Abstract
Background
The aim of this study was to determine the relationship between hematuria and volume, position of stone, and hydronephrosis in patients with a solitary stone, using unenhanced multidetector computed tomography (MDCT).
Material/Methods
This retrospective study evaluated the clinical and radiological records of 83 patients undergoing MDCT for the evaluation of acute flank pain and suspected renal colic, who also underwent a microscopic urinalysis at the emergency department of our hospital during a 1-year period. Inclusion criteria of the MDCT study were solitary urolithiasis and cumulative stone diameter under 1 cm.
Results
A total of 83 patients were included in the study, with a mean age of 42.1±14.4 years; 48 (57.8%) were females and 35 (42.2%) were males. Detection of 5 or more red cells on urinalysis was regarded as microscopic hematuria, and was positive in 46 patients (55.4%). There was a positive correlation between the position of the stone (especially upper two-thirds ureteral stones) and microhematuria rate (r: 0.28, p=0.009). There was a statistically significant difference in presence of hydronephrosis between the microhematuria (36 patients, 78%) and non-microhematuria (12 patients, 32%) groups (p<0.001). The median stone volume between the microhematuria and non-microhematuria groups were not statistically different, 37.5 mm3 (range 5–425) and 28 mm3 (range 4–412), respectively (p=0.39).
Conclusions
Although stone volume is one of the best indicators of stone burden, it was not correlated with microhematuria. However, in patients with renal colic, microhematuria requires ultrasound examination whether hydronephrosis and ureteral stones are present or not. Further studies with larger sample sizes are warranted.
Keywords: renal colic, hematuria, multidetector computed tomography, urolithiasis
Background
Accurate assessment of a patient’s stone burden has an important role in management for urolithiasis [1[. Various radiological tests may be performed for quantification of stone-burden including plain abdominal x-ray, ultrasound (US) or unenhanced multidetector computed tomography (MDCT) [2]. Today CT is the gold standard imaging modality in the work up of suspected renal colic. Ccompared with the other imaging methods, MDCT has the highest sensitivity and specificity to detect stones and it is the most accurate imaging modality to measure stone size [2,3]. Several stone parameters that reflect stone burden, including the cumulative stone diameter (CSD), stone surface area (SA), and volume, have been evaluated for CT imaging of suspected urolithiasis [1]. A recent study showed that among the several parameters regarding the renal stone burden, the 3-dimensional volume measurements could better quantify the stone burden and predict treatment outcomes [1,4].
Microhematuria on urinalysis is frequently used as a diagnostic screening test for urolithiasis [5]. However, there are some concerns about results of the diagnostic comparison value of microhematuria versus radiological studies [5–10]. There are several reasons of inconsistent results, largely due to different urinalysis tests, use of different imaging modalities as gold standard, and differences in the patient populations studied [5–10].
In this study, our aim was to determine the association between hematuria testing and volume, position of stone, and hydronephrosis in patients with a solitary stone on the unenhanced MDCT as the reference standard.
Material and Methods
Following institutional ethics committee approval, unenhanced MDCT studies of 83 patients presenting to the emergency department with flank colic pain during a 1-year period from June 2011 to June 2012 were retrospectively analyzed. Patients who had a solitary stone with calculus size <1 cm at unenhanced MDCT were included. Patients with age under 18 years old, those with vaginal bleeding, those who reported the use of bowel evacuants, phenolphthalein or rifampicin (drugs that affect urinalysis results), and those with more than 1 stone were excluded from the study. Patients who had received lithotripsy before were also excluded.
Examinations were performed with a 4-slice MDCT (HiSpeed; GE Medical Systems, Milwaukee, Wisconsin, USA). Stone protocols were: collimation 2.5 mm, table movement 10 mm, pitch 1, 120 kV, 60–100 mAs, without oral or intravenous contrast medium administration. Three-mm slices from the suprarenal region to the symphysis pubis were obtained.
The position of the stone (upper vs. lower ureter), stone side (right or left), age, sex, and presence of hydronephrosis were recorded for each patient. The stone volume was obtained from measurements on reformatted images of the stone from the raw images at a dedicated CT workstation via a volume analysis program (Voxtool 3.0.54 pi, GE Medical Systems, Milwaukee, Wisconsin, USA) (Figure 1).
Figure 1.
