi: 10.1016/s0030-5898(05)70256-x. [DOI] [PubMed] [Google Scholar]
- 45.Willis A A, Berger R A, Cooney W P III. Arthroplasty of the distal radioulnar joint using a new ulnar head endoprosthesis: preliminary report. J Hand Surg Am. 2007;32(2):177–189. doi: 10.1016/j.jhsa.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 46.Garcia-Elias M, Hagert E. Surgical approaches to the distal radioulnar joint. Hand Clin. 2010;26(4):477–483. doi: 10.1016/j.hcl.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 47.Swanson A B. Implant arthroplasty for disabilities of the distal radioulnar joint. Use of a silicone rubber capping implant following resection of the ulnar head. Orthop Clin North Am. 1973;4(2):373–382. [PubMed] [Google Scholar]
- 48.Stanley D, Herbert T J. The Swanson ulnar head prosthesis for post-traumatic disorders of the distal radio-ulnar joint. J Hand Surg [Br] 1992;17(6):682–688. doi: 10.1016/0266-7681(92)90201-c. [DOI] [PubMed] [Google Scholar]
- 49.Sagerman S D, Seiler J G, Fleming L L, Lockerman E. Silicone rubber distal ulnar replacement arthroplasty. J Hand Surg [Br] 1992;17(6):689–693. doi: 10.1016/0266-7681(92)90202-d. [DOI] [PubMed] [Google Scholar]
- 50.McMurtry R Y, Paley D, Marks P, Axelrod T. A critical analysis of Swanson ulnar head replacement arthroplasty: rheumatoid versus nonrheumatoid. J Hand Surg Am. 1990;15(2):224–231. doi: 10.1016/0363-5023(90)90099-d. [DOI] [PubMed] [Google Scholar]
- 51.van Schoonhoven J, Fernandez D L, Bowers W H, Herbert T J. Salvage of failed resection arthroplasties of the distal radioulnar joint using a new ulnar head prosthesis. J Hand Surg Am. 2000;25(3):438–446. doi: 10.1053/jhsu.2000.6006. [DOI] [PubMed] [Google Scholar]
- 52.Fernandez D L, Joneschild E S, Abella D M. Treatment of failed Sauvé-Kapandji procedures with a spherical ulnar head prosthesis. Clin Orthop Relat Res. 2006;445:100–107. doi: 10.1097/01.blo.0000205901.13609.70. [DOI] [PubMed] [Google Scholar]
- 53.Sauder D J, King G J. Hemiarthroplasty of the distal ulna with an eccentric prosthesis. Tech Hand Up Extrem Surg. 2007;11(1):115–120. doi: 10.1097/bth.0b013e3180336d0a. [DOI] [PubMed] [Google Scholar]
- 54.Garcia-Elias M. Eclypse: partial ulnar head replacement for the isolated distal radio-ulnar joint arthrosis. Tech Hand Up Extrem Surg. 2007;11(1):121–128. doi: 10.1097/bth.0b013e31803261e2. [DOI] [PubMed] [Google Scholar]
- 55.Atwal N S, Clark D A, Amirfeyz R, Bhatia R. Salvage of a failed Sauve-Kapandji procedure using a total distal radio-ulnar joint replacement. Hand Surg. 2010;15(2):119–122. doi: 10.1142/S021881041000476X. [DOI] [PubMed] [Google Scholar]
- 56.O'Flynn H M, Rosen A, Weiland A J. Failure of the hinge mechanism of a trispherical total wrist arthroplasty: a case report and review of the literature. J Hand Surg Am. 1999;24(1):156–160. doi: 10.1053/jhsu.1999.jhsu24a0156. [DOI] [PubMed] [Google Scholar]
- 57.Groot D, Gosens T, Leeuwen N C, Rhee M V, Teepen H J. Wear-induced osteolysis and synovial swelling in a patient with a metal-polyethylene wrist prosthesis. J Hand Surg Am. 2006;31(10):1615–1618. doi: 10.1016/j.jhsa.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 58.Stuart P R, Berger R A, Linscheid R L, An K N. The dorsopalmar stability of the distal radioulnar joint. J Hand Surg Am. 2000;25(4):689–699. doi: 10.1053/jhsu.2000.9418. [DOI] [PubMed] [Google Scholar]


