Abstract
This randomized study examined the efficacy of motivational interviewing (MI) to reduce substance use among adults with depression in outpatient psychiatry. The sample consisted of 104 participants ages 18 and over who reported hazardous drinking (three drinks or more per occasion), illegal drug use or misuse of prescription drugs in the prior 30days, and who scored ≥15 on the Beck Depression Inventory–II (BDI-II). Participants were randomized to receive either three sessions of MI or printed literature about alcohol and drug use risks, as an adjunct to usual outpatient depression care, and completed telephone follow-up interviews at 3 and 6months (93 and 99% of the baseline sample, respectively). Among participants reporting any hazardous drinking at baseline (n=73), MI-treated participants were less likely than controls to report hazardous drinking at 3months (60.0 vs. 81.8%, p=.043). MI is a promising intervention to reduce hazardous drinking among depression patients.
Keywords: Depression, Hazardous drinking, Cannabis, Motivational interviewing
1. Introduction
Hazardous drinking, e.g., drinking over recommended limits, may have a significant, negative impact on individuals with depression (Barry et al., 2006; National Institute on Alcohol Abuse and Alcoholism, 2005). Population-based studies have found an association between elevated depression symptoms and heavy drinking (O'Donnell, Wardle, Dantzer, & Steptoe, 2006), and clinical studies have shown relationships between depression and alcohol problems (McDermut, Mattia, & Zimmerman, 2001). Even moderate drinking may be contraindicated for patients in treatment for depression, as it may decrease antidepressant response, reduce treatment adherence and increase side effects (Worthington et al., 1996). Individuals with depression are also at risk for escalation of alcohol problems (Abraham & Fava, 1999). These findings suggest that alcohol use among patients seeking depression treatment is likely to be clinically problematic.
Drug use also complicates treatment for depression patients. In a survey of primary care patients with depression, 26.3% of women and 29.4% of men reported drug use, including misuse of prescription drugs and illicit drug use (Roeloffs, Fink, Unutzer, Tang, & Wells, 2001). Drug and alcohol use co-occur frequently, and polysubstance use is associated with higher rates of psychiatric disorders and greater depression severity (Brunette, Noordsy, Xie, & Drake, 2003). The use of cannabis can interfere with treatment of depression (Bricker et al., 2007) perhaps by decreasing adherence to behavioral interventions or other aspects of care.
In spite of high prevalence and associated risks, little is known about how to address alcohol and drug use among patients with depression. One approach that could improve outcomes is motivational interviewing (MI). MI has been applied to a variety of behavioral health problems, but most extensively tested in reducing alcohol use (Vasilaki, Hosier, & Cox, 2006). MI is a short-term, directive, patient-centered style of counseling to help explore and resolve ambivalence. Active components include empathic listening, and increasing self-efficacy and the perceived discrepancy between actual and ideal behavior (Rollnick & Miller, 1995). The therapist's approach is one of non-judgmental guidance, helping the patient move to a higher degree of readiness to change and verbalize intent to change.
MI has been identified as potentially useful for patients with co-occurring substance use and psychiatric problems, although prior research has been limited (Saitz, Svikis, D'Onofrio, Kraemer, & Perl, 2006). It has been hypothesized that depressed or anxious patients may be more receptive to MI than others (Wells-Parker, Dill, Williams, & Stoduto, 2006), on the assumption that psychological distress can increase motivation. A German study examined reduction in problematic drinking among patients with either comorbid anxiety or depression, and did not find an impact of four-session telephone-administered MI after 12months. This sample included severe, dependent drinkers, which may help explain the lack of findings (Grothues et al., 2008) because individuals with alcohol dependence may require more extensive treatment (Saitz et al., 2006). Aside from this study, MI comorbidity research has focused primarily on patients with schizophrenia or on general psychiatric inpatients (Baker et al., 2002; Martino, Carroll, Nich, & Rounsaville, 2006; Swanson, Pantalon, & Cohen, 1999), and has not examined the broader population of depressed outpatients who might benefit from this treatment.
In this study we aimed to examine the efficacy of MI as a supplement to usual outpatient care for depression patients. We hypothesized that the intervention would reduce hazardous drinking and potentially reduce drug use and depression. Hazardous drinking was identified as the primary outcome of interest because alcohol is the most commonly used substance in this population (Davis et al., 2005; Satre, Wolfe, Eisendrath &Weisner, 2008). We anticipated that depression outcomes potentially could be improved in the MI intervention group if substance use reduction leads to improved depression treatment effectiveness (e.g., antidepressant medication provided as part of usual care); and therefore examined treatment group differences in depression symptoms at follow-up. We also examined hazardous drinking reduction as a potential mediator of depression symptom reduction.
In addition to testing the impact of MI, we examined predictors of hazardous drinking at 6months, including depression severity, baseline hazardous drinking frequency, and demographic factors (e.g., older age) based on prior studies of motivation among adults with depression (Satre, Chi, et al., 2011; Wells-Parker et al., 2006). We anticipated that results would provide initial evidence for the impact of MI, including estimates of effect sizes, and contribute to the development of larger controlled trials of MI in this important clinical population.
2. Materials and methods
2.1. Participants
Study participants were adults 18 and over seeking outpatient services in the Langley Porter Hospital and Clinics (LPPHC), at the University of California, San Francisco (UCSF) Medical Center. Patients are mainly referred by their insurance carrier, self-referred, or referred by providers in the community. The study was conducted in the Adult Psychiatry Clinic (APC) and Partial Hospitalization Program (PHP), which are two programs of the LPPHC. The APC provides evaluation, psychotherapy and medication management for patients with a range of mental health problems. The PHP is a more intensive outpatient service in which patients typically attend individual and group treatment for 5hours each day for 10 consecutive weekdays, followed by tapering of services; and serves a more acute population than the APC. In both clinics, patients receive treatment from psychiatry residents, faculty, and clinical staff.
