Abstract
Purpose Proximal row carpectomy is a well-established technique for the management of wrist arthritis; however, patient selection and long-term durability of proximal row carpectomy is still a matter of controversy. Hence, we conducted a systematic review of the English literature to determine the best evidence on long-term outcomes following proximal row carpectomy.
Methods A MEDLINE search using the term “proximal row carpectomy” was performed. A total of 192 studies were identified. All studies with 10 or more years of follow-up were included in the review. Data extracted included patient demographics, indications for surgery, previous surgery, outcome assessment, and information on complications and failures.
Results A total of 147 patients from six studies met the inclusion criteria and were included in the study. The majority of patients were male and involved in manual labor. There was no significant difference between the preoperative and long-term postoperative motion. The weighted mean for postoperative grip strength was 68.4% compared with the contralateral side. Disabilities of the arm, shoulder, and hand; patient-rated wrist examination; and Mayo wrist scores were comparable to those reported for four-corner arthrodesis. There were 21 failures (14.3%) requiring re-operation. Failures were not associated with a specific preoperative diagnosis but distributed among patients with Kienböck disease, scaphoid nonunion advanced collapse, and scapholunate advanced collapse arthritis.
Conclusions This systematic review confirms the long-term durability of proximal row carpectomy when used for the treatment of wrist arthritis. Although radiocapitate arthritis develops over time in most patients, the clinical significance of this finding is undetermined and does not necessarily correlate with failure of proximal row carpectomy. Poorer long-term outcomes are likely to result in patients engaged in heavy manual labor, whereas better outcomes may be obtained in patients undergoing proximal row carpectomy for trauma or earlier-stage Kienböck disease.
Keywords: proximal row carpectomy, outcomes, wrist, arthritis
Degenerative conditions of the wrist often necessitate surgical intervention. Proximal row carpectomy (PRC) is a well-accepted procedure for the treatment of this diagnosis, and has been reported to relieve pain and preserve wrist range of motion and grip strength.1,2,3 However, the literature is conflicted as to the success of this operation over the course of long-term follow-up. Development of arthritis at the radiocapitate articulation may predispose to recurrent pain requiring wrist arthroplasty or arthrodesis.
Although several studies have been published on the outcomes of PRC, very few of these provide long-term follow-up, and only a handful present higher-level evidence to guide selection of patients for surgery. PRC has been recommended for patients with moderate functional demands, whereas four-corner fusion is generally accepted for patients having evidence of midcarpal arthritis or who require greater grip strength postoperatively and perform manual labor.4,5,6 PRC has been stated to provide better postoperative range of motion compared with four-corner fusion,7 whereas other studies suggest that PRC results in decreased4,5 or equivalent6 grip strength when compared with four-corner fusion.
With questions still remaining with regard to patient selection and long-term durability of PRC, we performed a systematic literature review in an attempt to provide data to help guide patient selection and clinical practice. The aim of this study was to review the long-term outcomes of PRC in patients at least 10 years beyond surgery.
Materials and Methods
A MEDLINE database search was performed to identify all English language citations relating to PRC published between 1965 and 2012. In total, 192 citations were identified. The key words used for the search were “proximal” combined with “row” and “carpectomy.” Citations in which the abstract was unclear underwent formal article review. Inclusion criteria were patients who had undergone PRC followed up for a period of at least 10 years. Due to a paucity of high-level studies, such as randomized controlled trials or prospective studies, all case series were included in the analysis.
Data extracted from the studies reviewed included patient demographic information, indications for surgery, previous surgery, outcome assessment, and information on complications and failures. Where common continuous outcome measures were used, we calculated the weighted means. Specifically, age at time of surgery; flexion/extension arc; grip strength; disabilities of the arm, shoulder, and hand (DASH) scores; patient-rated wrist examination (PRWE) scores; and Mayo wrist scores, when available, were pooled together by generating information on the weighted means.
