Abstract
Purpose
To describe our initial experience with the second-generation Single Port Instrument Delivery Extended Reach (SPIDER) laparoendoscopic single-site surgical system in a porcine model.
Materials and Methods
In four swine weighing approximately 32 to 35 kg, five nephrectomies, four adrenalectomies, three pyeloplasties, and three partial cystectomies and closures were performed by a single surgeon. The swine were placed in the lateral flank position under general anesthesia. The SPIDER surgical system was introduced through a single incision and the various urological procures were performed by use of flexible instrumentation.
Results
All five nephrectomies, four adrenalectomies, three pyeloplasties, and three partial cystectomies and closures were performed successfully without additional skin incisions. The mean time to set up the SPIDER platform was 3.5 minutes. The mean operative time for the right and left nephrectomies was 45.4 minutes and 47.8 minutes, respectively. The mean operative time for the right and left adrenalectomies was 37.6 minutes and 35.4 minutes, respectively. The mean operative time for the pyeloplasties for one right and two left ureters was 45.6 minutes and 47.3 minutes, respectively. The mean operative time for the partial cystectomies and closures was 18.6 minutes. There were no noticeable intraoperative complications except for minimal urine leakage in the first pyeloplasty.
Conclusions
In this initial pilot evaluation, the second-generation SPIDER surgical system offered intuitive instrument maneuverability and restored triangulation. However, retraction was challenging because of the lack of strength and the limited ability for precise manipulation of the tip. Future refinements of the technology and prospective studies are needed to optimize the application of this technology in urology.
Keywords: Laparoscopy, Robotics, Urologic surgical procedures
INTRODUCTION
Recent advancements in laparoscopic instrumentation and continued efforts to further minimize the nature of minimally invasive access for laparoscopic procedures have led to the emergence of new surgical approaches, such as natural orifice transluminal endoscopic surgery (NOTES) and laparoendoscopic single-site surgery (LESS). NOTES involves diagnostic or therapeutic interventions being performed via existing natural orifices of the human body. Despite the promising initial report of a transvaginal laparoscopic nephrectomy in a porcine model by Gettman et al. [1] in 2002, the many challenges associated with NOTES, such as suboptimal instrumentation, instrument clashing, disoriented view, and a steep learning curve, have limited its application in humans. LESS represents another approach that attempts to optimize access during laparoscopic procedures. LESS is characterized by attempting to introduce all necessary instruments and perform surgery through a single small incision [2]. LESS is based on the concept that by reducing abdominal ports, port-related morbidity is reduced for a better cosmetic outcome. Although the advantages of LESS over conventional laparoscopy have not been clearly proven, the feasibility of using LESS has been widely demonstrated in various urologic procedures [3-11].
Nevertheless, LESS is still challenged with a number several difficulties associated with contemporary instrumentation, such as the lack of instrument triangulation, instrument shaft clashing, disoriented view, and diminished surgical dexterity for intracorporeal reconstructive procedures. In an attempt to overcome the aforementioned drawbacks of LESS, specially designed instrumentation such as prebent or articulating instruments, end-on light sources, and flexible optics have recently been introduced [12].
Additionally, several variations of LESS have emerged, including hybrid NOTES, needlescopic-assisted and robotic-assisted LESS, and the Single Port Instrument Delivery Extended Reach (SPIDER) LESS surgical system. Ideally, a practical single-port system would need to effectively replicate multiport laparoscopy in which triangulation, ergonomic manipulation, and ideal visualization are achieved.
The SPIDER surgical system by TransEnterix (Durham, NC, USA) currently facilitates single-port surgery by use of a flexible laparoscopic platform. The SPIDER surgical system allows multiple instruments to be used through a single incision. The system may thus result in fewer incisions and allow a faster recovery for the patient, while providing enhanced surgical capabilities for the surgeon. Since its introduction in 2009, it has been applied mostly in the general surgery community for cholecystectomy and bariatric procedures. The goal of this report was to describe our initial experience performing various urological procedures with the use of a second-generation SPIDER surgical system in a porcine model.
