Abstract
This study reports the current results of an international multicenter study of one last generation total wrist arthroplasty (TWA) (“ReMotion,” Small Bone Innovation, Morristown, PA).
The two first authors (G.H. and M.B.) built a Web-based prospective database including clinical and radiological preoperative and postoperative reports of “ReMotion” TWA at regular intervals. The cases of 7 centers with more than 15 inclusions were considered for this article.
A total of 215 wrists were included. In the rheumatoid arthritis (RA; 129 wrists) and nonrheumatoid arthritis (non-RA; 86 wrists) groups, there were respectively 5 and 6% complications requiring implant revision with a survival rate of 96 and 92%, respectively, at an average follow-up of 4 years. Within the whole series, only one dislocation was observed in one non-RA wrist. A total of 112 wrists (75 rheumatoid and 37 nonrheumatoid) had more than 2 years of follow-up (minimum: 2 years, maximum: 8 years). In rheumatoid and non-RA group, visual analog scale (VAS) pain score improved by 48 and 54 points, respectively, and QuickDASH score improved by 20 and 21 points, respectively, with no statistical differences. Average postoperative arc of wrist flexion–extension was 58 degrees in rheumatoid wrists (loss of 1 degree) compared with 63 degrees in non-RA wrists (loss of 9 degrees) with no statistical differences. Grip strength improved respectively by 40 and 19% in rheumatoid and non-RA groups (p = 0.033). Implant loosening was observed in 4% of the rheumatoid wrists and 3% of the non-RA wrists with no statistical differences.
A Web-based TWA international registry was presented. Our results suggest that the use of the “ReMotion” TWA is feasible in the midterm both for rheumatoid and non-RA patients. This is a significant improvement compared with the previous generation TWA. The level of evidence for this study is IV.
Keywords: total wrist arthroplasty, multicenter study, wrist arthrtitis, wrist arthrosis
Total wrist arthroplasty (TWA) is one of the most controversial procedures in surgery of the arthritic wrist.1 The high rate of complications of the first generation TWA is well known.2,3,4,5 The early results of last generation metal-polyethylene TWA with new designs seem to be better both in terms of clinical results and incidence of complications as shown in some recent studies.6,7 However, few cases were included in these studies. Another recent study of 24 cases of one last generation TWA at a minimum of 5 years of follow-up showed a high rate of failure, most often because of carpal component loosening.8 The improvement of survival rate and complications with last generation TWA remains to be proven. We made the hypothesis that a well-designed prospective multicenter study of one last generation TWA could provide larger numbers of patients and useful information. The purpose of this article was to report the results of this multicenter international study.
Methods
Only the ball and socket “ReMotion” TWA (Small Bone Innovation, Morristown, PA) resurfacing implant was used in this study. The two first authors (G.H. and M.B.) of this article built a Web-based database including clinical and radiological preoperative and postoperative reports at 6 weeks, 6 months, 12 months, and on a yearly basis. The database was built in cooperation with the Technical University of Denmark (S.M.). In addition to the etiology of the arthritis and classic clinical criteria (visual analog scale pain score, active wrist and forearm motion, grip strength with Jamar Dynamometer), QuickDASH score figures and patient's satisfaction were recorded. Operative data were recorded as well as complications and reoperations.
Radiological criteria included the subjective evaluation by the surgeon of the position of the implants (optimal, suboptimal, poor) and signs of loosening. All patients were included through a specifically designed Web site. Each surgeon participating in the study received a confidential code to enter his data. Statistics and survival rates were automatically generated and updated.
A total of 215 wrists in 210 patients operated on between 2003 and 2012 were included. All surgical centers were subspecialized for wrist surgery. The database could sort the cases according to surgeons and surgical centers. Only cases from surgical centers with more than 15 wrists were included in this series.