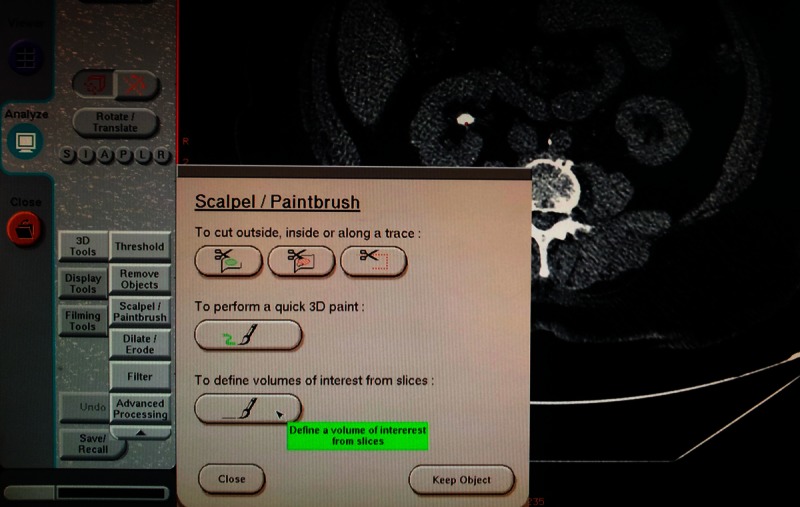
Representation of how to calculate stone volume at a dedicated CT workstation via a volume analysis program.
The results of each patient’s urinalysis for the presence or absence of blood in the urine were obtained from the hospital’s main computer system and recorded if this test was performed within a maximum of 2 hours before the unenhanced MDCT scans. The formal urinalysis included microscopic examination of the urine by a technologist. The urinalysis was classified as positive for hematuria when 5 or more erythrocytes per high power field (RBCs/HPF) were detected. Urine dipstick tests (UDT) are usually performed in our hospital as well, but these results are not always found in the database, so dipstick test results were not evaluated. According to the result of urinalysis, patients were divided into 2 groups: Group I consisted of patients with microhematuria (5 or more RBCs/HPF), and Group II consisted of patients without microhematuria (4 or less RBCs/HPF).
We also analyzed the ultrasound results to determine any possible correlation between hydronephrosis and the position of the stones, as well as the microhematuria rate.
The Mann-Whitney U-test was used for the asymmetric distributed continuous variables. Spearman correlation coefficient was used for the analysis of correlation. Categorical variables were reported as counts and percentage, and the independence was tested by the chi-square test.
Results
The study population was 83 patients, with a mean age of 42.1±14.4 years, and included 48 (57.8%) females and 35 (42.2%) males. In our study population, 46 (55.4%) patients had microhematuria (Group I) and 37 (44.6%) patients were without microhematuria (Group II). Table 1 shows a comparison of the patients’ demographic features and stone measurement outcomes of between the 2 groups.
Table 1.
Comparison of patients and stone data between cases presenting microhematuria and non-microhematuria.
| Group I (patients with microhematuria) | Group II (patients without microhematuria) | p value | |
|---|---|---|---|
| Patients (n, %) | 46 (55.4) | 37 (44.6) | |
| Age (year) | 41.4±15.8 | 42.9±12.5 | 0.64* |
| Sex | 0.138** | ||
| Female | 15 | 18 | |
| Male | 31 | 19 | |
| Stone Side | 0.284** | ||
| Right | 17 | 18 | |
| Left | 29 | 19 | |
| Stone location | <0.001** | ||
| Kidney | 8 | 23 | |
| Upper two-thirds of ureter | 18 | 1 | |
| Lower third of ureter | 20 | 13 | |
| Volume (mm3) | 37.5 (range 5–425) | 28 (range 4–412) | 0.39* |
| Hydronephrosis | 36 | 12 | <0.001** |
Mann-Whitney test;
Chi-square test.
Among the 83 patients, 31 (37.3%) were diagnosed with a kidney stone, 19 (22.9%) with an upper two-thirds ureteral stone, and 33 (39.8%) with a lower third ureteral stone; the corresponding incidences of microhematuria were 26%, 95%, and 61%, respectively. There was a statistically significant difference between the position of the stone and microhematuria (p<0.001) and positive correlation between those parameters (r: 0.28, p=0.009). In addition, the stones in the upper ureter (mean volume 89 mm3) were larger than the lower ureteral stones (mean volume 50 mm3). However, this difference did not reach statistical significance (p>0.05)
The difference in presence of hydronephrosis between Group I (36 patients, 78%) and Group II (12 patients, 32%) was statistically significant (p<0.001). The median stone volume between the microhematuria and non-microhematuria groups were not statistically different, 37.5 mm3 (range 5–425) and 28 mm3 (range 4–412), respectively (p=0.39).
