Abstract
Objective
To determine the influence of choice of prescription and other child-, family- and intervention-related factors on speech, language, and functional performance of hearing-impaired children by three years of age.
Design and study sample
A randomized controlled design was implemented as part of a population-based, longitudinal study on outcomes of children with hearing impairment (LOCHI) in Australia. Two hundred and eighteen children were randomly assigned to either the NAL or the DSL prescription for first fitting of hearing aids. Their performance outcomes were evaluated.
Results
Prescriptive targets were closely matched in children's hearing aids. There were not significant differences in children's language, speech production, or functional performance between prescriptions. Parents' ratings of children's device usage and loudness discomfort were not significantly different between prescription groups. Functional performance within the first year of fitting together with degree of hearing loss, presence of additional disabilities, and maternal education explained 44% of variation in language ability of children by three years of age.
Conclusions
There was no significant association between choice of hearing-aid prescription and variance in children's outcomes at three years of age. In contrast, additional disability, maternal educational level, and early functional performance were significant predictive factors of children's outcomes.
Keywords: Hearing-aid prescription, children, NAL-NL1, DSL v.4.1, randomized controlled trial, DSL m[i/o], NAL-NL2, maternal education, socio-economic status, language, speech, functional performance, PEACH, PLS-4, PPVT, CDI, DEAP
The implementation of universal newborn hearing screening has made it possible for early identification of hearing loss and provision of intervention. As a crucial component of intervention, timely amplification with optimal gain-frequency responses is essential. The prescribed responses of the National Acoustic Laboratories (NAL) procedure (Byrne et al, 2001) and the Desired Sensation Level (DSL) procedure (Seewald et al, 1997; Scollie et al, 2005) are widely adopted by clinicians as targets for fitting hearing aids to children. These procedures differ in rationale. The NAL procedure aims to maximize predicted speech intelligibility while limiting total loudness to no greater than that perceived by a normal hearer listening to the same sound; whereas the DSL procedure aims to normalize loudness at different frequencies. For this reason, the prescriptions sometimes differ markedly in terms of gain-frequency responses for the same audiometric configurations (Byrne et al, 2001; Ching et al, 2010; Johnson & Dillon, 2011). Despite their worldwide adoption, the relative effectiveness of the respective prescriptions for supporting children's speech and language development is yet to be established.
Over the past decade, we have increased our understanding of the effects of choice of prescriptions for school-aged children through both independent research and collaborative research between the National Acoustic Laboratories and the University of Western Ontario. First, large differences in gain-frequency responses prescribed by the NAL and the DSL prescriptions were generally not achieved in real-life fitting of hearing aids. On average, the gain difference between the two prescriptions achieved in hearing aids was 7 dB for mid input levels (Ching et al, 2010). Second, speech perception by children in laboratory settings was similar for both prescriptions (Scollie et al, 2010). Third, loudness ratings of speech amplified with either prescription were within the range of comfortable listening. Even though the different prescriptions led to predictable differences in loudness rating at initial fitting, these differences largely disappeared with several weeks of listening experience (Jenstad et al, 1999, 2000, 2007; Scollie et al, 2010). Fourth, children preferred to listen to amplified speech in laboratory conditions at levels to which they were accustomed (Ching et al, 1996; Scollie et al, 2000, 2010). Fifth, children's preferences in everyday life were largely driven by auditory experience, although there were some variations related to real-world environments. They preferred the DSL prescription when listening to soft speech, but the NAL prescription when listening to speech in noisy environments (Scollie et al, 2010). Overall, the existing evidence suggests that the choice of prescription has little consequence in speech understanding or listening comfort for older children with largely late-identified mild to moderately severe hearing loss. However, the effects of auditory experience cannot be separated from those of electroacoustic differences resulting from application of the respective prescriptions in hearing aids (Ching et al, 2010). Such differences may be important for children's development of speech, language, and functional skills in the short and longer term when amplification is provided from the first few months of life. There were no current studies that examined the developmental impact of prescription choice on young children newly identified with hearing loss.
As with all aspects of intervention, the effectiveness of hearing-aid fitting needs to be established by evaluating and monitoring children's performance with amplification. For infants and young children, evaluation tools that rely on parent observations and reports on children's functional performance in real-world environments are widely used (Zimmerman-Phillipps et al, 1998; Weichbold et al, 2004; Ching & Hill, 2007; Coninx et al, 2009). Such tools may be used to check whether amplification characteristics may need to be altered (Byrne & Ching, 1997) or, in the more extreme case, if different management practices including cochlear implantation, alternative communication modes, and styles of early educational intervention should be considered. Furthermore, if functional performance assessed shortly after the implementation of amplification were predictive of longer term outcomes, strategies may be designed to target children with low early functional levels. However, no prospective studies have been conducted to collect such data.
The present study was designed to address the evidence gaps by evaluating the relative effectiveness of the NAL and DSL prescriptions for infants and young children who were newly identified with hearing loss. The existence of a national hearing service network, Australian Hearing (AH), for hearing-impaired children in Australia ensures that consistent and uniform services are provided to all children. As the research arm of AH, we conducted a randomized controlled trial of prescriptions for children who first received intervention for hearing loss before three years of age. This trial is a sub-component of the population-based longitudinal study on outcomes of children with hearing impairment (LOCHI study, ACTRN12611000429954). Through the national service provision network, we invited families to participate in this study. Once informed consent was obtained, children were randomly assigned to either a NAL or DSL prescription for hearing-aid fitting. Their hearing thresholds, hearing-aid real-ear gains, and outputs were assessed and monitored via the service provision network; and their outcomes were evaluated at several time points by researchers. The outcomes measures included speech production, expressive and receptive language, social skills and real-life functional performance.
On the basis of current knowledge, it was hypothesized that children's development at three years of age would not differ according to the prescription used for fitting. We speculated that family and intervention related factors would be important to speech, language, and functional outcomes. The primary aim of this study was to quantify the contribution of prescription method, together with other putative child, family, and intervention related factors, to explaining children's development of receptive and expressive language, speech production, and functional performance by three years of age. A secondary aim was to investigate whether functional performance assessed shortly after intervention could be a significant predictor of variability in outcomes at three years of age.
Method
Design of the study
This is a randomized controlled study. We compared outcomes of children with bilateral hearing loss according to their exposure from inception to either the NAL or the DSL procedure for hearing-aid fitting. A prospective approach was used to examine development after amplification, with measures conducted at 6 and 12 months after hearing-aid fitting, and at the chronological age of three years. This paper reports the children's performance at three years of age (children's age at evaluation ranged between 34 and 42 months, with 96% of the evaluations performed between 36 and 42 months).
Participants
All families of children with hearing loss born between 2002 and 2007 were invited to participate in the LOCHI study (Ching et al, 2010) if they: (1) were residing in the Australian states of New South Wales, Victoria, and Queensland (excluding regional Queensland), and (2) first presented for hearing services at AH paediatric centres before the children turned three years of age. The sample in this trial of hearing-aid prescription comprised the sub-group of children diagnosed with bilateral hearing loss who enrolled in the study prior to hearing-aid fitting, and who were using bilateral hearing aids by three years of age. There were 218 children, comprising 129 boys (59%) and 89 girls (41%). This sample size permits an effect size of 0.28 within-group standard deviation to be detected with a power of 80%, for an alpha level of 0.05.
Demographic characteristics
The demographic characteristics of children were solicited from parents using custom-designed questionnaires. Family socioeconomic status was determined from the Australian Census-based socio-economic indexes for areas (SEIFA) index for relative socioeconomic advantage and disadvantage (Australian Bureau of Statistics, 2008). The index defines relative socioeconomic advantage and disadvantage in terms of `people's access to material and social resources, and their ability to participate in society' (ABS, 2008, p. 6). A lower index is associated with greater relative disadvantage. Maternal education was specified in terms of a 3-point scale: less than or equal to 12 years of school attendance, diploma or certificate, and university qualification.