Results
Demographic Information
Six studies fulfilled our inclusion criteria8,9,10,11,12,13; all were retrospective case series that analyzed success of PRC in patients followed for at least 10 years (Table 1). These studies were published between 2003 and 2012 and included 147 patients who underwent proximal row carpectomy for a variety of reasons. The length of follow-up varied within and between different studies and ranged from 10 to 36.3 years. The study by Ali et al8 analyzed data from 81 patients for demographic data but only presented follow-up data on 61 patients. Similarly, the study by Liu et al12 presented demographic data on 12 patients but follow-up data on only 10 patients. Hence, demographic and preoperative data for a total of 169 patients were available.
Table 1. Study characteristics.
| Study, first author | Year | N | Study design | Diagnosis | Mean follow-up, years | Not satisfied/poor satisfaction, N (%) | Reoperation, N (%) |
|---|---|---|---|---|---|---|---|
| Ali8 | 2012 | 61 | Case series | Mixed | 19.8 | 46 (75.4%) | 12 (19.7%) |
| Croog9 | 2008 | 21 | Case series | Kienböck | 10 | 3 (14.3%) | 3 (14.3%) |
| DiDonna10 | 2004 | 22 | Case series | Mixed | 14 | 4 (18.2%) | 4 (18.2%) |
| Jebson11 | 2003 | 20 | Case series | Mixed | 13.1 | 3 (15.0%) | 2 (10.0%) |
| Liu12 | 2009 | 10 | Case series | Mixed | 16.5 | 0 | 0 |
| Lumsden13 | 2008 | 13 | Case series | Kienböck | 15 | 0 | – |
Demographic and preoperative data are presented in Table 2. The weighted mean age of all patients was 39.7 years. The majority of patients were male and involved in occupations that required manual labor. The indications for surgery were as follows: scaphoid nonunion advanced collapse (SNAC) (n = 25 [14.8%]), scapholunate advanced collapse (SLAC) (n = 46 [27.2%]), Kienböck disease (n = 55 [32.5%]), trauma (n = 25 [14.8%]), neuromuscular spasticity (n = 12 [7.1%]) and rheumatoid arthritis (n = 6 [3.6%]). Of the patients who underwent a PRC for trauma, 10 had an old trans-scaphoid perilunate fracture-dislocation, and 2 had a perilunate dislocation. Information on the exact etiology of trauma was not available for 13 patients.8 Patients who underwent a PRC for neuromuscular spasticity were limited to the paper by Ali et al8 and had a wrist flexion deformity from either cerebral palsy or arthrogryposis. Surgery was performed not for wrist pain but to improve wrist extension.
Table 2. Demographic and preoperative data.
| Study, first author | N | Mean age (range) | Male gender (% of total) | Occupation manual labor (% of total) | Extremity dominance(% of total) | Indication for surgery | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| SNAC | SLAC | Kienböck | Trauma | Others | ||||||
| Ali8 | 81 | 41 (10–72) | 53 (65.4%) | 62 (76.5%) | 55 (67.9%) | 8 | 29 | 13 | 13 | 18 |
| Croog9 | 21 | 38 (19–59) | N.S. | 7 (33.3%) | 15 (71.4%) | 0 | 0 | 21 | 0 | 0 |
| DiDonna10 | 22 | 38 (19–57) | N.S. | 10 (45.5%) | 15 (68.2%) | 6 | 9 | 7 | 0 | 0 |
| Jebson11 | 20 | 43 (24–72) | 20 (100%) | 12 (60%) | 11 (55%) | 11 | 8 | 0 | 1 | 0 |
| Liu12 | 12 | 39 (21–54) | 5 (41.7%) | N.S. | 9 (75%) | 0 | 0 | 1 | 11 | 0 |
| Lumsden13 | 13 | 33 (16–44) | N.S. | 7 (53.8%) | N.S. | 0 | 0 | 13 | 0 | 0 |
Abbreviations: N.S., not stated in paper; SLAC, scapholunate advanced collapse; SNAC, scaphoid nonunion advanced collapse.