The LPPHC does not offer specialized services for patients whose primary presenting issue is substance dependence. Individuals are screened by telephone prior to intake, and those seeking intensive chemical dependency treatment or who report serious alcohol or drug problems are referred to treatment programs in the community (Satre et al., 2008). However, prior studies have identified substantial prevalence of heavy episodic drinking and drug use among patients in this clinic (Satre, Chi, et al., 2011; Satre, Sterling, Mackin, & Weisner, 2011).
Study inclusion criteria were based on hazardous drinking (i.e., three drinks or more in a day for both men and women) or drug use (including any illicit drug use and non-prescribed use of prescription drugs in the prior 30days) and moderate or greater symptoms of depression [≥15 on the Beck Depression Inventory II (BDI-II)] at clinic intake (Steer, Brown, Beck, & Sanderson, 2001). We chose a hazardous drinking standard slightly more conservative than that recommended for the general population (National Institute on Alcohol Abuse and Alcoholism, 2005) because patients in this treatment population are frequently taking antidepressant medication that can have adverse interactions with alcohol (e.g., reduced medication efficacy (Worthington et al., 1996) or increase the risk of side effects and toxicity (Koski, Vuori, & Ojanpera, 2005; Silverstone, Williams, McMahon, Fleming, & Fogarty, 2008). Patients with current mania or psychosis were excluded; as such patients would likely require more intensive services than those typically provided as part of outpatient depression care, and inclusion could introduce too much heterogeneity for research at this stage.
2.2. Usual depression care
All study participants received usual depression care based on current best practices for medication management and empirically supported forms of individual and group psychotherapy. Treatment decisions were made collaboratively by clinicians and patients. Selective serotonin reuptake inhibitors (SSRIs) were usually the medication of first choice in the clinic based on standards of care for depression.
2.3. Measures
Demographic information for participants was obtained from medical records, including results of a computerized assessment battery (Satre et al., 2008). Alcohol and drug questions included substance type (cannabis, cocaine, amphetamine-type stimulants, hallucinogens, inhalants, sedatives other than as prescribed, opioids other than as prescribed, heroin or methadone, alcohol, tobacco and other). For each substance, participants were asked the number of days of use in the past 30days.
Alcohol questions include usual drinking frequency (days per month), typical number of standard drinks consumed, and frequency of hazardous drinking (three drinks or more) in the past 30days (Sobell & Sobell, 2003). The alcohol readiness ruler and cannabis readiness ruler are 10-point scales developed in prior MI studies to measure readiness to change. The scales ask how ready respondents are to cut down or stop use, ranging from 1 (not ready) to 10 (very ready) (Heather, Smailes, & Cassidy, 2008).
The Beck Depression Inventory-II (BDI-II) is a valid 21-item depression scale. A score of ≥15 is indicative of moderate or greater depression symptoms (Steer et al., 2001).
Components of usual care were measured for use as covariates. Data on usual care patients received apart from the study were drawn from computerized administrative records at baseline and self-report at 6months (individual and group psychotherapy attendance, antidepressant medication utilization, total number of mental health care visits, whether advice was given to cut back on alcohol or drug use, and utilization of specialty alcohol or drug treatment services).
2.4. Procedures
Study procedures were approved by the UCSF Committee on Human Subjects. Participants were identified via provider referrals, self-referral in response to flyers in clinic waiting area, and a research registry of LPPHC patients who have given permission to be contacted for future studies (Satre et al., 2008). The research assistant determined eligibility based on alcohol and drug use patterns and depression score reported at clinical intake, recruited patients by telephone, and completed enrollment procedures in person. Participants were offered $50 for the baseline interview, $50 for the 3-month interview, and $100 for the 6-month interview.
Study baseline measurement of demographic characteristics, alcohol and drug use, alcohol-related problems and depression utilized computerized clinic intake data (90% of participants) or paper-and-pencil measures (10%). Clinic baseline alcohol and drug use assessment was chosen for the study because it included all alcohol and drug questions required. This approach helped to minimize assessment reactivity, which has been hypothesized to have an intervention effect in brief intervention studies (Jenkins, McAlaney, & McCambridge, 2009). Self-administered computerized assessment of alcohol and drug use may increase patient comfort and self-report validity compared with face-to-face interviews (Paperny, Aono, Lehman, Hammar, & Risser, 1990). Participants were enrolled in the study an average of 24.6days (SD=16.0) after clinic intake, with a median of 22days.
After complete description of the study, written informed consent was obtained. Patients who met study criteria and gave informed consent completed additional baseline measures in paper and pencil format, including the readiness rulers and were randomized to one of the two study arms. Standard randomization procedures used in psychotherapy studies were followed (Hulley et al., 2001). Blocked randomization was employed using a block size of 4, with a 1:1 allocation into either the treatment or control condition. Participants were stratified by gender and by source clinic (APC or PHP). A research assistant who had no other involvement with the study used a Web-based randomization tool to generate group assignments and placed individual assignments into sealed security envelopes given to the study therapist, who was directed to open the envelopes in sequence as participants were enrolled.
