Abstract
Delay discounting is an index of impulsive decision-making and reflects an individual’s preference for smaller immediate rewards relative to larger delayed rewards. Multiple studies have indicated comparatively high rates of discounting among tobacco, alcohol, cocaine, and other types of drug users, but few studies have examined discounting among marijuana users. This report is a secondary analysis of data from a clinical trial that randomized adults with marijuana dependence to receive one of four treatments that involved contingency management (CM) and cognitive–behavioral therapy interventions. Delay discounting was assessed with the Experiential Discounting Task (Reynolds & Schiffbauer, 2004) at pretreatment in 93 participants and at 12 weeks posttreatment in 61 participants. Results indicated that higher pretreatment delay discounting (i.e., more impulsive decision-making) significantly correlated with lower readiness to change marijuana use (r = − 0.22, p = .03) and greater number of days of cigarette use (r = .21, p = .04). Pretreatment discounting was not associated with any marijuana treatment outcomes. CM treatment significantly interacted with time to predict change in delay discounting from pre- to posttreatment; participants who received CM did not change their discounting over time, whereas those who did not receive CM significantly increased their discounting from pre- to posttreatment. In this sample of court-referred young adults receiving treatment for marijuana dependence, delay discounting was not strongly related to treatment outcomes, but there was some evidence that CM may protect against time-related increases in discounting.
Keywords: marijuana, cannabis, delay discounting, impulsivity, marijuana treatment
Over four million Americans meet criteria for marijuana use disorders, and one million Americans received treatment for marijuana use in 2010 (Substance Abuse & Mental Health Services Administration, 2011). Although there are now several empirically validated therapies for marijuana use disorders (Denis, Lavie, Fatseas, & Auriacombe, 2008), abstinence rates reported for existing interventions are modest. One potential strategy for improving marijuana abstinence involves identifying individual characteristics that predict poor treatment response and tailoring interventions to more effectively address these characteristics.
Delay discounting is one individual characteristic that may predispose substance users to poor treatment response. Delay discounting is an index of impulsive decision-making and reflects individuals’ preference for smaller immediate rewards relative to larger delayed rewards (Ainslie, 1975; Kirby, 1997; Logue, 1988). Delay discounting has substantial relevance for understanding addictive behavior, as it may explain individuals’ preference for immediate transient effects of drug use at the cost of future benefits from abstinence, as well as self-control failure and ambivalence related to abstinence. A recent meta-analysis of discounting and addictive behavior demonstrated that high rates of discounting characterize individuals with addictive behaviors, particularly individuals who meet criteria for an addictive disorder (MacKillop et al., 2011). However, few studies have examined discounting in marijuana users. One study of adults with current marijuana dependence, former marijuana dependence, or no history of regular marijuana use observed that discounting showed a nonsignificant trend toward being higher in individuals with current marijuana dependence compared with the other two groups; thus, the effect size of discounting may be smaller for marijuana than for other drugs (Johnson et al., 2010).
One explanation for the relationship of delay discounting to poor treatment response may be the concurrent relationship of delay discounting with other characteristics that themselves impact response to treatment. For example, characteristics that predict poor abstinence outcomes or treatment retention include greater severity of substance use (Adamson, Sellman, & Frampton, 2009; Foulds et al., 2006); polysubstance use (see reviews by Agrawal, Budney, & Lynskey, 2012 and Peters, Budney, & Carroll, 2012; Poling, Kosten, & Sofuoglu, 2007; Toneatto, Sobell, Sobell, & Kozlowski, 1995); and higher self-reported impulsivity (Patkar et al., 2004), all of which are related to more impulsive discounting (de Wit, Flory, Acheson, McCloskey, & Manuck, 2007; Kirby & Petry, 2004; Kirby, Petry, & Bickel, 1999; Mitchell, Fields, D’Esposito, & Boettiger, 2005; Petry, 2001; Petry & Casarella, 1999; Sweitzer, Donny, Dierker, Flory, & Manuck, 2008; cf., Crean, de Wit, & Richards, 2000; Dom, De Wilde, Hulstijn, & Sabbe, 2007; Dom, De Wilde, Hulstijn, van den Brink, & Sabbe, 2006; Mitchell, 1999). Readiness to change is commonly assessed in treatment outcome studies because of its association with treatment response (DiClemente & Hughes, 1990; McKay & Weiss, 2001), yet to our knowledge, its relationship to delay discounting has not been described.
Although most studies of delay discounting are cross-sectional in nature, data from randomized clinical trials of addiction treatments that longitudinally evaluate correlates of discounting are now emerging. Generally, higher pretreatment delay discounting (i.e., more impulsive decision-making) is associated with poorer abstinence outcomes in tobacco smokers (Krishnan-Sarin et al., 2007; MacKillop & Kahler, 2009; Sheffer et al., 2012; Yoon et al., 2007) and cocaine users (Washio et al., 2011). Other indices of impulsive decision-making have associations with abstinence outcomes in alcohol drinkers (Tucker, Roth, Vignolo, & Westfall, 2009; Tucker, Vuchinich, Black, & Rippens, 2006; Tucker, Vuchinich, & Rippens, 2002) and opiate users (Passetti et al., 2011; Passetti, Clark, Mehta, Joyce, & King, 2008). Only one study has evaluated how pretreatment discounting is associated with abstinence outcomes in marijuana users (Stanger et al., 2012). In this study, adolescent marijuana users completed four different discounting tasks: two with hypothetical monetary rewards with magnitudes of $100 and $1,000 as the reinforcer, and two with amounts of marijuana subjectively equivalent to $100 and $1,000 as the reinforcer. Discounting of $1,000 of money was related to several abstinence outcomes; however, discounting of the smaller magnitude of money and of either amount of marijuana were not. Evaluating the relationship of delay discounting to established clinical indicators and to abstinence outcomes is important for understanding shared and unique contributions of delay discounting to treatment response.
The emerging clinical trials literature also suggests that discounting appears stable over time (Audrain-McGovern et al., 2009; Beck & Triplett, 2009; Kirby, 2009; Takahashi, Furukawa, Miyakawa, Maesato, & Higuchi, 2007). Thus, some assert that discounting may be considered a personality trait (Odum, 2011). Arguing against the stability of discounting over time, however, are studies showing that short-term deprivation from substance use increases, and psychosocial treatment for substance use decreases, impulsive responding. For example, among smokers, 13 hours of deprivation from nicotine was associated with an increase in discounting for cigarettes (Field, Santarcangelo, Sumnall, Goudie, & Cole, 2006), and five days of reductions in nicotine use were related to increases in discounting of cigarettes and monetary rewards (Yi et al., 2008). Similarly, opioid deprivation was associated with increases in discounting of both heroin and monetary rewards among opioid-dependent adults (Giordano et al., 2002). On the other hand, receiving buprenorphine plus either contingency management or standard counseling was related to reductions in discounting among opioid-dependent individuals (Landes, Christiansen, & Bickel, in press), and receiving 12-step and relapse prevention treatment was associated with significant decreases in performance on the Balloon Analogue Risk Task, a measure of risk-taking propensity, but not in discounting (Aklin, Tull, Kahler, & Lejuez, 2009).
