Abstract
Objective
To examine the associations between poverty dynamics and the long-term risk of developing overweight or obesity.
Design and methods
Our data are a representative sample of U.S. children from the National Longitudinal Survey of Youth 1979 Child and Young Adult Survey (1986-2008). We used survival analysis to compare risk of developing overweight or obesity among 5,613 children aged 4 to 14 from never poor households, transient poor households (those that became poor only once), recurrent poor households (those that became poor more than once), and persistent poor households (those that became poor and remained poor for at least 4 consecutive years) and examined interactions by race/ethnicity, gender, and age.
Results
Compared with children from never poor households, children from transient poor households (HR 0.79, 95% CI: 0.68, 0.92), recurrent poor households (HR: 0.73, 95% CI: 0.62, 0.87), and persistently poor households (HR: 0.62, 95% CI: 0.51, 0.74) had significantly reduced risks of becoming overweight or obese. These associations did not vary by race/ethnicity, gender, or age.
Conclusions
Our findings suggest that poverty experiences are associated with reduced risk of becoming overweight or obese among children 4 to 14.
Keywords: childhood overweight, poverty, childhood obesity, survival analysis
INTRODUCTION
Childhood overweight and obesity continue to present a substantial public health concern in the United States, where recent estimates suggest that approximately 17% of children ages 2 through 19 are obese (≥95th percentile of BMI-for-age) and 32% are overweight (≥85th and <95th percentile of BMI-for-age) (1). Overweight and obesity in early life are associated with increased risk of diabetes mellitus, hypertension, heart disease, sleep disturbances and a higher risk of obesity in adulthood (2-4). Although the prevalence of childhood overweight and obesity rose dramatically from the early 1970s until the early 2000s, socioeconomic disparities in these outcomes decreased during this period (5). In recent years, prevalence of child overweight has reached a plateau or begun to decline (1, 6). Of concern, however, is evidence that this leveling off has not occurred across all socioeconomic groups. Recent studies have reported that the prevalence of obesity among children and adolescents living in poverty has increased more than the prevalence among non-poor children (6-9). These findings suggest that socioeconomic disparities in childhood obesity may be widening, even as overall rates are leveling off.
Although socioeconomic disadvantage has been linked to higher prevalence of childhood obesity, these associations are not consistent across race/ethnicity, gender, and age. In general, inverse associations between family income and prevalence of overweight are strongest among white children (10-12), especially girls (5, 11); among non-Hispanic black girls, higher family income is associated with higher prevalence of overweight (5, 11). In some studies, associations between income and overweight or obesity are stronger among older children (11) or adolescents (8). However, most previous research has relied on cross-sectional data, and longitudinal research is needed to further our understanding of the causal relation between poverty and childhood obesity.
Moreover, little is known about the effects of poverty dynamics on children’s body weight. Americans tend to fall into and out of poverty throughout the lifecourse (13-15). In recent years, increasing numbers of households with children have fallen into poverty, likely due to effects of the Great Recession (http://www.census.gov/prod/2011pubs/acsbr10-05.pdf). Yet, little is known about how these dynamic poverty experiences affect children’s health, specifically their body weight. A cumulative risk model suggests that the total accumulation of family income across childhood should be the most salient predictor of health (13-16), and recent work has in fact shown that the proportion of childhood spent in poverty is positively associated with later BMI (17). On the other hand, temporary dips into poverty may signal the occurrence of other major life events such as job loss, a wage earner returning to school or a parent choosing to stay home instead of work, or a divorce or separation. Some of these events may be stressful, and household stressors are linked to childhood obesity (18).
The objective of this study was to examine the longitudinal associations between poverty dynamics and the risk of developing overweight and/or obesity between the ages of 4 to 14 in a representative cohort of U.S. children. We used survival analysis to compare the risk of developing overweight or obesity, comparing children from never poor households, transient poor households (those that became poor only once), recurrent poor households (those that became poor more than once), and persistent poor households (those that became poor and remained poor for at least 4 consecutive years). Because previous research indicates that the associations between family income and childhood obesity differ by children’s race/ethnicity, gender, and age, we also examined interactions between poverty groups and these factors.
METHODS AND PROCEDURES
Data and study sample
We used data from the National Longitudinal Survey of Youth 1979 (NLSY79) Child and Young Adult Survey, a national sample of US adolescents who were 14 to 22 in 1979. The NLSY Child and Young Adult Survey is a prospective study of 11,495 (as of 2008) children born to the original NLSY79 women. With appropriate weighting, these children may be considered a nationally representative sample of children who have been born to women who were 14 to 22 years old in 1979.