The intervention consisted of one 45-minute in-person MI session followed by two 15-minute telephone “booster” sessions, similar to the format successful in prior MI alcohol studies (Fleming et al., 2010). The treatment guidelines were based on the widely used Motivational Interviewing text by Miller and Rollnick (2002).Within a standardized protocol, the MI model allows for flexibility in tailoring the intervention to individual patients based on readiness to change. The therapist encouraged patients to minimize use of alcohol, illegal drugs, and misuse of prescription drugs, depending on which were reported by each participant at baseline. The intervention incorporated information about substance use risks for people in depression treatment (e.g., alcohol/medication interactions and the potential for alcohol and drug use to interfere with depression treatment), provided in a respectful way consistent with MI-recommended feedback style. Intervention sessions were delivered within 6weeks of enrollment.
In a brief meeting (<5minutes) the study therapist gave control group participants two-page brochures on substance use and risks specific to the substances they reported, consistent with prior MI studies (Bernstein et al., 2005; Dunn, Deroo, & Rivara, 2001). These brochures produced by the NIH and the National Office of National Drug Control Policy Fast Facts series reference published information by the National Institutes of Health regarding drug use risks and adverse alcohol interactions with medications (National Institute on Alcohol Abuse and Alcoholism, 2007; U.S. Department of Justice, 2003). Brochures were selected as the control condition in order to give patients some access to information regarding substance use, but not an experience of the specific MI treatment (e.g., resolving ambivalence about change, empathic listening, increasing self-efficacy) hypothesized to comprise the active components of MI. All control participants received at least one brochure. We considered using a more active control condition. However, because all participants had access to treatment as usual for depression including outpatient psychotherapy and medication management visits, this was not considered necessary.
The therapist delivering the intervention was a licensed marriage and family therapist (MFT) on the clinic staff but not involved in usual patient care. The therapist participated in approximately 15hours of instruction, and received supervised practice of three training patients in MI and study procedures, consistent with the average number of hours provided in past clinical trials (Dunn et al., 2001). Components included reading about the MI model, study of the manuals, practice role-plays with feedback, and reviews of videotaped practice sessions conducted with training patients. Learning goals included developing familiarity with MI theory, practicing basic patient-centered counseling skills, recognizing and reinforcing change talk, and helping develop behavior change plans (Miller & Moyers, 2006).
Monitoring fidelity to the MI model was conducted using the Motivational Interviewing Treatment Integrity (MITI) code (Pierson et al., 2007) and taped therapist training sessions as well as actual sessions with participants. This training model has been effective in obtaining a high degree of fidelity (Madson & Campbell, 2006). The PI and the trainers were available for follow-up review of MI methods and additional coaching, which has been associated with better development of skills. After training was completed, a random subsample of 17 MI sessions were coded by an expert consultant outside the study team. Mean MITI scores were obtained for empathy [5.4 (SD=.09)], MI spirit [5.5 (SD=0.5)], reflection to question ratio [1.7 (SD=2.2)], percent open-ended questions [65.3 (SD=26.9)], percent complex reflections [62.8 (SD=12.7)], and percent MI adherent [92.4 (SD=15.6)]. Descriptively, these scores fall in the range between the MITI categories of proficiency and competence, and are indicative of a high degree of fidelity to MI; and 98% of intervention group participants received all three sessions.
The research assistant contacted participants by telephone 3 and 6months after enrollment for a 20-minute interview to administer follow-up measures. Patient reporting via telephone follow-up has been reliable in substance use studies (B. B. Cohen & Vinson, 1995).The 6-month interview included questions about usual care and alcohol and drug specialty care services. The research assistant was blinded to participants' treatment condition.
2.5. Analyses
As a check on the randomization process, initial analyses examined comparability of the intervention and control groups on demographic characteristics (age, gender, ethnic composition and marital status), depression symptoms (BDI-II), and baseline substance use and readiness to change alcohol and cannabis use, using t-tests and Pearson's chi-square test. We also compared the two groups on measures of usual care services received (e.g., type of outpatient services, number of clinic visits, and any alcohol or drug treatment received apart from the study).
Group differences and effect sizes were calculated on measures of hazardous drinking, cannabis use and depression (Cohen, 1988). We used t-tests and Pearson's chi-square test to examine group differences in outcomes. In an exploratory step, treatment group differences in change between baseline, 3 and 6months were examined using mixed effects linear models for the BDI-II and nonlinear mixed-effects models for the binary measures of any three or more drinking days and any cannabis use. Models included terms for treatment condition, assessment point and interaction terms between condition and time.
Among patients who reported hazardous drinking at baseline (n=73), we examined differences between intervention and control groups on measures of hazardous drinking, and usual drinking quantity and frequency at 3 and 6months. We tested a model of mediational effects to see if the assignment to treatment condition led to a change in hazardous drinking at the 3-month assessment which, in turn, would lead to a change in BDI scores at the 6-month assessment.
Multivariate logistic regression was used to examine predictors of hazardous drinking in the entire sample at 6months, including factors based on the literature associated with better alcohol outcomes: older age, female gender, greater baseline depression (Grothues et al., 2005; Satre, Chi, et al., 2011; Wells-Parker et al., 2006); with greater baseline hazardous drinking frequency, study condition, baseline cannabis use, and substance abuse treatment (any treatment outside the study reported at the time of the six month follow-up) included as control variables. All predictors were entered at the same time. Statistical analyses were conducted using SAS v9.2 and SPSS.