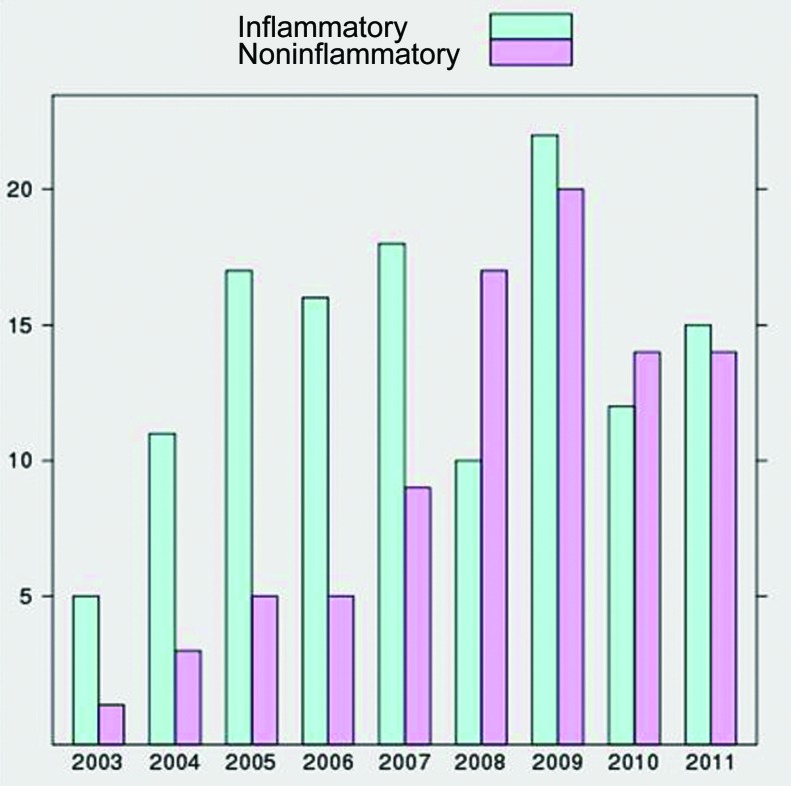
The etiology of wrist arthritis was RA in 129 wrists (60%) and non-RA in 86 wrists (40%). The significant number of non-RA wrists allowed the authors to consider separately the results of these two categories. Of the non-RA wrists, 62% were posttraumatic. The percentage of non-RA etiologies increased over the years (Fig. 1). Within the rheumatoid group, the female to male ratio was 76 to 24 and the average age was 63 years (minimum: 31 years, maximum: 86 years). Within the non-RA group, the female to male ratio was 66 to 34 and the average age was 63 years (minimum 33 years, maximum 84 years). A total of 112 wrists had more than 2 years of follow-up with an average of 4 years and a maximum of 8 years. Within these 112 wrists, 75 (67%) were rheumatoid wrists and 37 (33%) were non-RA wrists. The TWA was used without cement in most cases. Cement was used for both radial and carpal components in seven wrists and for the radial component in one wrist.
Figure 1.
Increase of nonrheumatoid indications over the years.
Kaplan–Meier survival analysis was used to estimate the cumulative probability of remaining free of revision (i.e., reoperation with total or partial removal of the implants). A nonparametric Wilcoxon signed rank test was used for data that were not normally distributed (QuickDASH scores and patient satisfaction) and the parametric Student t test was used for normally distributed data (flexion, extension, radial deviation, ulnar deviation, pronation, supination, and VAS scores). Significance was set at a p value of less than 0.05.
Results
Complications and Survival Rate of the Whole Series of 215 Wrists
Overall, there were 6 (5%) complications requiring implant revision (implant loosening: 4, wrist ankylosis: 1, and deep infection: 1) in the rheumatoid group. Four wrists sustained subsequent fusion and two wrists sustained reimplantation of a TWA. There were 5 (6%) complications requiring implant revision (implant loosening: 2, dislocation: 1, malposition: 1, ankylosis: 1) in the non-RA group. Three wrists sustained subsequent fusion and two wrists sustained reimplantation of a TWA.
