Abstract
Background
Low adherence to antihypertensive medication is an important barrier to achieving blood pressure control. Few data are available on medication adherence in adults with chronic kidney disease (CKD).
Study Design
Cross-sectional
Setting & Participants
3936 and 9129 participants with and without CKD, respectively, taking antihypertensive medication in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. CKD was defined as albuminuria ≥ 30 mg/g or an estimated glomerular filtration rate < 60 ml/min/1.73m2.
Outcomes
Medication adherence and uncontrolled hypertension.
Measurements
Medication adherence was assessed using a validated 4-item scale. Blood pressure was measured two times by trained staff.
Results
Among REGARDS participants with and without CKD, 1426 (36.2%) and 2421 (26.5%) had uncontrolled hypertension ≥ 140/90 mmHg and 2656 (67.5%) and 5627 (61.6%) ≥ 130/80 mmHg. Also, 27.7% of those with CKD and 27.9% of those without CKD responded “yes” to ever forgetting to take their medication and 4.4% and 4.2%, respectively, responded being careless about taking their medication. Also, 5.7% and 5.3% responded “yes” to missing taking medication when they felt better and 4.2% and 3.6% to missing it when they felt sick. Overall, 23.3% and 23.7% of participants with and without CKD responded “yes” to one adherence question while 7.7% and 7.2% responded “yes” to ≥ 2 adherence questions, respectively. Among those with CKD, the multivariable adjusted odds ratio for uncontrolled hypertension (≥140/90 mmHg) for individuals answering “yes” to 1 and ≥2 versus 0 adherence questions was 1.26 (95% CI: 1.05 – 1.51) and 1.49 (95% CI: 1.12 – 1.98), respectively. The analogous odds ratios for systolic/diastolic blood pressure ≥ 130/80 mmHg were 1.06 (95% CI: 0.78 – 1.45) and 1.20 (95% CI: 0.88 – 1.64).
Limitations
Pharmacy fill data were not available.
Conclusions
Individuals with CKD had similarly poor medication-taking behaviors as those without CKD.
Inadequately controlled hypertension is considered one of the most important risk factors for the progression of chronic kidney disease (CKD)1–3. The prevalence of hypertension among adults with CKD in previous studies has consistently exceeded 60%4–6. Despite the high prevalence of hypertension in patients with CKD, low rates of hypertension control have been reported5–7. Although many patients with CKD and uncontrolled blood pressure may be considered by their physician to have refractory hypertension, a significant factor contributing to poor blood pressure control may in fact be low adherence to prescribed therapy8.
Low adherence to antihypertensive medications has been reported to be common and associated with uncontrolled hypertension in the general population9–14. For example, the odds ratio for hypertension control in a meta-analysis was 3.44 (95% confidence interval [CI], 1.60–7.37) for adherent versus non-adherent individuals15. However, data on medication adherence among adults with CKD are limited. Several correlates of low medication adherence (e.g., lower income, poor quality of life, lack of social support) are more common among adults with CKD, compared to their counterparts without CKD, suggesting it may be a substantial problem in this high risk population16–19.
The goal of the current analysis was to evaluate levels of medication adherence among adults with and without CKD. Additionally, because identifying mediators of hypertension control may be useful for developing interventions to improve blood pressure control, we investigated the association of level of medication adherence with hypertension control. To accomplish these goals, we analyzed data from the baseline visit of the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study.
METHODS
Study Participants
The REGARDS study is a community-based investigation of stroke incidence among U.S. adults ≥ 45 years of age20. The study was designed to oversample African Americans and to provide approximate equal representation of men and women. The composition of final cohort was 26% African-American women, 16% African-American men, 29% Caucasian women, and 29% Caucasian men. By design, 56% (goal 50%) of the sample was recruited from the eight Southern U.S. states, commonly referred to as the “stroke buckle” (coastal North Carolina, South Carolina, and Georgia) and “stroke belt” (remainder of North Carolina, South Carolina, and Georgia as well as Alabama, Mississippi, Tennessee, Arkansas and Louisiana), with the remaining 44% of the sample recruited from the other 40 contiguous U.S. states. Participants were identified from commercially available lists of residents and recruited through an initial mailing followed by telephone contacts. Overall, 30,239 African-American and Caucasian U.S. adults were enrolled between January 2003 and October 2007. Of those contacted with a mailing, 33% completed a telephone study interview and the cooperation rate (number of participants divided by the number eligible that were ever contacted) was 49%21. These rates are similar to other large epidemiological studies22. The current analysis was limited to participants who were taking antihypertensive medication at baseline (n=14,672). Participants receiving hemodialysis (n=84), missing serum creatinine measurements (n=621), without valid urinary albumin and creatinine measurements (n=582) and who did not answer questions on the adherence scale (n=320) were excluded, leaving 13,065 participants with complete data for the present analysis. The REGARDS protocol was approved by the Institutional Review Boards governing research in human subjects at the participating centers and all participants provided informed consent.
Data Collection
Socio-demographic and clinical data were collected at baseline through a telephone interview, a self-administered questionnaire and an in-home examination. Trained interviewers conducted computer-assisted telephone interviews to obtain information on participants’ demographics, current cigarette smoking, marital status, annual household income, education, symptoms of depression, and self-reports of a prior diagnosis of major co-morbid conditions (i.e., diabetes, hypertension, myocardial infarction, stroke, coronary revascularization, and chronic kidney disease). Symptoms of depression were defined as being present for participants with scores ≥ 4 on the 4-item CES-D[ND1] (Centers for Epidemiologic Studies of Depression) scale23. Cognitive impairment was assessed using a 6-Item test of global cognitive function that includes recall and temporal orientation items24.
Medication adherence was assessed via a validated 4-item scale. In a prior study, this scale was reported to have acceptable internal consistency (Cronbach’s alpha = 0.61), the items maintained a high item-to-total correlation (>0.4 for each item), and scores were correlated with blood pressure control25. The 4 items had response options of “No” or “Yes”. These items are:
Do you ever forget to take medications?