Given conflicting findings on the malleability of discounting over time, further research appears warranted, and research on specific types of substance use treatment that are associated with changes in discounting would be especially beneficial. For example, contingency management appears to be an especially effective treatment for substance users with higher discounting due to its provision of relatively immediate rewards (Marlowe, Festinger, Dugosh, Arabia, & Kirby, 2008; Petry, 2002) and, thus, may also have therapeutic effects on discounting.
This report describes a secondary analysis of data on delay discounting among adults in a randomized clinical trial of psychosocial treatments for marijuana dependence (Carroll et al., 2012) and aims to address three hypotheses. First, we hypothesized that pretreatment delay discounting would correlate with indicators of treatment response; specifically, we hypothesized that higher discounting (i.e., more impulsive responding) would correlate with greater severity of marijuana use, higher self-reported impulsivity, greater tobacco use, and lower readiness to change marijuana use. Second, we hypothesized that higher pretreatment delay discounting would be associated with poorer treatment abstinence and retention across study treatments. Third, we investigated whether the specific treatments provided in this trial [contingency management (CM) and cognitive–behavioral therapy (CBT)] were associated with changes in discounting over time. Because CM has been associated with improvement in discounting in opioid users (Landes et al., in press), we hypothesized that CM would be associated with improvement in discounting in these marijuana users. To our knowledge, no study has yet evaluated the impact of CBT on discounting; thus, we had no specific hypotheses about the direction of the effect of CBT on discounting over time.
Method
Participants
Participants in the primary trial were 127 individuals aged 18 and above who met Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM–IV; American Psychiatric Association, 2000) criteria for current marijuana dependence. Although participants could have self-referred for treatment, the majority (93.7%) of randomized individuals were referred for marijuana treatment by the Office of Adult Probation to the Substance Abuse Treatment Unit in New Haven, Connecticut. Participants provided written informed consent to participate and were randomized to receive one of four psychosocial treatments provided over the course of 12 weeks.
Treatment
Cognitive-Behavioral Therapy (CBTalone)
CBTalone was delivered in 50-min individual weekly sessions. CBT encouraged marijuana abstinence using standard techniques such as functional analysis for high-risk situations, coping strategies development, and cognitive restructuring related to marijuana use (Steinberg et al., 2005). Material discussed during each session was supplemented with extra-session homework tasks intended to foster implementation and mastery of skills.
CBT + CM for Adherence (CBT + CMadher)
In addition to CBT as above, participants in this condition were offered chances to win prizes contingent on session attendance and homework completion. Following procedures developed by Petry (Petry, Alessi, Marx, Austin, & Tardif, 2005; Petry, Martin, Cooney, & Kranzler, 2000; Petry, Tedford, & Martin, 2001), participants earned two draws each time they attended a CBT session. The number of draws earned escalated by one draw per consecutive weekly session of scheduled attendance. If a participant failed to attend a scheduled session, the number of draws earned reset to two for the next session attended. To promote extra-session skill practice, participants could earn bonus draws contingent on bringing completed homework assignments to their CBT sessions. Reinforcement for homework completion also occurred on an escalating schedule, with the number of bonus draws starting at one and escalating by one draw per consecutive time homework was completed, to a maximum of 13 bonus draws per session. Participants who were fully compliant with attendance and homework assignments could earn a maximum of 178 draws.
The same prize bowl was used for all three CM conditions (outlined below), in which, on average, participants had an expected maximum earning of $250 in prizes. The bowl contained 650 cards of which 375 were winning cards. Of these, 269 were small prizes (participant’s choice of $1 fast food coupons, bus tokens, etc.), 75 were medium prizes worth up to $5 in value (t-shirts, hats, etc.), 30 were large prizes worth up to $20 in value (movie tickets, CDs, phone cards, etc.), and one jumbo prize worth up to $100 (small TV, or five large prizes).
CM for abstinence (CMabst)
Participants in this condition had the opportunity to draw from a bowl and earn prizes each time they provided urine samples that were negative for marijuana at the 12 weekly assessment sessions. At the first assessment session where the participant provided a urine sample that tested negative for marijuana, he earned four draws. To promote continuous abstinence, the number of draws participants earned increased by two for each successive negative sample submitted, up to a maximum of 26 draws per weekly session. Participants could earn up to 180 drawings. Participants were not offered individual CBT or other treatment but met weekly with a research assistant. Meetings were about five minutes long and limited to collection of urine samples, calculation and redemption of prizes, as well as minimal monitoring via the Timeline Follow-Back (TLFB; Sobell & Sobell, 1992).
CM for abstinence plus CBT (CMabst+CBT)
Participants in this condition received prize CM for submitting urine specimens negative for marijuana and weekly individual CBT as above. CBT was adapted for this condition in order to facilitate more durable CM effects. Unlike in the CBTalone condition, therapists in this condition addressed the following issues: (a) identification of behaviors or skills that were implemented when the participant submitted marijuana-negative urine specimens; (b) focus on the participant’s cognitions regarding his decision to use or not use marijuana, encouraging recognition of these decisions as choices so as to foster internal attribution of change; (c) practice of specific skills and strategies the participant could use to earn draws in the future; and (d) encouragement of self-rewards to offset dependence on external reinforcers.
Procedure
Participants were assessed at pretreatment, weekly during treatment, at 12-weeks posttreatment, and at 3-month intervals for 1 year. Complete self-reported substance use data were available for 87% of the randomized sample at the 12-week posttreatment assessment and for 69% of the randomized sample at the 1-year follow-up assessment, with no significant differences in assessment completion by treatment condition. Study procedures were approved by the Yale University Human Investigations Committee.
