Abstract
Purpose Total wrist arthroplasty (TWA) is an evolving procedure for the treatment of arthritis of the wrist joint. The purpose of this study is to compare outcomes of three different total wrist implants.
Methods A retrospective review of the Biaxial, Universal 2, and Re-Motion total wrist arthroplasties was performed. Patients were evaluated for clinical outcome, radiographic analysis, review of complications (incidence and type), and conversion to wrist fusion. Patient function measures included: the Mayo wrist score, the Patient Related Wrist Evaluation, and Disabilities of Arm, Shoulder, and Hand (DASH) score.
Results Forty-six wrist implants were performed in 39 patients. There were 36 rheumatoid and 10 posttraumatic cases. The average follow-up was 6 years (3.5 to 15). The total wrist inserted included 16 resectional arthroplasties (Biaxial) and 30 resurfacing designs (Universal 2 and Re-Motion). Nine implant failures were noted. Causes for arthroplasty failure included distal component implant loosening and wrist instability. Salvage procedures included revision TWA or wrist fusion. In successful cases, flexion and extension motion averaged 30 and 38 degrees, respectively, and grip strength improved by 3 kg. Mayo wrist scores, in successful cases, increased from 40 (preoperative) to 76 (postoperative). The Mayo wrist scores for posttraumatic conditions averaged 87 points versus 71 points for rheumatoid arthritis. The average DASH score for the two resurfacing designs were 20 and 37, and 48 for the resectional arthroplasty design.
Discussion Total wrist replacement maintains itself and provides good pain relief and functional motion in over 80% of all cases and in 97% of resurfacing implants. Better results were correlated with improved distal component fixation and minimal resection of the distal radius.
Level of Evidence Level 3 Case Control
Keywords: arthroplasty, rheumatoid, total wrist, joint
Total wrist arthroplasty (TWA) can provide the motion, strength, and the stability needed to perform activities of daily living.1,2,3 Clinical series reporting on total wrist arthroplasty, however, have been limited. Problems related to implant loosening and instability have limited the clinical application of TWA.3,4,5,6,7 Wrist arthroplasty provides the potential of improving hand strength secondary to maximizing resting muscle tension as well as better positioning the hand for functional use in daily activities. Total wrist arthroplasty has traditionally required large bone resection from the carpus and distal radius, and the results have been fraught with difficulties including proximal and distal component prosthetic loosening and instability4,5,6,7,8,9,10,11 New designs for TWA that are lower profile and more anatomic and utilize minimal bone resection and a resurfacing arthroplasty concept are now available. Comparative studies of older-generation implants and newer resurfacing implants have not been performed. For clarification, in our study we refer to the Biaxial wrist system as a resectional arthroplasty due to the larger bone resection required for proper insertion of the implant compared with the newer-generation implants. In this study, we examined a single resectional-based arthroplasty (Biaxial, Depuy Orthopedics, Warsaw, Indiana, USA) with two resurfacing designs (Universal 2, Integra Life Sciences, Plainsboro, New Jersey, USA; and Re-Motion, Avanta, Small Bone Innovation, Morristown, Pennsylvania, USA). Fig. 1 illustrates each implant design.
Fig. 1.
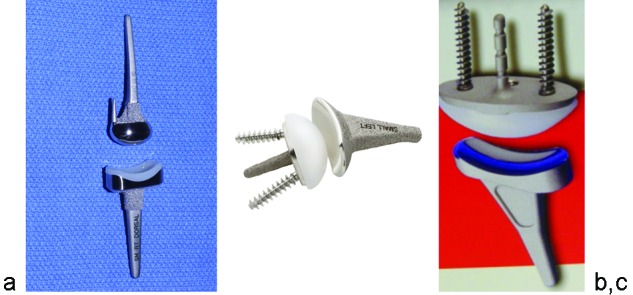
Photographs of the Biaxial total wrist with single proximal and central distal stem (a); the Re-motion total wrist arthroplasty (TWA), in which a proximal radial component articulates with a central polyethylene sphere (b); and the Universal 2 TWA (c).