Are you ever careless in taking your medications?
Do you ever miss taking your medications when you are feeling better?
Do you ever miss taking any of your medications because you are feeling sick?
One point was assigned to each “yes” response, the points were summed, and medication adherence was grouped into three levels: scores of 0, 1, and ≥ 2 with a higher score indicating worse adherence26.
Trained and certified health professionals conducted in-home study visits that included the review of medication pill bottles, a physical examination, and the collection of blood and urine samples. During the in-home visit, participants were asked to provide the bottles for all medications they had taken in the past two weeks, and medication names were recorded and subsequently coded into drug classes. Antihypertensive medication classes were defined using those listed in the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure27. Blood pressure was measured two times using aneroid sphygmomanometers following a standardized protocol. Participants were asked to sit for three minutes with both feet on the floor prior to the blood pressure measurement. Based on the average of the two blood pressure measurements, hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, and/or self-reported use of antihypertensive medication. Diabetes was defined as a serum glucose ≥ 126 mg/dL for participants who had fasted ≥ 8 hours prior to sampling, serum glucose ≥ 200 mg/dL for those who had not fasted, or self-report of a prior diagnosis of diabetes with current use of insulin or oral hypoglycemic medications. Body mass index (BMI)was calculated as weight in kilograms divided by height in meters squared and overweight and obesity were defined as a BMI of 25 to 29 kg/m2 and ≥ 30 kg/m2, respectively. A history of cardiovascular disease (CVD) was defined based on a self-reported history of myocardial infarction or coronary revascularization (coronary angioplasty or bypass surgery) or stroke.
Using isotope-dilution mass spectrometry (IDMS)-traceable serum creatinine, estimated glomerular filtration rate (eGFR) was calculated using the CKD-EPI[ND2] (CKD Epidemiology Collaboration) equation28. Using a random spot urine collection, albuminuria was defined as an albumin-creatinine ratio ≥ 30 mg/g. CKD was defined as the presence of albuminuria or an eGFR < 60 ml/min/1.73 m2.29
Statistical Analysis
Participant characteristics were calculated by adherence scale score (0, 1, ≥ 2) for those without and with CKD, separately, as means for continuous variables and proportions for categorical variables. The statistical significance of trends across adherence scale scores was determined using least squares and maximum likelihood as appropriate. The distributions of responses (“no” or “yes”) to each of the four questions on the adherence scale and overall scale scores were calculated for individuals with and without CKD, separately. Using logistic regression, the odds ratios for responses were calculated comparing individuals with CKD to their counterparts without CKD. Multinomial logistic regression models were used to calculate the odds ratios for adherence scale scores of 1 and ≥ 2 versus 0 comparing REGARDS study participants with versus without CKD. Next, multivariable adjusted odds ratios for adherence scale scores of 1 and ≥ 2 versus 0 associated with participant characteristics were calculated for individuals with CKD using multinomial logistic regression. Multivariable adjustment included the following a priori selected variables: age, sex, race, education, income, current smoking, alcohol consumption, overweight and obesity, marital status, region of residence, symptoms of depression, cognitive impairment, diabetes, history of CVD and number of antihypertensive medications being taken.
Rates of uncontrolled hypertension and multivariable adjusted odds ratios for uncontrolled hypertension were calculated by responses to each adherence question and for adherence scale scores of 0, 1 and ≥ 2 for participants with and without CKD, separately. Although a target systolic/diastolic blood pressure < 140/90 mmHg is recommended for most adults, individuals with CKD are recommended a target systolic/diastolic blood pressure < 130/80 mmHg. As the vast majority of participants in REGARDS were unaware of having CKD, we assessed uncontrolled hypertension using two separate cut-points: systolic/diastolic blood pressure ≥ 140/90 mmHg and ≥130/80 mmHg. All analyses were conducted using SAS 9.2 (SAS Institute, www.sas.com).
RESULTS
Among those without and with CKD, participants with worse adherence scale scores were younger (Table 1). Cigarette smokers and those with symptoms of depression were more likely to have worse adherence scale scores. Additionally, worse adherence scale scores were associated with higher levels of BMI, eGFR, albuminuria, and SBP and DBP. Additionally, among those without CKD, being African-American, having less education, and lower income were associated with worse adherence scale scores while men and those living in the stroke buckle versus non-belt regions and who were married had better adherence scale scores.
Table 1.
[ND3]. Characteristics of the REGARDS study cohort taking antihypertensive medication, by CKD status and level of medication adherence.