MATERIALS AND METHODS
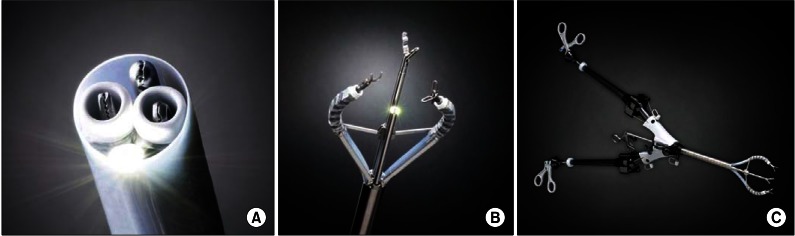
The SPIDER surgical system by TransEnterix (Durham) is a novel technology that has been reported to be safe and effective for LESS cholecystectomy in an animal model. We used the second-generation SPIDER surgical system to complete laparoscopic urological procedures in a porcine model with the approval of the animal use committee. The second-generation SPIDER surgical system uses a single-operator platform that accommodates a range of multiple flexible surgical instruments through a single port/cannula (outer diameter, 18 mm) encapsulating four working channels (two flexible and two rigid). The surgical system eliminates the need for multiple abdominal punctures, because it requires only an umbilical incision (Fig. 1A). A retractable sheath that covers the distal end of the SPIDER includes the main body port (cannula) and the extended reach instrument delivery tubes (IDTs). The IDTs are positioned laterally to include extended lumens to facilitate manipulation of flexible surgical instruments, enabling control of the instruments over extended distances. True right and true left instrumentation and triangulation can be achieved through two IDTs with 360-degree range of motion. The redesigned IDTs in the second-generation SPIDER surgical system incorporate a vertebral design to increase the forces generated at the distal instrument tips and to reduce the length of the articulating portion of the IDTs to 13.4 cm. Various articulating instruments are available that are flexible and offer both a standard and a long length with 360-degree range of motion to help achieve desired operative reach through the IDTs. The SPIDER flex instruments are specifically designed for use with the SPIDER surgical platform. These include a wavy grasper, a Maryland dissector, Endoshears, a suction irrigator (probe and adaptor), a fenestrated grasper, a clip applier, a monopolar hook, and a needle driver. Two rigid channels, superiorly (12 o'clock) and inferiorly (6 o'clock), can accommodate a 5-mm endoscope or any of the common off-the-shelf rigid surgical instruments with a diameter less than 6 mm. When the SPIDER surgical system is advanced into the abdominal cavity, the flexible IDTs open up umbrella-like within the abdominal cavity and are used to guide the flexible surgical instruments (Fig. 1B). The sheath protects the internal tissues as the cannula is advanced through the abdominal wall and is pulled back once the cannula is in position. The SPIDER eliminates the awkward crossed arms movement and allows a single surgeon to operate the device more ergonomically for true right and left instrument manipulation (Fig. 1C). In addition to four working channels, three distinct ports allow for insufflations or smoke evacuation. The SPIDER device also includes a support arm accessory to mount and stabilize the device. Once the procedure is completed, the SPIDER surgical system closes up and is removed through the same incision.
FIG. 1.
(A) Single Port Instrument Delivery Extended Reach (SPIDER) surgical system, encapsulating four working channels (two flexible and two rigid). Two flexible SPIDER instruments are placed in the 3 o'clock and 9 o'clock channels. The laparoscope is placed at the 6 o'clock channel, and the rigid instrument is placed at the 12 o'clock channel. (B) SPIDER instrument delivery tubes (IDTs). The IDTs open up umbrella-like within the abdomen. The laparoscope is seen at the 6 o'clock channel and the rigid laparoscopic grasper is placed at the 12 o'clock channel. (C) Overview of the SPIDER single-port surgical device depicting the main body cannula and two instrument delivery tubes (IDTs). Two IDTs are opened with two flexible SPIDER instruments being placed in the 3 and 9 o'clock active channels and the rigid laparoscopic grasper being placed through the 12 o'clock static channel.
In the present study, the insertion and setup of the SPIDER surgical system were thoroughly assessed. In four domestic swine weighing approximately 32 to 35 kg, five nephrectomies, four adrenalectomies, three pyeloplasties, and three partial cystectomies and closures were performed by a single surgeon. Each swine was placed in the lateral flank position under general anesthesia for the nephrectomy, adrenalectomy, and pyeloplasty procedures. For partial cystectomy and closure, the animal was placed in the moderate Trendelenburg position. An open Hasson technique was applied at the midumbilical area to introduce a 12-mm trocar, and a 45-cm bariatric 30-degree 5-mm scope was introduced to visualize the abdominal cavity. Under pneumoperitoneum, the 12-mm trocar was removed and the SPIDER surgical system was inserted into the peritoneal cavity under direct visualization. The SPIDER surgical system was placed in optimal working angles facing the kidney area and the platform was locked in position by using the docking ball (Fig. 2). A 45-cm bariatric 30-degree 5-mm scope was introduced through a static channel (6 o'clock) of the SPIDER platform to visualize the intra-abdominal cavity. During the different surgical steps, the SPIDER system was repositioned as needed to obtain an optimal working space and angles.