Although the incidence of microhematuria seemed to increase from patients with stones sized 1–10 mm3 (42%) to patients with stones sized 75–100 mm3 (83%) (Table 2), the correlation between the volume of stones and the incidence of microhematuria was not statistically significant.
Table 2.
Size of stones and incidence of microhaematuria and hydronephrosis in patients with one stone.
| Volume of stone (mm3) | Total number of patients | Number of patients with microhaematuria | Number of patients without microhaematuria | Incidence of microhaematuria (%) | Incidence of hydroneprosis (%) |
|---|---|---|---|---|---|
| 1–10 | 12 | 5 | 7 | 42 | 33 |
| 10–25 | 23 | 12 | 11 | 52 | 74 |
| 25–50 | 19 | 12 | 7 | 63 | 68 |
| 50–75 | 8 | 5 | 3 | 63 | 62 |
| 75–100 | 6 | 5 | 1 | 83 | 67 |
| 100–150 | 2 | 1 | 1 | 50 | 0 |
| 150–200 | 5 | 2 | 3 | 40 | 20 |
| 200–250 | 5 | 2 | 3 | 40 | 60 |
| 250–500 | 3 | 2 | 1 | 67 | 33 |
Discussion
This study examined the relationship between stone volume and microhematuria on urinalysis for urolithiasis. To our knowledge, this is the first study to compare stone volume and microhematuria. However, there was no statistically significant difference between these parameters. Our study emphasizes that microhematuria is closely correlated with hydronephrosis and presence of ureteral stone (especially upper two-thirds ureteral stones).
Previous studies have reported inconsistent outcomes regarding the sensitivity of microhematuria for diagnosing urolithiasis in patients with flank colic pain, including different numbers of patients, use of a variety of examinations as the gold standard, different urine tests, and different cut-off values for defining microhematuria [5–10]. These studies also confirmed that CT is considered the gold standard for diagnosing urolithiasis and is now universally accepted as the preferred method [11]. However, in these studies, cumulative stone diameter was compared with microhematuria in CT evaluation [5,8]. However, this measurement is not indicative of total stone burden, particularly because each stone typically has a complex 3-dimensional shape [4]. Perhaps due to fact that this reason, there is no agreement between microhematuria and presence of stone in these studies. However, stone volume is one of the best methods for estimation of stone burden [1], we did not find a correlation between stone volume and microhematuria, although the incidence of microhematuria seemed to increase from patients with stones sized 1–10 mm3 (42%) to patients with stones sized 75–100 mm3 (83%).
Looking for hydronephrosis as a surrogate marker for kidney stones, some studies reported a sensitivity and specificity of emergency ultrasound in patients with flank pain and microhaematuria of 88% and 85%, respectively [12]. Several studies found that ultrasound-detected hydronephrosis was present in approximately 90% of patients with urinary stones and colic pain [5,13,14]. In our study, hydronephrosis was present in 95% and 91% of patients with urinary stones in the proximal two-thirds of the ureter and lower segment, respectively. Statistically significant difference was found between the microhematuria and non-microhematuria groups for presence of hydronephrosis.
Kartal et al. [15] prospectively evaluated an algorithm in which patients with hematuria and hydronephrosis were spared of further testing; the authors reported that with use of this algorithm, more than 50% of patients with acute flank pain were safely discharged from the emergency department. The authors concluded that ultrasound can be safely employed using this diagnostic approach.
A few studies have investigated the possible association between stone position and microhematuria. Xafis et al found no statistically significant correlation between the position of the stone and microhematuria [5]. However, we found a significant positive correlation between the position of the stone (especially in the upper two-thirds of the ureter) and microhematuria rate. This may be a result of continuing mucosal damage during passage of the stone in the proximal ureter. In a recent study that reported the role of US in the diagnosis of urolithiasis, Mos et al, using with a variety of maneuvers, successfully found 11 stones in the middle ureter among 217 patients with urolithiasis [16]. The combination of urinalysis and ultrasound can be used to diagnose ureterolithiasis without performing a CT scan.