There were respectively 2% (carpal tunnel syndrome) and 7% (carpal tunnel syndrome, reflex sympathetic dystrophy) of complications not requiring revision in rheumatoid and non-RA groups of patients.
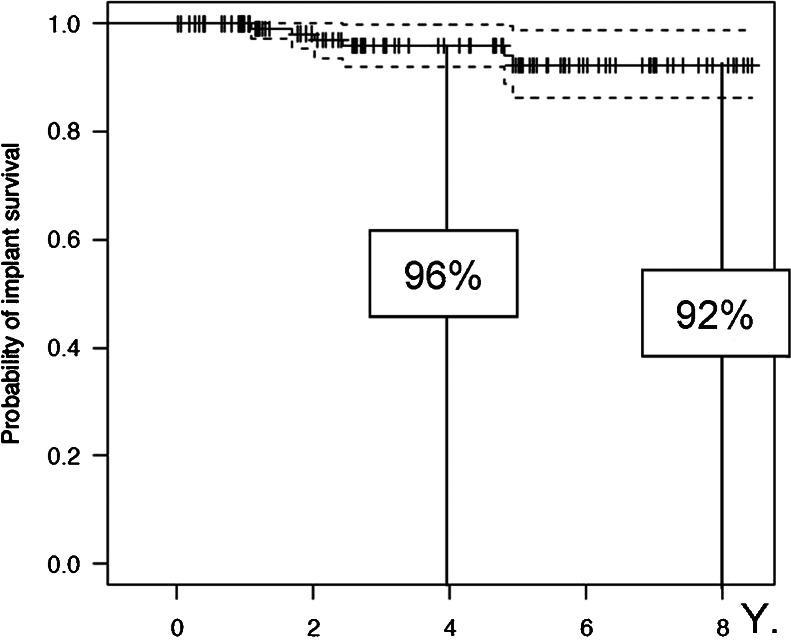
The Kaplan–Meier survival graphs are shown in Figs. 2 and 3. At the average follow-up of this study, the survival rate (with failure defined as implant revision) was 96% in the rheumatoid group of wrists and 92% in the non-RA group.
Figure 2.
Probability of implant survival in rheumatoid patients (failure defined as revision).
Figure 3.
Probability of implant survival in nonrheumatoid patients (failure defined as revision).
Clinical and Radiological Results of 112 Wrists with More Than 2 Years of Follow-Up
The clinical results (mean: 4 years; minimum: 2 years, maximum: 8 years) are reported in Table 1. Except for radial deviation and grip strength improvement, we could not find any statistically significant differences between rheumatoid and non-RA wrists. Patient's satisfaction was high both in the rheumatoid (88% very satisfied or satisfied) and in the non-RA groups (95% very satisfied or satisfied).
Table 1. Clinical Results of TWA in 112 Wrists with At Least 2 Years of Follow-Up.
| Rheumatoid | Nonrheumatoid | Statistical Significance (p) | |
|---|---|---|---|
| VAS pain improvement (100-point scale) | 48 points | 54 points | ns |
| QuickDASH improvement | 20 points | 21 points | ns |
| Wrist extension, degrees | 29 (+2) | 36 (−4) | ns |
| Wrist flexion, degrees | 29 (−3) | 37 (−5) | ns |
| Ulnar deviation, degrees | 24 (+7) | 28 (+2) | ns |
| Radial deviation, degrees | 5 (−1) | 10 (−4) | 0.015 |
| Grip strength improvement (% of preoperative value) | 40 | 19 | 0.033 |
ns, not significant; TWA, total wrist arthroplasty; VAS, visual analog scale.