Assessments
Pretreatment
Self-report assessments gathered information on demographics and history of substance use. Percentage of days in the 28 days pretreatment in which participants used marijuana and cigarettes was assessed with the TLFB (Sobell & Sobell, 1992). Trait impulsivity was assessed with the Barratt Impulsiveness Scale–11 (BIS−11; Patton, Stanford, & Barratt, 1995) and the Behavioral Inhibition System/Behavioral Activation System (BIS/BAS; Carver & White, 1994). The BIS−11 yields subscale scores of Nonplanning, Motor, and Attentional Impulsivity, and the BIS/BAS yields subscale scores of Inhibition, Reward Responsiveness, Drive, and Fun-Seeking; higher subscale scores indicate higher impulsivity. Readiness to change marijuana use was assessed with the 32-item University of Rhode Island Change Assessment (URICA; DiClemente & Hughes, 1990). URICA items are averaged to yield subscale scores of Precontemplation, Contemplation, Action, and Maintenance, and Readiness Composite scores are calculated by subtracting Precontemplation subscale scores from the sum of scores on the Contemplation, Action, and Maintenance subscales. Higher Readiness Composite scores indicate greater readiness to change.
Delay discounting was assessed with the Experiential Discounting Task (EDT; Reynolds & Schiffbauer, 2004). The EDT is a computerized real-time task in which participants experience chosen rewards at specified times throughout the assessment. Participants completed four session blocks associated with different time delays, three of which involved choices between an adjusting and certain amount (initially, $0.15) that was delivered immediately or a standard amount of $0.30 that was delayed and had a 35% chance of being delivered, that is, expected value of $0.10 (1/2). For the other session block, there was no delay to the standard option.
Choice options were indicated by the “illumination” of light bulbs on the computer screen. The adjusting immediate amount was adjusted in value (i.e., increased by a set percentage following an immediate choice). As described in Reynolds and Schiffbauer (2004), the adjusting-option amount was always set to an initial value of $0.15 (half of the standard-option amount). Following a response to the adjusting option, the adjusting-option amount decreased in value, but it inversely increased in value following responses to the standard option. The initial percentage of decrease or increase was always 15% of the starting adjusting-option value (rounded to the nearest cent). The percentage of change decreased at a rate of 2% for every choice that decreased or increased the adjusting-option amount from its initial value.
The delayed standard amount was fixed, and the standard option choice resulted in a wait of a specified delay (0, 7, 14, and 28 seconds). The standard option was made uncertain because of past research showing insensitivity to comparable delays when all options were certain (Hyten, Madden, & Field, 1994). Further, in more ecologically valid choice contexts, delayed options are necessarily uncertain due to possible intervening factors that might occur during the delay-to-reward period (Reynolds & Schiffbauer, 2004). Thus, the uncertainty of the task’s delayed option helps to more fully model naturalistic choice contexts involving delays.
If the money was delivered, it could be transferred to the “bank” by clicking on the “illuminated” bank building image, which resulted in coin delivery from a coin dispenser. Money was transferred to the “bank” in order to depict the amount of money that participants would receive upon completion of the task and to provide real-time consummatory feedback.
For each choice block, participants made choices until an indifference point was reached, defined as choosing an option (i.e., immediate and delayed) three times within six consecutive choice trials, thus holding the adjusting amount constant over those six choices. After an indifference point was established or the delayed option was chosen 15 times (reflecting minimal discounting), the session ended. The remaining sessions (7, 14, and 28 seconds) were completed in ascending order.
The indifference points were normalized by dividing all indifference points to the indifference point at 0-s delay to control for individual differences in probabilistic discounting. For each participant, the four normalized indifference points for each delay were fit with the hyperbolic function (Mazur, 1987) of indifference point = (larger later amount)/(1 + k * delay). This function was used to calculate the free parameter k, which was used as the index of delay discounting. Higher k represents higher discounting (i.e., more impulsive decision-making).
The EDT was introduced to this study after the first 14 randomized participants enrolled, so 113 participants were available for the pre- and posttreatment assessment. Of the 113 participants available at pretreatment, 13 participants did not complete the task and seven completed the task but had data that could not be analyzed (e.g., had missing data at the 0-s delay session); thus, 93 participants were included in analyses of pretreatment delay discounting. Of the 113 potential participants at the 12-week post-treatment assessment, 50 participants did not complete the task and two had data that could not be analyzed (e.g., computer task malfunctioned); thus, 61 participants had valid posttreatment delay discounting scores. Pretreatment delay discounting scores did not significantly differ between participants who did and did not complete the posttreatment delay discounting assessment, t(91) = −0.20, p = .84, suggesting that those with higher pretreatment delay discounting were not more or less likely to have missing posttreatment values.
Posttreatment
Weekly throughout treatment, the TLFB (Sobell & Sobell, 1992) collected self-report data on substance use since the prior assessment. Urine samples to verify self-report marijuana use data were collected pretreatment and weekly throughout treatment. Follow-up assessments included the TLFB and collection of urine samples. Posttreatment marijuana abstinence outcomes included: self-reported percent days of marijuana abstinence during treatment, biochemically verified longest period of marijuana abstinence during treatment, and percent of urines positive for marijuana during treatment. Number of days in treatment and treatment sessions attended were also examined. The follow-up marijuana abstinence outcome was self-reported percent days of marijuana abstinence during follow-up.
Data Analysis
Bivariate Pearson correlations examined the concurrent associations of pretreatment delay discounting with age, percentage of days of marijuana and cigarette use in the 28 days prior to treatment, age first used marijuana, URICA Readiness Composite score, and BIS−11 and BIS/BAS subscale scores. For categorical variables, independent-samples t tests examined concurrent associations of pretreatment delay discounting by comparing discounting scores between demographic groups based on race (White vs. non-White), education (high school graduate vs. less than high school graduate), gender (male vs. female), marital status (married vs. not married), and employment status (working full- or part-time vs. not working).
Linear regression models examined the predictive associations of pretreatment delay discounting with the posttreatment and follow-up outcomes from the primary trial (identified above). Generalized estimating equations (GEEs) modeled the main effects of time (pre- and posttreatment) and treatment, and the interaction of time and treatment, on change in delay discounting scores from pretreatment to posttreatment. GEE models incorporate all available data (i.e., do not exclude individuals who are missing any observations) and were used to minimize any influence of missing posttreatment EDT data on change in discounting from pre- to posttreatment. Three a priori treatment contrasts were examined in the parent trial (Carroll et al., 2012) and, thus, were examined in this report through a series of three GEEs: (a) contrasts of the four treatment groups; (b) contrasts of the three treatments that incorporated CM versus the one that did not (CBT + CMadher, CMabst, CMabst + CBT vs. CBTalone); and (c) contrasts of the three treatments that incorporated CBT versus the one that did not (CBT + CMadher, CMabst + CBT, CBTalone vs. CMabst). Consistent with prior studies of delay discounting in marijuana users (Johnson et al., 2010; Stanger et al., 2012), k parameter estimates of pretreatment and posttreatment delay discounting were positively skewed and were transformed with the natural logarithm (ln k) prior to statistical analysis.