Over the past decade, a newer generation of wrist implants have been developed that includes minimal resection of the distal radius, preservation of the distal radioulnar joint, and resection of only the proximal carpal row.12,13 More reliable distal fixation of the implant with bone screws is combined with a press-fit radial component. There are currently two implant designs that fit this concept of resurfacing implants: the Universal 2 (Integra Life Sciences) and the Re-Motion (Avanta). These implants consist of a press-fit, bone ingrowth radial component, a central ellipsoidal polyethylene sphere and distal fixation with a central capitate peg and cancellous bone screws. The resection of the distal radius is minimal or absent, allowing preservation of the dorsal and volar radiocarpal ligaments. There is a third implant that utilizes screw fixation distally (Maestro, Biomet, Warsaw, Indiana, USA), but the system requires a more significant distal radius resection than the Universal 2 and Re-Motion.
The resectional arthroplasty has had a recent history of failure whereas reports of resurfacing arthroplasty are limited.12,13,14,15,16 Our hypothesis, based on the clinical experience presented in this study, is that resurfacing arthroplasty will have better clinical results in comparison to resectional arthroplasty. This hypothesis is based on the principles that the resurfacing implants will be more reliable with fewer complications of prosthetic loosening because there is less amount of bone removed and the dorsal and volar carpal ligaments are preserved for load sharing. In addition, due to relative abundance of residual bone, salvage options such as revision arthroplasty or arthrodesis may be favorable with resurfacing designs.
The purpose of this study is to report our institution's experience with resectional arthroplasty versus resurfacing arthroplasty. The study has formal approval of the orthopedic research committee and the institutional review board at our institution. Conflict of interest was reviewed and approved by the institutional conflict of interest and medical-industry relations committees.
Methods and Materials
The patients were identified for inclusion in this study by our institutional total joint registry database. Between the years of 1994 to 2006, there were a total of 39 patients with 47 total wrist replacements identified. One of the implants included the Maestro design and was excluded from the study and analysis. Thus, a total of 46 implants in 39 patients were included for this study. The patients were reviewed with respect to motion, strength, and survivorship (successful retention) of the implant as well as subjective clinical outcome. Surgeries were performed by one of five orthopedic trained hand surgeons at a single institution, and the implant chosen was at the discretion of the senior surgeon. It should be noted that not all implants were available at the same time. The Biaxial was initially available, followed by the Universal 2 and Re-Motion. The Universal 2 and Re-Motion were available at approximately the same time. Patients were evaluated preoperatively and postoperatively by the orthopedic hand surgery staff and for follow-up assessment contacted by a clinical coordinator with request to complete a questionnaire letter and/or contacted by phone for follow-up data from the Total Joint Registry. Outcomes were assessed with the Mayo wrist score, the Disability of Arm, Shoulder, and Hand (DASH) score, and Patient Related Wrist Evaluation (PRWE).13,17,18,19 Full subjective data assessment was limited to 30 patients because not all patients were available for follow-up.
There were 28 women and 11 men in the study with an average age of 57 years (range 33 to 80 years; Table 1). Diagnoses included 10 wrists (10 patients) with posttraumatic arthritis and 36 wrists (29 patients) with rheumatoid arthritis. Major wrist surgeries performed prior to total wrist replacement included 4 partial and 2 complete wrist fusions, 2 previous wrist soft tissue arthroplasties, 2 proximal row carpectomies, and 1 prior open wrist synovectomy.