In terms of radiological results, implant positioning was subjectively judged by the operating surgeon as optimal (86%) or suboptimal (11%) in 97% of the rheumatoid wrists and 100% of the non-RA wrists (optimal: 79% and suboptimal: 21%). Loosening with implant migration was observed in 4% of the rheumatoid wrists and 3% of the non-RA wrists (nonsignificant [ns], p = 1.000). Loosening without implant migration was observed in 8% of the rheumatoid wrists and 15% of the non-RA wrists (ns, p = 0.2520). Overall, the incidence of signs of periprosthetic loosening was 12% in the rheumatoid group compared with 18% in the non-RA group (the Fischer exact test; level of significance 0.05).
Discussion
The use of TWA to treat end-stage rheumatoid and non-RA arthritis is very controversial due to the high range of complications reported in previous series.1 Historically, the first total silicone wrist implants were abandoned because of unacceptable revision rates.5 They were followed by a first generation of metal-polyethylene total wrist arthroplasties that still had high complications and revisions rates.9 Even some newer metal-polyethylene prostheses designs showed at first promising results followed by unacceptable longer follow-up results.10,11 A recent systematic meta-analysis of a large series of total wrist arthroplasties (most of the first generation metal-polyethylene TWA) concluded that existing data do not support widespread application of TWA for rheumatoid arthritic wrists.5
This is why many surgeons prefer total wrist fusion to treat end-stage rheumatoid or non-RA wrist arthritis. Indeed, total wrist fusion will remain the only option for a destroyed RA wrist with bony destruction and complete loss of the carpal architecture.12 However, there are many debatable issues about total wrist fusion for end-stage arthritic wrist. It cannot be considered as a panacea for several reasons, both in rheumatoid and non-RA destroyed wrists. Wrist fusion may not provide optimal results in terms of daily activities as personal hygiene care, combing, dressing, or if multiple upper extremity joints are involved, or if there is bilateral wrist involvement.13 A wrist fusion implies the loss of the synergistic motion of wrist extension and long fingers flexion, which is very important to provide a good prehension. Wrist fusion may be followed by complications as hardware problems, secondary tendon ruptures, or carpal tunnel syndrome.14,15,16 The optimal position of the fusion for prehension, that is, slight extension and ulnar deviation is not always obtained.17 In some series of first generation total wrist arthroplasties where rheumatoid patients had a fusion on one side and a TWA on the other side, they almost always preferred arthroplasty.18 In osteoarthritic patients, total wrist fusion for end-stage destruction may leave a high percentage of residual pain or substantial dysfunction.19,20
Little has been written regarding the results of the newest resurfacing metal-polyethylene implants characterized by a smaller size allowing for minimal bone resection. The series are small and the follow-ups are still short or medium term.6,7 The only series with long-term follow-up showed a high percentage of revisions.8 Our current preliminary short-term results suggest that one last generation TWA may have better outcomes that those reported on more limited numbers of patients or old generation TWA. The results in terms of pain are good and active motion is consistent with functional wrist motion (30-degree extension, 5-degree flexion, 15-degree ulnar deviation, and 10-degree radial deviation) according to Palmer et al.21 The percentage of radiological loosening was relatively low and similar in rheumatoid and non-RA wrists (3 and 4%, respectively). The significance of periprosthetic osteolysis without loosening is unclear and needs further investigation. The overall revision rate is lower than those previously reported. The current survival rate of our study exceeds 90% at an average of 4 years of follow-up, both in rheumatoid and non-RA wrists.
In comparison with the first generation metal-polyethylene TWA, our current results suggest a significant improvement in terms of survival rate for revision (Table 2). In comparison with the few articles6,7,8 reporting the results of new generation TWA, our results are based on much larger groups of patients, which allowed analyzing rheumatoid and non-RA wrists, separately, for the first time. Indeed, these are very different categories of patients with very different lives, prognoses, and functional needs. The survival rates of these two groups were surprisingly high and similar (Table 3).