Data collection on children’s height and weight began in 1986. For this analysis, we defined the study period for each child as the time (in months) from the first BMI observation between the ages of 2 and 14 (baseline) and either 1) the first survey in which the child was overweight or obese, 2) the last survey before the child was lost to follow-up or reached the age of 15, or 3) 2008, whichever came first. Our sample included children between the ages of 2 and 14 years (n=10,087) who had at least one BMI measurement (n=9,963). We excluded children over the age of 14 because 1) we hypothesize that predictors of change in BMI in later adolescence may have a different set of influential factors as children gain independence from their parents, and 2) the NLSY survey began surveying children separately at age 15. We further restricted the analysis to children who were not overweight or obese at their baseline survey (n=7,362), children for whom household poverty data was available for at least 75 percent of the study period (n=5,630), and children for whom baseline maternal educational attainment or marital status was not missing (n=5,613). This final analytic sample was similar to the target population of 9,963 in terms of race/ethnicity, children’s age distribution, and maternal age, educational attainment, marital status, pre-pregnancy BMI, and employment status.
Measures
Outcome variables
The majority of children’s weights and heights were measured by an in home interviewer using a portable scale and tape measure (e.g., at the last follow-up survey, 63% of heights and 61% of weights were measured). The remaining weights and heights were reported by the mother or child (for older children). We calculated children’s BMI percentile at each time point where data was available on height, weight, and age using the anthropometry SAS program provided by the Centers for Disease Control (CDC) (http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm). We categorized childhood overweight and obesity according to the CDC’s definitions: BMI ≥85th and <95th percentile is considered overweight, and BMI ≥95th percentile is considered obese. Our primary outcome was the time in months from baseline until the first survey in which a child was either overweight or obese.
Measures of household poverty dynamics
The longitudinal nature of the NLSY79 data allowed us to examine the poverty dynamics of children’s households over the study period. Our primary measure was poverty status (yes/no), which is calculated based on maternal self-reported total net family income compared to the federal poverty level. Following previous work (19), we created four groups to describe the poverty dynamics of these households: the never poor; the transient poor (household became poor only once during study period); the recurrent poor (household became poor more than once during study period); and the persistent poor (household was poor for at least 4 consecutive years during study period).
Covariates
Race/ethnicity of children in the NLSY79 was assigned based on their mothers’ race/ethnicity and categorized by NLSY79 as black/non-Hispanic, Hispanic, and non-black/non-Hispanic (20). (In the original NLSY79 sample, those classified as non- Black/non-Hispanic primarily self-identified as being of European descent [68%], with the rest self-identifying as Asian/Pacific Islander [1%], American Indian [8%], “American” [9%], or other [14%]). We categorized maternal educational attainment as less than high school (<12 years), high school graduate (12 years), some college (13-15 years), or college graduate (≥16 years). We categorized maternal BMI based on the World Health Organization definitions of underweight (<18.5), normal weight (18.5 – 24.9), overweight (25.0 – 29.9), and obese (≥30.0). Maternal employment status was categorized as employed, unemployed, or out of the labor force.
Statistical Analysis
We calculated the frequency and weighted percent of baseline child and maternal characteristics (i.e., child gender, race/ethnicity, and age at baseline and maternal baseline age, educational attainment, BMI, marital status, and employment status) by the four poverty classes using weights to account for survey sampling and loss to follow–up.
We used survival analysis to compare the risk of developing overweight or obesity during the study period among children whose households had temporary, recurrent, or persistent poverty to those whose households were never poor. Survival analysis enabled us to estimate the risk of developing overweight or obesity over time, accounting for the fact that the baseline and end point of the study point differed by child and that some children were lost to follow–up before age 14. First, we examined the unadjusted Cox proportional hazards of becoming overweight or obese during the study period across the four poverty classes. We then calculated the Cox proportional hazards of becoming overweight or obese for the four poverty classes, adjusting for baseline child and maternal characteristics (described above). We also adjusted for year at baseline to account for secular trends in overweight. Maternal BMI and employment status were the only covariates with substantial amounts of missing data, and we used missing indicator variables for these variables. We calculated robust standard errors to account for potential correlation of outcomes between children of the same mother and weighted the analyses to account for survey sampling and differential non–response. Finally, we examined potential interactions between the four poverty groups and child age categories, race/ethnicity, and gender, using Wald tests of statistical significance for each set of interaction terms.