Results
Sample Description
Table 1 presents characteristics of the 93 participants who completed the pretreatment EDT. The median untransformed k value was 0.036 (25th–75th percentiles = 0.022–0.074) at pre-treatment, and the mean transformed value (ln k) was −3.2 [standard deviation (SD) = 0.9]. Pretreatment delay discounting rates in the current sample were higher than in prior samples of adults who have completed the EDT; the median untransformed k value among cigarette smokers was 0.028 (Reynolds, 2006) and among social drinkers was 0.008 (Reynolds, Richards, & de Wit, 2006), with higher k values indicating more impulsive decision-making. Discounting rates (ln k) did not differ among participants in the four treatment groups, F(3, 89) = 0.22, p = .88, between those who did and did not receive CM, t(91) = 0.24, p = .81, or between those who did and did not receive CBT, t(91) = 0.57, p = .57.
Table 1.
Sample Characteristics (N = 93)
| Pretreatment characteristic | Mean (Standard deviation)/% |
|---|---|
| Age | 26.1 (7.5) |
| % Female | 14.0 |
| % Caucasian | 19.4 |
| % Married/cohabiting | 10.8 |
| % High school education | 58.1 |
| % Unemployed | 38.7 |
| Days of substance use in 28 days prior to treatment | |
| Marijuana | 15.8 (9.8) |
| Cigarette | 18.8 (12.6) |
| Alcohol | 2.3 (3.6) |
| % Daily cigarette smokers | 63.4 |
| Delay discounting score (natural logarithm of k) | −3.2 (0.9) |
Pretreatment Delay Discounting and Indicators of Treatment Response
Delay discounting rates (ln k) did not significantly differ based on race, education, gender, marital status, or employment status and did not correlate with age. Pretreatment discounting rates were not associated with frequency of current marijuana use, age of marijuana use onset, or self-reported impulsivity (see Table 2). However, higher delay discounting rates did significantly correlate with lower URICA Readiness Composite scores and greater percent days of cigarette use in the 28 days prior to the pretreatment assessment.
Table 2.
Zero-Order Correlations Between Pretreatment Delay Discounting and Indicators of Treatment Response (N = 93)
| Pretreatment characteristic | r |
|---|---|
| Percent days of substance use in 28 days prior to treatment | |
| Marijuana | −.04 |
| Cigarette | .21* |
| URICA Readiness Composite Score | −.22* |
| Age first used marijuana | .08 |
| Barratt Impulsivity Scale–11 | |
| Nonplanning impulsivity | .00 |
| Motor impulsivity | −.02 |
| Attentional impulsivity | −.02 |
| Behavioral Inhibition System/Behavioral Activation System | |
| Inhibition | −.11 |
| Reward responsiveness | −.11 |
| Drive | .01 |
| Fun-seeking | .04 |
Note. Pearson product-moment correlation coefficients (r) are presented.
URICA = University of Rhode Island Change Assessment.
p <.05.
Delay Discounting and Treatment Outcomes
Pretreatment delay discounting rates did not significantly predict any posttreatment or follow-up marijuana use outcome (see Table 3). Post hoc tests evaluated whether significant correlates of discounting, that is, pretreatment URICA Readiness Composite scores and days of cigarette use, were associated with treatment outcomes. Higher URICA Readiness Composite scores significantly related to greater percent days of marijuana abstinence during treatment (β = 0.24, p = .03) but did not relate to any other outcome. Frequency of pretreatment cigarette use was not associated with any marijuana use outcome.
Table 3.
Pretreatment Delay Discounting as a Predictor of Treatment Outcomes
| Outcome | β |
|---|---|
| Percent days of marijuana abstinence during treatment | .06 |
| Maximum consecutive days of marijuana abstinence during treatment | −.07 |
| Percent marijuana-positive urine specimens during treatment | .03 |
| Number of days in treatment | .10 |
| Number of treatment sessions attended | .01 |
| Percent days of marijuana abstinence during follow-up | .01 |
Note. Standardized coefficients (β) from linear regression models are presented, with delay discounting scores (natural logarithm of k) as the predictor. Posttreatment outcomes were assessed at 12 weeks, and the follow-up outcome was assessed at 1 year.
In the GEE that evaluated the effect of time and the contrasts among the four treatment groups in predicting the change in discounting rates from pre- to posttreatment, there was a significant main effect of time (Wald = 4.79, df = 1, p = .03), such that posttreatment discounting rates (M = −2.85, SD = 1.21) were higher than pretreatment rates (M = −3.17, SD = 0.89) in the omnibus test across all four treatment groups. There was no significant main effect of treatment group (Wald = 4.94, df = 3, p = .18) and no significant interaction of time and treatment group (Wald = 6.61, df = 3, p = .09).
In the GEE that evaluated the effect of time and the contrast of the three treatments that provided CM versus the one that did not (Figure 1), there was a significant interaction of time and CM treatment in predicting the change in discounting rates from pre- to posttreatment (Wald = 5.36, df = 1, p = .02); participants who received any type of CM treatment had mean discounting scores of −3.19 (SD = 0.82) at pretreatment and −3.09 (SD = 0.92) at posttreatment, although those who did not receive CM treatment had mean scores of −3.14 (SD = 1.08) at pretreatment and −2.08 (SD = 1.65) at posttreatment. The increase in discounting from pretreatment to posttreatment that was observed in the omnibus test assessing time effects may, therefore, be attributed primarily to the individuals who did not receive CM. In the GEE the evaluated the effect of time and the contrast of the three treatments that provided CBT versus the one that did not, there was no interaction of time and CBT treatment (Wald = 0.17, df = 1, p = .68), and no main effect of time (Wald = 2.36, df = 1, p = .13) or CBT treatment (Wald = 0.06, df = 1, p = .81).
Figure 1.