Hearing-aid fitting
All children had bilateral sensorineural hearing loss. Following enrolment, individual children were randomly assigned to hearing-aid fitting with either the NAL prescription (NAL-NL1; Byrne et al, 2001) or the DSL prescription (DSL[i/o] v.4.1; Seewald et al, 1997). All children were fitted bilaterally with multi-channel hearing aids that have wide-dynamic-range compression capabilities, in accordance with the AH national paediatric amplification protocol (King, 2010). Hearing thresholds were estimated from electrophysiological measures at diagnosis or, where applicable, behavioural measures were obtained using standard audiological procedures. A real-ear-aided gain approach (Moodie et al, 1994; Seewald et al, 1999; Ching & Dillon, 2003; Bagatto et al, 2005) was used for fitting. This involved using either individual real-ear-to-coupler differences (RECD) or age-appropriate values to derive gain targets in an HA2-2cc coupler by using the NAL-NL1 or the DSL v.4.1 standalone software. Hearing aids were adjusted in an HA2-2cc coupler, using a broadband speech-weighted stimulus generated by the Aurical system to measure gain-frequency responses at low, mid, and high input levels, and a swept pure tone presented at 90 dB SPL for measuring maximum output. Verification was achieved by comparing the measured 2cc coupler gain/output to custom target values.
As an integral part of the ongoing audiological service provision, children's hearing-aid fittings were adjusted as and when there were changes in hearing thresholds and when updated versions of prescriptive procedures become available. At the time of evaluations reported in this study, the DSL group comprised 57 children fitted according to DSL m[i/o] (Scollie et al, 2005), with the remaining children fitted according to DSL v.4; and all children in the NAL group used hearing aids fitted according to NAL-NL1. Subsequent to evaluations, the hearing-aid fittings of all children have been updated, according to their assigned group, to either DSL m[i/o] or NAL-NL2 (Dillon et al, 2011). For purposes of comparing children's hearing-aid gain-frequency responses used at evaluations to current versions of each of the two prescriptive procedures, we used the standalone software to derive custom targets for individual children. These targets were compared to the measured hearing-aid gain and output values to quantify the deviation of user values from optimal gain/output based on current knowledge.
Evaluation Measures
A team of qualified speech pathologists who were blinded to children's hearing aid characteristics administered a range of age-appropriate measures directly to children at three years of age. These included the Preschool Language Scale (PLS-4; Zimmerman et al, 2002), and the Peabody Picture Vocabulary Test (PPVT; Dunn & Dunn, 1997, 2007) for assessing expressive and receptive language and vocabulary; and the Diagnostic Evaluation of Articulation and Phonology test (DEAP; Dodd et al, 2002) for assessing speech production. Also, speech pathologists provided a rating on the overall intelligibility of speech produced by children. In addition, parents completed written questionnaires. These included checklists based on the Child Development Inventory (CDI; Ireton, 2005) for children's expressive and receptive language as well as social skills development, and the Parents' Evaluation of Aural/oral functional performance of CHildren (PEACH; Ching & Hill, 2007) for children's functional performance in real life. The PEACH also provided a measure of usage of hearing device and listening comfort in daily lives, as reported by parents.
Data analyses
To examine the effect of prescription and other factors on outcomes, three separate principal components analyses (e.g. Johnson, 1998; Strube, 2003) were used to aggregate multiple measures to represent outcomes in language, speech production, and functional performance. Multivariate linear regression was performed to estimate the contribution of respective predictor variables to the variance in each of the principal component scores. The regression coefficients for different predictors with 95% confidence intervals and p values were reported, and the coefficients of determination (R2) for the whole models were reported to quantify explained variance. We used two-tailed tests for all analyses, and set statistical significance at p < 0.05. All statistical analyses were carried out using Statistica software (Statsoft Inc., Release 7.1).
Results
Two hundred and eighteen children participated in this study. As shown in Figure 1, at three years of age there were 122 children using the NAL-NL1 prescription (NAL group) and 96 children using the DSL prescription (DSL group). The NAL group included both 115 children initially assigned to the NAL prescription and an additional seven children who were initially assigned to the DSL fitting but were subsequently refitted with a NAL-NL1 prescription at their parents' request. The 96 children in the DSL group were fitted with the DSL v.4.1 prescription, 58 of whom had their hearing aids updated with the DSL m[i/o] prescription as part of the routine services provided by AH prior to their evaluations at three years of age. Demographic characteristics for all children are summarized in Table 1.
Figure 1.
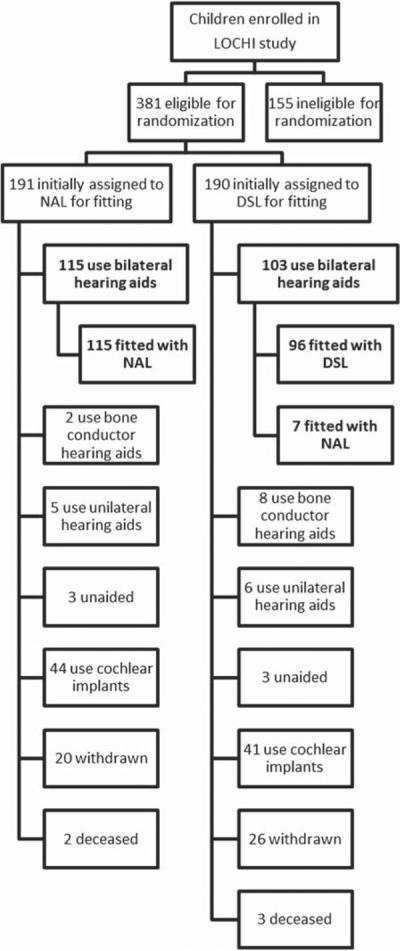
Enrolment and randomization of children participating in the current trial of prescription (in bold).
Table 1.
Demographic characteristics of children and their families
| Characteristics | NAL group (n = 122) | DSL group (n = 96) | Difference p value |
|---|---|---|---|
| Gender – Female no. (%) | 47 (39) | 42 (44) | p = 0.62 |
| Age at fitting (months) | p = 0.06 | ||
| Median | 6.3 | 4.8 | |
| Interquartile range | 3.2 to 20.9 | 2.9 to 10.7 | |
| Minimum to maximum | 1.4 to 36.0 | 1.4 to 33.6 | |
| Degree of hearing loss# – no. (%) | p = 0.22 | ||
| Moderate (40–60 dB) | 84 (69) | 72 (75) | |
| Severe (61–80 dB) | 28 (23) | 16 (17) | |
| Profound (> 80 dB) | 10 (8) | 8 (8) | |
| Additional disability – no. (%) | 22 (18) | 18 (19) | p = 0.95 |
| English used at home – no. (%) | 109 (89) | 89 (91) | p = 0.83 |
| Socio-economic status (decile) | p = 0.17 | ||
| Median | 6.8 | 7.4 | |
| Interquartile range | 5.0 to 9.0 | 6.0 to 9.0 | |
| Minimum to maximum | 1.0 to 10.0 | 1.0 to 10.0 | |
| Maternal education – no. (%) | p = 0.40 | ||
| ≤ 12 years of schooling | 45 (37) | 37 (39) | |
| Certificate or diploma | 25 (21) | 23 (24) | |
| ≥ University degree | 48 (39) | 32 (33) | |
| Intervention: Oral mode of communication – no. (%) | 96 (79) | 72 (75) | p = 0.71 |
| Intervention hours | p = 0.05 | ||
| Median | 92 | 116 | |
| Interquartile range | 28 to 124 | 58 to 136 |
Averaged hearing levels across 0.5 to 4 kHz in the better ear, expressed in terms of dB HL.