Table 1. Patient demographics.
| Patient population | |
| Males | 11 |
| Females | 28 |
| Patient age (range) | 57 (33–80) |
| Diagnoses | |
| Rheumatoid arthritis | 35 |
| Posttraumatic arthritis | 11 |
| Treated extremity | |
| Left | 23 |
| Right | 23 |
| Dominant extremity | |
| Left | 6 |
| Right | 40 |
Clinical information recorded included implant type, date of surgery, range of motion, and strength (Table 2). Pain was recorded on a visual analog scale (VAS) score of 1 to 10 along with the range of wrist motion and grip strength. Assessment by the Wrightington radiographic score of the patients with rheumatoid arthritis demonstrated type III (N = 9) and type IV (N = 27) joint disease involvement.20 Patients were evaluated for radiographic loosening of the distal and proximal prosthetic components using the method described by Cobb and Beckenbaugh.15
Table 2. Patient-by-patient specific data.
| Patient | Implant type | Pre-op F/E | Pre-op R/U | Post-op F/E |
Post-op R/U |
Post-op grip (kg) |
|---|---|---|---|---|---|---|
| 1 | Biaxial | 10/40 | 5/20 | 25/50 | 5/10 | 8 |
| 2 | Biaxial | 50/40 | 0/20 | 25/50 | 5/10 | 5 |
| 3 | Biaxial | 60/50 | 20/40 | Fused | – | 3 |
| 4 | Biaxial | 20/50 | 15/10 | Fused | – | 7 |
| 5 | Biaxial | 28/48 | 3/15 | 10/30 | 0/15 | 6 |
| 6 | Biaxial | 30/35 | 10/35 | 42/45 | 10/30 | 42 |
| 7 | Biaxial | 30/50 | 15/0 | Fused | – | |
| 8 | Biaxial | 20/45 | 10/15 | 30/37 | 10/25 | 9 |
| 9 | Biaxial | 52/30 | 15/20 | 60/29 | 20/24 | 14 |
| 10 | Biaxial | 50/55 | 10/30 | 20/44 | 15/21 | 19 |
| 11 | Biaxial | 18/40 | 10/15 | 25/35 | 2/16 | 6 |
| 12 | Biaxial | 45/−10 | −10/15 | 33/42 | 10/28 | 5 |
| 13 | Biaxial | 30/45 | 10/30 | Fused | – | 15 |
| 14 | Biaxial | 26/43 | 6/22 | 31/43 | 7/24 | 12 |
| 15 | Biaxial | 30/35 | 10/20 | Fused | – | – |
| 16 | Biaxial | Fused | – | Fused | – | – |
| 17 | Re-Motion | 28/38 | 10/25 | 55/45 | 15/40 | 30 |
| 18 | Re-Motion | 24/−10 | 0/10 | 24/33 | −2/18 | 12 |
| 19 | Re-Motion | 55/47 | 20/30 | 12/37 | 0/27 | 6 |
| 20 | Re-Motion | 42/26 | 5/15 | 15/20 | 5/10 | 25 |
| 21 | Re-Motion | 33/22 | 12/25 | 33/42 | 5/22 | 14 |
| 22 | Re-Motion | 65/45 | 25/25 | 44/34 | 17/31 | 14 |
| 23 | Re-Motion | 50/50 | 15/30 | 20/33 | 6/14 | 18 |
| 24 | Re-Motion | 25/44 | 15/20 | 20/50 | 5/10 | – |
| 25 | Re-Motion | 28/34 | 10/40 | 20/45 | 7/25 | 20 |
| 26 | Re-Motion | 18/48 | 11/21 | 20/25 | 10/15 | 4 |
| 27 | Re-Motion | 60/40 | 10/35 | 35/33 | 8/24 | 12 |
| 28 | Re-Motion | 27/31 | 6/15 | 10/40 | 5/10 | – |
| 29 | Re-Motion | 30/20 | 0/20 | 10/35 | 0/15 | 2 |
| 30 | Re-Motion | 30/42 | 15/20 | 40/27 | 5/20 | 11 |
| 31 | Re-Motion | 40/45 | 15/15 | 20/45 | 5/20 | 8 |
| 32 | Re-Motion | 31/35 | 29/25 | 45/25 | 5/20 | 10 |
| 33 | Re-Motion | 45/35 | 10/20 | 35/40 | 10/20 | – |
| 34 | Re-Motion | 55/45 | 10/20 | 50/45 | 10/25 | – |
| 35 | Re-Motion | 63/40 | 15/30 | 40/50 | 20/0 | – |
| 36 | Re-Motion | 35/70 | 5/40 | 20/56 | 11/20 | – |
| 37 | Re-Motion | 33/42 | 10/22 | 40/50 | 10/40 | 18 |
| 38 | Re-Motion | Fused | – | 20/30 | 5/15 | 20 |
| 39 | Universal 2 | 20/40 | 33/0 | 25/25 | 6/30 | 8 |
| 40 | Universal 2 | 40/40 | 10/25 | 35/35 | 6/25 | 19 |
| 41 | Universal 2 | 51/52 | 16/19 | 20/20 | 15/20 | 12 |
| 42 | Universal 2 | 26/43 | 6/22 | 30/37 | 5/5 | 10 |
| 43 | Universal 2 | 65/30 | 0/21 | Fused | – | 20 |