FIG. 2.
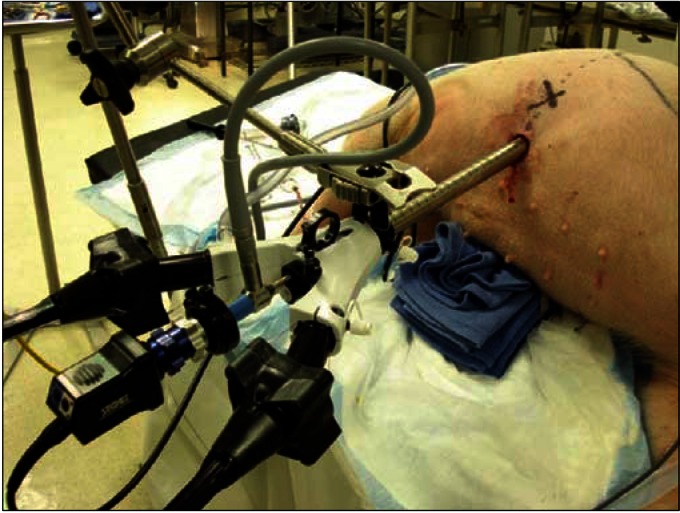
Basic operative setup of the Single Port Instrument Delivery Extended Reach (SPIDER) surgical system. The surgical system is inserted through the right lower quadrant of the swine and faces the target area. The SPIDER platform is locked in position by using the docking ball. The swine is in the left lateral position.
For nephrectomy, a combination of the SPIDER fenestrated grasper, Maryland dissector, monopolar hook, and Endoshears was used. The hilum was first dissected carefully by using a combination of a fenestrated grasper and a monopolar hook. The renal artery and vein were separately dissected and clipped by using a SPIDER 5-mm Weck clip (Hem-O-Lok, Teleflex Inc., Research Triangle Park, NC, USA) applier. The SPIDER suction/irrigator was used to clean the surgical field. The kidney was freed and kept in the abdomen.
For adrenalectomy, a SPIDER fenestrated grasper and a monopolar hook were used to meticulously isolate the adrenal gland from the aorta or inferior vena cava. For pyeloplasty, a combination of SPIDER Endoshears, Maryland dissector, fenestrated grasper, and needle drivers were used to isolate, transect, spatulate, and anastomose the ureter.
For partial cystectomy, the bladder dome was excised in half by use of the SPIDER wavy grasper, Endoshears, and a monopolar hook. Closure of the bladder was performed by using a single layer of absorbable suture with the SPIDER needle drivers. Intraoperative parameters included operative time, time to manage the renal pedicle, estimated blood loss, complications, the addition of extra ports, and the degree of surgeon's comfort.
RESULTS
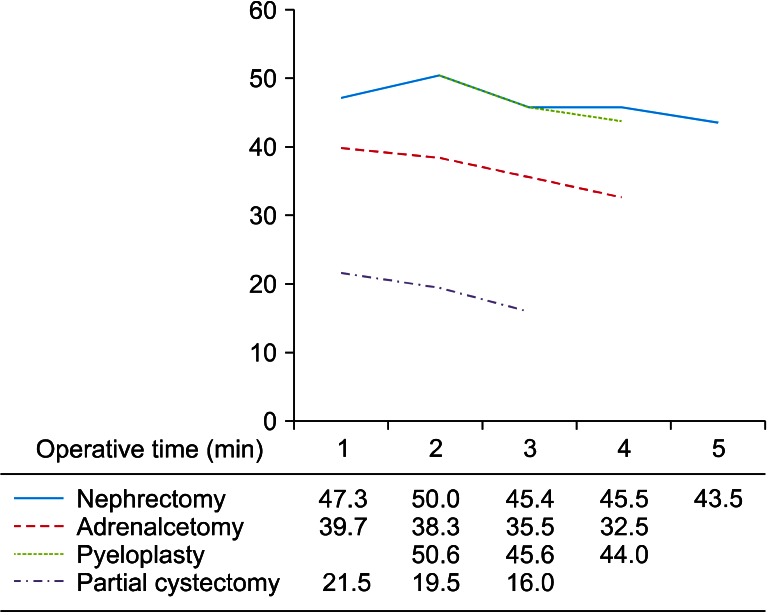
All five nephrectomies, four adrenalectomies, three pyeloplasties, and three partial cystectomies and closures were performed successfully without additional skin incisions for laparoscopic ports, instrument clashing, or open convertsion. The operative time data are shown in Fig. 3.