Figure 2 shows the distribution of four-frequency-average hearing loss (4FA, averaged across octave frequencies between 0.5 and 4 kHz) for children assigned to the NAL and the DSL groups. On average, neither the audiogram slope from 0.5 to 4 kHz nor the four frequency average (4FA, averaged across octave frequencies between 0.5 and 4 kHz) hearing level was significantly different between the two groups of children (Slope: F(1,434) = 0.29,p = 0.58; 4FA hearing level: F = 2.54, p = 0.11).
Figure 2.
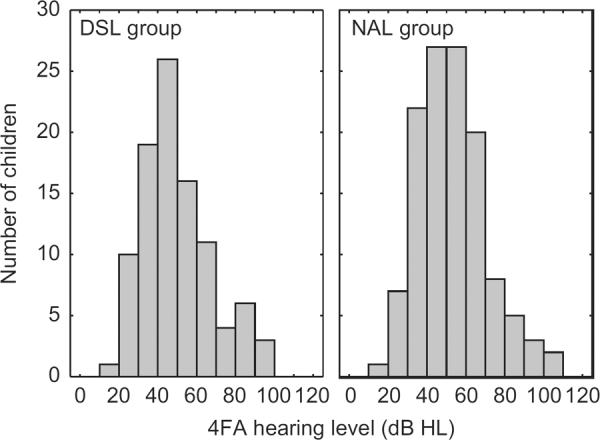
Distribution of four-frequency average hearing level (4FA, thresholds averaged across octave frequencies from 0.5 to 4 kHz) in the better ear for the DSL group (left panel) and the NAL group (right panel).
Based on an audiogram averaged across all children in the study, a snapshot of the differences between the gain-frequency responses prescribed by the NAL and the DSL procedures for children is captured in Figure 3. Whereas DSL v.4 and DSL m[i/o] prescribed gain-frequency responses that were comparable, NAL-NL2 prescribed steeper response slopes than its predecessor NAL-NL1. Overall, the DSL procedures prescribed more low-frequency gain than the NAL procedures, resulting in flatter response slopes. Compared to NAL-NL1, the DSL v.4 and DSL m[i/o] prescribed more gain at low and high frequencies over a range of input levels. Consequently, the prescribed overall gain is higher for the DSL than for the NAL procedures.
Figure 3.
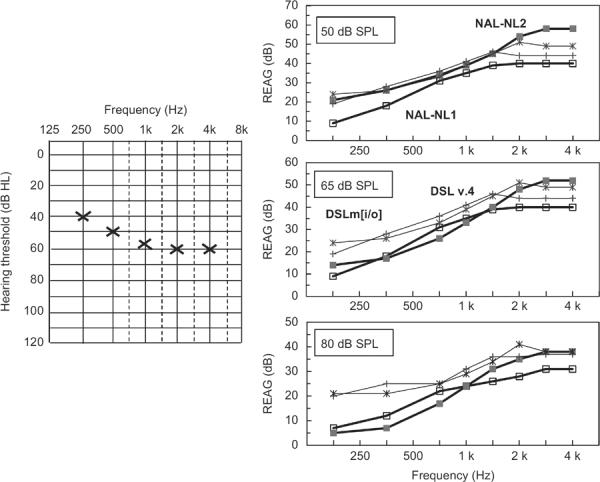
The left panel shows the averaged audiogram for all children in the study. The right panels show real-ear-aided gain (REAG) prescribed by NAL-NL1 (open squares), NAL-NL2 (filled squares), DSL v.4 (crosses), and DSL m[i/o] (asterisks) at low (50 dB SPL), mid (65 dB SPL) and high (80 dB SPL) input levels.
Hearing-aid fitting to targets
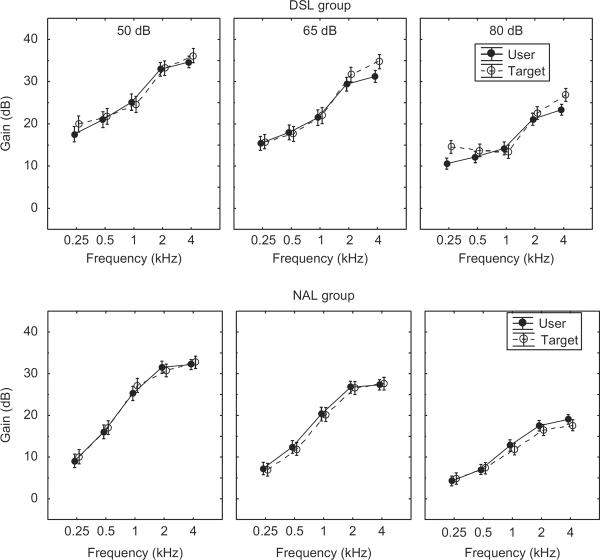
The hearing aid gain-frequency responses used by children at their evaluations at three years of age were measured within six months of the time of evaluation. Figure 4 shows the mean gains used in hearing aids for low (50 dB SPL), mid (65 dB SPL), and high (80 dB SPL) input levels in relation to prescriptive targets, separately for children assigned to the NAL and the DSL groups. Averaged over all children, the root-mean-square differences between achieved and target 4FA gains were less than 3 dB at low, mid, and high input levels.
Figure 4.
Mean gains for user settings (solid line with filled circles) and prescribed targets (broken line with open circles) as a function of frequency. Mean values for low input level (50 dB SPL), mid input level (65 dB SPL), and high input level (80 dB SPL) are shown. The top panels depict mean values for the DSL group, and the bottom panels depict mean values for the NAL group.
Tables 2 and 3 show the mean 4FA gains and frequency responses of hearing-aids at user settings, together with targets used for fitting. Absolute deviations from targets in terms of gains and frequency response slopes are shown in Tables 4 and 5 respectively. On average, prescribed frequency response slopes from 0.5 to 4 kHz were matched within 3 dB/octave.
Table 2.
Mean, standard deviation (SD), and range of gains in user device compared to targets used for fitting (DSL or NAL prescription, depending on assigned group), as well as targets prescribed by the NAL-NL2 and DSL m[i/o] formulae.
| Gain averaged between 0.5 and 4 kHz (4FA gain) |
||||||
|---|---|---|---|---|---|---|
| Level | User | Target | NAL-NL2 | DSL m[i/o] | ||
| DSL group | 50 | Mean | 28.4 | 28.9 | 26.7 | 29.6 |
| SD | 11.0 | 11.6 | 10.8 | 10.5 | ||
| Range | 5.5 to 57.5 | 5.5 to 64.8 | 7.3 to 56.5 | 9.5 to 59.3 | ||
| 65 | Mean | 25.0 | 26.5 | 20.7 | 26.8 | |
| SD | 10.9 | 12.1 | 10.5 | 11.7 | ||
| Range | 4.0 to 51.5 | 3.3 to 61.8 | 2.2 to 52.9 | 7.0 to 59.3 | ||
| 80 | Mean | 17.6 | 19.1 | 12.9 | 19.6 | |
| SD | 9.0 | 10.4 | 9.0 | 10.3 | ||
| Range | 2.0 to 40.3 | 1.5 to 49.0 | 0.7 to 43.7 | 4.0 to 48.8 | ||
| NAL group | 50 | Mean | 26.2 | 26.9 | 29.6 | 32.6 |
| SD | 10.9 | 11.7 | 10.8 | 10.4 | ||
| Range | 2.8 to 63.0 | 7.5 to 65.5 | 6.2 to 61.8 | 11.3 to 67.5 | ||
| 65 | Mean | 21.7 | 21.5 | 23.4 | 29.9 | |
| SD | 10.5 | 10.8 | 10.7 | 11.8 | ||
| Range | 2.0 to 59.5 | 4.0 to 61.3 | 5.3 to 59.6 | 8.5 to 67.5 | ||
| 80 | Mean | 14.2 | 13.3 | 15.0 | 22.3 | |
| SD | 8.9 | 9.3 | 9.6 | 10.6 | ||
| Range | 0.3 to 44.8 | 0.5 to 46.8 | 3.7 to 51.6 | 5.8 to 59.0 | ||
Table 3.