| 44 | Universal 2 | 28/50 | 5/12 | 35/48 | 2/10 | 3 |
| 45 | Universal 2 | 40/30 | 12/25 | 33/34 | 21/33 | 8 |
| 46 | Universal 2 | 20/15 | 10/20 | 20/20 | 0/15 | – |
Abbreviations: F/E, flexion extension; R/U, radial ulnar.
All surgical procedures were performed under axillary block anesthesia with sedation under tourniquet control. Biplanar imaging was used during the procedures to confirm proper reaming of the distal radius and preparation of the carpus for implant placement. In advanced rheumatoid arthritis, the distal component radial screw or rod was inserted across the second carpal metacarpal joint, the central peg was placed into the capitate or across the carpometacarpal joint into the third metacarpal, and the ulna screw or peg was placed within the hamate or across the fourth carpometacarpal joint, depending in part on the type of implant being inserted. After reflection of the extensor retinaculum, an extensor tendon synovectomy was performed in rheumatoid patients. The distal radius was completely resected with the Biaxial wrist, partially resected for the Universal 2 total wrist, and preserved with the Re-Motion total wrist. The proximal prosthesis component was press fit in 38 implants, fixed with bone cement in 2 components (Biaxial total wrist), and augmented with bone graft (or bone substitute) in 5 cases (3 Biaxial and 2 Re-Motion total wrists).
For the implantation of the distal component, the proximal carpal row and portions of distal carpal row was resected. Less carpal bone resection was generally performed with the Universal 2 and Re-Motion total wrist than with the Biaxial implant. In most cases, the proximal row (proximal scaphoid, lunate, and triquetrum) and base of the capitate were excised. The distal carpal row (distal scaphoid, capitate, and hamate) were preserved and intercarpal fusion performed during the procedure.
For distal fixation, the Biaxial implant used a central stem with two adjacent pegs or two peripheral stems inserted into the second, third, or fourth metacarpals. A central sintered peg placed in the capitate was combined with two peripheral cancellous bone screws in the Universal 2 and Re-Motion implants. Bone cement was used distally in 11 of the 16 Biaxial implants. Bone cement was not used in any of the Universal 2 or Re-Motion distal component implants.
The distal ulna was resected in 28 cases (all with rheumatoid arthritis), replaced with an ulna head implant in 3 cases, and fused with proximal pseudarthrosis in 1 case. The distal ulna was not addressed in the remaining 13 wrists. Intra-operative complications were recorded. Postoperatively, immobilization of the wrist and forearm (long arm cast or splint) was performed in all cases for an average of 2 weeks.
The data are summarized descriptively using counts and percentages for categorical data and means and standard deviations for continuous data. The DASH and PRWE outcomes were compared between the three types of implants using analysis of variance. Similar analysis was performed to compare the DASH and PRWE between the subset of patients whose implant failed and those with successful implants. All statistical tests were two-sided and p-values less than 0.05 were considered statistically significant.
Figs. 2, 3, and 4 illustrate clinical cases of the Biaxial, Universal 2, and Re-motion wrists.
Fig. 2.