3. Results
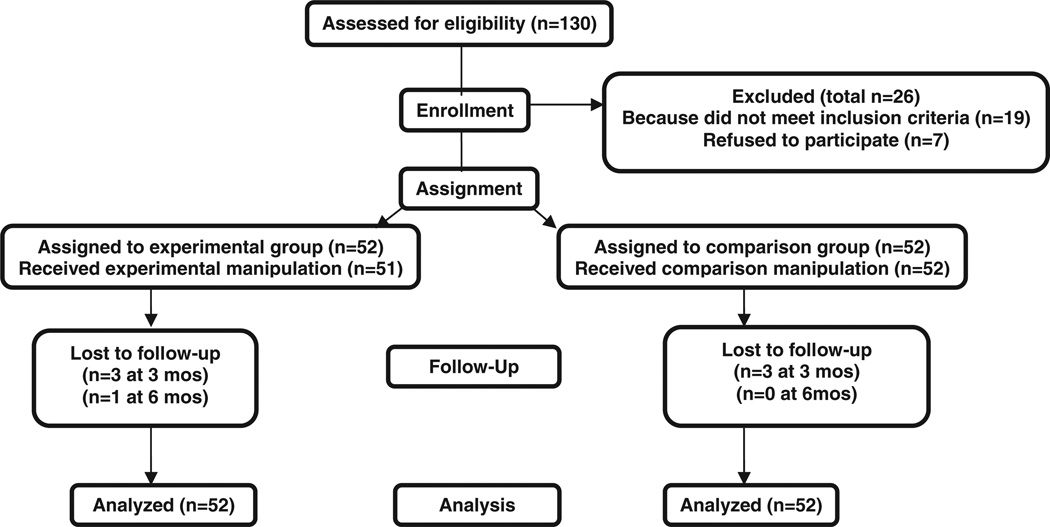
During the 18-month study intake window, 209 patients who we anticipated to be eligible based on clinical intake were approached regarding the study (including telephone calls to patients in the research registry and follow-ups to referrals by clinicians). Of these, 130 expressed interest in participating and completed a telephone screening for psychosis and mania; and 19 were excluded. There were 111 patients who agreed to participate, of which 7 later could not be contacted or explicitly withdrew. Of the 104 enrolled participants, 98 (93%) completed the 3-month telephone follow up and 103 (99%) completed the 6-month follow up (Fig. 1).
Fig. 1.
Flow of participants (motivational interviewing and control groups). Note. This flowchart is an adaptation of the flowchart offered by the CONSORT Group. Experimental group participants received three sessions of motivational interviewing. Comparison group participants received a brochure on alcohol and drug use risks.
The sample ranged in age from 19 to 69, with a mean age of 42.4 (SD=13.7) and was 64.4% female. Mean BDI-II score was 24.7 (SD=10.4), a level consistent with a diagnosis of major depressive disorder (Steer et al., 2001). Table 1 displays demographic characteristics, baseline depression symptoms, and alcohol and drug use prevalence in the study groups. Hazardous drinking (any three or more drinks on at least one occasion) and cannabis were most frequently reported. The control group was significantly more likely to report cannabis use in the 30days prior to intake, χ2 (N=104)=4.7, 1 df, p=.025. However, among cannabis users (n=30), MI group participants scored higher than control group participants on the 10-point readiness to change scale, mean=6.5 (SD=3.0) in the MI group vs. 3.9 (SD=3.4) in the control group (not shown). Other substances included cocaine (5%), amphetamines (3%), hallucinogens/ MDMA (3%), sedative misuse (11%) and opioid misuse (1%), not shown. There were no differences between groups in type or number of usual care psychiatry clinic visits between intake and 6month follow up (Table 1).
Table 1.
Adults with depression recruited to motivational interviewing (MI) study to reduce hazardous drinking and drug use: intervention and control group characteristics (N=104).
| MI intervention |
Control |
χ2 | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Total study group | 52 | 52 | |||
| Gender (% female) | 32 | 61.5 | 35 | 67.3 | 0.4 |
| Hispanic | 4 | 7.7 | 3 | 5.8 | 0.2 |
| Race/Ethnicity | 5.2 | ||||
| White | 44 | 84.8 | 42 | 80.6 | |
| Black | 4 | 7.7 | 2 | 3.8 | |
| Asian American | 0 | 0.0 | 2 | 3.0 | |
| Mixed/other | 4 | 7.7 | 6 | 11.5 | |
| Marital status | 0.4 | ||||
| Married | 7 | 13.5 | 6 | 11.5 | |
| Separated or divorced | 12 | 23.1 | 10 | 19.2 | |
| Never married | 33 | 63.5 | 36 | 69.2 | |
| Highest educational degree | 4.1 | ||||
| High school/GED | 8 | 15.4 | 6 | 11.5 | |
| Some college/AA | 10 | 19.2 | 5 | 9.6 | |
| BA/BS | 28 | 53.8 | 19 | 36.5 | |
| MA/MS or higher | 15 | 28.8 | 13 | 25.0 | |
| Baseline alcohol and drug use | |||||
| Any alcohol use | 42 | 80.8 | 42 | 80.8 | 0.0 |
| Any 3+ drinking days | 37 | 72.5 | 36 | 69.2 | 0.1 |
| Any cannabis use | 10 | 19.2 | 20 | 38.5 | 4.7.* |
| Any other drug use | 10 | 19.2 | 14 | 26.8 | 0.6 |
| Usual care service type | |||||
| Partial hospitalization program | 22 | 42.3 | 23 | 44.2 | 0.1 |
| Medication management | 43 | 87.8 | 38 | 79.2 | 1.3 |
| Individual psychotherapy | 45 | 91.8 | 40 | 83.3 | 1.6 |
| Group psychotherapy | 16 | 32.6 | 14 | 29.2 | 0.1 |
| Usual care provider encouraged | 16 | 32.7 | 13 | 27.1 | 0.4 |
| alcohol or drug use reduction | |||||
| Received alcohol or drug treatment | 5 | 10.2 | 5 | 10.4 | 0.1 |
| Mean | SD | Mean | SD | t (df) | |
| Age | 44.3 | 14.0 | 40.6 | 13.3 | 1.4 (102) |
| Motivation to reduce drinking | 5.9 | 3.5 | 4.9 | 3.1 | 1.4 (96) |
| Total usual care visits | 10.5 | 13.8 | 7.8 | 11.2 | 0.3 (96) |
Notes: Baseline questions refer to alcohol and drug consumption in the previous 30days. Significance of group differences was tested using chi-square and t-tests. Usual care services were measured retrospectively at the 6-month follow up interview.
p<.05.