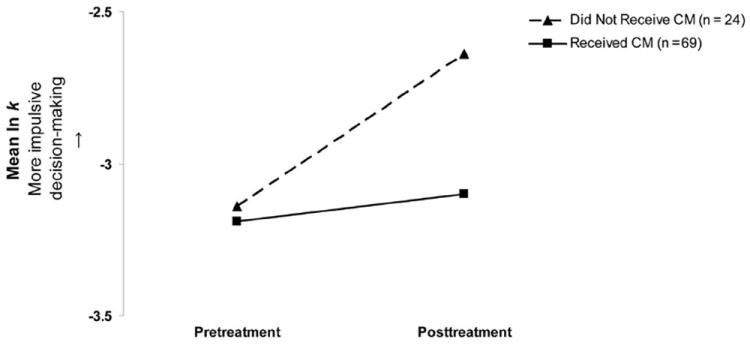
Effect of Contingency Management Treatment on Posttreatment Delay Discounting. Participants in the three treatment conditions that provided contingency management are represented by the solid lines with rectangles, and participants in the one treatment condition that did not provide contingency management are represented by the dashed line with triangles. Assessment timepoints are plotted on the x-axis, and mean natural logarithm (ln) of k values are plotted on the y-axis. Higher ln k values indicate higher delay discounting (i.e., more impulsive decision-making). CM = contingency management.
Discussion
Three main findings can be drawn from this examination of delay discounting among adults receiving psychosocial treatments for marijuana dependence: (a) higher pretreatment delay discounting significantly correlated with lower readiness to change marijuana use and greater frequency of tobacco use but did not correlate with pretreatment demographic or marijuana use or severity variables, (b) pretreatment delay discounting was not significantly associated with marijuana use outcomes during treatment or follow-up or with retention in treatment, and (c) the psychosocial interventions provided in this study were not associated with significant improvements in discounting over time, although a significant interaction effect emerged between CM and non-CM treatments over time.
Delay discounting has been associated with multiple indicators of substance use severity and impulsivity in prior studies of adults who smoke tobacco, drink alcohol, and use other drugs of abuse; therefore, we hypothesized that we would observe similar patterns among adults with marijuana dependence. Contrary to expectation, pretreatment discounting did not significantly correlate with frequency of pretreatment marijuana use or age of marijuana use onset. The lack of association between discounting and marijuana use was not expected due to several prior studies with smokers, drinkers, and drug abusers in which discounting has been significantly related to individuals’ use of their primary drug; however, it is in agreement with one prior study in nontreatment-seeking adult marijuana users in which discounting was not robustly associated with marijuana use (Johnson et al., 2010). Also contrary to expectation, pretreatment discounting did not significantly correlate with self-reported impulsivity. Although behaviorally assessed discounting seems to overlap conceptually with self-reported impulsivity and has correlated with self-reported impulsivity in some studies (de Wit et al., 2007; Kirby et al., 1999; Mitchell et al., 2005), our results are more consistent with studies demonstrating that discounting and impulsivity appear to be distinct constructs (Crean et al., 2000; Dom et al., 2007; Dom et al., 2006; Mitchell, 1999).
Of note, higher delay discounting correlated with lower readiness to change marijuana use, suggesting that individuals who discount at high rates may be less ready to alter their marijuana use when initiating treatment. Furthermore, lower readiness to change was related to fewer days of marijuana abstinence in this study and has related to poorer outcomes in other studies (DiClemente & Hughes, 1990; McKay & Weiss, 2001). Although the current study did not set out to explicate the relationships among discounting, readiness to change, and marijuana treatment outcomes, an interesting focus of future research might be the evaluation of how discounting and readiness to change interact to predict marijuana treatment outcomes. Pretreatment delay discounting was also associated with greater tobacco smoking, similar to other studies (Johnson et al., 2010; MacKillop et al., 2011). Tobacco smoking, however, was not associated with any marijuana treatment outcomes. Overall, the few direct relationships between discounting and clinical indicators suggest that, among legally referred adults with marijuana dependence, discounting may not contribute substantial information relevant to treatment.
Delay discounting has been associated with poorer outcomes in prior treatment studies with tobacco- and cocaine-using populations (Krishnan-Sarin et al., 2007; MacKillop & Kahler, 2009; Sheffer et al., 2012; Washio et al., 2011; Yoon et al., 2007); therefore, we hypothesized that discounting would have similar associations with marijuana treatment outcomes. Pre-treatment delay discounting, however, was not significantly associated with posttreatment or follow-up marijuana use outcomes. The lack of association contrasts with results from the only other study of the ability of discounting to predict marijuana treatment outcomes, in which responding to a discounting task was significantly associated with posttreatment marijuana use outcomes among adolescents (Stanger et al., 2012).
Methodological differences between the current study and the Stanger et al. (2012) study may explain divergent findings. First, sample differences (i.e., adults in the current sample and adolescents in the Stanger et al. (2012) study) may underlie differences in decision-making, as brain systems responsible for effective decision-making are still under development in adolescence (Casey, Jones, & Hare, 2008). Second, several aspects of the discounting tasks may account for different patterns of results. The EDT used in this study is a discounting task that was designed to be naturalistic (i.e., model real-world choice scenarios), to provide feedback in real time, and to provide the actual amount of money chosen at the completion of the task, while the tasks used in the Stanger et al. (2012) study were for hypothetical amounts of money and marijuana. In the EDT, delays were in real time and terminated at 28 seconds, while the delays in the Stanger et al. (2012) study were hypothetical and terminated at 6 months. Finally, the magnitude of rewards differed in the two studies: the maximum amount of reward in this study was $0.30, while the maximum amount in the Stanger et al. (2012) study was $1,000. Importantly, in the Stanger et al. (2012) study, responding to a discounting task with a magnitude of $1,000 predicted outcomes, although responding to a task with a smaller magnitude of $100 did not; thus, in the current study, the magnitude of reward ($0.30) may not have been sufficient to evidence relationships with treatment outcome.
Regardless of differences in features of the discounting tasks, the EDT has correlated with other measures of discounting using hypothetical rewards (Reynolds, 2006; Reynolds et al., 2006; cf., Krishnan-Sarin et al., 2007), suggesting that discounting measures with real-time and hypothetical rewards likely assess the similar construct of impulsive decision-making (Reynolds, Penfold, & Patak, 2008). Nonetheless, different features of the discounting tasks may have contributed to divergent findings on the ability of discounting to predict marijuana treatment outcomes. Future studies that evaluate larger magnitude rewards across similar samples may resolve discrepant findings on the predictive potential of discounting among marijuana users.
Another potential explanation for the lack of relationship between discounting and marijuana treatment outcomes may concern the nature of this sample. This sample’s rates of discounting appeared higher than in other samples who have completed the EDT (Reynolds, 2006; Reynolds et al., 2006), indicating that discounting rates are relatively high among young adults with marijuana dependence. However, most individuals in this sample were receiving treatment because they were pressed to do so by the criminal justice system. Perhaps due to their court-referred status, this sample was characterized by low engagement in treatment (Carroll et al., 2012). Thus, it is possible that, relative to discounting, factors such as criminal history and treatment engagement bear stronger relationships to marijuana treatment outcomes. Future studies with marijuana users seeking treatment of their own volition may reveal different patterns of association between discounting and marijuana use.