Preoperative posteroanterior (a) and lateral (b) and postoperative posteroanterior (c) and lateral (d) radiographs of a patient who underwent total wrist arthroplasty with the Biaxial implant. Note the press-fit proximal component and the use of bone cement distally.
Fig. 3.
Clinical example of a preoperative posteroanterior (a) and lateral (b) and postoperative posteroanterior (c) and lateral (d) radiographs of a patient who underwent total wrist arthroplasty with the Universal 2 implant.
Fig. 4.

The Re-Motion total wrist. Preoperative posteroanterior (a) and lateral (b) and postoperative posteroanterior (c) and lateral (d) clinical example radiographs of implant inserted. It is press fit into the distal radius and peripheral screw fixation with central peg secures the carpal component.
Results
A stable wrist within a physiologic range of motion28 and reasonable strength was obtained in 22 of 22 Re-motion total wrists, in 7 of 8 Universal 2 total wrists, and in 8 of 16 Biaxial total wrists. The VAS score improved from mean of 7 preoperatively to 2.3 at follow-up. Pain was improved in all patients with a successful wrist implant replacement, N = 39, with no pain in 32 wrists and mild pain in 7 wrists.
A successful retention of the original total wrist implant was present in 97% of the resurfacing implants and in 50% of the resectional implants. Complications leading to failure of the total wrist included distal loosening in 7 wrists and 2 with carpal instability. There were 9 failures: 8 with Biaxial arthroplasties, and 1 with Universal 2. The average time to revision was 78.5 months with a range of 21 to 153 months. One loose Biaxial was successfully salvaged with a Universal 2 total wrist. Two Biaxial arthroplasties with instability were salvaged by revision of the distal component. Five of the 7 Biaxial wrists with distal loosening ultimately required wrist fusion. Clinical loosening of the distal or proximal implant was present in only 1 of the Universal 2 implants and none of the Re-Motion implants. The Universal 2 that failed secondary to clinical loosening was revised to an arthrodesis. Intra-operative complications were recorded in 4 cases. They were partial laceration of the extensor carpi radialis brevis tendon (N = 3) and a stable distal radius fracture (N = 1), each treated by repair during the surgical procedure.
The total range of motion in the successful total wrists averaged 38 degrees of extension, 30 degrees of flexion, with 8 degrees of radial and 20 degrees of ulnar deviation. Pronation averaged 75 degrees and supination 70 degrees. There was no statistical difference in the range of motion between the successful resectional arthroplasty and the resurfacing arthroplasty designs. The change of range of motion from preoperative measures was also not statistically significant. Motion was better in patients after total wrist replacement for posttraumatic arthritis in comparison to those with rheumatoid arthritis. For all participants where data was available, grip strength mean was 13 kg and improved 3 kg from preoperative measures.
Although not completed by every participant in the study, average DASH and PRWE scores are presented in Tables 3 and 4. Although a trend suggested better subjective scores for the Universal 2 and Re-Motion wrist implants with both the DASH and PRWE, none of the comparisons were statistically significant.
Table 3. Postoperative DASH statistical comparison.
| Total N = 30 | Number | Mean |
|---|---|---|
| Universal 2 | 8 | 20 |
| Biaxial | 8 | 48 |
| Re-Motion | 16 | 37 |
Notes: Excludes wrist fusions; p-value = 0.07; r2 = 0.24.
Table 4. Postoperative PRWE statistical comparison.
| Total N = 30 | Number | Mean |
|---|---|---|
| Universal 2 | 8 | 25 |
| Biaxial | 8 | 40 |
| Re-Motion | 16 | 32 |
Notes: Excludes wrist fusions; p-value = 0.65; r2 = 0.05.