Outcomes in the entire sample (N=104) are shown on Table 2. Effect sizes were calculated for observed differences at 3 and 6months. Results of exploratory analysis using mixed effects models of reported three or more drinking, cannabis use and BDI-II score at each measurement point found no significant effect for treatment group or time of measurement (not shown).
Table 2.
Motivational interviewing (MI) versus control group outcomes among adults in treatment with depression who report hazardous drinking or drug use (N=104).
| MI intervention |
Control |
χ2 | Effect size h |
|||
|---|---|---|---|---|---|---|
| N | % | n | % | |||
| Total study group | 52 | 52 | ||||
| Any 3+ drinking days | ||||||
| Baseline | 37 | 72.6 | 36 | 69.2 | 0.1 | - |
| 3months | 24 | 49.0 | 31 | 63.3 | 2.0 | .29 |
| 6months | 24 | 47.1 | 30 | 57.7 | 1.2 | .21 |
| Any cannabis use | ||||||
| Baseline | 10 | 19.2 | 20 | 38.5 | 4.7.* | - |
| 3months | 8 | 16.3 | 21 | 42.9 | 8.3.* | .61 |
| 6months | 11 | 21.6 | 19 | 36.5 | 2.8 | .23 |
| Mean | SD | Mean | SD | t (df) | Effect size d |
|
| BDI-II Depression score | ||||||
| Baseline | 24.8 | 9.6 | 24.6 | 11.3 | 0.1 (102) | - |
| 3months | 20.3 | 12.0 | 20.8 | 11.8 | 0.2 (96) | .04 |
| 6months | 17.4 | 11.4 | 18.3 | 12.4 | 0.4 (101) | .08 |
Notes: Baseline, 3- and 6-month questions refer to alcohol and drug consumption in the previous 30days. Significance of intervention and control group differences was tested using chi-square and t-tests. We report Cohen's (1988) h for proportions and d for means.
p<.05.
Among those who reported any three or more drinking days at baseline (n=73), we examined treatment group differences. MI and control groups were similar in age, sex, baseline depression score and readiness to change alcohol use (not shown); and 10.8% of MI participants and 27.8% of control participants in this sub-sample reported cannabis use at baseline (not significant). At 3months, MI participants were significantly less likely than controls to report any hazardous drinking in the prior 30days (60.0% vs. 81.8%, n=73, 1 df, χ2=3.9, p=.043). Both groups trended lower at 6months, and group differences narrowed (to 58.3% in the MI group and 72.2% in the control group) and this difference was not significant (Table 3).
Table 3.
Changes in alcohol use patterns between baseline and 6months among motivational interviewing (MI) versus control group participants who reported any hazardous drinking at baseline (n=73).
| MI intervention | Control | χ2 | Effect size h |
|||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Total study group | 37 | 36 | ||||
| Any 3+ drinking days | ||||||
| Baseline | 37 | 100.0 | 36 | 100.0 | 0.0 | - |
| 3months | 21 | 60.0 | 27 | 81.8 | 3.9.* | .47 |
| 6months | 21 | 58.3 | 26 | 72.2 | 1.5 | .47 |
| Mean | SD | Mean | SD | t (df) | Effect size d |
|
| Usual drinking quantity | ||||||
| Baseline | 2.7 | 1.5 | 2.7 | 1.0 | 0.1 (71) | - |
| 3months | 2.3 | .9 | 2.2 | 1.3 | 0.5 (67) | .09 |
| 6months | 1.8 | 1.2 | 2.2 | 1.3 | 1.4 (71) | .32 |
| Usual drinking frequency | ||||||
| Baseline | 12.9 | 8.3 | 12.2 | 7.8 | 0.4 (72) | .09 |
| 3months | 9.3 | 8.0 | 8.5 | 6.8 | 0.4 (67) | .11 |
| 6months | 9.5 | 8.1 | 10.0 | 9.0 | 0.3 (71) | .06 |
Notes: All participants in this sub-sample reported hazardous drinking at baseline. Baseline, 3- and 6- month questions refer to alcohol consumption in the previous 30days. Significance of intervention and control group differences was tested using chi-square and t-tests. We report Cohen's (1988) h for proportions and d for means.
p<.05.
In the mediation model to see if the assignment to treatment condition led to a change in hazardous drinking at the 3-month assessment which, in turn, would lead to a change in BDI scores at the 6-month assessment, no significant effects were found (not shown).
Using logistic regression we tested candidate predictors of participants' reporting any three or more drinking days at 6months, including older age, female gender, greater baseline depression; with greater baseline hazardous drinking frequency, study condition, baseline cannabis use, and substance abuse treatment (any treatment outside the study reported at the time of the 6month follow-up) included as control variables (n=97). Factors approaching significance included higher BDI-II score (p=.065), not reporting any cannabis use at baseline (p=.056), and lower frequency of three or more drinking at baseline (p=.062); Cox and Snell pseudo-R2=.18, p=.007 (not shown).
4. Discussion
This study examined the efficacy of a three-session MI intervention to reduce hazardous drinking and drug use among patients with depression, because of the potential for adverse effects of substance use in this population. Results found that at 3months, MI had a significant impact on the primary outcome of interest, reduction in hazardous drinking; although no impact was found on cannabis use or depression symptoms. These findings have implications for the development of appropriate alcohol interventions, which are integral to the delivery of effective psychiatric services, in which patients frequently present with alcohol and drug use in addition to major depression (Satre, Chi, et al., 2011).