Mean, standard deviation (SD), and range of frequency response slopes in user devices compared to targets used for fitting (DSL or NAL prescription, depending on group assignment), as well as the NAL-NL2 and DSL m[i/o] prescriptions.
| Slope between 0.5 and 4 kHz (dB/octave) |
||||||
|---|---|---|---|---|---|---|
| Level | User | Target | NAL-NL2 | DSL m[i/o] | ||
| DSL group | 50 | Mean | 4.6 | 4.8 | 9.4 | 5.6 |
| SD | 3.3 | 3.7 | 2.8 | 3.4 | ||
| Range | −7.7 to 12.3 | −8.3 to 15.3 | −3.5 to 16.2 | −8.3 to 15.3 | ||
| 65 | Mean | 4.5 | 5.7 | 9.8 | 6.2 | |
| SD | 3.2 | 3.7 | 2.9 | 3.6 | ||
| Range | −8.7 to 13.3 | −8.0 to 16.7 | −3.1 to 18.9 | −8.0 to 16.7 | ||
| 80 | Mean | 3.8 | 4.42 | 7.6 | 4.8 | |
| SD | 2.8 | 3.16 | 2.7 | 3.2 | ||
| Range | −7.3 to 11.7 | −6.7 to 14.7 | −0.7 to 18.7 | −6.7 to 14.7 | ||
| NAL group | 50 | Mean | 5.4 | 5.2 | 9.2 | 5.0 |
| SD | 3.5 | 2.9 | 2.6 | 3.1 | ||
| Range | −7.7 to 12.0 | −2.7 to 11.3 | −0.7 to 15.5 | −5.3 to 14.3 | ||
| 65 | Mean | 5.1 | 5.3 | 9.7 | 5.58 | |
| SD | 3.2 | 3.0 | 2.7 | 3.43 | ||
| Range | −6.3 to 11.3 | −4.0 to 11.0 | −1.5 to 15.6 | −5.0 to 16.3 | ||
| 80 | Mean | 4.1 | 3.5 | 7.9 | 4.1 | |
| SD | 2.6 | 2.6 | 2.5 | 3.0 | ||
| Range | −3.3 to 10.0 | −6.3 to 9.7 | −1.0 to 15.4 | −4.0 to 13.7 | ||
Table 4.
Mean deviations of user four-frequency-average gain (4FA, gains averaged over 0.5, 1, 2, 4 kHz) from prescribed gains at low (50 dB SPL), mid (65 dB SPL) and high (80 dB SPL) input levels. Mean deviation of user maximum power output (MPO) from prescribed output is shown in the last column.
| User gain minus Target gain (dB) |
User minus Target MPO |
||||
|---|---|---|---|---|---|
| Low | Mid | High | MPO | ||
| DSL group | Mean | −0.5 | −1.5 | −1.4 | −0.3 |
| SD | 2.4 | 2.7 | 3.1 | 4.8 | |
| CI | −0.9 to −0.2 | −1.9 to −1.1 | −1.9 to −1.0 | −0.9 to 0.4 | |
| Range | −10.3 to 3.5 | 4.5 to 2.7 | −11.8 to 4.5 | −16.8 to 10.3 | |
| NAL group | Mean | −0.7 | 0.1 | 0.8 | −0.1 |
| SD | 2.7 | 2.0 | 2.3 | 4.1 | |
| CI | −1.0 to −0.4 | 0.1 to −0.1 | 0.5 to 1.0 | −0.6 to 0.4 | |
| Range | −11.3 to 5.3 | −8.8 to 6.3 | −12.3 to 6.8 | −22.3 to 10.3 | |
Table 5.
Mean deviations of user frequency response slope (averaged over 0.5 to 4 kHz, expressed in terms of dB/octave) from prescribed response slopes at low (50 dB SPL), mid (65 dB SPL), and high (80 dB SPL) input levels. Also shown are standard deviation (SD), confidence interval (CI) and range.
| User minus Target slope (dB/octave) |
||||
|---|---|---|---|---|
| Low | Mid | High | ||
| DSL group | Mean | −0.2 | −1.3 | −0.7 |
| SD | 2.3 | 2.3 | 1.9 | |
| CI | −0.6 to 0.1 | −1.6 to −1.0 | −0.9 to −0.4 | |
| Range | −9.7 to 3.7 | −10.0 to 2.3 | −8.3 to 2.7 | |
| NAL group | Mean | 0.2 | −0.3 | 0.6 |
| SD | 1.9 | 1.5 | 1.7 | |
| CI | −0.1 to 0.4 | −0.5 to −0.1 | 0.3 to 0.8 | |
| Range | −6.3 to 8.3 | −5.7 to 7.0 | −5.0 to 8.0 | |
Effect of prescription and other factors on outcomes
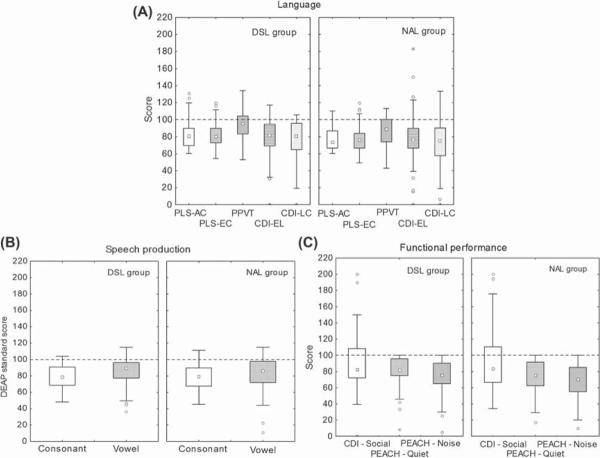
Figure 5 shows the median scores for each outcomes measure, together with the quartile and range of scores. Ratings provided by parents indicated that on average, children used their hearing devices for more than 75% of their waking hours, and the incidence for loudness discomfort was very low. Separate analysis of variance revealed that there were no significant differences between the two prescription groups for usage (F(1,117) = 0.643, p = 0.4) and for loudness discomfort (F = 0.013, p = 0.9).
Figure 5.
Scores for developmental outcomes grouped according to Language, Speech production, and Functional performance. In each group, the left panel shows scores for the DSL group, and the right panel shows scores for the NAL group. The Language scores include PLS-4 Auditory comprehension (AC) subscale, PLS-4 Expressive communication (EC) subscale, PPVT, CDI Expressive language (EL) subscale, and CDI Language comprehension (LC) subscale. The Speech production group include DEAP: Consonant score and DEAP: Vowel score. The Functional performance group include CDI: Social subscale, PEACH: Quiet subscale, and PEACH: Noise subscale. Values are expressed as the median (square in the middle of each box), with the quartiles (top and bottom of the box), and range (I bar), with outof-range observations (i.e. > 1.5 times the interquartile range beyond the quartile) shown as circles, and extremes shown as asterisks.
A primary interest in this study was to determine the influence of prescription and a range of other factors on the language, speech and functional outcomes of children at three years of age. Using principal components analysis, a Total Language component score was created, based on a linear combination of scores obtained from all measures of language (PLS-4 Auditory comprehension, PLS-4 Expressive communication, PPVT receptive vocabulary, CDI-Language comprehension, and CDI-Expressive language). In a similar manner, a speech production component score was created from three measures of speech production (Speech intelligibility rating, DEAP-vowels and DEAP-consonants); and a Functional performance component score from measures of social and functional performance (CDI-social scale, PEACH-quiet and PEACH-noise measures). Table 6 shows the factor loadings of each measure used in separate principal component analyses on each of the domains of language, speech, and functional performance. The principal components scores accounted for 68% of the variance in the total language measures (item communalities ranging from 0.68 to 0.90), 65% of the variance in speech production measures (item communalities ranging from 0.65 to 0.90), and 71% of the functional performance measures (item communalities ranging from 0.64 to 0.92).