In addition to the DASH and PWRE subjective scores reported earlier, Mayo wrist scores were tabulated. The average Mayo wrist score increase was 40 points in successful arthroplasty over preoperative assessment. Excluding the wrist fusions cases, the average Mayo wrist score was 78 points. The Universal 2 wrist score was 77 points (mean) and 82 (mode) (range 65 to 90); the Biaxial wrist score was 73 points (mean) and 75 points (mode) (range 50 to 95); and Re-Motion wrist score was 80 points (mean) and 82 points (mode) (range 50 to 100). The cases of posttraumatic arthritis score averaged 87 points versus the rheumatic arthritis score of 72 points. Resurfacing arthroplasty score was 79 versus 73 points for resectional arthroplasty. Wrist fusion scores averaged 45 points.
Discussion
The development of TWA has been an evolving process. Initial implants were ball and socket designs with intramedullary stems placed into the distal radius and hand metacarpal bones. Wide resection of the radius was performed for most early designs, and bone cement was often required for fixation.3,4,5,6,9 Volz proposed an ellipsoidal design with a proximal polyethylene articulation (backed by metal) and metal distal component with two distal prongs.5 Results from these implants proved unsuccessful due to implant loosening and instability.6,7,8,21,22
The Biaxial total wrist was a further advance on the concept of ellipsoidal articulation. This implant design consisted of a proximal radial stem component for bone ingrowth that was covered distally with a concave polyethylene articulation.13,23 It articulated with the ellipsoidal distal component, which was originally held with a central long stem and two peripheral pegs. Early clinical trials showed improvement in pain and good clinical function, but longer follow-up revealed distal stem loosening that resulted in the need for revision of the carpal component.14,15,16,24
Resurfacing implant designs for total wrist replacement apply similar concepts that limit resection of the distal radius, preserving the distal radioulnar joint and dorsal and volar wrist support ligaments.2,12,13,27 One major advantage of both the tested resurfacing implants appears to be the Menon concept of screw fixation of the distal component.25 To date, this distal fixation appears to limit the risk of prosthetic loosening in all but the most osteoporotic rheumatoid cases, in which total wrist is not indicated or in which bone cement should be considered. This current study shows that this is less of a problem with the resurfacing designs.
Clinical studies related to outcomes of the resurfacing total wrist arthroplasty reported in this study are limited to date. Most reports detail the principles of wrist implant surgery and the operative technique.12,13,25 With respect to other studies of total wrists, several past-published reports focus on prostheses that are no longer manufactured.3,4,5,6,8,9,21 The Biaxial implant results demonstrated reasonable early results but eventual problems with implant loosening.14,15,23,24 From the United Kingdom, Wrightington Orthopedic center, Takwale et al reported success in 83% of total wrist cases using Kaplan Meier survival curves using revision surgery as the end point at 8 years, but eventually noted failure of 36% of Biaxial total wrists due to distal stem loosening.16
In 2002, Divelbiss et al reported encouraging short-term results, with only 3 of 22 arthroplasties requiring revision using the Universal II wrist implant.26 This design incorporated the potential for bone in growth proximally and distally and improved prosthetic balance with more variety of the polyethylene articulation spheres and a deeper radial cup. As with other implant systems, problems occurred in patients with advanced synovitis (wet type rheumatoid disease) including dorsal carpal instability and radial implant subsidence.2,3,26 In 2010, van Winterswijk and coauthors report similar findings with 1 of 17 Universal 2 total wrist arthroplasties needing revision due to distal component loosening at 2- to 6-year follow-up.27
In this study, a resectional arthroplasty (Biaxial total wrist) is compared with two resurfacing arthroplasties (Universal 2 and Re-Motion). The Biaxial wrist was noted to provide excellent proximal fixation in the distal radius without incidence of prosthetic loosening but distal component fixation and instability occurred in 8 of 16 wrists. Problems related to total wrist replacement include implant loosening and instability of the wrist. These are uncommonly noted in the resurfacing total wrist implants reviewed, but our follow-up is relatively short (3.5 to 6 years). One of nine Universal 2 implants had distal stem loosening and instability requiring wrist fusion in a case of advanced rheumatoid arthritis, similar to what has been previously reported.26
The best results in this series occurred in well-controlled cases of rheumatoid arthritis and posttraumatic arthritis. The DASH and PWRE scores were best with the Universal 2 implant, although not statistically significant in comparison to the Re-Motion wrist. All three total wrist designs demonstrated Mayo wrist scores that improved from preoperative measures excluding cases of wrist fusion. In this study, we present promising improvement with resurfacing implants and believe that total wrist replacement, in our opinion, provides a reasonable treatment option in properly selected patients.