We conducted a secondary analysis in which we restricted our sample to children from households that were not poor at baseline (n=3,776). Although this analysis reduced our sample size, by comparing children from households that never became poor to those that were not poor at baseline but did become poor sometime during the study period, we were able to gain a more focused estimate of the association between becoming poor and development of child overweight and obesity. (Note that households not poor at baseline were still able to be categorized in the persistent poverty group if they became poor and remained poor for at least 4 years during study period.)
We conducted a number of tests of robustness. First, we repeated the analysis using obesity only as our outcome (instead of combing overweight and obesity). Next, we estimated models restricting our sample to only those records where both the height and weight at follow-up were measured instead of self-reported. (Because data on source of height and weight were not available for 1986, we were not able to restrict our sample to measured heights and weights at baseline.) Because the use of missing indicator variables has been shown to lead to biased estimates (21), we also conducted a complete case analysis excluding observations with missing data for any covariates. We observed that children in the transient, recurrent, and persistent poor groups were more likely to be older at baseline, which could bias our findings if these children were more likely to have already developed overweight before entering the study. We therefore repeated the analysis only among children who were five years old or less at baseline. Finally, height and weight can vary substantially across childhood and small errors in reporting may lead to incorrectly classifying children as overweight based on only one measure. Therefore, we repeated the analysis where children had to have two consecutive measures of overweight to be classified with the outcome.
RESULTS
Of the 5,613 children in our study, 16.4% were black/non Hispanic, 7.7% were Hispanic, and 75.9% were non-black/non-Hispanic. The majority of the children were between 3 and 5 years at baseline. At baseline, approximately 55% of mothers were normal weight, 22% were overweight, and 15% were obese. Other maternal baseline characteristics are described in Table 1. Almost 41 percent of children in the study sample became overweight or obese during the study period. Approximately 68% of children’s households were never poor during the study period, 14% became poor once, 9% became poor more than once, and 10% became poor and remained poor for at least four years. Children from households with any experience of poverty during the study period were more likely to be older and of Black/non-Hispanic or Hispanic race/ethnicity, and these mothers were more likely to be older, less educated, unmarried, unemployed, or out of the labor force at baseline (Table 1).
Table 1.
Distribution of maternal and child characteristics, National Longitudinal Survey of Youth 1979 Child/Young Adult (n=5,613)
| Full sample | Never poor | N (weighted%) Transient poor |
Recurrent poor | Persistent poor | |
|---|---|---|---|---|---|
| Poverty experience | 5613 (100.0) | 3250 (67.6) | 896 (13.9) | 725 (8.9) | 742 (9.6) |
| Became overweight or obese during study period | 2177 (40.9) | 1293 (42.2) | 602 (35.1) | 271 (38.2) | 319 (43.2) |
| Child sex | |||||
| Female | 2797 (49.0) | 1612 (48.0) | 466 (53.1) | 343 (46.3) | 376 (52.1) |
| Male | 2816 (51.0) | 1638 (52.0) | 430 (46.9) | 382 (53.7) | 366 (47.9) |
| Child age (years)a | |||||
| Less than 3 | 1525 (30.6) | 969 (32.6) | 212 (27.9) | 148 (22.6) | 196 (27.5) |