Outcomes Assessment
Objective outcomes data are presented in Table 3. Patients who had failure of PRC or who were unable to return to the office for examination were excluded from outcomes analysis in three studies.9,10,11 Hence, the pooled number of patients available for analysis was 135. Range of motion at the wrist was inconsistently presented as degrees, percentage of normal status, and percentage of the uninvolved wrist. Preoperative and postoperative information on the flexion/extension arc was available in three studies,8,11,13 with a weighted preoperative mean value of 73.4 degrees and a weighted postoperative mean value of 73.5 degrees. Preoperative and postoperative information on radial/ulnar deviation was available in two studies,8,11 with a weighted preoperative mean value of 32.3 degrees and a weighted postoperative mean value of 31.5 degrees. Grip strength was presented variably in different studies, either as an absolute value or percentage of the contralateral side. Five studies8,9,10,11,13 provided meaningful information on postoperative grip strength compared with the contralateral side, with a weighted mean value of 68.4%.
Table 3. Objective outcome measures.
| Study, first author | N | Flexion/extension arca | Radial/ulnar deviationa | Grip strengtha | |||||
|---|---|---|---|---|---|---|---|---|---|
| Preop (degrees) | Postop (degrees) | Preop (degrees) | Postop (degrees) | Preop (kg) | Postop (kg) | Preop (% contralateral side) | Postop (% contralateral side) | ||
| Ali8 | 61 | 70 | 69.4 | 30.4 | 30.8 | 16.8 | 14.3 | 52 | 48 |
| Croog9 | 18 | N.S. | 105 | N.S. | 42 | N.S. | 35 | N.S. | 87 |
| DiDonna10 | 15 | N.S. | 72 | N.S. | 40 | N.S. | N.S. | N.S. | 91 |
| Jebson11 | 18 | 84b | 77 | 39b | 34 | 19.5c | 29.5 | N.S. | 83 |
| Liu12 | 10 | N.S. | N.S. | N.S. | N.S. | N.S. | N.S. | N.S. | 75–99 |
| Lumsden13 | 13 | 76d | 88 | N.S. | N.S. | 14d | 32 | N.S. | 92 |
Abbreviation: N.S., not stated in paper.
Average values.
n = 17; 1 patient in this series had no information documented.
n = 14; 14 of 18 patients in this series had information available on grip strength.
n = 11; preoperative data available for 11 of 13 patients in this series.
Several scoring systems were also used in three studies (Table 4). The DASH score14 was used in two studies, while the QuickDASH,15 a shortened version of the DASH outcome measure, was used in one study. The PRWE16 and Mayo wrist17 scoring systems were used in two studies. The weighted mean DASH score was 21.5 (n = 79), whereas the weighted mean PRWE score was 28.7 (n = 79) and the weighted mean Mayo wrist score was 66.9 (n = 79).
Table 4. Scoring systems.
| Study, first author | N | DASH score | QuickDASH score | PRWE score | Mayo wrist score |
|---|---|---|---|---|---|
| Ali8 | 61 | 25.2 | – | 32.2 | 61.8 |
| Croog9 | 18 | – | 12 | 17 | 84 |
| DiDonna10 | 18 | 9 | – | – | – |
Abbreviations: DASH, disabilities of the arm, shoulder, and hand; PRWE, patient-rated wrist examination.
Failures
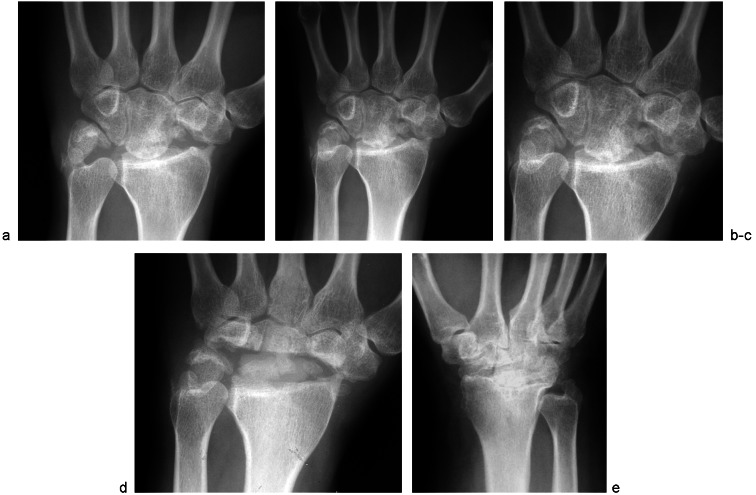
Of 147 patients in the six studies analyzed, there were a total of 21 failures (14.3%) requiring re-operation and conversion to arthrodesis or arthroplasty (Table 5). The average time to failure and reoperation was 53.4 months (range 5 to 240). Failures were evenly divided among a range of wrist pathology, inclusive of Kienböck disease, SNAC, and SLAC wrist (Fig. 1).