Few studies exist on how substance abuse treatment may reduce discounting of delayed rewards, although available evidence supports the beneficial impact of CM on discounting in opioid users (Landes et al., in press). Therefore, we hypothesized that CM would improve posttreatment discounting in marijuana users. While receiving any type of CM did significantly interact with time to lead to a change in discounting, CM was not associated with improvement in discounting but instead was related to maintenance of discounting; patients who did not receive CM demonstrated increases in discounting over time. The examination of the effect of psychosocial treatments on discounting may have been confounded by the fact that participants who received any type of CM received additional rewards during treatment, and those who received CBT only did not. That is, monetary rewards provided in the context of treatment may have confounded the discounting of monetary rewards provided in the context of the task. Additional studies are needed and should attempt to minimize such confounds, but if these results are replicated, they may indicate that CM has protective effects on potential changes in discounting.
Strengths of this study include its assessment of delay discounting with a previously validated experimental paradigm (Reynolds & Schiffbauer, 2004) and use of data from a well-controlled randomized clinical trial with a reasonable interval (i.e., 12 weeks) separating assessments, thereby minimizing reactivity or practice effects. Limitations include a small sample size in each treatment condition, missing posttreatment delay discounting data from 32 participants, and lack of discounting data at the 1-year follow-up assessment. Another limitation is the predominantly male sample. Although marijuana dependence is more common in men than women (Compton, Grant, Colliver, Glantz, & Stinson, 2004), a more balanced gender distribution would make results more generalizable to both men and women with marijuana dependence.
In summary, among a sample of court-referred adults receiving treatment for marijuana dependence, delay discounting did not appear to be robustly associated with marijuana use and was not significantly decreased by psychosocial interventions that targeted marijuana use. Nevertheless, a potentially intriguing interaction effect between CM treatment and changes in discounting over time was noted. If replicated, these results may suggest that CM has protective effects on discounting, but larger and longer-term studies are needed.
Acknowledgments
We gratefully acknowledge the assistance of Karen Hunkele and Cody Brennan for data management and preparation, Joanne Corvino for training and quality assurance, and Sally Vitollo, Haley Ford, and Monica Canning-Ball for carrying out the study. This research was supported by National Institute on Drug Abuse grants T32-DA007238 (ENP), P30-DA023918 (NMP), and P50-DA09241 (KMC). The funding sources had no role other than financial support. Drs. Carroll, Petry, and LaPaglia conceived and designed the study; Drs. LaPaglia and Reynolds provided assistance for data collection and assembly; Dr. Peters analyzed the data and wrote the first draft of the article and all authors contributed to writing. All authors approve the final article.
Footnotes
The authors have no conflicts of interest to declare.
Contributor Information
Erica N. Peters, Department of Psychiatry, Yale University School of Medicine
Nancy M. Petry, Department of Psychiatry, University of Connecticut Health Center
Donna M. LaPaglia, Department of Psychiatry, Yale University School of Medicine
Brady Reynolds, Department of Pediatrics, Ohio State University.
Kathleen M. Carroll, Department of Psychiatry, Yale University School of Medicine
References
- Adamson SJ, Sellman JD, Frampton CMA. Patient predictors of alcohol treatment outcome: A systematic review. Journal of Substance Abuse Treatment. 2009;36:75–86. doi: 10.1016/j.jsat.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Agrawal A, Budney AJ, Lynskey MT. The co-occurring use and misuse of cannabis and tobacco: A review. Addiction. 2012;107:1221–1233. doi: 10.1111/j.1360-0443.2012.03837.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ainslie G. Specious reward: A behavioral theory of impulsiveness and impulse control. Psychological Bulletin. 1975;82:463–496. doi: 10.1037/h0076860. [DOI] [PubMed] [Google Scholar]
- Aklin WM, Tull MT, Kahler CW, Lejuez CW. Risk-taking propensity changes throughout the course of residential substance abuse treatment. Personality and Individual Differences. 2009;46:454–459. doi: 10.1016/j.paid.2008.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Epstein LH, Cuevas J, Rodgers K, Wileyto EP. Does delay discounting play an etiological role in smoking or is it a consequence of smoking? Drug and Alcohol Dependence. 2009;103:99–106. doi: 10.1016/j.drugalcdep.2008.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck RC, Triplett MF. Test-retest reliability of a group-administered paper-pencil measure of delay discounting. Experimental and Clinical Psychopharmacology. 2009;17:345–355. doi: 10.1037/a0017078. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Nich C, LaPaglia DM, Peters EN, Easton CJ, Petry NM. Combining cognitive behavioral therapy and contingency management to enhance their effects in treating cannabis dependence: Less can be more, more or less. Addiction. 2012;107:1650–1659. doi: 10.1111/j.1360-0443.2012.03877.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, White TL. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS Scales. Journal of Personality and Social Psychology. 1994;67:319–333. doi: 10.1037//0022-3514.67.2.319. [DOI] [Google Scholar]
- Casey BJ, Jones RM, Hare TA. The adolescent brain. Annals of the New York Academy of Sciences. 2008;1124:111–126. doi: 10.1196/annals.1440.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. Journal of the American Medical Association. 2004;291:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- Crean JP, de Wit H, Richards JB. Reward discounting as a measure of impulsive behavior in a psychiatric outpatient population. Experimental and Clinical Psychopharmacology. 2000;8:155–162. doi: 10.1037/1064-1297.8.2.155. [DOI] [PubMed] [Google Scholar]
- Denis C, Lavie E, Fatseas M, Auriacombe M. Psychotherapeutic interventions for cannabis abuse and/or dependence in outpatient settings. Cochrane Database of Systematic Reviews. 2008;(3) doi: 10.1002/14651858.CD005336.pub2. Art No.: CD005336. [DOI] [PubMed] [Google Scholar]