| 3-5 | 2898 (54.1) | 1733 (55.2) | 427 (50.8) | 335 (49.0) | 403 (55.3) |
| 6-8 | 814 (10.7) | 371 (8.4) | 164 (14.3) | 163 (19.5) | 116 (13.5) |
| 9-11 | 301 (3.7) | 137 (2.9) | 61 (4.8) | 76 (8.5) | 27 (3.6) |
| 12 and over | 75 (0.9) | 40 (0.9) | 32 (2.2) | 3 (0.5) | 0 (0) |
| Maternal race/ethnicity | |||||
| Black/non-Hispanic | 1548 (16.4) | 557 (9.0) | 243 (18.2) | 310 (36.5) | 438 (47.2) |
| Hispanic | 1038 (7.7) | 569 (6.4) | 149 (7.6) | 160 (12.8) | 160 (12.0) |
| Non-Black/non-Hispanic | 3027 (75.9) | 2124 (84.7) | 504 (74.2) | 255 (50.7) | 144 (40.8) |
| Maternal age (years)a | |||||
| 21-29 | 3454 (48.6) | 1708 (40.2) | 657 (62.2) | 602 (76.0) | 487 (62.5) |
| 30-39 | 1915 (45.3) | 1369 (52.5) | 213 (33.7) | 115 (23.0) | 218 (31.9) |
| 40-52 | 244 (6.1) | 173 (7.3) | 26 (4.1) | 8 (1.0) | 37 (5.6) |
| Maternal educational attainmenta | |||||
| Less than high school (<12 years) | 1620 (20.6) | 479 (10.8) | 353 (30.7) | 380 (45.1) | 408 (52.2) |
| High school graduate (12 years) | 2181 (38.9) | 1324 (38.8) | 346 (40.6) | 247 (38.9) | 264 (37.0) |
| Some college (12 to <16 years) | 1067 (19.7) | 766 (22.1) | 141 (17.4) | 95 (15.7) | 65 (9.9) |
| College graduate (16 or more years) | 745 (20.8) | 681 (28.3) | 56 (11.2) | 3 (0.3) | 5 (0.9) |
| Maternal marital statusa | |||||
| Unmarried | 1897 (24.2) | 453 (10.2) | 400 (34.6) | 468 (58.3) | 576 (76.6) |
| Married | 3716 (75.8) | 2797 (89.8) | 496 (65.4) | 257 (41.7) | 166 (23.4) |
| Maternal BMI categorya | |||||
| Underweight (<18.5) | 232 (4.1) | 123 (3.8) | 45 (4.7) | 38 (6.5) | 26 (3.7) |
| Normal (18.5–24.9) | 2988 (54.8) | 1792 (56.8) | 492 (54.3) | 392 (54.0) | 312 (42.1) |
| Overweight (25.0-29.9) | 1272 (22.2) | 749 (22.1) | 169(18.5) | 152 (21.3) | 202 (29.0) |
| Obese (≥30) | 843 (14.3) | 444 (13.3) | 131 (15.5) | 106 (13.3) | 162 (20.6) |
| Missing | 278 (4.5) | 142 (4.0) | 59 (7.0) | 37 (4.9) | 40 (4.6) |
| Maternal employment statusa | |||||
| Employed | 2773 (50.5) | 1992 (57.6) | 393 (45.3) | 234 (34.3) | 154 (23.5) |
| Unemployed | 388 (5.3) | 114(2.7) | 92 (9.2) | 98 (12.7) | 84(10.5) |
| Out of the labor force | 2045 (33.7) | 829 (26.6) | 373 (38.9) | 382 (51.2) | 461 (59.7) |
| Missing | 407 (10.5) | 315 (13.1) | 38 (6.6) | 11(1.8) | 43 (6.2) |
At baseline survey
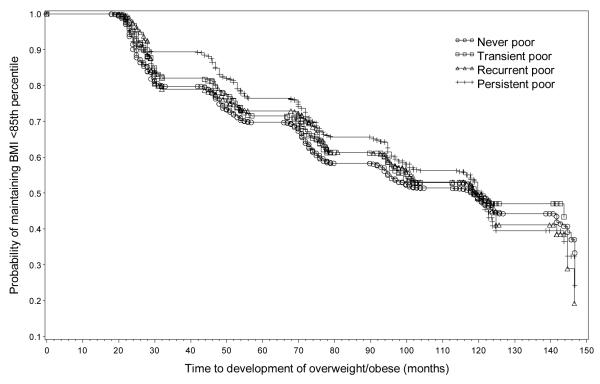
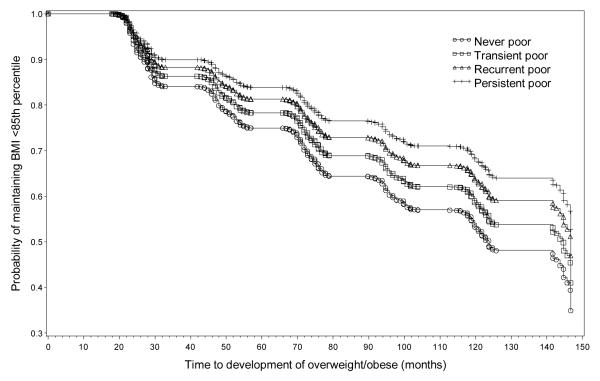
Figure 1 presents the unadjusted Kaplan-Meier curves for each poverty group. In unadjusted Cox proportional hazard models, children in transient poor households had 0.83 times the hazard of becoming overweight during the study period compared to children whose households never became poor (95% CI: 0.71, 0.97). Children in recurrent poor households had 0.84 (95% CI: 0.72, 0.98) the hazard of becoming overweight compared to the never poor, and children in persistent poor households had 0.89 (95% CI: 0.77, 1.00) times the hazard of becoming overweight. In adjusted Cox models, hazard rates for the three less advantaged poverty trajectories diverged even further from the never poor group (Table 2). Compared to children from never poor households, children from transient poor households had 0.79 times the hazard (95% CI: 0.68, 0.93), children from recurrent poor households had 0.74 times the hazard (95% CI: 0.62, 0.88), and children from persistently poor households had 0.61 times the hazard (95% CI: 0.51, 0.74) of becoming overweight. Figure 2 illustrates these adjusted survival curves for children from never poor, transient poor, recurrent poor, and persistent poor households. We found no evidence of statistically significant interactions between poverty groups and race/ethnicity (p=0.68), gender (p=0.65), or child’s age categories (p=0.47).