Table 5. Failures requiring wrist arthrodesis or arthroplasty.
| Study, first author | Age at PRC (years) | Diagnosis | Occupation | Gender | Time to reoperation (months) | Surgery performed | Previous operations |
|---|---|---|---|---|---|---|---|
| Ali8 | N.S. | Arthrogryposis | N.S. | N.S. | 240 | Arthrodesis | None |
| Croog9 | 38 | Kienböck | Clerk | F | 5 | Arthrodesis | None |
| Croog9 | 31 | Kienböck | MT | M | 11 | Arthrodesis | None |
| Croog9 | 38 | Kienböck | Mechanic | M | 53 | Arthrodesis | None |
| DiDonna10 | 26 | SNAC | Laborer | M | 140 | Arthrodesis | Scaphoid bone graft × 2 |
| DiDonna10 | 28 | Kienböck | Laborer | M | 8 | Arthrodesis | None |
| DiDonna10 | 35 | SNAC | Welder | M | 130 | Arthrodesis | Scaphoid bone graft, styloidectomy |
| DiDonna10 | 25 | Kienböck | Clerk | F | 81 | Arthrodesis | Silicone lunate prosthesis |
| Jebson11 | N.S. | SNAC | N.S. | M | 28 | Arthrodesis | N.S. |
| Jebson11 | N.S. | SLAC | Machinist | M | 40 | Arthrodesis | N.S. |
| Alia (n = 11) | N.S. | Mixed | N.S. | N.S. | Mean 35 | Arthrodesis or arthroplasty | N.S. |
Abbreviations: MT, maintenance technician; N.S., not stated in paper; PRC, proximal row carpectomy; SLAC, scapholunate advanced collapse; SNAC, scaphoid nonunion advanced collapse.
Pooled data listed because individual patient data was not provided in this study.
Fig. 1.
Anterior-to-posterior radiographs of a patient who underwent proximal row carpectomy for scapholunate advanced collapse arthritis in 1979 (a). Over the course of the next 24 months, the patient developed increasing pain in the wrist and deterioration within the head of the capitate (b and c). The proximal row carpectomy was converted to a silicone wrist prosthesis in 1980 (d). Compare part b with part e, which shows the radiocapitate joint in a patient some 15 years after proximal row carpectomy. Despite the advanced arthrosis, this patient did not request a revision procedure for his wrist function or wrist pain.
Radiographic Findings
Radiographic findings were not reported for all patients in the six studies analyzed. Of 82 patients in five studies where radiographic data was available, 65 had evidence of radiocapitate degenerative joint disease (79.3%). The classification described by Culp et al3 in which the degree of radiocapitate arthrosis was divided into minimal, moderate, and severe grades was used in three studies,8,11,13 whereas the severity of radiocapitate arthrosis was classified as partial or complete in two studies.9,10 Where the degree of radiocapitate arthrosis was divided into minimal, moderate, and severe grades, there were 16 patients (43.2%) with minimal arthrosis, 8 (21.6%) with moderate arthrosis, and 13 (35.1%) with severe arthrosis. Where the severity of radiocapitate arthrosis was classified as partial or complete, 17 patients (60.7%) had partial arthrosis and 11 (39.3%) had complete arthrosis. Radiographic changes were not significantly correlate with clinical findings, objective and subjective outcomes measures, or time from proximal row carpectomy.