Table 6.
Factor loadings of measures used in separate principal component analyses on each of the domains of language, speech production, and functional performance.
| Principle component | Measure | Factor loading |
|---|---|---|
| Total language | PLS-4 Auditory comprehension | −0.878 |
| PLS-4 Expressive communication | −0.902 | |
| PPVT | −0.675 | |
| CDI: Expressive language | −0.799 | |
| CDI: Language comprehension | −0.841 | |
| Speech | Speech intelligibility rating | −0.646 |
| DEAP: consonants | −0.895 | |
| DEAP: vowels | −0.851 | |
| Functional performance | CDI: Social subscale | −0.638 |
| PEACH: Quiet subscale | −0.935 | |
| PEACH: Noise subscale | −0.916 |
General linear regression analysis was performed with each principal component score as a dependent variable and 10 predictors relating to child, family, and intervention characteristics as independent variables. The categorical variables included: prescription group (DSL or NAL); gender (male or female); additional disability (presence or absence); and communication mode in intervention (oral or combined mode). The six continuous variables included: age at first fitting; 4FA hearing thresholds in the better ear; maternal education; socio-economic status (SEIFA in decile); hours of educational intervention (from enrolment to three years of age); and deviation of user 4FA gains from the average of NAL-NL2 and DSL m[i/o] 4FA gains at low input level. Table 7 shows the Beta values for each component score.
Table 7.
Multivariate linear regression analyses of principal component scores of Language, Speech production, and Functional performance with respect to potential predictors. The reference level of effect for 'Gender' was 'Male', 'Prescription' was 'DSL', 'Additional disability' was 'Absent', and 'Communication mode in intervention' was 'Oral'. Values significant at 5% level were marked by asterisks.
| Language |
Speech production |
Functional performance |
||||
|---|---|---|---|---|---|---|
| Coefficient (95% CI@) | p | Coefficient (95% CI) | p | Coefficient (95% CI) | p | |
| 4FA hearing level in better ear | −0.17 (−0.31 to −0.03) | 0.01* | −0.02 (−0.18 to 0.14) | 0.77 | −0.09 (−0.23 to 0.051) | 0.21 |
| Additional disability | 0.11 (−0.04 to 0.26) | 0.14 | −0.01 (−0.19 to 0.16) | 0.87 | 0.35 (0.19 to 0.51) | < 0.001* |
| Age at fitting | −0.03 (−0.17 to 0.11) | 0.69 | 0.07 (−0.09 to 0.23) | 0.38 | −0.14 (−0.28 to 0.005) | 0.06 |
| Gender | 0.08 (−0.11 to 0.26) | 0.42 | 0.05 (−0.16 to 0.27) | 0.64 | −0.03 (−0.23 to 0.16) | 0.72 |
| Prescription group | 0.21 (−0.01 to 0.42) | 0.06 | −0.02 (−0.27 to 0.23) | 0.88 | 0.14 (−0.08 to 0.36) | 0.22 |
| Maternal education | −0.23 (−0.36 to −0.09) | < 0.001* | −0.25 (−0.40 to −0.09) | 0.002 | −0.20 (−0.33 to −0.06) | 0.005* |
| Socio-economic status | 0.15 (0.02 to 0.28) | 0.03* | 0.02 (−0.13 to 0.17) | 0.80 | 0.009 (−0.13 to 0.15) | 0.90 |
| Communication mode in intervention | 0.21 (0.06 to 0.36) | 0.008* | 0.003 (−0.18 to 0.18) | 0.97 | 0.29 (0.13 to 0.46) | < 0.001* |
| Hours of intervention | −0.17 (−0.32 to −0.03) | 0.02* | 0.009 (−0.16 to 0.18) | 0.92 | −0.13 (−0.28 to 0.02) | 0.09 |
| User 4FA gain minus Averaged NAL-NL2 and DSL m[i/o] gain at low input level | 0.08 (−0.08 to 0.24) | 0.31 | 0.11 (−0.07 to 0.29) | 0.23 | −0.005 (−0.17 to 0.16) | 0.95 |
| Language component score | - | - | 0.70 (0.56 to 0.84) | < 0.0001* | 0.38 (0.23 to 0.52) | < 0.0001* |
denotes confidence interval.
In the regression analysis examining the language component score, the baseline predictors accounted for 27% of the variation in scores (Table 7). Five factors were associated with language scores at the 5% level of significance. Language component scores were higher for children who received early intervention using an oral only mode of communication than for those who used a mode that combined oral and manual methods. Scores were higher for children from higher socio-economic backgrounds than those from lower socio-economic backgrounds. Also, scores were higher for children with less severe hearing loss, and higher for children whose mothers had a university degree compared to children whose mothers had completed ≤ 12 years of schooling. More hours of intervention were associated with lower language component scores.
In the analysis examining the speech production component score, the baseline predictors accounted for less than 1% of the total variation. A subsequent analysis added language component score as a predictor variable, based on the premise that language ability has been linked to speech production skills in previous studies (Blamey et al, 2001). The predictors accounted for 37% of the variation, with language being the only factor associated with the speech production component score at the 5% significance level.
In examining functional performance, the baseline predictors accounted for 22% of the variation in component scores. Three of the predictors were associated with functional scores at 5% significance level. Scores were higher for children who did not have additional disability than those who did; and higher for those who used oral-only mode of communication in early intervention than those who used a combination of oral and manual modes. Functional scores were also higher for those whose mothers completed university education than for those who completed 12 years or less schooling. In a subsequent analysis that included language component score as a predictor (based on the premise that language skills may be associated with functional performance in real life (Duchesne et al, 2009)), the predictors accounted for 32% of the total variation in functional scores. Language ability, presence of additional disability, and oral mode of communication were associated with functional performance scores at 5% significance level.
A secondary aim of this study was to determine whether early functional performance scores were predictive of outcomes at three years of age. PEACH data were available from parents of 82 children who completed the questionnaire between 6 and 12 months after their children received initial amplification (mean age of children: 13.5 months, SD: 5.1, Range: 6 to 25 months). The regression analysis used seven predictors, including age at fitting, 4FA hearing level, socio-economic status, maternal education, prescription for hearing-aid fitting, presence or absence of additional disability, and early PEACH score (see Table 8).
Table 8.
Multivariate linear regression analyses of language, speech production and functional performance component scores with respect to potential baseline predictors and early functional performance status. The reference level of effect for Additional disability was 'Absent', and 'Prescription level' was 'DSL'. Values significant at 5% level are marked by asterisks.
| Language |
Speech production |
Functional performance |
||||
|---|---|---|---|---|---|---|
| Coefficient (95% CI@) | p | Coefficient (95% CI) | p | Coefficient (95% CI) | p | |
| 4FA hearing level in better ear | −0.20 (−0.37 to 0.02) | 0.03* | −0.11 (−0.33 to 0.11) | 0.33 | −0.12 (−0.31 to 0.07) | 0.22 |
| Additional disability | 0.33 (0.15 to 0.51) | < 0.001* | 0.10 (−0.12 to 0.32) | 0.38 | 0.36 (0.16 to 0.55) | < 0.001* |
| Age at fitting | 0.10 (−0.08 to 0.27) | 0.28 | 0.14 (−0.08 to 0.36) | 0.20 | 0.02 (−0.18 to 0.22) | 0.84 |
| Prescription group | 0.15 (−0.02 to 0.32) | 0.08 | 0.11 (−0.10 to 0.33) | 0.38 | 0.01 (−0.23 to 0.25) | 0.93 |
| Socio-economic status | 0.18 (−0.006 to 0.37) | 0.06 | 0.05 (−0.19 to 0.29) | 0.68 | −0.07 (−0.28 to 0.14) | 0.49 |
| Maternal education | −0.32 (−0.51 to 0.14) | < 0.001* | −0.18 (−0.42 to 0.06) | 0.13 | −0.21 (−0.41 to −0.002) | 0.04* |
| PEACH: Early functional status | 0.20 (0.02 to 0.38) | 0.03* | 0.22 (−0.004 to 0.45) | 0.05 | 0.27 (0.07 to 0.47) | 0.008* |
denotes confidence interval.