Figure 1.
Kaplan-Meier curves for development of overweight or obesity among children in never poor, transient poor, recurrent poor, and persistent poor households.
Table 2.
Hazard ratiosa for development of overweight and/or obesity during study period
| HR (95% CI) | ||
|---|---|---|
| All children (n=5,613) |
Children from households not poor at baseline (n=3,776) |
|
| Poverty experience | ||
| Never poor | (ref) | (ref) |
| Transient poor | 0.79 (0.68, 0.93) | 0.71 (0.60, 0.84) |
| Recurrent poor | 0.74 (0.62, 0.88) | 0.47 (0.36, 0.62) |
| Persistent poor | 0.61 (0.51, 0.74) | 0.26 (0.15, 0.47) |
| Child age (years) | ||
| Less than 3 | 1.06 (0.95, 1.19) | 1.07 (0.96, 1.20) |
| 3-5 | (ref) | (ref) |
| 6-8 | 0.91 (0.76, 1.08) | 0.81 (0.67, 0.98) |
| 9-11 | 0.77 (0.55, 1.09) | 0.47 (0.28, 0.80) |
| 12 and over | 0.97 (0.31, 3.08) | 1.28 (0.50, 3.27) |
| Race/ethnicity | ||
| Black/non-Hispanic | 1.15 (1.03, 1.29) | 1.15 (1.00, 1.32) |
| Hispanic | 1.01 (0.89, 1.14) | 0.99 (0.86, 1.13) |
| Non-Black/non-Hispanic | (ref) | (ref) |
| Maternal age (years) | ||
| 23-29 | (ref) | (ref) |
| 30-39 | 1.07 (0.89, 1.28) | 1.05 (0.87, 1.26) |
| 39-51 | 1.34 (0.93, 1.95) | 1.20 (0.83, 1.75) |
| Maternal educational attainment | ||
| Less than high school (<12 years) | 1.49 (1.22, 1.81) | 1.45 (1.19, 1.77) |
| High school graduate (12 years) | 1.25 (1.06, 1.48) | 1.23 (1.04, 1.44) |
| Some college (12 to <16 years) | 1.26 (1.05, 1.50) | 1.22 (1.03, 1.44) |
| College graduate (16 or more years) | (ref) | (ref) |
| Maternal marital status | ||
| Unmarried | 1.35 (1.18, 1.53) | 1.24 (1.07, 1.44) |
| Married | (ref) | (ref) |
| Maternal BMI category | ||
| Underweight (<18.5) | 0.82 (0.60, 1.12) | 0.63 (0.44, 0.92) |
| Normal (18.5 – 24.9) | (ref) | (ref) |
| Overweight (25.0-29.9) | 1.59 (1.40, 1.80) | 1.51 (1.33, 1.71) |
| Obese (≥30) | 2.09 (1.82, 2.40) | 2.22 (1.94, 2.55) |
| Maternal employment status | ||
| Employed | (ref) | (ref) |
| Unemployed | 1.17 (0.94, 1.44) | 1.15 (0.88, 1.49) |
| Out of the labor force | 0.92 (0.81, 1.04) | 0.90 (0.80, 1.02) |
| Baseline year | 1.03 (1.01, 1.06) | 1.02 (0.99, 1.04) |
Estimates from Cox proportional hazard models with robust standard errors to account for clustering by mother and weighted to account for survey sampling and differential non-response
Figure 2.
Adjusted survival curves for development of overweight or obesity among children in never poor, transient poor, recurrent poor, and persistent poor households.
Results from the model restricted to children in non-poor households at baseline showed an even stronger negative association between becoming poor and the hazard of developing of childhood overweight or obesity (Table 2). Compared to children from never poor households, children from transient poor households had 0.71 times the hazard (95% CI: 0.60, 0.84), children from recurrent poor households had 0.47 times the hazard (95% CI: (0.36, 0.62), and children from persistently poor households had 0.26 times the hazard (95% CI: 0.15, 0.47) of becoming overweight. Table 2 also shows other factors that were significantly related to increased risk of developing overweight included Black/non-Hispanic race/ethnicity, older maternal age, mother being unmarried at baseline, and mother being overweight or obese at baseline.