| No CKD | CKD | |||||||
|---|---|---|---|---|---|---|---|---|
| Adherence scale score | p-trend | Adherence scale score | p-trend | |||||
| 0 (better; n=6301) |
1 (n=2167) | ≥ 2 (worse; n=661) |
0 (better; n=2715) |
1 (n=916) | ≥ 2 (worse; n=305) |
|||
| Age, years | 65.3 (8.5) | 64.4 (8.1) | 63.3 (8.5) | <0.001 | 69.7 (9.1) | 68.6 (9.3) | 66.6 (9.8) | <0.001 |
| Men, % | 43.3 | 42.8 | 32.2 | <0.001 | 46.8 | 47.5 | 41.0 | 0.2 |
| African-American, % | 48.2 | 46.8 | 61.1 | <0.001 | 51.3 | 48.3 | 62.0 | 0.07 |
| Region, % | ||||||||
| Non–stroke belt | 42.5 | 41.7 | 49.2 | ref | 45.1 | 46.8 | 45.9 | ref |
| Stroke belt | 35.6 | 38.1 | 37.2 | 0.9 | 33.3 | 34.6 | 32.5 | 0.8 |
| Stroke buckle | 22.0 | 20.2 | 13.6 | <0.001 | 21.6 | 18.6 | 21.6 | 0.3 |
| Married, % | 58.7 | 60.3 | 46.8 | <0.001 | 51.0 | 53.1 | 48.9 | 0.9 |
| Education, % | ||||||||
| Less than high school | 13.5 | 12.4 | 18.5 | ref | 19.3 | 19.2 | 17.1 | ref |
| High school graduate | 26.7 | 28.1 | 29.2 | 0.5 | 27.7 | 27.4 | 32.5 | 0.2 |
| Some college | 26.8 | 28.2 | 27.7 | 0.4 | 25.5 | 25.8 | 25.3 | 0.6 |
| College graduate | 33.0 | 31.3 | 24.7 | <0.001 | 27.6 | 27.5 | 25.3 | 0.9 |
| Income, % | ||||||||
| <$20,000 | 20.9 | 20.7 | 31.9 | ref | 30.0 | 25.9 | 36.1 | ref |
| $20,000 – $34,999 | 28.0 | 29.8 | 27.2 | 0.01 | 32.1 | 32.1 | 34.6 | 0.9 |
| $35,000 – $74,999 | 34.4 | 34.1 | 30.5 | <0.001 | 28.6 | 31.6 | 22.9 | 0.6 |
| ≥$75,000 | 16.7 | 15.5 | 10.5 | <0.001 | 9.3 | 10.4 | 6.4 | 0.5 |
| Current smoking, % | 12.6 | 12.7 | 17.6 | 0.01 | 13.5 | 15.0 | 18.4 | 0.02 |
| Symptoms of depression, % | 10.7 | 13.5 | 22.4 | <0.001 | 11.7 | 13.1 | 18.5 | 0.002 |
| Cognitive impairment, % | 7.6 | 7.0 | 6.6 | 0.3 | 12.1 | 9.6 | 10.6 | 0.1 |
| Prior CKD diagnosis, % | 0.9 | 0.8 | 1.2 | 0.6 | 4.8 | 5.1 | 6.6 | 0.2 |
| BMI, kg/m2 | 30.3 (6.3) | 31.1 (6.1) | 31.4 (6.4) | <0.001 | 30.6 (6.7) | 31.0 (6.4) | 31.2 (6.9) | 0.04 |
| Diabetes, % | 23.8 | 25.9 | 23.3 | 0.4 | 41.4 | 41.5 | 47.5 | 0.1 |
| History of CVD, % | 29.0 | 29.2 | 31.0 | 0.4 | 41.6 | 41.5 | 42.0 | 0.9 |
| eGFR, ml/min/1.73m2 | 88.5 (15.2) | 88.6 (15.0) | 90.7 (16.3) | 0.003 | 65.0 (24.5) | 65.8 (24.6) | 68.7 (28.0) | 0.02 |
| Albuminuria, mg/g | 6.9 (4.6–11.3) | 6.7 (4.6–11.3) | 7.5 (4.9–12.3) | 0.02 | 43.4 (12.7–123.7) | 47.1 (13.9–144.1) | 55.9 (20.0–150.0) | 0.007 |
| SBP, mmHg | 129.5 (15.2) | 130.4 (16.3) | 132.7 (16.7) | <0.001 | 133.9 (17.7) | 135.3 (18.3) | 136.8 (20.0) | 0.003 |
| DBP, mmHg | 77.5 (9.0) | 77.9 (9.6) | 80.4 (10.7) | <0.001 | 76.9 (10.4) | 77.6 (11.2) | 79.9 (12.0) | <0.001 |
| No. of antihypertensive drug classes, % |
||||||||
| 1 | 38.8 | 38.0 | 39.6 | ref | 26.5 | 24.7 | 27.9 | Ref |
| 2 | 39.5 | 40.3 | 39.5 | 0.911 | 36.8 | 36.7 | 40.0 | 0.606 |
| 3 | 17.2 | 17.2 | 15.7 | 0.607 | 27.2 | 27.0 | 23.3 | 0.535 |
| ≥ 4 | 4.5 | 4.5 | 5.2 | 0.587 | 9.5 | 11.7 | 8.9 | 0.506 |
Numbers in table are mean (standard deviation) or percent, except albuminuria, which is median (25th – 75th percentiles)
CKD was defined as an albumin-creatinine ratio ≥ 30 mg/g or an estimated glomerular filtration rate < 60 ml/min/1.73m2
Conversion factor for eGFR in ml/min/1.73m2 to ml/s/1.73m2, x0.01667.
Abbreviations: BMI, body mass index; eGFR, estimated glomerular filtration rate; CVD, cardiovascular disease; CKD, chronic kidney disease; ref, reference; REGARDS,Reasons for Geographic and Racial Differences in Stroke; SBP, systolic blood pressure; DBP, diastolic blood pressure.
The distribution of responses to each medication adherence scale item and scale scores was similar for participants with and without CKD (Table 2). Overall, 23.3% and 23.7% of participants with and without CKD responded “yes” to one scale item and 7.7% and 7.2% answered “yes” to two or more items. Compared to the reference group of an adherence scale score of 0 (i.e., answering “no” to all four questions), the age, sex, race adjusted odds ratio for adherence scale scores of 1 and ≥ 2 for individuals with versus without CKD was 1.04 (95% CI: 0.94 – 1.14) and 1.19 (95% CI: 1.02 – 1.38), respectively. This association was attenuated and not statistically significant after further multivariable adjustment.
Table 2.