FIG. 3.
Operative time depending on the surgery. 1,3,5: right side; 2,4: left side.
Three right and two left nephrectomies were performed without any incidence. The mean time to set up the SPIDER platform was 3.5 minutes without any complications associated with the insertion. The mean operative time for right and left nephrectomy was 45.4 minutes (range, 43.5 to 47.3 minutes) and 47.8 minutes (range, 45.5 to 50.0 minutes), respectively. The mean time to control the renal pedicle for right and left renal kidneys was 16.8 minutes and 17.5 minutes, respectively. Frequent adjustment of the SPIDER system was required to mobilize the kidney after the hilar control to obtain an optimal working space. No complications were observed in the nephrectomy procedures and the blood loss was negligible.
Two right and two left adrenalectomies were performed. The mean operative time for the right and left adrenalectomy was 37.6 minutes (range, 35.5 to 39.7 minutes) and 35.4 minutes (range, 32.5 to 38.3 minutes), respectively. Minimal adjustment of the SPIDER system was needed to complete the procedures and the blood loss was less than 5 mL.
One right and two left pyeloplasties were performed. The mean operative time for the pyeloplasty for the right and left ureter was 45.6 minutes and 47.3 minutes (range, 44.0 to 50.6 minutes), respectively. Because of the blunt nature of the SPIDER Endoshears, the spatulation of the medial end of the distal ureter was made after the initial anchoring suture was completed at the lateral end of the spatulated ureter. After the medial anchoring sutures were placed, continuous suture bites were taken to complete the anastomosis of the posterior wall and, subsequently, the anterior wall was anastomosed in continuous suture bites to complete watertight anastomosis. All of the ureteral manipulation and suturing were completed by using only two flexible SPIDER instruments. Generally, a total of 8 to 9 circumferential suture bites were taken on the ureter to complete the anastomosis. Indigo carmine was injected intravenously to test watertight status. All of the pyeloplasties were confirmed to have watertight anastomosis except in the first left pyeloplasty, which showed minimal urine leakage.
The mean operative time for the partial cystectomies and closures was 18.6 minutes (range, 15.0 to 21.5 minutes). Closure of the bladder was performed in a single layer.
DISCUSSION
Since the introduction of laparoscopy in the late 1980s, the technique has been widely performed in various surgical disciplines, including urology, general surgery, transplant surgery, and surgical oncology, because of its ability to reduce morbidity and shorten the recovery period [13]. During the past decade, interest and efforts have continued to further advance minimally invasive surgical procedures. The development of novel surgical techniques has triggered the surgical innovations known as NOTES and LESS. NOTES quickly became the next minimally invasive surgical frontier in general surgery [14,15]. Although NOTES was theoretically attractive, suboptimal instrument design and functionality have limited its wide application in the surgical community. Enthusiastic urologists have been applying LESS surgery techniques to various laparoscopic procedures in urology. With the ability to eliminate visual scars and improve cosmesis compared with multiport laparoscopy, LESS may also improve resumption to early normal activities by reducing procedure-related infections and requirements for postoperative pain medication.
Despite relatively limited experience with the technique worldwide, LESS has already been shown to have results comparable to those of conventional laparoscopy for most of the urologic procedures that have been reported. For example, Desai et al. [16] performed a total of 100 LESS procedures, including simple prostatectomy (32%), donor nephrectomy (17%), pyeloplasty (17%), simple nephrectomy (14%), and partial nephrectomy (6%). White et al. [17] reported the same number of LESS procedures, including donor nephrectomy (19%), partial nephrectomy (15%), sacral colpopexy (13%), and renal cryotherapy (8%). Those authors reported favorable data compared with conventional laparoscopic series with postoperative complications in the range of 5% to 10%. Similarly, Raman et al. [18] and Raybourn et al. [19] demonstrated that there were no major differences between LESS and conventional laparoscopic nephrectomies.