Estimates from models for development of obesity only, those restricted to children five years or less at baseline, those where we required consecutive measures of overweight models, those restricted to measured heights and weights only, and the complete case analysis were similar in both magnitude and significance to the original models (Table 3). Estimates for the transient poor group were attenuated and not significant for the obesity only model and marginally significant for the complete case analysis.
Table 3.
Hazard ratios1 for development of overweight and/or obesity during study period from alternative models
| Hazard ratios (95% CI) | |||||
|---|---|---|---|---|---|
| N | N (weighted percent) with event |
Transient poor | Recurrent poor | Persistent poor | |
| Model for development of obesity only | 6,529 | 1,457 (23.3) | 0.90 (0.77, 1.05) | 0.74 (0.62, 0.89) | 0.58 (0.48, 0.71) |
| Sample restricted to records with measured height and weight | 3,202 | 1,318 (45.3) | 0.77 (0.64, 0.92) | 0.76 (0.63, 0.92) | 0.57 (0.46, 0.70) |
| Complete case analysis | 4,936 | 1,919 (41.4) | 0.85 (0.74, 0.98) | 0.77 (0.66, 0.90) | 0.56 (0.47, 0.66) |
| Model restricted to children ≤5 years at baseline | 4,423 | 1,923 (44.1) | 0.79 (0.67, 0.93) | 0.71 (0.59, 0.86) | 0.63 (0.52, 0.77) |
| Model restricting children classified as developing overweight to those with two consecutive observations of overweight |
4,668 | 1,582 (32.5) | 0.78 (0.66, 0.93) | 0.56 (0.45, 0.69) | 0.38 (0.31, 0.48) |
Estimates from Cox proportional hazard models with robust standard errors to account for clustering by mother and weighted to account for survey sampling and differential non-response. Models additionally adjusted for child age and race/ethnicity and maternal age, educational attainment, marital status, BMI, and employment status
DISCUSSION
We examined the associations between becoming poor and development of childhood overweight or obesity between the ages of 4 and 14 in a representative sample of children. Findings show that, compared to children whose households were never poor during the study period, children whose households were poor for at least four consecutive years (persistent poor) had a 39% lower risk of developing overweight/obesity by age 14. Compared to children whose households were never poor, children whose households became poor more than once but not for four consecutive years (recurrent poor) had a 26% lower risk of becoming overweight or obese, and children whose households became poor only once (transient poor) had a 21% lower risk of developing overweight/obesity by age 14. Moreover, when comparing children from households that were not poor at baseline, we find even stronger evidence that becoming poor is strongly associated with reduced risk of developing overweight.
Previous cross-sectional research has found that family income is inversely associated with child overweight and obese status (22), although this association is strongest among non-Hispanic white children (10, 12), especially females (5, 11) and, in some studies, older children and adolescents (8, 11). Only recently have researchers begun to examine the longitudinal associations between household income and BMI in children. In a sample of 329 children from rural, upstate New York, Wells and colleagues (17) found that the proportion of a child’s early life spent in poverty was positively associated with BMI growth trajectories between the ages of 9 to 17. In a sample of 1,356 children from the Study of Early Child Care and Youth Development, Kendzor and colleagues estimated household income trajectories from birth to age 15 and examined the associations between five different trajectories and BMI percentile at age 15. Children from households that experience downward mobility or stable low income had on average greater BMI percentile at age 15 compared to those from upwardly mobile households or households with stable, adequate income (23).
Our findings differ from this previous work, suggesting that the experience of becoming poor may have different implications for development of childhood overweight and obesity than does long-term poverty. We propose several possible explanations for our findings, but caution that much additional work is needed to confirm our results and to examine the mechanisms connecting poverty dynamics to body weight in children. First, becoming poor may be associated with behavioral changes, such as reduced spending on food outside the home, that are associated with lower body weight. Interestingly, a related body of work finds that physical activity increases and body weight decreases during recessions and hypothesizes that this is due to increased leisure time or reduced spending on unhealthy food among those who lose their jobs (24, 25). Second, dips into poverty, even those that reoccur or last for four years, may signal household events such as a parent returning to school or dropping out of the labor force to stay home with children that may lead to healthier behaviors in the family as a whole. Mothers who work more hours are, in fact, more likely to have a child who is overweight (26, 27). Either of these hypotheses could be consistent with our results while not contradicting other evidence that long term poverty is associated with obesity in childhood or adolescence.