Table 2. Comparisons of Survival Rates between the First and the Last Generation TWA.
| Name of TWA | Survival Rate for Revision at Maximal Follow-Up | |
|---|---|---|
| Cobb and Beckenbaugh22 | Biaxial | 83% at 10 years |
| Meuli23 | Meuli | 77% at 10 years |
| Takwale et al9 | Biaxial | 83% at 8 years |
| Krukhaug et al2 | Biaxial | 77% at 10 years |
| Current study | ReMotion (new generation) | 92% at 8 years |
TWA, total wrist arthroplasty.
Table 3. Comparisons of Survival Rates within New Generation TWA Series.
| Ratio Rheumatoid/Nonrheumatoid Etiologies | Survival Rate for Revision at Average Follow-Up | ||
|---|---|---|---|
| Ward et al8 | UTW1 | 24/0 | 60% at 7 years |
| Ferreres et al6 | UTW2 | 14/7 | 100% at 5.5 years |
| Herzberg7 | ReMotion | 13/6 | 100% at 2.8 years |
| Current series | ReMotion | 129/86 | RA: 96% at 4 years Non-RA: 92% at 4 years |
TWA, total wrist arthroplasty; UTW, Universal total wrist; RA, rheumatoid arthritis.
This study has limitations. It is a multicenter study, and the current follow-up is only a midterm follow-up. The radiographs were not gathered electronically and the radiological criteria were based on surgeon's judgment. This may have led to slightly different interpretations. The strengths of this study are the homogeneous recording into the database, the automatic update of statistics, and the large number of patients, which allows for the first time to individualize a consistent non-RA group of patients.
Our study suggests that the ReMotion TWA is feasible in the midterm and may be used in selected non-RA patients. Our results need to be confirmed at a longer follow-up.
Footnotes
Conflict of Interest There was no conflict of interests from any of the authors of this article.
References
- 1.Trail I A, Stanley J K. Philadelphia, PA: Lippincott Williams & Wilkins; 2010. Total wrist arthroplasty; pp. 457–471. [Google Scholar]
- 2.Krukhaug Y, Lie S A, Havelin L I, Furnes O, Hove L M. Results of 189 wrist replacements. A report from the Norwegian Arthroplasty Register. Acta Orthop. 2011;82(4):405–409. doi: 10.3109/17453674.2011.588858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rizzo M, Ackerman D B, Rodrigues R L, Beckenbaugh R D. Wrist arthrodesis as a salvage procedure for failed implant arthroplasty. J Hand Surg Eur Vol. 2011;36(1):29–33. doi: 10.1177/1753193410376283. [DOI] [PubMed] [Google Scholar]
- 4.Harlingen D Heesterbeek P JC, J de Vos M. High rate of complications and radiographic loosening of the biaxial total wrist arthroplasty in rheumatoid arthritis: 32 wrists followed for 6 (5–8) years Acta Orthop 2011826721–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cavaliere C M, Chung K C. A systematic review of total wrist arthroplasty compared with total wrist arthrodesis for rheumatoid arthritis. Plast Reconstr Surg. 2008;122(3):813–825. doi: 10.1097/PRS.0b013e318180ece3. [DOI] [PubMed] [Google Scholar]
- 6.Ferreres A, Lluch A, Del Valle M. Universal total wrist arthroplasty: midterm follow-up study. J Hand Surg Am. 2011;36(6):967–973. doi: 10.1016/j.jhsa.2011.03.034. [DOI] [PubMed] [Google Scholar]