There are several limitations to this study. It is a retrospective study with data collected in an institutional total joint registry. The assessment and data are exclusively from one medical center. The authors want to clearly note that one of the authors is a co-designer of the Re-Motion implant. However, the data was assessed independently by a hand fellow, another independent hand surgeon, and by separate statistical review in an effort to provide accurate reporting. Additional limitations of this study are related to lack of preoperative DASH and PRWE scores in all patients and the inability to examine every patient in follow-up for physical and X-ray exams. Multiple attempts were performed to reach all patients by phone and/or questionnaire to determine reported outcomes. The follow-up range of 3.5 to 10 years in the life of a joint implant is short, and long-term studies are needed to evaluate evidence of implant failures.
The long term success of total wrist replacement remains uncertain, but newer implants offer encouragement in this process and, to date, a high level of patient satisfaction. However, should these implants fail, as they may, wrist fusion should provide a good option for salvage due to the fact that these resurfacing implants resect minimal carpal bone stock and distal radius.
References
- 1.Swanson A B Flexible implant arthroplasty for arthritic disabilities of the radiocarpal joint. A silicone rubber intramedullary stemmed flexible hinge implant for the wrist joint Orthop Clin North Am 1973. Apr;42383–394. [PubMed] [Google Scholar]
- 2.Adams B D. Total wrist arthroplasty. Orthopedics. 2004;27(3):278–284. doi: 10.3928/0147-7447-20040301-12. [DOI] [PubMed] [Google Scholar]
- 3.Meuli H C. Arthroplasty of the wrist. Clin Orthop Relat Res. 1980;149(149):118–125. [PubMed] [Google Scholar]
- 4.Meuli H C, Fernandez D L. Uncemented total wrist arthroplasty. J Hand Surg Am. 1995;20(1):115–122. doi: 10.1016/S0363-5023(05)80069-3. [DOI] [PubMed] [Google Scholar]
- 5.Volz R G. Total wrist arthroplasty: a new approach to wrist disability. Clin Orthop Relat Res. 1977;128(128):180–189. [PubMed] [Google Scholar]
- 6.Figgie H E III, Ranawat C S, Inglis A E, Straub L R, Mow C. Preliminary results of total wrist arthroplasty in rheumatoid arthritis using the Trispherical total wrist arthroplasty. J Arthroplasty. 1988;3(1):9–15. doi: 10.1016/s0883-5403(88)80048-2. [DOI] [PubMed] [Google Scholar]
- 7.Cooney W P III, Beckenbaugh R D, Linscheid R L. Total wrist arthroplasty. Problems with implant failures. Clin Orthop Relat Res. 1984;187(187):121–128. [PubMed] [Google Scholar]
- 8.Vogelin E, Nagy L. Fate of failed Meuli total wrist arthroplasty. J Hand Surg [Br] 2003;28(1):61–68. doi: 10.1054/jhsb.2002.0812. [DOI] [PubMed] [Google Scholar]
- 9.Alnot J Y Guepar's total arthroplasty of the wrist in rheumatoid polyarthritis [in French]. Acta Orthop Belg 1988542178–184. [PubMed] [Google Scholar]
- 10.Rahimtoola Z O, Hubach P. Total modular wrist prosthesis: a new design. Scand J Plast Reconstr Surg Hand Surg. 2004;38(3):160–165. doi: 10.1080/02844310310023945. [DOI] [PubMed] [Google Scholar]
- 11.Rahimtoola Z O, Rozing P M. Preliminary results of total wrist arthroplasty using the RWS Prosthesis. J Hand Surg [Br] 2003;28(1):54–60. doi: 10.1054/jhsb.2002.0868. [DOI] [PubMed] [Google Scholar]