This is the first study of which we are aware to examine the longitudinal associations between becoming poor and the risk of developing overweight in childhood, taking into account different poverty dynamics. The NLSY79 Children and Young Adult Survey provides data on household poverty and child height and weight for over 20 years and is representative of U.S. children born to women who were 14 to 22 years of age in 1979. The survival analysis strengthens these findings because we are able to account for loss to follow-up and differing lengths of study period for each child. Our findings are further strengthened by our finding of a dose-response relationship with the most disadvantaged children having the lowest risk of developing overweight. Our results were also robust to a variety of alternative specifications.
Our study is not without limitations, however. We were unable to include children without measures of BMI and those with a large majority of missing data on household income; however, these respondents did not differ substantially from the target population of 9,963 nor from the overall population of NLSY children (n=11,495) in terms of mother’s race/ethnicity, educational attainment, marital status, BMI, or poverty status at entry into NLSY79. One might wonder if the unexpected findings are because the sample is selectively different from other nationally representative samples. However, our sample is similar in terms of race/ethnicity and income to children 2 to 18 in the National Health and Nutrition Examination Surveys (NHANES) from the same time period (results available upon request); the overall prevalences of overweight and obesity are slightly higher in our sample than in NHANES, but overall, we are confident that our data are a reasonably representative sample of US children from the late 1980s to mid-2000s.
A subset of children in our sample had self-reported weights and heights, but excluding these children from the analysis did not substantially change our results. We also lacked data on factors such as food insecurity, diet, physical activity, television viewing, and other factors that could have enabled us to explore potential mediators of the relation between poverty dynamics and child overweight, and we did not have data on poverty status prior to baseline. Although longitudinal analyses such as this one improve our ability to examine causal relations (relative to cross sectional studies), we caution that our findings are based on observational data and therefore cannot be interpreted as causal.
Given the sizable proportion of children in the US living in poverty and the substantial fluctuation in and out of poverty of households in our country, it is important that we understand the influences of these dynamic poverty experiences on children’s health and well-being. Although our findings suggest that poverty experiences may be associated with a decrease in children’s risk of developing overweight or obesity, there will likely be other negative impacts of these experiences on health and social outcomes. More research is needed to confirm our findings in other longitudinal samples of children; to explore the impacts of dynamic poverty experiences on risk factors for child overweight such as diet, physical activity, stress, and sleep; and to understand the influences of poverty experiences on other health and social outcomes among children.
What is already known about this subject
- The prevalence of obesity among children living in poverty appears to be increasing while the prevalence among non-poor children is leveling off.
- Previous cross-sectional studies show that socioeconomic disadvantage is linked to higher prevalence of childhood obesity, but these associations are not consistent across race/ethnicity, gender, and age.
What this study adds
- We use survival analysis to examine the longitudinal associations between poverty dynamics and development of overweight and obesity in childhood in a representative sample of children.
- We find that poverty experiences such as temporary, recurrent, and persistent poverty are associated with reduced risk of becoming overweight or obese among children 4 to 14, compared to never poor children.
ACKNOWLEDGEMENTS
CMZ and CC conceived of and designed the study. CMZ conducted the literature review, data management, and analysis. CMZ drafted the manuscript, and CC edited the manuscript. This work was supported by a grant from the American Cancer Society (RSGT-11-010-01-CPPB) to C. Cubbin and by grant 5 R24 HD042849 awarded to the Population Research Center at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Health and Child Development.
Footnotes
CONFLICTS OF INTEREST STATMENT None of the authors have relationships, financial or otherwise, for which a conflict of interest exists.