Although LESS is an attractive surgical modality that has advanced to the ultimate aim of minimally invasive surgery, it does have some technical limitations. First, the conventional triangular arrangement of instruments is not achieved in LESS. Therefore, conventional laparoscopic suturing techniques cannot be applied, which makes the meticulous suturing of renal parenchyma and other reconstructive suturing more technically challenging [20]. Second, the currently available instruments for the procedure provide limited triangulation and suboptimal movements and require extensive fascial trauma. In order to overcome some of these drawbacks, several variations of LESS devices have recently been introduced. The first is hybrid and pure NOTES. This technique facilitates the natural orifices of the body such as the mouth, anus, vagina, and urethra as an access point to the abdominal cavity. In humans so far, transvaginal access has been the only site proven as feasible [21]. However, clinical experience with transvaginal NOTES is still limited. Another approach is needlescopic-assisted LESS. In this approach, apart from the introduction of conventional LESS instruments through the multichannel port, additional "needle-like" 2-mm to 3-mm instruments are used. The main advantage of needlescopic-assisted LESS is that it solves one of the basic limitations of LESS, which is the lack of instrument triangulation. The safety and efficacy of needlescopic-assisted LESS were proven by Gill et al. [22] and Desai et al. [23]. Nevertheless, this is not true single-port surgery. Also, using an additional port in LESS as practiced by others defeats the purpose of the single-port surgery.
The newly developed second-generation SPIDER surgical system represents an innovative surgical platform that overcomes many of the limitations inherent with the current instrumentation. The SPIDER surgical system is designed for less invasive surgery that maintains the principles of standard laparoscopic surgery. This system allows the surgeon to perform different procedures by using a combination of multiple flexible and common laparoscopic instruments through a single port (outer diameter, 18 mm) containing four working channels, thereby eliminating the need for multiple abdominal ports, which is an essential feature of the "true" concept of single-port surgery. The SPIDER surgical system replicates the visual and instrument orientation of the operative field and maintains standard laparoscopic techniques and critical views throughout the surgical procedures.
Recently, Pryor et al. [24] demonstrated the feasibility of LESS cholecystectomy with use of the first-generation SPIDER system. Those authors showed that true triangulation and simple retraction are achieved without added operative time or the need to tolerate uncomfortable techniques that may lead to frustration of the surgeons. In addition, low morbidity, faster recovery, and improved cosmesis are other appealing advantages of the SPIDER system. We have also demonstrated in this study that various urological procedures can be performed effectively in a reasonable operative time with minimal complications by use of the SPIDER surgical system.
In terms of technical aspects, many of the mechanical advantages of the surgical system were apparent: triangulation to obtain a critical operative view, ergonomic handling of the instrument tips, and operation through a true single port. The reduced length of the articulating IDTs and the vertebral design provide the width of two flexible instrument tips in an optimal position with increased forces at the distal instrument tips, thereby facilitating an optimal working environment. Prior laparoscopic experience of the surgeon represented an important variable in the operative procedures. The operating surgeon had only 20 to 30 minutes of device introduction and manipulation and proceeded to perform the surgical procedures on the basis of the protocol. Surgeons with advanced laparoscopic skills will feel comfortable handling the SPIDER platform. Among the procedures performed, pyeloplasty was still challenging compared with the other ablative procedures such as nephrectomy and adrenalectomy. During the pyeloplasty procedures, spatulation of the distal cut-end ureter was difficult because of the blunt end of the Endoshears. Furthermore, continuous suturing with only two flexible needle drivers made accurate needle tip placement rather challenging. The surgeon had to hold the sutures in place with the left needle driver to provide optimal tension on both cut ends of the upper ureter for the subsequent suture bites, because the current needle drivers did not have a locking handle mechanism. Use of a straight laparoscopic instrument to hold the suture through the static channel might have eased the suturing effort. During the different surgical steps in nephrectomy and adrenalectomy, the SPIDER system was repositioned as needed to allow an optimal view and working angles. This movement might have prolonged the operative time in nephrectomy and adrenalectomy. Basic surgical maneuvers such as dissection, grasping, cutting, and cauterization were performed without any difficulty by using the SPIDER monopolar hook, Endoshears, and Maryland graspers. However, retracting and suction/irrigation were somewhat difficult with the current SPIDER flexible instruments. Nearly half of the operative time in nephrectomy was devoted to surgical steps in mobilizing the kidney after the hilar control because of suboptimal instrument strength. At this time, a third-generation device is in the final stage and should address some of the mechanical limitations mentioned here. In this study, the SPIDER surgical system provided a stable single-port platform with restored triangulation, diminished external instrument clashing, ergonomic handling, and critical working views. The drawbacks of the second-generation SPIDER surgical system require further improvement in design and modification to optimize its clinical application in urology.