In many centers MDCT has been used as the initial diagnostic tool in urolithiasis because it has been reported to be superior to ultrasound, especially in ureterolithiasis [14,17,18], but this higher degree of accuracy may not always be necessary. Ureterolithiasis is generally a self-limited disease that can be managed conservatively [19,20]. Spontaneous passage of a stone is probable when stone size is less than 5 mm [20,21]. Urgent intervention is seldom necessary. The complication rate from conservative management has been observed to be as low as 7% when symptoms last less than 4 weeks [20,22]. In addition to the information in favor of MDCT examination in the diagnosis of urolithiasis patients, its cumulative radiation exposure is significant [20,23,24] and likely to be a public health problem in the future [24,25]. Patients with a history of recurrent ureterolithiasis appear to be among those at highest risk for extreme radiation exposure from diagnostic imaging [20,26]. Therefore, CT may be able not to be performed, for example, in patients with microhematuria and no sonographic ureteral pathologies, including hydronephrosis and stones, if other probable diagnosis can be ruled out clinically at the emergency department as proposed by Kartal et al. [15].
Our results must be interpreted in light of several limitations. Firstly, our sample size was small because of strict inclusion criteria. We selected solitary urolithiasis and CSD <1cm in order to provide a standard. Secondly, the effect of hydration status on the ability of ultrasonography to detect hydronephrosis is well known; hydration status was not known for the patients in this study due to its retrospective nature.
Conclusions
Although stone volume is one of the best methods for reflection of stone burden, microhematuria is not correlated with stone volume. However, in patients with renal colic, microhematuria requires ultrasound examination whether hydronephrosis and ureteral stones are present or not. Therefore CT can be avoided in patients with microhematuria and normal US, if renal colic is the only diagnosis suspected. Further studies with larger sample size are warranted.
Footnotes
There are no conflicts of interest.
Source of support: Departmental sources
References
- 1.Ito H, Kawahara T, Terao H, et al. The Most Reliable Preoperative Assessment of Renal Stone Burden as a Predictor of Stone-free Status After Flexible Ureteroscopy With Holmium Laser Lithotripsy: A Single-center Experience. Urology. 2012;80(3):524–28. doi: 10.1016/j.urology.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 2.Patel SR, Stanton P, Zelinski N, et al. Automated renal stone volume measurement by noncontrast computerized tomography is more reproducible than manual linear size measurement. J Urol. 2011;186:2275–79. doi: 10.1016/j.juro.2011.07.091. [DOI] [PubMed] [Google Scholar]
- 3.Liden M, Andersson T, Broxvall M, et al. Urinary stone size estimation: a new segmentation algorithm-based CT method. Eur Radiol. 2012;22:731–37. doi: 10.1007/s00330-011-2309-x. [DOI] [PubMed] [Google Scholar]
- 4.Demehri S, Kalra MK, Rybicki FJ, et al. Quantification of urinary stone volume: attenuation threshold-based CT method – a technical note. Radiology. 2011;258:915–22. doi: 10.1148/radiol.10100333. [DOI] [PubMed] [Google Scholar]
- 5.Xafis K, Thalmann G, Benneker LM, et al. Forget the blood, not the stone! Microhaematuria in acute urolithiasis and the role of early CT scanning. Emerg Med J. 2008;25:640–44. doi: 10.1136/emj.2006.043703. [DOI] [PubMed] [Google Scholar]
- 6.Luchs JS, Katz DS, Lane MJ, et al. Utility of hematuria testing in patients with suspected renal colic: correlation with unenhanced helical CT results. Urology. 2002;59:839–42. doi: 10.1016/s0090-4295(02)01558-3. [DOI] [PubMed] [Google Scholar]
- 7.Li J, Kennedy D, Levine M, et al. Absent hematuria and expensive computerized tomography: case characteristics of emergency urolithiasis. J Urol. 2001;165:782–84. [PubMed] [Google Scholar]