REFERENCES
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999 2010. JAMA. 2012;307:483–90. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Preventing Childhood Obesity: Health in the Balance. National Academy of Sciences; Washington DC: 2005. [Google Scholar]
- 3.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518–25. [PubMed] [Google Scholar]
- 4.Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9:474–88. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 5.Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am J Clin Nutr. 2006;84:707–16. doi: 10.1093/ajcn/84.4.707. [DOI] [PubMed] [Google Scholar]
- 6.Wen X, Gillman MW, Rifas-Shiman SL, Sherry B, Kleinman K, Taveras EM. Decreasing prevalence of obesity among young children in Massachusetts from 2004 to 2008. Pediatrics. 2012;129:823–31. doi: 10.1542/peds.2011-1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Babey SH, Hastert TA, Wolstein J, Diamant AL. Income disparities in obesity trends among California adolescents. Am J Public Health. 2010;100:2149–55. doi: 10.2105/AJPH.2010.192641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miech RA, Kumanyika SK, Stettler N, Link BG, Phelan JC, Chang VW. Trends in the association of poverty with overweight among US adolescents, 1971-2004. JAMA. 2006;295:2385–93. doi: 10.1001/jama.295.20.2385. [DOI] [PubMed] [Google Scholar]
- 9.Singh GK, Siahpush M, Kogan MD. Rising social inequalities in US childhood obesity, 2003-2007. Ann Epidemiol. 2010;20:40–52. doi: 10.1016/j.annepidem.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 10.Bethell C, Read D, Goodman E, et al. Consistently inconsistent: a snapshot of across- and within-state disparities in the prevalence of childhood overweight and obesity. Pediatrics. 2009;123(Suppl 5):S277–86. doi: 10.1542/peds.2008-2780F. [DOI] [PubMed] [Google Scholar]
- 11.Gordon-Larsen P, Adair LS, Popkin BM. The relationship of ethnicity, socioeconomic factors, and overweight in US adolescents. Obes Res. 2003;11:121–9. doi: 10.1038/oby.2003.20. [DOI] [PubMed] [Google Scholar]
- 12.Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 13.Iceland J. Dynamics of economic well-being, poverty 1996-1999. Current Population Reports. U.S. Census Bureau; Washington, DC: 2003. pp. 70–91. [Google Scholar]
- 14.Rank MR, Hirschl TA. Rags or riches? Estimating the probabilities of poverty and affluence across the adult American life span. Social Science Quarterly. 2001;82:651–69. [Google Scholar]
- 15.Stevens AH. The dynamics of poverty spells: updating Bane and Ellwood. American Economic Review. 1994;84:34–7. [Google Scholar]
- 16.Chen E, Martin AD, Matthews KA. Trajectories of socioeconomic status across children’s lifetime predict health. Pediatrics. 2007;120:e297–303. doi: 10.1542/peds.2006-3098. [DOI] [PubMed] [Google Scholar]
- 17.Wells NM, Evans GW, Beavis A, Ong AD. Early childhood poverty, cumulative risk exposure, and body mass index trajectories through young adulthood. Am J Public Health. 2010;100:2507–12. doi: 10.2105/AJPH.2009.184291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gundersen C, Lohman BJ, Garasky S, Stewart S, Eisenmann J. Food security, maternal stressors, and overweight among low-income US children: results from the National Health and Nutrition Examination Survey (1999-2002) Pediatrics. 2008;122:e529–40. doi: 10.1542/peds.2008-0556. [DOI] [PubMed] [Google Scholar]
- 19.Muffels R, Fourage D, Dekker R. [Accessed July 1, 2012];Longitudinal Poverty and Income Inequality: A Comparative Panel Study for The Netherlands, Germany and the UK. Munich Personal RePEc Archive. 2000 http://mpra.ub.uni-muenchen.de/13298/
- 20.Bureau of Labor Statistics [Accessed January 26 2010];National Longitudinal Studies Handbook. 2008 http://www.bls.gov/nls/handbook/nlshndbk.htm.
- 21.Greenland S, Finkle WD. A critical look at methods for handling missing covariates in epidemiologic regression analyses. Am J Epidemiol. 1995;142:1255–64. doi: 10.1093/oxfordjournals.aje.a117592. [DOI] [PubMed] [Google Scholar]
- 22.Strauss RS, Knight J. Influence of the home environment on the development of obesity in children. Pediatrics. 1999;103:e85. doi: 10.1542/peds.103.6.e85. [DOI] [PubMed] [Google Scholar]
- 23.Kendzor DE, Caughy MO, Owen MT. Family income trajectory during childhood is associated with adiposity in adolescence: a latent class growth analysis. BMC Public Health. 2012;12:611. doi: 10.1186/1471-2458-12-611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ruhm CJ. Are recessions good for your health? Quarterly Journal of Economics. 2000;115:617–50. [Google Scholar]
- 25.Ruhm CJ. Healthy living in hard times. Journal of Health Economics. 2005;24:341–63. doi: 10.1016/j.jhealeco.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 26.Anderson PM, Butcher KF, Levine PB. Maternal employment and overweight children. J Health Econ. 2003;22:477–504. doi: 10.1016/S0167-6296(03)00022-5. [DOI] [PubMed] [Google Scholar]
- 27.Hawkins SS, Cole TJ, Law C. Maternal employment and early childhood overweight: findings from the UK Millennium Cohort Study. Int J Obes (Lond) 2008;32:30–8. doi: 10.1038/sj.ijo.0803682. [DOI] [PMC free article] [PubMed] [Google Scholar]