Distribution and ORs for responses to the medication adherence scale comparing individuals with and without CKD
| OR (95% CI) † | ||||
|---|---|---|---|---|
| No CKD | CKD | Multivariable 1* | Multivariable 2** | |
| Adherence question*** | ||||
| Item 1. Do you ever forget to take your medications? | 27.9 | 27.7 | 1.06 (0.97 – 1.15) | 1.03 (0.92 – 1.15) |
| Item 2. Are you ever careless in taking your medications? |
4.2 | 4.4 | 1.09 (0.90 – 1.32) | 1.15 (0.90 – 1.46) |
| Item 3. Do you ever miss taking your medications when you are feeling better? |
5.3 | 5.7 | 1.19 (1.00 – 1.40) | 1.21 (0.97 – 1.49) |
| Item 4. Do you ever miss taking any of your medications because you are feeling sick? |
3.6 | 4.2 | 1.24 (1.02 – 1.52) | 1.15 (0.90 – 1.47) |
| Adherence scale score‡ | ||||
| 0 (better adherence) | 69.0 | 69.0 | 1 (ref) | 1 (ref) |
| 1 | 23.7 | 23.3 | 1.04 (0.94 – 1.14) | 1.00 (0.89 – 1.12) |
| 2+ (worse adherence) | 7.2 | 7.7 | 1.19 (1.02 – 1.38) | 1.13 (0.94 – 1.36) |
Values shown are percentage or OR (95% CI)
OR for answering yes versus no comparing individuals with versus without CKD
OR for adherence score compared to score of 0 comparing individuals with versus without CKD
Multivariable 1 – includes adjustment for age, race, and sex.
Multivariable 2 – includes adjustment for age, sex, race, education, income, current smoking, alcohol consumption, marital status, region of residency (stroke belt, stroke belt or other), symptoms of depression, cognitive impairment, diabetes, history of cardiovascular disease, and number of antihypertensive medications taken.
Percentages shown are those who responded “yes” to the question.
Abbreviations: CKD – chronic kidney disease, OR – odds ratio, CI – confidence interval; ref, reference
Among participants with CKD, older age and higher income were associated with lower odds ratios for medication adherence scores of 1 and ≥ 2 versus 0; indicating better adherence among these groups (Table 3). In contrast, symptoms of depression were associated with a higher odds ratio for medication adherence score ≥ 2 versus 0. No other participant characteristics showed trends in the association with medication adherence.
Table 3.
ORs for medication adherence scale score categories among REGARDS participants with CKD
| 0 (better adherence) |
1 | ≥ 2 (worse adherence) |
|
|---|---|---|---|
| Age, per 10 years | 1 (ref) | 0.92 (0.81, 1.03) | 0.76 (0.63, 0.91) |
| Men | 1 (ref) | 0.97 (0.78, 1.20) | 0.73 (0.51, 1.04) |
| African-American | 1 (ref) | 0.81 (0.67, 0.97) | 1.25 (0.95, 1.60) |
| Region (stroke belt/buckle) | |||
| Belt versus non-belt | 1 (ref) | 1.03 (0.83, 1.28) | 0.95 (0.67, 1.34) |
| Buckle versus non-belt | 1 (ref) | 0.85 (0.66, 1.10) | 0.88 (0.59, 1.32) |
| Education (versus < high school) | |||
| High school graduate | 1 (ref) | 0.74 (0.55, 1.01) | 1.29 (0.79, 2.12) |
| Some college | 1 (ref) | 0.80 (0.59, 1.10) | 1.51 (0.91, 2.50) |
| College graduate | 1 (ref) | 0.71 (0.51, 0.99) | 1.52 (0.87, 2.63) |
| Income (versus <$20,000) | |||
| $20,000 – $34,999 | 1 (ref) | 1.39 (1.07, 1.82) | 1.04 (0.71, 1.54) |
| $35,000 – $74,999 | 1 (ref) | 1.30 (1.00, 1.70) | 0.67 (0.44, 1.00) |
| ≥$75,000 | 1 (ref) | 1.29 (0.84, 1.98) | 0.72 (0.37, 1.41) |
| Current smoking | 1 (ref) | 1.17 (0.88, 1.56) | 1.29 (0.85, 1.94) |
| Alcohol consumption | |||
| Moderate versus none | 1 (ref) | 1.00 (0.82, 1.22) | 1.04 (0.76, 1.43) |
| Heavy versus none | 1 (ref) | 1.60 (1.01, 2.51) | 1.10 (0.48, 2.52) |
| Currently married | 1 (ref) | 1.00 (0.82, 1.22) | 1.22 (0.90, 1.67) |
| BMI (versus <25 kg/m2) | |||
| 25–29.9 kg/m2 | 1 (ref) | 1.37 (1.06, 1.77) | 1.11 (0.74, 1.67) |
| ≥ 30 kg/m2 | 1 (ref) | 1.45 (1.12, 1.87) | 1.10 (0.74, 1.63) |
| Diabetes mellitus | 1 (ref) | 1.00 (0.84, 1.20) | 1.14 (0.86, 1.51) |
| History of CVD | 1 (ref) | 0.94 (0.77, 1.15) | 1.29 (0.94, 1.77) |
| Symptoms of depression | 1 (ref) | 1.25 (0.94, 1.77) | 1.62 (1.08, 2.43) |
| Cognitive impairment | 1 (ref) | 0.72 (0.52, 1.01) | 0.92 (0.56, 1.50) |
| # of Anti-hypertensive medication classes | |||
| 2 versus 1 | 1 (ref) | 1.03 (0.81, 1.32) | 0.95 (0.65, 1.38) |
| 3 versus 1 | 1 (ref) | 1.07 (0.82, 1.40) | 0.72 (0.46, 1.12) |
| ≥ 4 versus 1 | 1 (ref) | 1.34 (0.98, 1.81) | 1.07 (0.62, 1.85) |
Numbers in table are OR (95% confidence interval)
All variables were included simultaneously in a single regression model.