- 8.Argyropoulos A, Farmakis A, Doumas K, Lykourinas M. The presence of microscopic hematuria detected by urine dipstick test in the evaluation of patients with renal colic. Urol Res. 2004;32:294–97. doi: 10.1007/s00240-004-0413-y. [DOI] [PubMed] [Google Scholar]
- 9.Bove P, Kaplan D, Dalrymple N, et al. Reexamining the value of hematuria testing in patients with acute flank pain. The J Urol. 1999;162:685–87. doi: 10.1097/00005392-199909010-00013. [DOI] [PubMed] [Google Scholar]
- 10.Eray O, Cubuk MS, Oktay C, et al. The efficacy of urinalysis, plain films, and spiral CT in ED patients with suspected renal colic. Am J Emerg Med. 2003;21:152–54. doi: 10.1053/ajem.2003.50027. [DOI] [PubMed] [Google Scholar]
- 11.Tack D, Sourtzis S, Delpierre I, et al. Low-dose unenhanced multidetector CT of patients with suspected renal colic. AJR Am J Roentgenol. 2003;180:305–11. doi: 10.2214/ajr.180.2.1800305. [DOI] [PubMed] [Google Scholar]
- 12.Gaspari RJ, Horst K. Emergency ultrasound and urinalysis in the evaluation of flank pain. Acad Emerg Med. 2005;12:1180–84. doi: 10.1197/j.aem.2005.06.023. [DOI] [PubMed] [Google Scholar]
- 13.Seitz C, Tanovic E, Kikic Z, et al. Rapid extracorporeal shock wave lithotripsy for proximal ureteral calculi in colic versus noncolic patients. Eur Urol. 2007;52:1223–27. doi: 10.1016/j.eururo.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Moak JH, Lyons MS, Lindsell CJ. Bedside renal ultrasound in the evaluation of suspected ureterolithiasis. Am J Emerg Med. 2012;30:218–21. doi: 10.1016/j.ajem.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 15.Kartal M, Eray O, Erdogru T, Yilmaz S. Prospective validation of a current algorithm including bedside US performed by emergency physicians for patients with acute flank pain suspected for renal colic. Emerg Med J. 2006;23:341–44. doi: 10.1136/emj.2005.028589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mos C, Holt G, Iuhasz S, et al. The sensitivity of transabdominal ultrasound in the diagnosis of ureterolithiasis. Med Ultrason. 2010;12:188–97. [PubMed] [Google Scholar]
- 17.Rengifo Abbad D, Rodriguez Caravaca G, et al. Diagnostic validity of helical CT compared to ultrasonography in renal-ureteral colic. Arch Esp Urol. 2010;63:139–44. [PubMed] [Google Scholar]
- 18.Teichman JM. Clinical practice. Acute renal colic from ureteral calculus. N Engl J Med. 2004;350:684–93. doi: 10.1056/NEJMcp030813. [DOI] [PubMed] [Google Scholar]
- 19.Miller OF, Kane CJ. Time to stone passage for observed ureteral calculi: a guide for patient education. J Urol. 1999;162:688–90. doi: 10.1097/00005392-199909010-00014. [DOI] [PubMed] [Google Scholar]
- 20.Ekici S, Sinanoglu O. Comparison of conventional radiography combined with ultrasonography versus nonenhanced helical computed tomography in evaluation of patients with renal colic. Urol Res. 2012;40(5):543–47. doi: 10.1007/s00240-012-0460-8. [DOI] [PubMed] [Google Scholar]
- 21.Segura JW, Preminger GM, Assimos DG, et al. Ureteral Stones Clinical Guidelines Panel summary report on the management of ureteral calculi. J Urol. 1997;158:1915–21. doi: 10.1016/s0022-5347(01)64173-9. [DOI] [PubMed] [Google Scholar]
- 22.Hubner WA, Irby P, Stoller ML. Natural history and current concepts for the treatment of small ureteral calculi. Eur Urol. 1993;24:172–76. doi: 10.1159/000474289. [DOI] [PubMed] [Google Scholar]
- 23.Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176:289–86. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 24.Brenner DJ, Hall EJ. Computed tomography – an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–84. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 25.Brenner DJ, Doll R, Goodhead DT, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci USA. 2003;100:13761–66. doi: 10.1073/pnas.2235592100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Birnbaum S. Radiation safety in the era of helical CT: a patient-based protection program currently in place in two community hospitals in New Hampshire. J Am Coll Radiol. 2008;5:714–18. doi: 10.1016/j.jacr.2008.02.016. [DOI] [PubMed] [Google Scholar]