Results contribute to the limited literature on MI in psychiatric populations. A study by Baker et al. (2002) of inpatients with substance abuse or dependence randomized participants to a single motivational interview or a self-help booklet. There was a modest short-term effect on alcohol and other drug use, but cannabis use remained high at 12months. A pilot study of inpatients with depression and cocaine dependence found that MI patients had better abstinence rates, mood status, adherence to post-discharge treatment plan, and lower re-hospitalization rates in the year following treatment (Daley, Salloum, Zuckoff, Kirisci, & Thase, 1998).Martino et al. (2006) compared two sessions of an MI procedure adapted for dual diagnosis to two sessions of a control condition psychiatric interview in patients with psychosis and drug use disorders. Results found no difference between the two conditions on substance use. In contrast to this prior work, our study focused on a larger and less acute population of depressed outpatients with hazardous drinking, including severity levels that may be more responsive to brief interventions. Our study findings contribute to the knowledge base for this important treatment model.
Understanding motivational factors is an important aspect of intervention development, especially given the motivation-focused approach of the model (Miller & Rollnick, 2002). Based on prior studies (Blume, Schmaling, & Marlat, 2001; Wells-Parker et al., 2006), it was anticipated that depression severity might be associated with a lower proportion of hazardous drinking in the sample at follow up. In the current study this relationship approached significance. If the relationship is found to be significant in future studies, this could indicate that patients presenting with more severe depression may indeed be amenable to reducing drinking over time.
Although treatments for alcohol problems are most successful at early stages, most people do not seek treatment until their condition is severe. Instead, many individuals with alcohol problems first seek psychiatric treatment (Weisner & Schmidt, 1992). In mental health service settings (including psychiatry and primary care clinics), however, providers often fail to recognize warning signs about problematic substance use that present opportunities for intervention. As a result, potential problems can go unrecognized and untreated. Screening, Brief Intervention and Referral to Treatment (SBIRT), which frequently incorporates MI, has been widely promoted as a public health approach to reducing hazardous drinking in medical and mental health settings (Babor et al., 2007). Our findings suggest that patients in depression treatment may be willing to participate in supplemental services focused on alcohol use reduction and that brief MI can help these patients reduce hazardous drinking.
4.1. Study limitations and strengths
Designed as an initial investigation of MI treatment efficacy in a new population, this study had a relatively small sample size and short-term follow up period, relied on self-report of substance use rather than biochemical verification, and included a heterogeneous sample of participants who used both alcohol and drugs. All intervention sessions were delivered by a single therapist, such that it is not possible to disentangle intervention effects from therapist effects.
The clinic pre-screened and excluded most patients with serious alcohol or drug problems, and the intervention was not designed to address dependence. We used computerized clinic alcohol and drug use measures to identify patients for recruitment. While such methods have been validated (Paperny et al., 1990), it is possible that some patients could have under-reported their use and thus would not have been identified. Therefore, the pool of patients identified for recruitment may not be representative of all patients with hazardous drinking or drug use in the clinic. In addition, 38% of potentially eligible patients declined to complete study screening procedures, and conclusions cannot be drawn regarding the potential MI treatment impact on these patients who may have been less inclined to discuss or change alcohol and drug use than study enrollees.
Patients in specialty psychiatric settings may have more severe depression problems than those in other contexts such as primary care. However, limiting the sample to patients scoring 15+ on the BDI-II in an outpatient setting helps make findings generalizable to the large majority of treatment-seeking depressed adults. Although there were more cannabis users in the control condition, which may have impacted group comparisons, the relevance of this imbalance is unclear as MI appeared to have no impact on reducing cannabis use. While the intervention targeted both alcohol and cannabis use, it is possible that cannabis users were more dependent than alcohol users in our sample. In addition, individuals with depression who use cannabis use could require a greater number of MI sessions or other treatment adaptations in order to benefit.
The study also had a number of strengths. This was a well-controlled study with very high follow-up rates, the study was conducted in an outpatient depression treatment context, and the intervention was monitored for MI fidelity. We controlled for the type of clinic in which participants received usual care services in our randomization, and measured other components of care. Assessment for alcohol and drug use and the treatment intervention resulted in no logistical complications or conflicts with usual care, suggesting that such a supplemental intervention may be integrated into outpatient settings. Results provide support for the use of MI to reduce hazardous drinking among patients in treatment for depression, including estimates of effect size that should be examined in larger clinical trials.
4.2. Conclusion
This study examined the efficacy of MI among depression patients as an adjunct to usual care in an outpatient psychiatry clinic setting. Results provide initial evidence for a positive impact on reduction in hazardous drinking based on short-term follow-up measures. Further research should be conducted in a larger sample with longer follow-up, and may benefit from stratification based on cannabis use. Examination of outcomes in primary care settings, in which many depression patients receive services, would also be a promising next step in the study of this treatment model.
Acknowledgments
This study was supported by grants from the Steven L. Merrill Family Foundation, the National Institute on Alcohol Abuse and Alcoholism (K23 AA015411, R01 AA020463, and RO1 AA016204) and the National Institute on Drug Abuse (P50 DA09253). We thank Maura McLane, M.F.T., and Sarah Olson, B.A., with assistance in conducting the study, Cynthia Chappell, B.A., for assistance in managing computerized clinic data, and Agatha Hinman, B.A., for assistance in preparing the manuscript.