Abbreviations: BMI, body mass index; CKD, chronic kidney disease; REGARDS, Reasons for Geographic and Racial Differences in Stroke; CVD, cardiovascular disease; ref, reference; OR, odds ratio
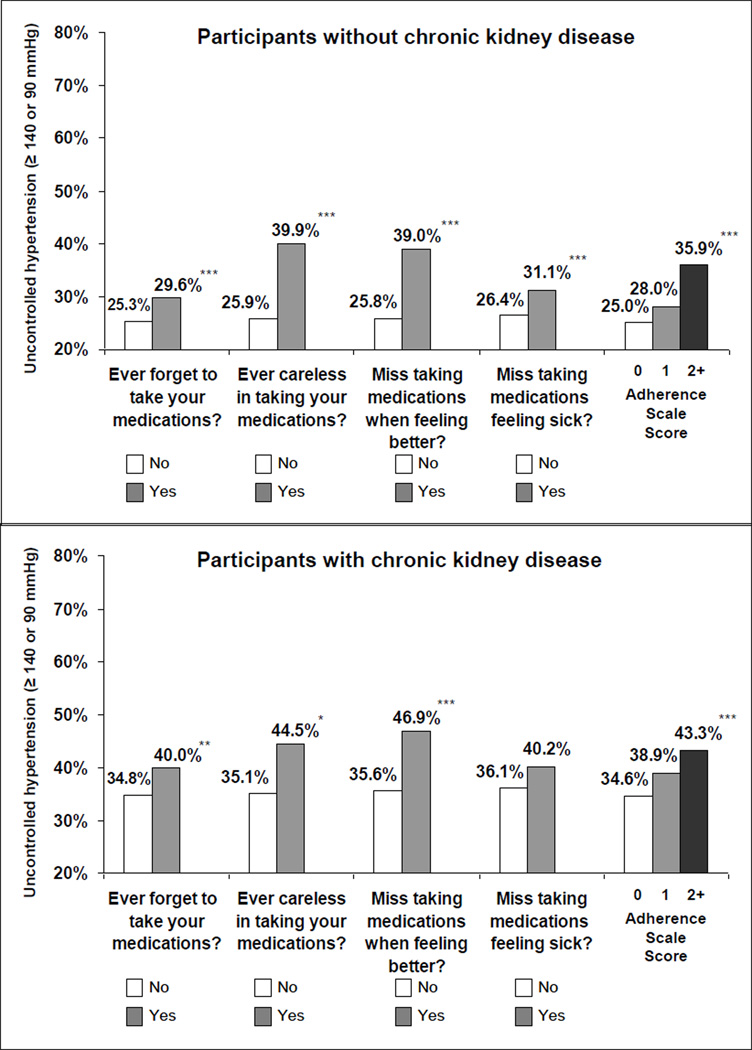
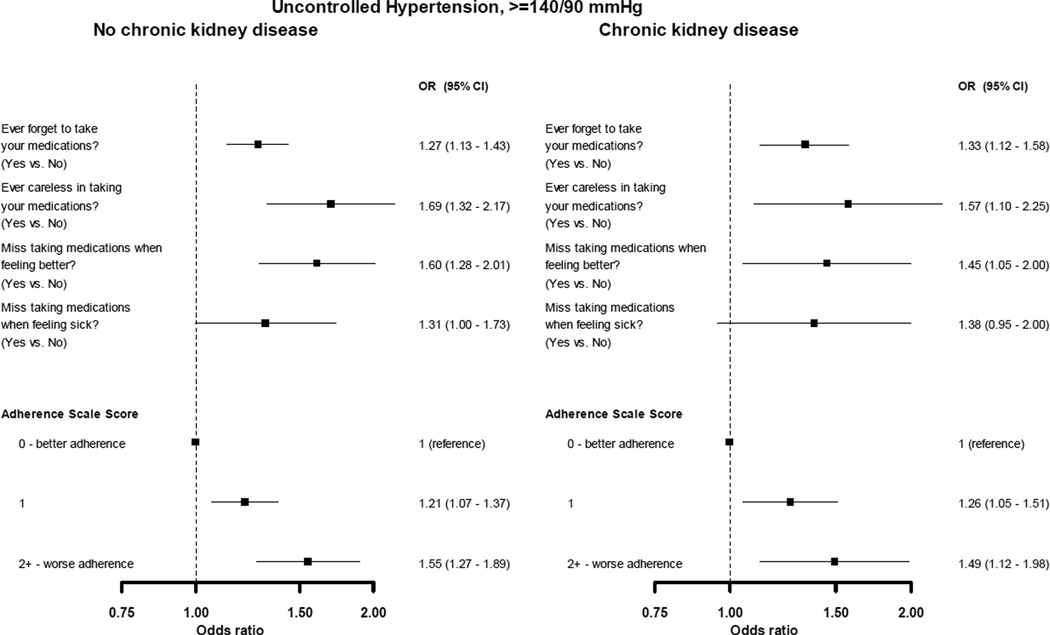
Among REGARDS participants without and with CKD taking antihypertensive medication, 26.5% and 36.2% had uncontrolled hypertension, respectively, when defined as systolic or diastolic blood pressure ≥ 140 or 90 mmHg. Using cut-points of systolic or diastolic blood pressure ≥ 130 or 80 mmHg, 61.6% and 67.5% of participants without and with CKD taking antihypertensive medication, respectively, had uncontrolled hypertension. Among those without and with CKD, uncontrolled hypertension (≥ 140 or 90 mmHg) was higher for participants who answered “yes” to each of the medication adherence questions (Figure 1). Additionally, a significant trend of higher uncontrolled hypertension rates at higher adherence scale scores (i.e., indicating worse adherence) was present. With the exception of missing taking medications when feeling sick among those with CKD, after multivariable adjustment for age, sex, race, education, income, current smoking, alcohol consumption, marital status, region of residency (stroke belt, stroke buckle, or other), symptoms of depression, cognitive impairment, diabetes, history of cardiovascular disease, and number of antihypertensive medications taken, poor medication-taking behaviors on each question were associated with uncontrolled hypertension defined as systolic or diastolic blood pressure ≥ 140 or 90 mmHg, respectively (Figure 2). Additionally, adherence scale scores of 1 and ≥ 2, versus a score of 0, were associated with increased odds ratios for uncontrolled hypertension. Differences in the association between adherence scale scores and uncontrolled hypertension (≥ 140/90 mmHg) were not significantly different for individuals with and without CKD (all p-values for interaction > 0.6).
Figure 1.