In examining language scores, the predictors accounted for 44% of the total variance. Table 8 shows that four factors, including hearing level, maternal education, additional needs, and early functional performance (early PEACH scores) were associated with language skills at the 5% level of significance. In examining speech production component scores, the predictors accounted for 10% of total variation. In examining functional performance component scores, the predictors accounted for 31% of the total variation. Higher maternal education, higher early PEACH scores, and the absence of additional disability were associated with higher functional performance component scores at three years of age at the 5% level of significance.
If early PEACH scores were the only known variable for predicting performance outcomes at three years, they accounted for 9% of the total variation in language component scores (p = 0.004),5% of the variation in speech production (p = 0.02), and 14% of the variation in functional scores (p = 0.003).
Discussion
Factors affecting outcomes
On average, children's performance was slightly poorer than 1 SD below the normative mean for language, speech, and functional performance outcomes. The baseline characteristics for the 122 children who were fitted with the NAL prescription were, on average, similar to those of the 96 children who were fitted with the DSL prescription (Table 1). Analysis of the outcomes of children at three years of age did not reveal a significant difference in language, speech production, and functional performance scores favouring one prescription over the other.
The choice of prescription method, nonetheless, resulted in marked differences in real-ear-gain. Estimated loudness from the application of the DSL procedures (including DSL v4.1 and DSL m[i/o]) in hearing aids was, on average, higher than that for the NAL-NL1 procedure by a factor of 2 when the input level was medium or high (Ching et al, this issue). Even though ratings by parents on loudness discomfort or device usage in the present study did not reveal an effect of prescription, such effects may be important when children are old enough to provide subjective ratings (Ching et al, 2010) and when they function in a range of real-world environments wider than the current ones.
The impact of prescription choice on predicted speech intelligibility was also quantified by using the speech intelligibility index model (ANSI, 1997) with an allowance for hearing loss desensitization that was empirically derived (Ching et al, 2011) and adopted in the derivation of the NAL-NL2 procedure (Dillon et al, 2011). It may be expected that higher audibility can be achieved by the prescription that provides higher gains, but the effectiveness of the audible signal for speech intelligibility would be reduced by distortions arising from listening at high SPLs and the decrease of a listener's ability to extract information from an audible signal as hearing loss increases (see Ching et al, this issue). Briefly, the modelling revealed that predicted speech intelligibility was higher for DSL than for NAL at low input level, similar between prescriptions at medium input level, but higher for NAL than for DSL at high input level. Nonetheless, the overall effect size was small. Consistent with that finding, the present analysis shows that deviation of user gains from targets prescribed by the updated versions of the two prescriptions was not related to any of the measured outcomes at the 5% significance level.
The use of an aural/oral mode of communication in intervention was associated with better outcomes in language development and functional performance, but not in speech production. Because there were changes in communication mode for some children during the first few years of intervention, the use of an aural/oral mode at three years of age might be an outcome rather than a predictor.
The factors that were found to be significantly associated with language and functional performance were socio-economic status and maternal education. This finding is consistent with the literature on development of children with normal hearing. Social disadvantage has been linked to poorer expressive and receptive language in normal-hearing children at four years of age (Reilly et al, 2010), speech production at three years of age (Dollaghan et al, 1999), and academic underachievement for school-aged children (Hart & Risley, 1995). Possibly, social disadvantage and maternal educational level influence the quantity and quality of language to which children are exposed in the home environment (Bornstein et al, 1998; Hoff-Ginsburg, 1998). Maternal (parental) educational level is also linked to parents' academic competence, their attitudes toward education (Fuligni, 1997; Brody & Flor, 1998), as well as their knowledge and beliefs about child development (Benasich & Brooks-Gunn, 1996; Tamis-LeMonda et al, 1998). Although it is not possible within the scope of the present study to pinpoint the reasons for the observed effects of socio-economic status and maternal education on language development of children with hearing impairment, it may be hypothesized that maternal education may have exerted its influence on child outcomes through its association with characteristics of communicative style and child-directed language (Pine et al, 1997; Haden, 1998). Understanding the relationships among particular socio-demographic variables, especially modifiable factors, and specific measures of early outcomes is an important area of research for children with hearing loss, and is a focus of the main LOCHI study.
Importance of early functional evaluation
Early functional level (as measured using the PEACH scale during the first year of amplification) together with degree of hearing loss, prescription method, presence or absence of additional needs, socio-economic status, and maternal education explained 44% of variation in language performance, and 31% of variation in functional performance scores for hearing-impaired children by three years of age. Early PEACH scores uniquely explained 6% of the total variation in language, 4% of the variation in speech production, and 9% of the variation in functional scores at three years; after allowing for the effects of all other predictors on component scores. If early PEACH scores were the only predictor variable, it accounted for 9% of the total variation in language, 5% of the total variation in speech production, and 14% of the variation in functional performance at three years of age. Compared to a study of normal-hearing children which revealed that maternal language level together with 10 risk factors accounted for only 4% to 7% of variation in children's language at two years of age (Reilly et al, 2007), the significance of the early PEACH scores in predicting language development by three years of age should not be underestimated. Early identification of hearing-impaired children who may be at risk for language development allows additional intervention to be implemented at an early age. Because the PEACH scale is less tied to a single socio-demographic context than is a standardized language measure, it can be used for culturally diverse populations. The PEACH scale is applicable for infants and young children, has published normative data with information on reliability and critical differences (Ching & Hill, 2007), and has been found to be significantly correlated with objective measures of audibility based on auditory evoked cortical responses in infants (Golding et al, 2007), and standardized measures of language ability in young children (Ching et al, 2010).
The strengths of the present study include its randomized controlled design that is community-based, its cohort of newly-identified children with hearing loss, its prospective measurements of a range of outcomes including language, speech, and functional performance, and its inclusion of standardized tests administered directly to participants as well as parent reports. Unlike previous studies on outcomes of children with hearing loss in which information about adequacy of hearing-aid fitting is typically lacking (Wake et al, 2004; Kennedy et al, 2006; Korver et al, 2010), the present study included comprehensive information about hearing-aid fitting and hearing threshold levels, thereby allowing for a more accurate estimation of the effects of amplification characteristics on developmentaloutcomes.
Summary of present findings
There was no significant association between choice of hearing-aid prescription and variance in children's speech production, language, and functional performance at three years of age.
Children's development of language and functional performance, by three years of age, is susceptible to influences of social disadvantage and maternal educational level. On average, performance was slightly poorer than 1 SD below normative mean.
Early functional level explained a significant proportion of variation in language, speech, and functional development by three years of age.
Our current findings cannot be generalized to children at other age groups. It remains to be seen whether relations between prescription choice and later development that were not discernible in the study participants at three years of age might emerge at later ages. Data collection for some of the participants at five years is currently under way, and we have also begun testing at nine years of age using additional measures of literacy and related skills.