References
- Abraham HD, Fava M. Order of onset of substance abuse and depression in a sample of depressed outpatients. Comprehensive Psychiatry. 1999;40:44–50. doi: 10.1016/s0010-440x(99)90076-7. [DOI] [PubMed] [Google Scholar]
- Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT): Toward a public health approach to the management of substance abuse. Substance Abuse. 2007;28:7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- Baker A, Lewin T, Reichler H, Clancy R, Carr V, Garrett R, et al. Evaluation of a motivational interview for substance use within psychiatric in-patient services. Addiction. 2002;97:1329–1337. doi: 10.1046/j.1360-0443.2002.00178.x. [DOI] [PubMed] [Google Scholar]
- Barry KL, Milner K, Blow FC, Impens A, Welsh D, Amash J. Screening psychiatric emergency department patients with major mental illnesses for at-risk drinking. Psychiatric Services. 2006;57:1039–1042. doi: 10.1176/ps.2006.57.7.1039. [DOI] [PubMed] [Google Scholar]
- Bernstein J, Bernstein E, Tassiopoulos K, Heeren T, Levenson S, Hingson R. Brief motivational intervention at a clinic visit reduces cocaine and heroin use. Drug and Alcohol Dependence. 2005;77:49–59. doi: 10.1016/j.drugalcdep.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Blume AW, Schmaling KB, Marlat GA. Motivating drinking behavior change depressive symptoms may not be noxious. Addictive Behaviors. 2001;26:267–272. doi: 10.1016/s0306-4603(00)00087-3. [DOI] [PubMed] [Google Scholar]
- Bricker JB, Russo J, Stein MB, Sherbourne C, Craske M, Schraufnagel TJ, et al. Does occasional cannabis use impact anxiety and depression treatment outcomes?: Results from a randomized effectiveness trial. Depression and Anxiety. 2007;24:392–398. doi: 10.1002/da.20248. [DOI] [PubMed] [Google Scholar]
- Brunette MF, Noordsy DL, Xie H, Drake RE. Benzodiazepine use and abuse among patients with severe mental illness and co-occurring substance use disorders. Psychiatric Services. 2003;54:1395–1401. doi: 10.1176/appi.ps.54.10.1395. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: LErlbaum Associates; 1988. [Google Scholar]
- Cohen BB, Vinson DC. Retrospective self-report of alcohol consumption: Test-retest reliability by telephone. Alcoholism, Clinical and Experimental Research. 1995;19:1156–1161. doi: 10.1111/j.1530-0277.1995.tb01595.x. [DOI] [PubMed] [Google Scholar]
- Daley DC, Salloum IM, Zuckoff A, Kirisci L, Thase ME. Increasing treatment adherence among outpatients with depression and cocaine dependence: Results of a pilot study. American Journal of Psychiatry. 1998;155:1611–1613. doi: 10.1176/ajp.155.11.1611. [DOI] [PubMed] [Google Scholar]
- Davis LL, Rush JA, Wisniewski SR, Rice K, Cassano P, Jewell M, et al. Substance use disorder comorbidity in major depressive disorder: An exploratory analysis of the Sequenced Treatment Alternatives to Relieve Depression cohort. Comprehensive Psychiatry. 2005;46:81–89. doi: 10.1016/j.comppsych.2004.07.025. [DOI] [PubMed] [Google Scholar]
- Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: A systematic review. Addiction. 2001;96:1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- Fleming MF, Balousek SL, Grossberg PM, Mundt MP, Brown D, Wiegel J, et al. Brief physician advice for heavy drinking college students: A randomized controlled trial in college health clinics. Journal of Studies on Alcohol and Drugs. 2010;71:23–31. doi: 10.15288/jsad.2010.71.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grothues JM, Bischof G, Reinhardt S, Hapke U, Meyer C, John U, et al. Intention to change drinking behaviour in general practice patients with problematic drinking and comorbid depression or anxiety. Alcohol and Alcoholism. 2005;40:394–400. doi: 10.1093/alcalc/agh182. [DOI] [PubMed] [Google Scholar]
- Grothues JM, Bischof G, Reinhardt S, Meyer C, John U, Rumpf HJ. Effectiveness of brief alcohol interventions for general practice patients with problematic drinking behavior and comorbid anxiety or depressive disorders. Drug and Alcohol Dependence. 2008;94:214–220. doi: 10.1016/j.drugalcdep.2007.11.015. [DOI] [PubMed] [Google Scholar]
- Heather N, Smailes D, Cassidy P. Development of a readiness ruler for use with alcohol brief interventions. Drug and Alcohol Dependence. 2008;98:235–240. doi: 10.1016/j.drugalcdep.2008.06.005. [DOI] [PubMed] [Google Scholar]
- Hulley SB, Newman TB, Cummings SR, Hearst N, Grady D, Browner WS. Designing clinical research: An epidemiologic approach. 2nd ed. New York: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- Jenkins RJ, McAlaney J, McCambridge J. Change over time in alcohol consumption in control groups in brief intervention studies: Systematic review and meta-regression study. Drug and Alcohol Dependence. 2009;100:107–114. doi: 10.1016/j.drugalcdep.2008.09.016. [DOI] [PubMed] [Google Scholar]
- Koski A, Vuori E, Ojanpera I. Newer antidepressants: Evaluation of fatal toxicity index and interaction with alcohol based on Finnish postmortem data. International Journal of Legal Medicine. 2005;119:344–348. doi: 10.1007/s00414-005-0528-x. [DOI] [PubMed] [Google Scholar]
- Madson MB, Campbell TC. Measures of fidelity in motivational enhancement: A systematic review. Journal of Substance Abuse Treatment. 2006;31:67–73. doi: 10.1016/j.jsat.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Martino S, Carroll KM, Nich C, Rounsaville BJ. A randomized controlled pilot study of motivational interviewing for patients with psychotic and drug use disorders. Addiction. 2006;101:1479–1492. doi: 10.1111/j.1360-0443.2006.01554.x. [DOI] [PubMed] [Google Scholar]