- 12.Adams B D. Total Wrist Arthroplasty. J Am Soc Surg Hand. 2001;1:236–249. [Google Scholar]
- 13.Cooney W P, Bussey R, Dobyns J H, Linscheid R L. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987;(214):136–147. [PubMed] [Google Scholar]
- 14.Rettig M E, Beckenbaugh R D. Revision total wrist arthroplasty. J Hand Surg Am. 1993;18(5):798–804. doi: 10.1016/0363-5023(93)90045-5. [DOI] [PubMed] [Google Scholar]
- 15.Cobb T K Beckenbaugh R D Biaxial total-wrist arthroplasty J Hand Surg Am 1996. Nov2161011–1021. [DOI] [PubMed] [Google Scholar]
- 16.Takwale V J, Nuttall D, Trail I A, Stanley J K. Biaxial total wrist replacement in patients with rheumatoid arthritis. Clinical review, survivorship and radiological analysis. J Bone Joint Surg Br. 2002;84(5):692–699. doi: 10.1302/0301-620x.84b5.12276. [DOI] [PubMed] [Google Scholar]
- 17.Hudak P L, Amadio P C, Bombardier C. The Upper Extremity Collaborative Group (UECG) . Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected] Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 18.MacDermid J C, Stratford P. Applying evidence on outcome measures to hand therapy practice. J Hand Ther. 2004;17(2):165–173. doi: 10.1197/j.jht.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 19.MacDermid J C, Turgeon T, Richards R S, Beadle M, Roth J H. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(8):577–586. doi: 10.1097/00005131-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Hodgson S P, Stanley J K, Muirhead A. The Wrightington classification of rheumatoid wrist x-rays: a guide to surgical management. J Hand Surg [Br] 1989;14(4):451–455. doi: 10.1016/0266-7681_89_90168-x. [DOI] [PubMed] [Google Scholar]
- 21.Lorei M P, Figgie M P, Ranawat C S, Inglis A E. Failed total wrist arthroplasty. Analysis of failures and results of operative management. Clin Orthop Relat Res. 1997;342(342):84–93. [PubMed] [Google Scholar]
- 22.Bosco J A III, Bynum D K, Bowers W H. Long-term outcome of Volz total wrist arthroplasties. J Arthroplasty. 1994;9(1):25–31. doi: 10.1016/0883-5403(94)90134-1. [DOI] [PubMed] [Google Scholar]
- 23.Beckanbaugh R D. New York: Churchill-Livingstone; 1993. Arthroplasty of the wrist; pp. 143–187. [Google Scholar]
- 24.Rizzo M, Beckenbaugh R D. Results of biaxial total wrist arthroplasty with a modified (long) metacarpal stem. J Hand Surg Am. 2003;28(4):577–584. doi: 10.1016/s0363-5023(03)00204-1. [DOI] [PubMed] [Google Scholar]
- 25.Menon J. Universal Total Wrist Implant: experience with a carpal component fixed with three screws. J Arthroplasty. 1998;13(5):515–523. doi: 10.1016/s0883-5403(98)90050-x. [DOI] [PubMed] [Google Scholar]
- 26.Divelbiss B J, Sollerman C, Adams B D. Early results of the Universal total wrist arthroplasty in rheumatoid arthritis. J Hand Surg Am. 2002;27(2):195–204. doi: 10.1053/jhsu.2002.31728. [DOI] [PubMed] [Google Scholar]
- 27.van Winterswijk P J, Bakx P A. Promising clinical results of the universal total wrist prosthesis in rheumatoid arthritis. Open Orthop J. 2010;4:67–70. doi: 10.2174/1874325001004020067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ryu J Y, Cooney W P III, Askew L J, An K N, Chao E Y. Functional ranges of motion of the wrist joint. J Hand Surg Am. 1991;16(3):409–419. doi: 10.1016/0363-5023(91)90006-w. [DOI] [PubMed] [Google Scholar]