Prevalence of uncontrolled hypertension (systolic or diastolic blood pressure ≥ 140/90 mmHg) among REGARDS participants taking antihypertensive medication without chronic kidney disease (top panel) and with chronic kidney disease (bottom panel) by level of medication adherence. * p<0.05; ** p<0.01; *** p<0.001 comparing “Yes” versus “No” responses or ptrend across adherence scale scores. An adherence score of 0 represents better adherence and a score of 2+ represents worse adherence.
Figure 2.
Multivariable adjusted odds ratios for uncontrolled hypertension (systolic or diastolic blood pressure ≥ 140/90 mmHg) associated with responses to the 4-item medication adherence screener among REGARDS participants without chronic kidney disease (left panel) and with chronic kidney disease (right panel) taking antihypertensive medication. Rectangles represent odds ratio, bar represents the 95% confidence interval. Odds ratios are adjusted for age, sex, race, education, income, current smoking, alcohol consumption, marital status, region of residency (stroke belt, stroke buckle, or other)[ND4], symptoms of depression, cognitive impairment, diabetes, history of cardiovascular disease, and number of antihypertensive medications taken.
Among participants without CKD, poor behaviors to each adherence scale item and higher adherence scale scores were associated with higher rates of systolic or diastolic blood pressure ≥ 130 or 80 mmHg (Figure S1, available as online supplementary material associated with this article at www.ajkd.org). For those with CKD, the prevalence of uncontrolled hypertension (≥130/80 mmHg) was higher for participants who reported missing taking medications when they felt better. Although the prevalence of uncontrolled hypertension using this lower cut-point was higher at higher adherence scale scores, the trend across scores was not statistically significant for those with CKD. These results were similar after multivariable adjustment (Fig S2). Differences in the association between adherence scale scores and uncontrolled hypertension (≥ 130/80 mmHg) were not significantly different for individuals with and without CKD (all p-values for interaction > 0.3).
DISCUSSION
Similar to previous studies, we report high rates of hypertension and low rates of blood pressure control among REGARDS study participants with CKD. However, the present study focused on medication adherence, which has not been extensively investigated among individuals with CKD. Many participants in the current study reported not taking their medication due to forgetfulness as well as intentional reasons. Among those with CKD, only 69% of participants reported appropriate adherence behaviors on all four items of the medication adherence scale. Importantly, progressively higher scores on the medication adherence screening, indicating worse adherence, were associated with a higher prevalence of uncontrolled hypertension among this sample of US adults with and without CKD.
Low adherence to medication is a well recognized barrier to achieving hypertension control in the general US population. Despite the availability of effective antihypertensive medications, only 63.9% of US adults ≥ 20 years of age taking such treatment have controlled their systolic and diastolic blood pressure to < 140 and 90 mmHg30. It has been hypothesized that low medication adherence is common and may in part explain the low percentage of controlled hypertension among US adults8;14. In prior studies, antihypertensive medication adherence rates have differed widely depending on the population studied. In a quantitative review of 129 studies of adherence to medical recommendations, including but not limited to adherence to pharmacologic therapy for cardiovascular disease, which were published between 1948 and 1998, a mean adherence rate of 76.6% was reported31. Adherence rates were slightly lower in the current study. The percentage of participants who reported suboptimal adherence behaviors was similar for participants with and without CKD. This is not entirely unexpected as the vast majority of patients with CKD in the REGARDS study were unaware of this diagnosis. Furthermore, this finding is consistent with a study assessing pharmacy fill rates for statins, beta-blockers, and renin-angiotensin system inhibitors following myocardial infarction32. In that study, dialysis patients had lower adherence to betablockers but participants with CKD, defined using diagnosis codes, had similar pharmacy fill rates to patients without CKD.
The asymptomatic characteristic and lifelong nature of hypertension are two factors which undoubtedly contribute to low adherence to medication regimens. Previous studies have identified several other factors affecting antihypertensive medication adherence including patient demographics, cost, number, and complexity of medications, patients’ knowledge, beliefs and attitudes about their treatment, psychosocial issues, and health care system issues9;10;33–36. Consistent with prior studies, several participant characteristics (e.g., age, income, and symptoms of depression) were associated with medication adherence among participants with CKD9;11;37;38. However, other factors that have been reported to be associated with low medication adherence in patients with different chronic diseases were not present in the current study of individuals with CKD. For example, prior studies have reported African-Americans to be more likely to have low adherence37. More studies are needed to identify individuals with both CKD and low adherence and the factors that influence low adherence in this population in order to efficiently implement interventions aimed at improving medication adherence. 13 Identifying patients with low adherence is a challenge. Over recent years, research efforts have focused on the use and evaluation of methods for measuring adherence that are practical in the outpatient setting10;39. Self-report scales, like the one used in the current study, are relatively simple and economically feasible to use, but also have the added advantage of soliciting information regarding situational factors that act as barriers to medication adherence (e.g. forgetfulness)13. For several of these self-report tools, high reliability and validity have been reported13;37;40. Other methods that are available to assess medication adherence include pill counts, electronic monitoring devices, and pharmacy fill rates. Each of these approaches has strengths and weaknesses but outside of certain settings they are currently limited in their applicability for use in clinical practice.
Longitudinal studies have noted strong associations between uncontrolled blood pressure and increased risk for cardiovascular disease, end-stage renal disease, and mortality. For example, in an analysis of pooled data from the ARIC (Atherosclerosis Risk in Communities) study and Cardiovascular Health Study, two population-based cohort studies, among those with CKD, the hazard ratio for stroke was ≥ 3 for individuals with systolic blood pressure ≥ 140 mmHg versus 120 to 129 mmHg41. Also, among ARIC study participants with CKD, the hazard ratio for coronary heart disease incidence was 2.37 (95% CI: 1.33 – 4.21) comparing those with a systolic blood pressure ≥ 139 mmHg versus < 110 mmHg42. However, these prior studies did not investigate the reasons for uncontrolled blood pressure. The current study suggests low medication adherence may be an important modifiable factor impacting uncontrolled hypertension, for a considerable proportion of individuals with CKD. Future studies are needed to investigate the role of medication adherence on kidney disease progression and clinical outcomes including cardiovascular and end-stage renal disease incidence in individuals with CKD.