- McDermut W, Mattia J, Zimmerman M. Comorbidity burden and its impact on psychosocial morbidity in depressed outpatients. Journal of Affective Disorders. 2001;65:289–295. doi: 10.1016/s0165-0327(00)00220-2. [DOI] [PubMed] [Google Scholar]
- Miller WR, Moyers TB. Eight stages in learning motivational interviewing. Journal of Teaching in the Addictions. 2006;5:3–18. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York: Guilford Press; 2002. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: A clinician's guide, updated 2005 edition. Rockville, MD: U.S. Department of Health and Human Services; 2005. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Harmful interactions: Mixing alcohol with medicines. Rockville, MD: U.S. Department of Health and Human Services (No. NIH Pub. No. 03-5329); 2007. [Google Scholar]
- O'Donnell K, Wardle J, Dantzer C, Steptoe A. Alcohol consumption and symptoms of depression in young adults from 20 countries. Journal of Studies on Alcohol. 2006;67:837–840. doi: 10.15288/jsa.2006.67.837. [DOI] [PubMed] [Google Scholar]
- Paperny DM, Aono JY, Lehman RM, Hammar SL, Risser J. Computer-assisted detection and intervention in adolescent high-risk health behaviors. Journal of Pediatrics. 1990;116:456–462. doi: 10.1016/s0022-3476(05)82844-6. [DOI] [PubMed] [Google Scholar]
- Pierson HM, Hayes SC, Gifford EV, Roget N, Padilla M, Bissett R, et al. An examination of the Motivational Interviewing Treatment Integrity code. Journal of Substance Abuse Treatment. 2007;32:11–17. doi: 10.1016/j.jsat.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Roeloffs CA, Fink A, Unutzer J, Tang L, Wells KB. Problematic substance use, depressive symptoms, and gender in primary care. Psychiatric Services. 2001;52:1251–1253. doi: 10.1176/appi.ps.52.9.1251. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Miller WR. What is motivational interviewing? Behavioural and Cognitive Psychotherapy. 1995;23:325–334. doi: 10.1017/S1352465809005128. [DOI] [PubMed] [Google Scholar]
- Saitz R, Svikis D, D'Onofrio G, Kraemer KL, Perl H. Challenges applying alcohol brief intervention in diverse practice settings: Populations, outcomes, and costs. Alcoholism, Clinical and Experimental Research. 2006;30:332–338. doi: 10.1111/j.1530-0277.2006.00038.x. [DOI] [PubMed] [Google Scholar]
- Satre DD, Chi FW, Eisendrath S, Weisner C. Subdiagnostic alcohol use by depressed men and women seeking outpatient psychiatric services: Consumption patterns and motivation to reduce drinking. Alcoholism, Clinical and Experimental Research. 2011;35:695–702. doi: 10.1111/j.1530-0277.2010.01387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Sterling S, Mackin RS, Weisner C. Patterns of alcohol and drug use among depressed older adults seeking outpatient psychiatric services. American Journal of Geriatric Psychiatry. 2011;19:695–703. doi: 10.1097/JGP.0b013e3181f17f0a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Wolfe W, Eisendrath S, Weisner C. Computerized screening for alcohol and drug use among adults seeking outpatient psychiatric services. Psychiatric Services. 2008;59:441–444. doi: 10.1176/appi.ps.59.4.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstone PH, Williams R, McMahon L, Fleming R, Fogarty S. Alcohol significantly lowers the seizure threshold in mice when co-administered with bupropion hydrochloride. Annual general psychiatry. 2008;7:11. doi: 10.1186/1744-859X-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol consumption measures. In: Allen JP, Wilson VB, editors. Assessing alcohol problems. A guide for clinicians and researchers. 2nd ed. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. pp. 75–100. [Google Scholar]
- Steer RA, Brown GK, Beck AT, Sanderson WC. Mean Beck Depression Inventory-II scores by severity of major depressive episode. Psychological Reports. 2001;88(3 Pt 2):1075–1076. doi: 10.2466/pr0.2001.88.3c.1075. [DOI] [PubMed] [Google Scholar]
- Swanson AJ, Pantalon MV, Cohen KR. Motivational interviewing and treatment adherence among psychiatric and dually diagnosed patients. The Journal of Nervous and Mental Disease. 1999;187:630–635. doi: 10.1097/00005053-199910000-00007. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Justice. Marijuana fast facts. Johnstown, PA: National Drug Intelligence Center; 2003. [Google Scholar]
- Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: A meta-analytic review. Alcohol and Alcoholism. 2006;41:328–335. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- Weisner C, Schmidt L. Gender disparities in treatment for alcohol problems. JAMA : The Journal of the American Medical Association. 1992;268:1872–1876. [PubMed] [Google Scholar]
- Wells-Parker E, Dill P, Williams M, Stoduto G. Are depressed drinking/driving offenders more receptive to brief intervention? Addictive Behaviors. 2006;31:339–350. doi: 10.1016/j.addbeh.2005.05.011. [DOI] [PubMed] [Google Scholar]
- Worthington J, Fava M, Agustin C, Alpert J, Nierenberg AA, Pava JA, et al. Consumption of alcohol, nicotine, and caffeine among depressed outpatients. Relationship with response to treatment. Psychosomatics. 1996;37:518–522. doi: 10.1016/S0033-3182(96)71515-3. [DOI] [PubMed] [Google Scholar]