Discussion
This study confirms the long-term efficacy of proximal row carpectomy for treatment of degenerative conditions of the wrist. We found that a functional arc of wrist motion was maintained as measured by the flexion/extension arc and radial/ulnar deviation in all patients after at least 10 years follow-up.18,19
There was a significant decrease in grip strength, suggesting that PRC may be better suited for patients not involved in heavy manual labor, which has also been mentioned by previous researchers.4,5 Upper extremity function as measured by the DASH and PRWE scores compared favorably with those reported postoperatively following four-corner arthrodesis,20,21,22 confirming that both procedures result in subjectively equivalent functional outcomes when graded by the patient.23,24
A significant proportion of the failures occurred in patients under 35 years of age involved in an active occupation. This likely correlates with increased loading of the wrist leading to early failure and re-operation, as suggested by DiDonna et al.10 It has also been suggested that failures occur more often in patients with Kienböck disease9; however, in this review, failures were evenly distributed among patients with different wrist pathology, suggesting that Kienböck disease does not predispose PRC to failure.
The significance of the radiographic development of radiocapitate arthritis is a matter of debate and has been found to occur uniformly over long-term follow-up.8,9,10,11,13 However, the severity of radiocapitate arthritis has yet to be directly linked to poorer outcomes, pain, or clinical function.8,9,10,11,13,25,26 Although all of the papers reviewed in this study reported radiographic changes in the vast majority of patients, only a small proportion of these required re-operation.
Progressive narrowing and arthrosis of the radiocapitate articulation inevitably occurs as PRC changes a complex carpal articulation to a hinge joint. The capitate was found to have a radius of curvature of only 64% of the lunate fossa on anteroposterior radiographs and 60% on true lateral radiographs.27 Another study using MRI imaging of the cartilaginous surfaces reported an even lower radius of curvature of the capitate compared with the lunate fossa of 37% on anteroposterior view and 57% on lateral view.28 In addition, because the broad contact between scaphoid, lunate, and radius in a normal wrist is compressed to a single radiocapitate articulation after PRC, this results in increased contact pressure, found to be 3.8 times that of the intact wrist within a decreased contact area 21 to 26% that of the intact wrist.29 Due to the discrepancy in shape of the capitate and lunate fossa, the capitate both translates and rotates on the radius.27,29 The translational motion of the capitate on the radius may dissipate load on a specific contact point, resulting in radiologic evidence of arthritis.27,29
The majority of PRC failures appear to occur early, within the first 2 to 3 years following surgery, and are prior to the radiographic development of radiocapitate arthritis. Unexplored factors, which may explain the 14% early failure rate following PRC, may include a discrepancy in the shape of the lunate fossa and capitate shape. Yazaki et al30 described three different capitate shapes, a flat type (65%), spherical type (22%), and V-shaped type (14%). The flat type had a lunate-capitate articulation oriented in a radio-ulnar plane and a scaphoid-capitate articulation oriented in a proximal-distal plane; the spherical type had a concave articulation formed by scaphoid and lunate articulations with an indistinct border between scaphoid and lunate facets; the V-shaped type had separate lunate and scaphoid facets that converged with a distinct inter-facet ridge at the central region of the proximal pole of the capitate. The significance of capitate shape and loading patterns across the lunate facet is still unclear, but it may contribute to early clinical failures or the time to radiographic manifestation of radiocapitate arthrosis in some patients but not others.
Of the papers analyzed in this review, the study by Ali et al8 had the longest follow-up but the greatest subset of patients with unsatisfactory results. In this study, patients had a much higher level of patient dissatisfaction, decreased wrist range of motion, and decreased grip strength, as well as increased DASH and PRWE scores. The proportion of patients involved in manual labor was the highest in this series (76.5%), with the longest average duration of follow-up (19.8 years). Although variations in surgical technique, rehabilitation protocols, and patient characteristics may explain some of the variation in long-term results between different studies, this study does suggest a high number of patients were dissatisfied with their surgical result due to ongoing pain and inability to perform daily activities when followed beyond a decade. Further studies over very long follow-up periods (more than 20 years) may be needed to determine the ultimate durability of PRC.