CONCLUSIONS
In this initial pilot evaluation, we have demonstrated that the second-generation SPIDER surgical system offered intuitive instrument maneuverability, restored triangulation without external instrument clashing, and provided critical intraoperative views. However, retraction was challenging because of the lack of strength and lack of precise manipulation of the tip when the instruments were fully deployed. Future refinements of the technology and prospective studies are needed to further optimize the application of this surgical system in urology.
Footnotes
The authors have nothing to disclose.
SUPPLEMENTARY MATERIALS
An accompanying video can be found in the 'Urology in Motion' section of the journal homepage (www.kjurology.org). The supplementary data can also be accessed by scanning a QR code located on the title page of this article.
References
- 1.Gettman MT, Lotan Y, Napper CA, Cadeddu JA. Transvaginal laparoscopic nephrectomy: development and feasibility in the porcine model. Urology. 2002;59:446–450. doi: 10.1016/s0090-4295(01)01568-0. [DOI] [PubMed] [Google Scholar]
- 2.Gettman MT, Box G, Averch T, Cadeddu JA, Cherullo E, Clayman RV, et al. Consensus statement on natural orifice transluminal endoscopic surgery and single-incision laparoscopic surgery: heralding a new era in urology? Eur Urol. 2008;53:1117–1120. doi: 10.1016/j.eururo.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 3.Autorino R, Cadeddu JA, Desai MM, Gettman M, Gill IS, Kavoussi LR, et al. Laparoendoscopic single-site and natural orifice transluminal endoscopic surgery in urology: a critical analysis of the literature. Eur Urol. 2011;59:26–45. doi: 10.1016/j.eururo.2010.08.030. [DOI] [PubMed] [Google Scholar]
- 4.Kaouk JH, Autorino R, Kim FJ, Han DH, Lee SW, Yinghao S, et al. Laparoendoscopic single-site surgery in urology: worldwide multi-institutional analysis of 1076 cases. Eur Urol. 2011;60:998–1005. doi: 10.1016/j.eururo.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 5.Tracy CR, Raman JD, Cadeddu JA, Rane A. Laparoendoscopic single-site surgery in urology: where have we been and where are we heading? Nat Clin Pract Urol. 2008;5:561–568. doi: 10.1038/ncpuro1215. [DOI] [PubMed] [Google Scholar]
- 6.Tugcu V, Ilbey YO, Mutlu B, Tasci AI. Laparoendoscopic single-site surgery versus standard laparoscopic simple nephrectomy: a prospective randomized study. J Endourol. 2010;24:1315–1320. doi: 10.1089/end.2010.0048. [DOI] [PubMed] [Google Scholar]
- 7.Andonian S, Rais-Bahrami S, Atalla MA, Herati AS, Richstone L, Kavoussi LR. Laparoendoscopic single-site Pfannenstiel versus standard laparoscopic donor nephrectomy. J Endourol. 2010;24:429–432. doi: 10.1089/end.2009.0185. [DOI] [PubMed] [Google Scholar]
- 8.Tracy CR, Raman JD, Bagrodia A, Cadeddu JA. Perioperative outcomes in patients undergoing conventional laparoscopic versus laparoendoscopic single-site pyeloplasty. Urology. 2009;74:1029–1034. doi: 10.1016/j.urology.2009.04.089. [DOI] [PubMed] [Google Scholar]
- 9.Jeong BC, Park YH, Han DH, Kim HH. Laparoendoscopic single-site and conventional laparoscopic adrenalectomy: a matched case-control study. J Endourol. 2009;23:1957–1960. doi: 10.1089/end.2009.0404. [DOI] [PubMed] [Google Scholar]
- 10.White WM, Goel RK, Kaouk JH. Single-port laparoscopic retroperitoneal surgery: initial operative experience and comparative outcomes. Urology. 2009;73:1279–1282. doi: 10.1016/j.urology.2009.01.051. [DOI] [PubMed] [Google Scholar]