Findings from the current analysis must be considered within the context of certain limitations. While the 4-item self-reported adherence measure used in the current study has been previously validated and correlated with pharmacy fill rates and blood pressure control25;40, it doesn’t address many adherence domains (e.g., cutting back on medication due to cost). Newer medication adherence scales that may provide more granularity for identifying individuals with low adherence as well as barriers to achieving medication adherence have been published recently13;40. Additionally, the adherence scale used in the REGARDS study assessed medication adherence in general and was not specific to antihypertensive medication. Data were derived from a single study visit and we were unable to ascertain the persistency of medication adherence and blood pressure control over time. As an observational study, caution should be taken when considering the causal nature of the association between medication adherence and hypertension control. While it is biologically plausible that low adherence would result in uncontrolled hypertension, it is possible that the observed results may be due to unmeasured confounding factors. Also, the current study relied on volunteers; studies may attract healthier individuals or those with better adherence behaviors compared to the population in general. Finally, given the low rate of hypertension control to < 130/80 mmHg among participants with CKD, the current study may have been under-powered to detect a significant association between adherence and this level of blood pressure control. Of note, a statistically significant association was present for participants without CKD and a test for interaction was not significant.
Despite these limitations, the current analysis maintains several strengths including the large, national population of patients with CKD enrolled in the REGARDS study and the extensive collection of demographic, socio-economic, behavioral, and medical-related factors. Such extensive data collection permitted conduct of a comprehensive analysis of factors associated with low medication adherence in those with CKD. Additional strengths include the use of a standardized protocol with stringent quality control procedures for the measurement of blood pressure. Finally, the current study included a geographically diverse sample of Caucasian and African-American US adults.
Hypertension is a common co-morbidity affecting the vast majority of patients with CKD. Given the high risk for CVD and CKD progression associated with hypertension, its control may have important benefits for patients with CKD.
The findings from the current study indicate that a substantial proportion of adults with CKD do not take their medication as prescribed. Over 30% of patients with CKD forget to take or are careless about taking their medication or stop taking their medications when they feel better or when they feel sick. This finding has direct clinical relevance. As suggested by the current study, low medication adherence may have a negative effect on achieving hypertension control among individuals with CKD. Further work is required to understand the factors that lead to low medication adherence in patients with CKD. In the meantime, health care providers should ask their patients about medication adherence, and among those with low adherence, discuss the barriers to taking their medication.
Supplementary Material
Figure S1. Prevalence of uncontrolled hypertension among REGARDS participants taking antihypertensive medication with and without CKD, by level of medication adherence.
Figure S2. Multivariable adjusted ORs for uncontrolled hypertension associated with responses to the 4-item medication adherence screen among REGARDS participants taking antihypertensive medication with and without CKD.
ACKNOWLEDGMENTS
Support: This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke (NINDS), National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS or the NIH. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data. Additional funding was provided by an investigator-initiated grant-in-aid from Amgen Corporation, which did not have any role in the design and conduct of the study, the collection, management, data analysis, or interpretation of the data, or the preparation or approval of the manuscript. Drs Muntner and Krousel-Wood received support from grant R01 AG022536 from the NIH National Institute on Aging (NIA).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: The authors declare that they have no relevant financial interests.
Reference List
- 1.He J, Whelton PK. Elevated systolic blood pressure and risk of cardiovascular and renal disease: overview of evidence from observational epidemiologic studies and randomized controlled trials. Am Heart J. 1999;138:211–219. doi: 10.1016/s0002-8703(99)70312-1. [DOI] [PubMed] [Google Scholar]
- 2.Klag MJ, Whelton P, Randall B, et al. Blood pressure and End-stage renal disease in men. NEJM. 1996;334:13–18. doi: 10.1056/NEJM199601043340103. [DOI] [PubMed] [Google Scholar]
- 3.Perneger T, Nieto J, Whelton P, Klag M, Comstock G, Szklo M. A prospective study of blood pressure and serum creatinine: Results from the 'Clue' study and the ARIC study. JAMA. 1993;269:488–493. [PubMed] [Google Scholar]
- 4.Coresh J, Wei GL, McQuillan G, et al. Prevalence of high blood pressure and elevated serum creatinine level in the United States: findings from the third National Health and Nutrition Examination Survey (1988–1994) Arch Intern Med. 2001;161:1207–1216. doi: 10.1001/archinte.161.9.1207. [DOI] [PubMed] [Google Scholar]
- 5.Parikh NI, Hwang SJ, Larson MG, Meigs JB, Levy D, Fox CS. Cardiovascular disease risk factors in chronic kidney disease: overall burden and rates of treatment and control. Arch Intern Med. 2006;166:1884–1891. doi: 10.1001/archinte.166.17.1884. [DOI] [PubMed] [Google Scholar]
- 6.Peralta CA, Hicks LS, Chertow GM, et al. Control of hypertension in adults with chronic kidney disease in the United States. Hypertension. 2005;45:1119–1124. doi: 10.1161/01.HYP.0000164577.81087.70. [DOI] [PubMed] [Google Scholar]
- 7.Plantinga LC, Miller ER, III, Stevens LA, et al. Blood pressure control among persons without and with chronic kidney disease: US trends and risk factors 1999–2006. Hypertension. 2009;54:47–56. doi: 10.1161/HYPERTENSIONAHA.109.129841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19:357–362. doi: 10.1097/01.hco.0000126978.03828.9e. [DOI] [PubMed] [Google Scholar]