Conversely, the studies by Liu12 and Lumsden13 reported no failures and a uniformly satisfied cohort on long-term follow-up. The patients in this series had a PRC for either trauma or Lichtman stage II and stage III Kienböck disease. This suggests that careful selection of patients with early Kienböck disease or in the setting of trauma may result in better long-term outcomes following PRC.
As of yet, we have limited long-term (> 10 year) outcome studies evaluating the results of other comparable surgical procedures, such as four-corner fusion or wrist arthroplasty. However, data from shorter-term studies analyzed in a recent systematic review comparing PRC and four-corner fusion31,32 suggests that whereas PRC has an increased rate of osteoarthritic changes, four-corner fusion has more complications overall due to nonunion, dorsal impingement, and hardware problems. PRC and four-corner fusion have not been found to result in differences in subjective and objective outcomes or patient satisfaction.
Adjunctive procedures such as dorsal capsule interposition, proximal capitate excision, radial styloidectomy, or posterior interosseous nerve (PIN) neurectomy have been suggested by some authors to result in improved outcomes following PRC.8,33 Only the study by Ali et al8 found that adjunctive PIN neurectomy resulted in improved PRWE and DASH scores compared with those patients who had only PRC.
This review was limited by the small number of studies with long-term follow-up identified in the literature, all of which were retrospective case series. There were no studies meeting level I or level II evidence with 10-year follow-up. By necessity, this decreases the level of evidence of this systematic review. Unfortunately, the literature on outcomes of PRC consists for the most part of retrospective case series using a variety of clinical scoring systems, which makes comparison between studies difficult. A definitive answer as regards the best indications for PRC and its long-term durability will require further prospective studies, studies with longer follow-up, and further basic science research into the morphology and kinematics of the capitate following PRC.
It appears that PRC is a procedure best suited for individuals greater than 35 years of age and involved in less demanding activities. We would recommend that patients selected for PRC should fulfill these criteria. PRC preserves a functional range of wrist motion (in this systematic review, flexion-extension arc of 73.5 degrees and radial/ ulnar deviation of 31.5 degrees) and can preserve up to 68% of grip strength. Failure rates for this procedure are low, occur early, and occur in approximately 14% of patients. PIN neurectomy at the time of surgery may improve long-term outcomes. All patients should be counseled that radiographic evidence of radiocapitate arthrosis will develop at 10 years following surgery, but this does not necessarily correlate with late failure.
References
- 1.Crabbe W A. Excision of the proximal row of the carpus. J Bone Joint Surg Br. 1964;46:708–711. [PubMed] [Google Scholar]
- 2.Green D P. Proximal row carpectomy. Hand Clin. 1987;3(1):163–168. [PubMed] [Google Scholar]
- 3.Culp R W, McGuigan F X, Turner M A, Lichtman D M, Osterman A L, McCarroll H R. Proximal row carpectomy: a multicenter study. J Hand Surg Am. 1993;18(1):19–25. doi: 10.1016/0363-5023(93)90239-y. [DOI] [PubMed] [Google Scholar]