- 11.White WM, Goel RK, Swartz MA, Moore C, Rackley RR, Kaouk JH. Single-port laparoscopic abdominal sacral colpopexy: initial experience and comparative outcomes. Urology. 2009;74:1008–1012. doi: 10.1016/j.urology.2009.02.086. [DOI] [PubMed] [Google Scholar]
- 12.Stolzenburg JU, Kallidonis P, Oh MA, Ghulam N, Do M, Haefner T, et al. Comparative assessment of laparoscopic single-site surgery instruments to conventional laparoscopic in laboratory setting. J Endourol. 2010;24:239–245. doi: 10.1089/end.2009.0296. [DOI] [PubMed] [Google Scholar]
- 13.Irwin BH, Rao PP, Stein RJ, Desai MM. Laparoendoscopic single site surgery in urology. Urol Clin North Am. 2009;36:223–235. ix. doi: 10.1016/j.ucl.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 14.de la Fuente SG, Demaria EJ, Reynolds JD, Portenier DD, Pryor AD. New developments in surgery: Natural Orifice Transluminal Endoscopic Surgery (NOTES) Arch Surg. 2007;142:295–297. doi: 10.1001/archsurg.142.3.295. [DOI] [PubMed] [Google Scholar]
- 15.Rattner D, Kalloo A ASGE/SAGES Working Group. ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery. October 2005. Surg Endosc. 2006;20:329–333. doi: 10.1007/s00464-005-3006-0. [DOI] [PubMed] [Google Scholar]
- 16.Desai MM, Berger AK, Brandina R, Aron M, Irwin BH, Canes D, et al. Laparoendoscopic single-site surgery: initial hundred patients. Urology. 2009;74:805–812. doi: 10.1016/j.urology.2009.02.083. [DOI] [PubMed] [Google Scholar]
- 17.White WM, Haber GP, Goel RK, Crouzet S, Stein RJ, Kaouk JH. Single-port urological surgery: single-center experience with the first 100 cases. Urology. 2009;74:801–804. doi: 10.1016/j.urology.2009.04.030. [DOI] [PubMed] [Google Scholar]
- 18.Raman JD, Bagrodia A, Cadeddu JA. Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol. 2009;55:1198–1204. doi: 10.1016/j.eururo.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 19.Raybourn JH, 3rd, Rane A, Sundaram CP. Laparoendoscopic single-site surgery for nephrectomy as a feasible alternative to traditional laparoscopy. Urology. 2010;75:100–103. doi: 10.1016/j.urology.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 20.Choi KH, Ham WS, Rha KH, Lee JW, Jeon HG, Arkoncel FR, et al. Laparoendoscopic single-site surgeries: a single-center experience of 171 consecutive cases. Korean J Urol. 2011;52:31–38. doi: 10.4111/kju.2011.52.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Autorino R, Haber GP, White MA, Khanna R, Altunrende F, Yang B, et al. Pure and hybrid natural orifice transluminal endoscopic surgery (NOTES): current clinical experience in urology. BJU Int. 2010;106(6 Pt B):919–922. doi: 10.1111/j.1464-410X.2010.09670.x. [DOI] [PubMed] [Google Scholar]
- 22.Gill IS, Canes D, Aron M, Haber GP, Goldfarb DA, Flechner S, et al. Single port transumbilical (E-NOTES) donor nephrectomy. J Urol. 2008;180:637–641. doi: 10.1016/j.juro.2008.04.028. [DOI] [PubMed] [Google Scholar]
- 23.Desai MM, Stein R, Rao P, Canes D, Aron M, Rao PP, et al. Embryonic natural orifice transumbilical endoscopic surgery (E-NOTES) for advanced reconstruction: initial experience. Urology. 2009;73:182–187. doi: 10.1016/j.urology.2008.04.061. [DOI] [PubMed] [Google Scholar]
- 24.Pryor AD, Tushar JR, DiBernardo LR. Single-port cholecystectomy with the TransEnterix SPIDER: simple and safe. Surg Endosc. 2010;24:917–923. doi: 10.1007/s00464-009-0695-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
An accompanying video can be found in the 'Urology in Motion' section of the journal homepage (www.kjurology.org). The supplementary data can also be accessed by scanning a QR code located on the title page of this article.