- de Wit H, Flory JD, Acheson A, McCloskey M, Manuck SB. IQ and nonplanning impulsivity are independently associated with delay discounting in middle-aged adults. Personality and Individual Differences. 2007;42:111–121. doi: 10.1016/j.paid.2006.06.026. [DOI] [Google Scholar]
- DiClemente CC, Hughes SO. Stages of change profiles in outpatient alcoholism treatment. Journal of Substance Abuse. 1990;2:217–235. doi: 10.1016/S0899-3289(05)80057-4. [DOI] [PubMed] [Google Scholar]
- Dom G, De Wilde B, Hulstijn W, Sabbe B. Dimensions of impulsive behavior in abstinent alcoholics. Personality and Individual Differences. 2007;42:465–476. doi: 10.1016/j.paid.2006.08.007. [DOI] [Google Scholar]
- Dom G, De Wilde B, Hulstijn W, van den Brink W, Sabbe B. Behavioural aspects of impulsivity in alcoholics with and without a cluster-B personality disorder. Alcohol and Alcoholism. 2006;41:412–420. doi: 10.1093/alcalc/agl030. [DOI] [PubMed] [Google Scholar]
- Field M, Santarcangelo M, Sumnall H, Goudie A, Cole J. Delay discounting and the behavioural economics of cigarette purchases in smokers: The effects of nicotine deprivation. Psychopharmacology. 2006;186:255–263. doi: 10.1007/s00213-006-0385-4. [DOI] [PubMed] [Google Scholar]
- Foulds J, Gandhi KK, Steinberg MB, Richardson DL, Williams JM, Burke MV, Rhoades GG. Factors associated with quitting smoking at a tobacco dependence treatment clinic. American Journal of Health Behavior. 2006;30:400–412. doi: 10.5993/AJHB.30.4.6. [DOI] [PubMed] [Google Scholar]
- Giordano LA, Bickel WK, Loewenstein G, Jacobs EA, Marsch L, Badger GJ. Mild opioid deprivation increases the degree that opioid-dependent outpatients discount delayed heroin and money. Psychopharmacology. 2002;163:174–182. doi: 10.1007/s00213-002-1159-2. [DOI] [PubMed] [Google Scholar]
- Hyten C, Madden GJ, Field DP. Exchange delays and impulsive choice in adult humans. Journal of the Experimental Analysis of Behavior. 1994;62:225–233. doi: 10.1901/jeab.1994.62-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK, Baker F, Moore BA, Badger GJ, Budney AJ. Delay discounting in current and former marijuana-dependent individuals. Experimental and Clinical Psychopharmacology. 2010;18:99–107. doi: 10.1037/a0018333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby KN. Bidding on the future: Evidence against normative discounting of delayed rewards. Journal of Experimental Psychology: General. 1997;126:54–70. doi: 10.1037/0096-3445.126.1.54. [DOI] [Google Scholar]
- Kirby KN. One-year temporal stability of delay-discount rates. Psychonomic Bulletin & Review. 2009;16:457–462. doi: 10.3758/PBR.16.3.457. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM. Heroin and cocaine abusers have higher discount rates for delayed rewards than alcoholics or non-drug-using controls. Addiction. 2004;99:461–471. doi: 10.1111/j.1360-0443.2003.00669.x. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General. 1999;128:78–87. doi: 10.1037/0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Reynolds B, Duhig AM, Smith A, Liss T, McFetridge A, Potenza MN, et al. Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug and Alcohol Dependence. 2007;88:79–82. doi: 10.1016/j.drugalcdep.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landes RD, Christiansen DR, Bickel WK. Delay discounting decreases in those completing treatment for opioid dependence. Experimental and Clinical Psychopharmacology. doi: 10.1037/a0027391. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logue AW. Research on self-control: An integrating framework. Behavioral and Brain Sciences. 1988;11:665–709. doi: 10.1017/S0140525X00053978. in press. [DOI] [Google Scholar]
- MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, Munafò MR. Delayed reward discounting and addictive behavior: A meta-analysis. Psychopharmacology. 2011;216:305–321. doi: 10.1007/s00213-011-2229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Kahler CW. Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug and Alcohol Dependence. 2009;104:197–203. doi: 10.1016/j.drugalcdep.2009.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlowe DB, Festinger DS, Dugosh KL, Arabia PL, Kirby KC. An effectiveness trial of contingency management in a felony preadjudication drug court. Journal of Applied Behavior Analysis. 2008;41:565–577. doi: 10.1901/jaba.2008.41-565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazur JE. An adjusting procedure for studying delayed reinforcement. In: Commons ML, Mazur JE, Nevin JA, Rachlin H, editors. Quantitative analyses of behavior: The effects of delay and of intervening events on reinforcement value. Vol. 5. Hillsdale, NJ: Erlbaum; 1987. pp. 55–73. [Google Scholar]
- McKay JR, Weiss RV. A review of temporal effects and outcome predictors in substance abuse treatment studies with long-term follow-ups. Preliminary results and methodological issues. Evaluation Review. 2001;25:113–161. doi: 10.1177/0193841X0102500202. [DOI] [PubMed] [Google Scholar]
- Mitchell JM, Fields HL, D’Esposito M, Boettiger CA. Impulsive responding in alcoholics. Alcoholism: Clinical and Experimental Research. 2005;29:2158–2169. doi: 10.1097/01.alc.0000191755.63639.4a. [DOI] [PubMed] [Google Scholar]
- Mitchell SH. Measures of impulsivity in cigarette smokers and non-smokers. Psychopharmacology. 1999;146:455–464. doi: 10.1007/PL00005491. [DOI] [PubMed] [Google Scholar]
- Odum AL. Delay discounting: Trait variable? Behavioural Processes. 2011;87:1–9. doi: 10.1016/j.beproc.2011.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passetti F, Clark L, Davis P, Mehta MA, White S, Checinski K, Abou-Saleh M, et al. Risky decision-making predicts short-term outcome of community but not residential treatment for opiate addiction. Implications for case management. Drug and Alcohol Dependence. 2011;118:12–18. doi: 10.1016/j.drugalcdep.2011.02.015. [DOI] [PubMed] [Google Scholar]
- Passetti F, Clark L, Mehta MA, Joyce E, King M. Neuropsychological predictors of clinical outcome in opiate addiction. Drug and Alcohol Dependence. 2008;94:82–91. doi: 10.1016/j.drugalcdep.2007.10.008. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Murray HW, Mannelli P, Gottheil E, Weinstein SP, Vergare MJ. Pre-treatment measures of impulsivity, aggression and sensation seeking are associated with treatment outcome for African-American cocaine-dependent patients. Journal of Addictive Diseases. 2004;23:109–122. doi: 10.1300/J069v23n02_08. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768∷AID-JCLP2270510607>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Peters EN, Budney AJ, Carroll KM. Clinical correlates of co-occurring cannabis and tobacco use: A systematic review. Addiction. 2012;107:1404–1417. doi: 10.1111/j.1360-0443.2012.03843.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM. Delay discounting of money and alcohol in actively using alcoholics, currently abstinent alcoholics, and controls. Psychopharmacology. 2001;154:243–250. doi: 10.1007/s002130000638. [DOI] [PubMed] [Google Scholar]