- 4.Baumeister S Germann G Dragu A Tränkle M Sauerbier M Functional results after proximal row carpectomy (PRC) in patients with SNAC-/SLAC-wrist stage II [in German]. Handchir Mikrochir Plast Chir 2005372106–112. [DOI] [PubMed] [Google Scholar]
- 5.Dacho A K, Baumeister S, Germann G, Sauerbier M. Comparison of proximal row carpectomy and midcarpal arthrodesis for the treatment of scaphoid nonunion advanced collapse (SNAC-wrist) and scapholunate advanced collapse (SLAC-wrist) in stage II. J Plast Reconstr Aesthet Surg. 2008;61(10):1210–1218. doi: 10.1016/j.bjps.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Laulan J, Bacle G, de Bodman C. et al. The arthritic wrist. II—the degenerative wrist: indications for different surgical treatments. Orthop Traumatol Surg Res. 2011;97(4, Suppl):S37–S41. doi: 10.1016/j.otsr.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Mulford J S, Ceulemans L J, Nam D, Axelrod T S. Proximal row carpectomy vs four corner fusion for scapholunate (Slac) or scaphoid nonunion advanced collapse (Snac) wrists: a systematic review of outcomes. J Hand Surg Eur Vol. 2009;34(2):256–263. doi: 10.1177/1753193408100954. [DOI] [PubMed] [Google Scholar]
- 8.Ali M H, Rizzo M, Shin A Y, Moran S L. Long-term outcomes of proximal row carpectomy: a minimum of 15-year follow-up. Hand (NY) 2012;7:72–78. doi: 10.1007/s11552-011-9368-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Croog A S, Stern P J. Proximal row carpectomy for advanced Kienböck's disease: average 10-year follow-up. J Hand Surg Am. 2008;33(7):1122–1130. doi: 10.1016/j.jhsa.2008.02.031. [DOI] [PubMed] [Google Scholar]
- 10.DiDonna M L, Kiefhaber T R, Stern P J. Proximal row carpectomy: study with a minimum of ten years of follow-up. J Bone Joint Surg Am. 2004;86-A(11):2359–2365. [PubMed] [Google Scholar]
- 11.Jebson P JL, Hayes E P, Engber W D. Proximal row carpectomy: a minimum 10-year follow-up study. J Hand Surg Am. 2003;28(4):561–569. doi: 10.1016/s0363-5023(03)00248-x. [DOI] [PubMed] [Google Scholar]
- 12.Liu M, Zhou H T, Yang Z M, Huang F G, Pei F X, Xiang Z. Clinical evaluation of proximal row carpectomy revealed by follow-up for 10–29 years. Int Orthop. 2009;33(5):1315–1321. doi: 10.1007/s00264-009-0770-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lumsden B C, Stone A, Engber W D. Treatment of advanced-stage Kienböck's disease with proximal row carpectomy: an average 15-year follow-up. J Hand Surg Am. 2008;33(4):493–502. doi: 10.1016/j.jhsa.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 14.Hudak P, Amadio P, Bombardier C. The Upper Extremity Collaborative Group (UECG) . Development of an upper extremity outcome measure: the DASH (disability of the arm, shoulder and hand) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 15.Beaton D E, Wright J G, Katz J N. Upper Extremity Collaborative Group . Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87(5):1038–1046. doi: 10.2106/JBJS.D.02060. [DOI] [PubMed] [Google Scholar]
- 16.MacDermid J C, Tottenham V. Responsiveness of the disability of the arm, shoulder, and hand (DASH) and patient-rated wrist/hand evaluation (PRWHE) in evaluating change after hand therapy. J Hand Ther. 2004;17(1):18–23. doi: 10.1197/j.jht.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 17.Cooney W P. London: Martin Dunitz; 1995. Open reduction of distal radius fractures (indications, classifications and functional assessment) pp. 118–125. [Google Scholar]
- 18.Ryu J Y, Cooney W P III, Askew L J, An K N, Chao E Y. Functional ranges of motion of the wrist joint. J Hand Surg Am. 1991;16(3):409–419. doi: 10.1016/0363-5023(91)90006-w. [DOI] [PubMed] [Google Scholar]