- 7.Herzberg G. Prospective study of a new total wrist arthroplasty: short term results. Chir Main. 2011;30(1):20–25. doi: 10.1016/j.main.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 8.Ward C M, Kuhl T, Adams B D. Five to ten-year outcomes of the Universal wrist arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2011;93(10):914–919. doi: 10.2106/JBJS.H.01614. [DOI] [PubMed] [Google Scholar]
- 9.Takwale V J, Trail I A, Stanley J K. Biaxial total wrist replacements in patients with rheumatoid arthritis. J Bone Joint Surg Br. 2002;84(5):692–699. doi: 10.1302/0301-620x.84b5.12276. [DOI] [PubMed] [Google Scholar]
- 10.Radmer S, Andresen R, Sparmann M. Wrist arthroplasty with a new generation of prostheses in patients with rheumatoid arthritis. J Hand Surg Am. 1999;24(5):935–943. doi: 10.1053/jhsu.1999.0935. [DOI] [PubMed] [Google Scholar]
- 11.Radmer S, Andresen R, Sparmann M. Total wrist arthroplasty in patients with rheumatoid arthritis. J Hand Surg Am. 2003;28(5):789–794. doi: 10.1016/s0363-5023(03)00307-1. [DOI] [PubMed] [Google Scholar]
- 12.Herren D B, Simmen B R. Limited and complete fusion of the rheumatoid wrist. J Am Soc Surg Hand. 2002;2:21–32. [Google Scholar]
- 13.Herzberg G. Management of bilateral advanced rheumatoid wrist destruction. J Hand Surg Am. 2008;33(7):1192–1195. doi: 10.1016/j.jhsa.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 14.Adams B D, Grosland N M, Murphy D M, McCullough M. Impact of impaired wrist motion on hand and upper-extremity performance(1) J Hand Surg Am. 2003;28(6):898–903. doi: 10.1016/s0363-5023(03)00424-6. [DOI] [PubMed] [Google Scholar]
- 15.De Smet L, Truyen J. Arthrodesis of the wrist for osteoarthritis: outcome with a minimum follow-up of 4 years. J Hand Surg [Br] 2003;28(6):575–577. doi: 10.1016/s0266-7681(03)00208-0. [DOI] [PubMed] [Google Scholar]
- 16.Meads B M, Scougall P J, Hargreaves I C. Wrist arthrodesis using a Synthes wrist fusion plate. J Hand Surg [Br] 2003;28(6):571–574. doi: 10.1016/s0266-7681(03)00146-3. [DOI] [PubMed] [Google Scholar]
- 17.Barbier O, Saels P, Rombouts J J, Thonnard J L. Long-term functional results of wrist arthrodesis in rheumatoid arthritis. J Hand Surg [Br] 1999;24(1):27–31. doi: 10.1016/s0266-7681(99)90015-3. [DOI] [PubMed] [Google Scholar]
- 18.Trieb K. Treatment of the wrist in rheumatoid arthritis. J Hand Surg Am. 2008;33(1):113–123. doi: 10.1016/j.jhsa.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 19.Adey L, Ring D, Jupiter J B. Health status after total wrist arthrodesis for posttraumatic arthritis. J Hand Surg Am. 2005;30(5):932–936. doi: 10.1016/j.jhsa.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 20.Sauerbier M, Kluge S, Bickert B, Germann G. Subjective and objective outcomes after total wrist arthrodesis in patients with radiocarpal arthrosis or Kienböck's disease. Chir Main. 2000;19(4):223–231. doi: 10.1016/s1297-3203(00)73484-6. [DOI] [PubMed] [Google Scholar]
- 21.Palmer A K, Werner F W, Murphy D, Glisson R. Functional wrist motion: a biomechanical study. J Hand Surg Am. 1985;10(1):39–46. doi: 10.1016/s0363-5023(85)80246-x. [DOI] [PubMed] [Google Scholar]
- 22.Cobb T K, Beckenbaugh R D. Biaxial total wrist arthroplasty. J Hand Surg Am. 1996;21(6):1011–1021. doi: 10.1016/S0363-5023(96)80309-1. [DOI] [PubMed] [Google Scholar]
- 23.Meuli H C. Total wrist arthroplasty. Experience with a noncemented wrist prosthesis. Clin Orthop Relat Res. 1997;(342):77–83. [PubMed] [Google Scholar]