- 9.Hyre AD, Krousel-Wood MA, Muntner P, Kawasaki L, DeSalvo KB. Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting. J Clin Hypertens (Greenwich ) 2007;9:179–186. doi: 10.1111/j.1524-6175.2007.06372.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krousel-Wood M, Hyre A, Muntner P, Morisky D. Methods to improve medication adherence in patients with hypertension: current status and future directions. Curr Opin Cardiol. 2005;20:296–300. doi: 10.1097/01.hco.0000166597.52335.23. [DOI] [PubMed] [Google Scholar]
- 11.Kim MT, Han HR, Hill MN, Rose L, Roary M. Depression, substance use, adherence behaviors, and blood pressure in urban hypertensive black men. Ann Behav Med. 2003;26:24–31. doi: 10.1207/S15324796ABM2601_04. [DOI] [PubMed] [Google Scholar]
- 12.Mann DM, Allegrante JP, Natarajan S, Halm EA, Charlson M. Predictors of adherence to statins for primary prevention. Cardiovasc Drugs Ther. 2007;21:311–316. doi: 10.1007/s10557-007-6040-4. [DOI] [PubMed] [Google Scholar]
- 13.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive Validity of a Medication Adherence Measure in an Outpatient Setting. J Clin Hypertens (Greenwich ) 2008;10:348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 14.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 15.DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40:794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Kurella TM, Wadley V, Yaffe K, et al. Kidney function and cognitive impairment in US adults: the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Am J Kidney Dis. 2008;52:227–234. doi: 10.1053/j.ajkd.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martins D, Tareen N, Zadshir A, et al. The association of poverty with the prevalence of albuminuria: data from the Third National Health and Nutrition Examination Survey (NHANES III) Am J Kidney Dis. 2006;47:965–971. doi: 10.1053/j.ajkd.2006.02.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bruce MA, Beech BM, Sims M, et al. Social environmental stressors, psychological factors, and kidney disease. J Investig Med. 2009;57:583–589. doi: 10.231/JIM.0b013e31819dbb91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shoham DA, Vupputuri S, Kshirsagar AV. Chronic kidney disease and life course socioeconomic status: a review. Adv Chronic Kidney Dis. 2005;12:56–63. doi: 10.1053/j.ackd.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 20.Howard VJ, Cushman M, Pulley L, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 21.Morton LM, Cahill J, Hartge P. Reporting participation in epidemiologic studies: a survey of practice. Am J Epidemiol. 2006;163:197–203. doi: 10.1093/aje/kwj036. [DOI] [PubMed] [Google Scholar]
- 22. [Accessed February 5, 2010]; http://mesa-nhlbi.org/participation.aspx. MESA Website [serial online] 2004
- 23.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 24.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Shalansky SJ, Levy AR, Ignaszewski AP. Self-reported Morisky score for identifying nonadherence with cardiovascular medications. Ann Pharmacother. 2004;38:1363–1368. doi: 10.1345/aph.1E071. [DOI] [PubMed] [Google Scholar]
- 27.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 28.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Kidney Foundation KDOQI Work Group. Definition and classification of stages of chronic kidney disease. Am J Kidney Dis. 2002;39:S46–S75. [Google Scholar]
- 30.Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 31.DiMatteo MR. Variations in patients' adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42:200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 32.Winkelmayer WC, Levin R, Setoguchi S. Associations of kidney function with cardiovascular medication use after myocardial infarction. Clin J Am Soc Nephrol. 2008;3:1415–1422. doi: 10.2215/CJN.02010408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hong TB, Oddone EZ, Dudley TK, Bosworth HB. Medication barriers and anti-hypertensive medication adherence: the moderating role of locus of control. Psychol Health Med. 2006;11:20–28. doi: 10.1080/14786430500228580. [DOI] [PubMed] [Google Scholar]
- 34.Ogedegbe G, Harrison M, Robbins L, Mancuso CA, Allegrante JP. Barriers and facilitators of medication adherence in hypertensive African Americans: a qualitative study. Ethn Dis. 2004;14:3–12. [PubMed] [Google Scholar]
- 35.Shea S, Misra D, Ehrlich MH, Field L, Francis CK. Correlates of nonadherence to hypertension treatment in an inner-city minority population. Am J Public Health. 1992;82:1607–1612. doi: 10.2105/ajph.82.12.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Horne R, Weinman J. Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47:555–567. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 37.Krousel-Wood M, Muntner P, Jannu A, Desalvo K, Re RN. Reliability of a medication adherence measure in an outpatient setting. Am J Med Sci. 2005;330:128–133. doi: 10.1097/00000441-200509000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17:504–511. doi: 10.1046/j.1525-1497.2002.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Choo PW, Rand CS, Inui TS, et al. Validation of patient reports, automated pharmacy records, and pill counts with electronic monitoring of adherence to antihypertensive therapy. Med Care. 1999;37:846–857. doi: 10.1097/00005650-199909000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Krousel-Wood M, Islam T, Webber LS, Re RN, Morisky DE, Muntner P. New medication adherence scale versus pharmacy fill rates in seniors with hypertension. Am J Manag Care. 2009;15:59–66. [PMC free article] [PubMed] [Google Scholar]
- 41.Weiner DE, Tighiouart H, Levey AS, et al. Lowest systolic blood pressure is associated with stroke in stages 3 to 4 chronic kidney disease. J Am Soc Nephrol. 2007;18:960–966. doi: 10.1681/ASN.2006080858. [DOI] [PubMed] [Google Scholar]
- 42.Muntner P, He J, Astor BC, Folsom AR, Coresh J. Traditional and nontraditional risk factors predict coronary heart disease in chronic kidney disease: results from the atherosclerosis risk in communities study. J Am Soc Nephrol. 2005;16:529–538. doi: 10.1681/ASN.2004080656. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Prevalence of uncontrolled hypertension among REGARDS participants taking antihypertensive medication with and without CKD, by level of medication adherence.
Figure S2. Multivariable adjusted ORs for uncontrolled hypertension associated with responses to the 4-item medication adherence screen among REGARDS participants taking antihypertensive medication with and without CKD.