Acknowledgements
We gratefully thank all the children, their families, and their teachers for participation in this study. We are also indebted to the many persons who served as clinicians for the study subjects, or assisted in other clinical or administrative capacities at Australian Hearing, Hear and Say Centre, the Shepherd Centre, and the Sydney Cochlear Implant Centre. Thanks are due to Nicole Mahler-Thompson, Julia Orsini, Helen-Louise Usher, Jo Ashdown, Cassandra Cook, Karen McGhie, Sonya Cornick, Gillian Zavos, Emma van Wanrooy, Leanne Skinner, and Robyn Massie for their assistance in data collection. We acknowledge the financial support of the Commonwealth of Australia through the establishment of the HEARing CRC and the Cooperative Research Centres Program. The project described was supported by Award Number R01DC008080 from the National Institute On Deafness And Other Communication Disorders. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute On Deafness And Other Communication Disorders or the National Institutes of Health. Support for this research was also provided by New South Wales Department of Health, Australia, Phonak Ltd., and the Oticon Foundation.
Abbreviations
- 4FA
Four-frequency average, across 0.5, 1, 2, and 4 kHz
- AH
Australian Hearing
- CDI
Child Development Inventory
- DEAP
Diagnostic Evaluation of Articulation and Phonology
- DSL
Desired Sensation Level
- DSL m[i/o]
Desired Sensation Level multi-stage input-output algorithm
- DSL v.4.1
Desired Sensation Level procedure version 4.1
- HTL
Hearing threshold level
- LOCHI
Longitudinal Outcomes of Children with Hearing Impairment study
- NAL
National Acoustic Laboratories
- NAL-NL1
National Acoustic Laboratories' hearing aid prescription for non-linear hearing aids, version 1
- NAL-NL2
National Acoustic Laboratories' hearing aid prescription for non-linear hearing aids, version 2
- PEACH
Parents' Evaluation of Aural/oral performance of CHildren
- PLS-4
Preschool Language Scale, 4th edition
- PPVT
Peabody Picture Vocabulary Test
- RECD
Real-ear-to-coupler difference
- SII
Speech Intelligibility Index
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Australian Bureau of Statistics . Socio-Economic Indexes for Areas (SEIFA) 2006: Technical paper. Brian Pink; Canberra: 2008. [Google Scholar]
- Benasich AA, Brooks-Gunn J. Maternal attitudes and knowledge of child-rearing: Associations with family and child outcomes. Child Dev. 1996;67:1186–1205. [PubMed] [Google Scholar]
- Blamey PJ, Sarant JZ, Paatsch LE, Barry JG, Bow CP, et al. Relationships among speech perception, production, language, hearing loss, and age in children with impaired hearing. J Speech Lang Hear Res. 2001;44:264–285. doi: 10.1044/1092-4388(2001/022). [DOI] [PubMed] [Google Scholar]
- Bornstein MH, Haynes MO, Painter KM. Sources of child vocabulary competence: A multivariate model. J Child Lang. 1998;25:367–393. doi: 10.1017/s0305000998003456. [DOI] [PubMed] [Google Scholar]
- Brody GH, Flor DL. Maternal resources, parenting practives, and child competence in rural, single-parent African American families. Child Dev. 1998;69:803–816. [PubMed] [Google Scholar]
- Byrne D, Ching TYC. Optimizing amplification for hearing-impaired children: I. Issues and procedures. Australian Journal of Education of the Deaf. 1997;3:21–28. [Google Scholar]
- Byrne D, Dillon H, Ching TYC, Katsch R, Keidser G. NAL-NL1 procedure for fitting nonlinear hearing aids: Characteristics and comparisons with other procedures. J Am Acad Audiol. 2001;12:37–51. [PubMed] [Google Scholar]
- Ching T, Newall P, Wigney D. Frequency response and gain requirements of severely and profoundly hearing-impaired children. The Australian Journal of Audiology. 1996;18:99–101. [Google Scholar]
- Ching TYC, Crowe K, Martin V, Day J, Mahler N, et al. Language development and everyday functioning of children with hearing loss assessed at three years of age. Int J Speech Lang Pathol. 2010;12:124–131. doi: 10.3109/17549500903577022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching TYC, Dillon H, Byrne D. Speech recognition of hearing-impaired listeners: Predictions from audibility and the limited role of high-frequency amplification. J Acoust Soc Am. 1998;103:1128–1140. doi: 10.1121/1.421224. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Dillon H, Lockhart F, van Wanrooy E, Flax M. Audibility and speech intelligibility revisited: implications for amplification. In: Dau T, Dalsgaard JC, Jepsen ML, Poulsen T, editors. International Symposium on Auditory and Audiological Research. The Danavox Jubilee Foundation; Denmark: 2012. pp. 11–19. [Google Scholar]
- Ching TYC, Hill M. The Parent's Evaluation of Aural/Oral Performance of Children (PEACH) Scale: Normative data. J Am Acad Audiol. 2007;18:220–235. doi: 10.3766/jaaa.18.3.4. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Johnson EE, Hou S, Dillon H, Zhang V, et al. A comparison of NAL and DSL prescriptive methods for paediatric hearing-aid fitting: Estimates of loudness and speech intelligibility. Int J Audiol. doi: 10.3109/14992027.2013.765041. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching TYC, Scollie SD, Dillon H, Seewald R. Across-over, double-blind comparison of the NAL-NL1 and the DSL v4.1 prescriptions for children with mild to moderately severe hearing loss. Int J Audiol. 2010;49:S4–S15. doi: 10.3109/14992020903148020. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Scollie SD, Dillon H, Seewald R, Britton L, et al. Prescribed real-ear and achieved real-life differences in children's hearing aids adjusted according to the NAL-NL1 and the DSL v.4.1 prescriptions. Int J Audiol. 2010;49:S16–S25. doi: 10.3109/14992020903082096. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Scollie SD, Dillon H, Seewald R, Britton L, et al. Evaluation of the NAL-NL1 and the DSL v.4.1 prescriptions for children: Paired-comparison intelligibility judgments, and functional performance ratings. Int J Audiol. 2010;49:S35–48. doi: 10.3109/14992020903095791. [DOI] [PubMed] [Google Scholar]
- Coninx F, Weichbold V, Tsiakpini L, Autrique E, Bescond GE. Validation of the LittlEARs auditory questionnaire in children with normal hearing. Int J Pediatr Otorhinolaryngol. 2009;73:1761–1768. doi: 10.1016/j.ijporl.2009.09.036. [DOI] [PubMed] [Google Scholar]
- Dillon H, Keidser G, Ching TYC, Flax M, Brewer S. The NAL-NL2 prescription procedure. Phonak Focus. 2011:1–10. doi: 10.4081/audiores.2011.e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodd B, Hua Z, Crosbie S, Holm A, Ozanne A. Diagnostic Evaluation of Articulation and Phonology. Psychological Corporation; London: 2002. [Google Scholar]
- Dollaghan CA, Campbell TF, Paradise JL, Feldman HM, Janosky JE, et al. Maternal education and measures of early speech and language. J Speech Lang Hear Res. 1999;42:1432. doi: 10.1044/jslhr.4206.1432. [DOI] [PubMed] [Google Scholar]
- Duchesne L, Sutton A, Bergeron F. Language achievement in children who received cochlear implants between one and two years of age: Group trends and individual patterns. J Deaf Stud Deaf Educ. 2009;14:465–485. doi: 10.1093/deafed/enp010. [DOI] [PubMed] [Google Scholar]
- Dunn LM, Dunn LM. Peabody Picture Vocabulary Test. 3rd edition American Guidance Services; Circle Pines, USA: 1997. [Google Scholar]