- 19.Palmer A K, Werner F W, Murphy D, Glisson R. Functional wrist motion: a biomechanical study. J Hand Surg Am. 1985;10(1):39–46. doi: 10.1016/s0363-5023(85)80246-x. [DOI] [PubMed] [Google Scholar]
- 20.Dacho A, Grundel J, Holle G, Germann G, Sauerbier M. Long-term results of midcarpal arthrodesis in the treatment of scaphoid nonunion advanced collapse (SNAC-Wrist) and scapholunate advanced collapse (SLAC-Wrist) Ann Plast Surg. 2006;56(2):139–144. doi: 10.1097/01.sap.0000194245.94684.54. [DOI] [PubMed] [Google Scholar]
- 21.Espinoza D P, Schertenleib P. Four-corner bone arthrodesis with dorsal rectangular plate: series and personal technique. J Hand Surg Eur Vol. 2009;34(5):609–613. doi: 10.1177/1753193409105684. [DOI] [PubMed] [Google Scholar]
- 22.Merrell G A, McDermott E M, Weiss A P. Four-corner arthrodesis using a circular plate and distal radius bone grafting: a consecutive case series. J Hand Surg Am. 2008;33(5):635–642. doi: 10.1016/j.jhsa.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 23.Nakamura R, Horii E, Watanabe K, Nakao E, Kato H, Tsunoda K. Proximal row carpectomy versus limited wrist arthrodesis for advanced Kienböck's disease. J Hand Surg [Br] 1998;23(6):741–745. doi: 10.1016/s0266-7681(98)80087-9. [DOI] [PubMed] [Google Scholar]
- 24.Cohen M S, Kozin S H. Degenerative arthritis of the wrist: proximal row carpectomy versus scaphoid excision and four-corner arthrodesis. J Hand Surg Am. 2001;26(1):94–104. doi: 10.1053/jhsu.2001.20160. [DOI] [PubMed] [Google Scholar]
- 25.Zhu Y L, Xu Y Q, Ding J, Li J, Chen B, Ouyang Y F. Biomechanics of the wrist after proximal row carpectomy in cadavers. J Hand Surg Eur Vol. 2010;35(1):43–45. doi: 10.1177/1753193409344527. [DOI] [PubMed] [Google Scholar]
- 26.Imbriglia J E. Proximal row carpectomy. Technique and long-term results. Atlas Hand Clin. 2000;5:101–109. [Google Scholar]
- 27.Imbriglia J E, Broudy A S, Hagberg W C, McKernan D. Proximal row carpectomy: clinical evaluation. J Hand Surg Am. 1990;15(3):426–430. doi: 10.1016/0363-5023(90)90054-u. [DOI] [PubMed] [Google Scholar]
- 28.Hawkins-Rivers S, Budoff J E, Ismaily S K, Noble P C, Haddad J. MRI study of the capitate, lunate, and lunate fossa with relevance to proximal row carpectomy. J Hand Surg Am. 2008;33(6):841–849. doi: 10.1016/j.jhsa.2008.02.021. [DOI] [PubMed] [Google Scholar]
- 29.Tang P, Gauvin J, Muriuki M, Pfaeffle J H, Imbriglia J E, Goitz R J. Comparison of the “contact biomechanics” of the intact and proximal row carpectomy wrist. J Hand Surg Am. 2009;34(4):660–670. doi: 10.1016/j.jhsa.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 30.Yazaki N, Burns S T, Morris R P, Andersen C R, Patterson R M, Viegas S F. Variations of capitate morphology in the wrist. J Hand Surg Am. 2008;33(5):660–666. doi: 10.1016/j.jhsa.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 31.Bain G I, Watts A C. The outcome of scaphoid excision and four-corner arthrodesis for advanced carpal collapse at a minimum of ten years. J Hand Surg Am. 2010;35(5):719–725. doi: 10.1016/j.jhsa.2010.01.025. [DOI] [PubMed] [Google Scholar]
- 32.Mulford J S, Ceulemans L J, Nam D, Axelrod T S. Proximal row carpectomy vs four corner fusion for scapholunate (Slac) or scaphoid nonunion advanced collapse (Snac) wrists: a systematic review of outcomes. J Hand Surg Eur Vol. 2009;34(2):256–263. doi: 10.1177/1753193408100954. [DOI] [PubMed] [Google Scholar]
- 33.Diao E, Andrews A, Beall M. Proximal row carpectomy. Hand Clin. 2005;21(4):553–559. doi: 10.1016/j.hcl.2005.08.006. [DOI] [PubMed] [Google Scholar]