- Petry NM. Discounting of delayed rewards in substance abusers: Relationship to antisocial personality disorder. Psychopharmacology. 2002;162:425–432. doi: 10.1007/s00213-002-1115-1. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Marx J, Austin M, Tardif M. Vouchers versus prizes: Contingency management treatment of substance abusers in community settings. Journal of Consulting and Clinical Psychology. 2005;73:1005–1014. doi: 10.1037/0022-006X.73.6.1005. [DOI] [PubMed] [Google Scholar]
- Petry NM, Casarella T. Excessive discounting of delayed rewards in substance abusers with gambling problems. Drug and Alcohol Dependence. 1999;56:25–32. doi: 10.1016/S0376-8716(99)00010-1. [DOI] [PubMed] [Google Scholar]
- Petry NM, Martin B, Cooney JL, Kranzler HR. Give them prizes, and they will come: Contingency management for treatment of alcohol dependence. Journal of Consulting and Clinical Psychology. 2000;68:250–257. doi: 10.1037//0022-006X.68.2.250. [DOI] [PubMed] [Google Scholar]
- Petry NM, Tedford J, Martin B. Reinforcing compliance with non-drug-related activities. Journal of Substance Abuse Treatment. 2001;20:33–44. doi: 10.1016/S0740-5472(00)00143-4. [DOI] [PubMed] [Google Scholar]
- Poling J, Kosten TR, Sofuoglu M. Treatment outcome predictors for cocaine dependence. The American Journal of Drug and Alcohol Abuse. 2007;33:191–206. doi: 10.1080/00952990701199416. [DOI] [PubMed] [Google Scholar]
- Reynolds B. The Experiential Discounting Task is sensitive to cigarette-smoking status and correlates with a measure of delay discounting. Behavioural Pharmacology. 2006;17:133–142. doi: 10.1097/01.fbp.0000190684.77360.c0. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Penfold R, Patak M. Dimensions of impulsive behavior in adolescents: Laboratory behavioral assessments. Experimental and Clinical Psychopharmacology. 2008;16:124–131. doi: 10.1037/1064-1297.16.2.124. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Richards JB, de Wit H. Acute-alcohol effects on the Experiential Discounting Task (EDT) and a question-based measure of delay discounting. Pharmacology, Biochemistry and Behavior. 2006;83:194–202. doi: 10.1016/j.pbb.2006.01.007. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Schiffbauer R. Measuring state changes in human delay discounting: An experiential discounting task. Behavioural Processes. 2004;67:343–356. doi: 10.1016/j.beproc.2004.06.003. [DOI] [PubMed] [Google Scholar]
- Sheffer C, MacKillop J, McGeary J, Landes R, Carter L, Yi R, Bickel W, et al. Delay discounting, locus of control, and cognitive impulsiveness independently predict tobacco dependence treatment outcomes in a highly dependent, lower socioeconomic group of smokers. The American Journal on Addictions. 2012;21:221–232. doi: 10.1111/j.1521-0391.2012.00224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. Clifton, NJ: Humana Press; 1992. pp. 41–72. [DOI] [Google Scholar]
- Stanger C, Ryan SR, Fu H, Landes RD, Jones BA, Bickel WK, Budney AJ. Delay discounting predicts adolescent substance abuse treatment outcome. Experimental and Clinical Psychopharmacology. 2012;20:205–212. doi: 10.1037/a0026543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg KL, Roffman RA, Carroll KM, McRee B, Babor TF, Miller M. Brief counseling for marijuana dependence: A manual for treating adults DHHS publication No (SMA) 05–4022. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2005. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2010 national survey on drug use and health: Summary of national findings, NSDUH Series H-41, HHS publication No (SMA) 11–4658. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011. [Google Scholar]
- Sweitzer MM, Donny EC, Dierker LC, Flory JD, Manuck SB. Delay discounting and smoking: Association with the Fagerström Test for nicotine dependence but not cigarettes per day. Nicotine & Tobacco Research. 2008;10:1571–1575. doi: 10.1080/14622200802323274. [DOI] [PubMed] [Google Scholar]
- Takahashi T, Furukawa A, Miyakawa T, Maesato H, Higuchi S. Two-month stability of hyperbolic discount rates for delayed monetary gains in abstinent inpatient alcoholics. Neuro Endocrinology Letters. 2007;28:131–136. [PubMed] [Google Scholar]
- Toneatto A, Sobell LC, Sobell MB, Kozlowski LT. Effect of cigarette smoking on alcohol treatment outcome. Journal of Substance Abuse. 1995;7:245–252. doi: 10.1016/0899-3289(95)90008-X. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Roth DL, Vignolo MJ, Westfall AO. A behavioral economic reward index predicts drinking resolutions: Moderation revisited and compared with other outcomes. Journal of Consulting and Clinical Psychology. 2009;77:219–228. doi: 10.1037/a0014968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JA, Vuchinich RE, Black BC, Rippens PD. Significance of a behavioral economic index of reward value in predicting drinking problem resolution. Journal of Consulting and Clinical Psychology. 2006;74:317–326. doi: 10.1037/0022-006X.74.2.317. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Vuchinich RE, Rippens PD. Predicting natural resolution of alcohol-related problems: A prospective behavioral economic analysis. Experimental and Clinical Psychopharmacology. 2002;10:248–257. doi: 10.1037//1064-1297.10.3.248. [DOI] [PubMed] [Google Scholar]
- Washio Y, Higgins ST, Heil SH, McKerchar TL, Badger GJ, Skelly JM, Dantona RL. Delay discounting is associated with treatment response among cocaine-dependent outpatients. Experimental and Clinical Psychopharmacology. 2011;19:243–248. doi: 10.1037/a0023617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi R, Johnson MW, Giordano LA, Landes RD, Badger GJ, Bickel WK. The effects of reduced cigarette smoking on discounting future rewards: An initial evaluation. The Psychological Record. 2008;58:163–174. doi: 10.1007/bf03395609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon JH, Higgins ST, Heil SH, Sugarbaker RJ, Thomas CS, Badger GJ. Delay discounting predicts postpartum relapse to cigarette smoking among pregnant women. Experimental and Clinical Psychopharmacology. 2007;15:176–186. doi: 10.1037/1064-1297.15.2.186. [DOI] [PubMed] [Google Scholar]