- Dunn LM, Dunn LM. Peabody Picture Vocabulary Test. 4th edition Pearson Assessments; Minneapolis, USA: 2007. [Google Scholar]
- Fuligni AJ. The academic achievement of adolescents from immigrant families: The roles of family background, attitudes, and behavior. Child Dev. 1997;68:351–363. doi: 10.1111/j.1467-8624.1997.tb01944.x. [DOI] [PubMed] [Google Scholar]
- Golding M, Pearce W, Seymour J, Cooper A, Ching T, et al. The relationship between obligatory cortical auditory evoked potentials (CAEPs) and functional measures in young infants. J Am Acad Audiol. 2007;18:117–125. doi: 10.3766/jaaa.18.2.4. [DOI] [PubMed] [Google Scholar]
- Haden CA. Reminiscing with different children: Relating maternal stylistic consistency and sibling similarity in talk about the past. Dev Psychol. 1998;34:99–114. doi: 10.1037/0012-1649.34.1.99. [DOI] [PubMed] [Google Scholar]
- Hart B, Risley T. Meaningful Differences in Everyday Parenting and Intellectual Development in Young American Children. Brookes; Baltimore, USA: 1995. [Google Scholar]
- Hoff-Ginsburg E. The relation of birth order and socioeconomic status to children's langauge experience and language development. App Psycholinguist. 1998;19:603–629. [Google Scholar]
- Ireton H. Child Development Inventory. Child Development Review; Minneapolis: 2005. [Google Scholar]
- Jenstad LM, Bagatto MP, Seewald RC, Scollie SD, Cornelisse LE, et al. Evaluation of the Desired Sensation Level [Input/Output] algorithm for adults with hearing loss: The acceptable range for amplified conversational speech. Ear Hear. 2007;28:793–811. doi: 10.1097/AUD.0b013e318157670a. [DOI] [PubMed] [Google Scholar]
- Jenstad LM, Seewald R, Cornelisse LE, Shantz J. Comparison of linear gain and wide dynamic range compression hearing aid circuits: Aided speech perception measures. Ear Hear. 1999;19:117–126. doi: 10.1097/00003446-199904000-00003. [DOI] [PubMed] [Google Scholar]
- Jenstad LM, Seewald R, Cornelisse LE, Shantz J. Comparison of linear gain and wide dynamic range compression hearing aid circuits: Aided loudness measures. Ear Hear. 2000;21:32–44. doi: 10.1097/00003446-200002000-00007. [DOI] [PubMed] [Google Scholar]
- Johnson EE, Dillon H. A comparison of gain for adults from generic hearing-aid prescriptive methods: Impacts on predicted loudness, frequency bandwidth, and speech intelligibility. J Am Acad Audiol. 2011;22:1–19. doi: 10.3766/jaaa.22.7.5. [DOI] [PubMed] [Google Scholar]
- Kennedy CR, McCann DC, Campbell MJ, Law CM, Mullee M, et al. Language ability after early detection of permanent childhood hearing impairment. N Engl J Med. 2006;354:2131–2141. doi: 10.1056/NEJMoa054915. [DOI] [PubMed] [Google Scholar]
- King AM. The national protocol for paediatric amplification in Australia. Int J Audiol. 2010;49:S64–S69. doi: 10.3109/14992020903329422. [DOI] [PubMed] [Google Scholar]
- Korver AMH, Konings S, Dekker FW, Beers M, Wever CC, et al. Newborn hearing screening vs. later hearing screening and developmental outcomes in children with permanent childhood hearing impairment. J Am Med Assoc. 2010;304:1701–1708. doi: 10.1001/jama.2010.1501. [DOI] [PubMed] [Google Scholar]
- Moodie KS, Seewald R, Sinclair ST. Procedure for predicting real ear hearing-aid performance in young children. Am J Audiol. 1994;3:23–31. [Google Scholar]
- Nelson HD, Nygren P, Walker M, Panoscha R. Screening for speech and language delay in preschool children: Systematic evidence review for the US Preventive Services Task Force. Pediatrics. 2006;117:e298–e319. doi: 10.1542/peds.2005-1467. [DOI] [PubMed] [Google Scholar]
- Pine JM, Lieven EV, Rowland CF. Stylistic variation at the `single-word' stage: Relations between maternal speech characteristics and children's vocabulary composition and usage. Child Dev. 1997;68:807–819. doi: 10.1111/j.1467-8624.1997.tb01963.x. [DOI] [PubMed] [Google Scholar]
- Quar TK, Ching TYC, Siti ZSM, Newall P. The parents' evaluation of aural/oral performance of children (PEACH) scale in the Malay language: Data of normal-hearing children. Int J Audiol. 2012;51:326–333. doi: 10.3109/14992027.2011.637079. [DOI] [PubMed] [Google Scholar]
- Reilly S, Wake M, Bavin E, Prior M, Williams J, et al. Predicting language at two years of age: A prospective community study. Pediatrics. 2007;120:e1441–e1449. doi: 10.1542/peds.2007-0045. [DOI] [PubMed] [Google Scholar]
- Reilly S, Wake M, Ukoumunne OC, Bavin E, Prior M, et al. Predicting language outcomes at four years of age: Findings from early language in Victoria study. Pediatrics. 2010;126:e1530–e1537. doi: 10.1542/peds.2010-0254. [DOI] [PubMed] [Google Scholar]
- Scollie S, Ching TYC, Seewald R, Dillon H, Britton L, et al. Evaluation of the NAL-NL1 and DSL v4.1 prescriptions for children: Preference in real world use. Int J Audiol. 2010;49:S49–S63. doi: 10.3109/14992020903148038. [DOI] [PubMed] [Google Scholar]
- Scollie S, Seewald R, Cornelisse LE, Moodie S, Bagatto M, et al. The Desired Sensation Level Multistage Input/Output Algorithm. Trends in Amplification. 2005;9:159–197. doi: 10.1177/108471380500900403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scollie S, Seewald R, Moodie KS, Dekok K. Preferred listening levels of children who use hearing aids: Comparison to prescriptive targets. J Am Acad Audiol. 2000;11:230–238. [PubMed] [Google Scholar]
- Scollie SD, Ching TYC, Seewald RC, Dillon H, Britton L, et al. Children's speech perception and loudness ratings when fitted with hearing aids using the DSL v.4.1 and the NAL-NL1 prescriptions. Int J Audiol. 2010;49:S26–S34. doi: 10.3109/14992020903121159. [DOI] [PubMed] [Google Scholar]
- Seewald R, Cornelisse LE, Ramji KV. Users' manual. University of Western Ontario Hearing Health Care Research Unit; London, Ontario: 1997. DSL v4.1 for Windows: A software implementation of the Desired Sensation Level (DSL[i/o]) method for fitting linear gain and wide-dynamic-range compression hearing instruments. [Google Scholar]
- Seewald RC, Moodie KS, Sinclair ST, Scollie SD. Predictive validity of a procedure for pediatric hearing instrument fitting. Am J Audiol. 1999;8:10. doi: 10.1044/1059-0889(1999/017). [DOI] [PubMed] [Google Scholar]
- Tamis-LeMonda CS, Chen LA, Bornstein MH. Mothers' knowledge about children's play and language development: Short-term stability and interrelations. Dev Psychol. 1998;34:115–124. doi: 10.1037/0012-1649.34.1.115. [DOI] [PubMed] [Google Scholar]
- Wake M, Hughes EK, Poulakis Z, Collins C, Rickards FW. Outcomes of children with mild-profound congenital hearing loss at 7 to 8 years: A population study. Ear Hear. 2004;25:1–8. doi: 10.1097/01.AUD.0000111262.12219.2F. [DOI] [PubMed] [Google Scholar]
- Weichbold V, Anderson I, D'Haese PS. Validation of three adaptations of the Meaningful Auditory Integration Scale (MAIS) to German, English and Polish. Int J Audiol. 2004;43:156–161. doi: 10.1080/14992020400050021. [DOI] [PubMed] [Google Scholar]
- Zimmerman-Phillipps S, Osberger MJ, Robbins JM. Infant-Toddler: Meaningful Auditory Integration Scale (IT-MAIS) In: Eastabrooks W, editor. Cochlear Implants for Kids. AG Bell Association for the Deaf; Washington DC: 1998. [Google Scholar]
- Zimmerman I, Steiner VG, Pond RE. Preschool Language Scale. 4th edition The Psychological Corporation; San Antonio: 2002. [Google Scholar]