Abstract
Study Objectives:
To compare the impact of a group educational program versus individual education on continuous positive airway pressure (CPAP) adherence.
Methods:
Post hoc assessment of a performance improvement initiative designed to improve clinic efficiency, access to care, and time to initiate therapy. Consecutive patients newly diagnosed with obstructive sleep apnea (OSA) initiating CPAP therapy participated in either an individual or group educational program. The content and information was similar in both strategies.
Results:
Of 2,116 included patients, 1,032 received education regarding OSA and CPAP through a group clinic, and 1,084 received individual education. Among the cohort, 76.6% were men, mean age 48.3 ± 9.2 years, mean body mass index 29.6 ± 4.6 kg/m2, and mean apnea-hypopnea index was 33.3 ± 24.4 events/hour. Baseline characteristics were similar between groups. CPAP adherence was significantly greater in those participating in a group program than those receiving individual education. Specifically, CPAP was used for more nights (67.2% vs. 62.1%, p = 0.02) and more hours per night during nights used (4.3 ± 2.1 vs. 3.7 ± 2.8, p = 0.03). Further, fewer individuals discontinued therapy (10.6% vs. 14.5%, p < 0.001), more achieved regular use of CPAP (45.2%. vs. 40.6%, p = 0.08), and time to initiate therapy was shorter (13.2 ± 3.1 versus 24.6 ± 7.4 days, p < 0.001). Group education resulted in a 3- to 4-fold increase in the number of patients seen per unit time.
Conclusions:
A group educational program facilitated improved CPAP adherence. If confirmed by prospective randomized studies, group CPAP education may be an appropriate alternative to individual counseling, may improve acceptance of and adherence to therapy, and decrease time to treatment.
Commentary:
A commentary on this article appears in this issue on page 551.
Citation:
Lettieri CJ; Walter RJ. Impact of group education on continuous positive airway pressure adherence. J Clin Sleep Med 2013;9(6):537-541.
Keywords: CPAP, OSA, adherence, education
The growing recognition of obstructive sleep apnea (OSA) continues to increase demands for clinical evaluations and continuity of care. Means to improve the efficiency of sleep medicine clinics and increase access to care without adversely affecting outcomes are needed.
While the benefits of continuous positive airway pressure (CPAP) are well recognized, acceptance of treatment and adherence with therapy remain problematic. Despite advances in CPAP platforms and comfort features, both short-term and long-term compliance patterns have not significantly improved. Current estimates indicate that 29% to 83% of patients prescribed CPAP are non-adherent with therapy (≤ 4 h of use per night).1
In light of the ongoing challenge of CPAP adherence, any methods implemented to improve the efficiency of sleep centers in order to meet growing demands should not impair CPAP use. To that end, methods that could both improve clinic output and foster better adherence would be ideal. Given that the use of CPAP during the initial treatment period, even the first few days of therapy, has been consistently shown to predict long-term use,2,3 strategies aimed at improving the process of therapy initiation could enhance both clinical operations and subsequent adherence.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Patient education regarding the effects of OSA, benefits for therapy, and proper use of CPAP are fundamental for improving both adherence to therapy and outcomes. Unfortunately, the demands for initial evaluations often impair the capacity of sleep centers to provide this service. Strategies that can enhance patient-directed education without compromising clinic efficiency are clearly needed.
Study Impact: A group educational program may facilitate both improved access to care and increased CPAP adherence.
Patients' lack of comprehension regarding the adverse effects of untreated OSA, benefits of therapy, and proper use of CPAP is an important contributor in the unacceptably poor observed rates of CPAP adherence.4–6 Like other disorders, comprehensive education regarding these factors is an important component of therapeutic acceptance and may improve treatment adherence by facilitating incorporation of patients into the therapeutic plan, thereby allowing them to participate in an active and informed manner in the decision-making process.7,8 Previous studies have demonstrated that intensive education and support may improve CPAP adherence.9–13 However, as the demand for sleep evaluations continues to increase, the ability for physicians to provide one-on-one, comprehensive education may diminish. Moreover, the allocation of time and resources needed to provide this education on an individual basis could limit access to care for new patient evaluations without exploring the use alternatives strategies or developing mechanisms to improve efficiency.
A comprehensive intensive educational approach appears to increase patient understanding and awareness, facilitate acceptance of therapy, and improve adherence.9–13 However, the efficacy, efficiency, and cost-effectiveness of these programs remains controversial.14,15 While intensive education may benefit individual patients, the clinical improvements it generates may not outweigh the allocation of resources it requires. In contrast, group educational programs increase access to care and reduce individual resource allocation. While this has not yet been explored for CPAP initiation, group patient education has been demonstrated to improve outcomes in several other disease processes, particularly diabetes mellitus and rheumatoid arthritis.7,8 While these programs decrease overall resource allocation, they also limit individualized education and counseling, and consequently, may negatively impact adherence.
While patient education affords significant benefits, it is associated with inherent costs related to clinic efficiency, time, resources, and access to care. In contrast, improving clinic efficiency at the expense of patient education will likely adversely affect adherence. Given the growing demand for sleep clinics to diagnose and treat OSA in the context of continued difficulties with CPAP adherence, initiating CPAP therapy in a group setting offers several potential benefits, such as more comprehensive education and additional patients cared for per unit of time. We sought to determine if adherence differed between patients who initiated CPAP therapy following individual counseling compared to a group class setting.
METHODS
Study Design
We report the outcomes of a performance improvement initiative designed to improve the efficiency and patient-specific outcomes in our sleep disorders center. The initiative involved development of a multidisciplinary group education clinic for patients with newly diagnosed OSA who were initiating CPAP therapy.
We included all adult patients initiating CPAP therapy in our center between January 2009 and July 2010. All patients received their care from a single academic sleep disorders center (Walter Reed Army Medical Center, Washington DC). Patients eligible for care in our institution constitute a range of Active Duty Service members, their dependents, and those retired from Military service. Our population represents a wide range of patient demographics (age, gender, ethnicity, educational, and socioeconomic backgrounds) which, in general, are representative of the US population and populations cared for at academic civilian institutions. Patients seen at our sleep disorders center have the option of being cared for in our institution or at a local civilian center. There is no cost to their health care regardless of where they are seen.
Individuals who were unable to participate in a group counseling center due to cognitive impairments or refusal to participate in a group setting were not included in this investigation. Otherwise no records were excluded from this analysis.
OSA was diagnosed by an attended, overnight level I polysomnogram in all patients, in accordance with the American Academy of Sleep Medicine guidelines.16 Patients undergoing either full-night diagnostic polysomnograms followed by CPAP titrations or split-night studies were eligible for inclusion. All polysomnographic studies were manually scored and interpreted by board certified sleep physicians in accordance with published guidelines.
The protocol was approved by our institution's Department of Clinical Investigation (Scientific Review Committee, Human Use Committee, and Institutional Review Board). No external funding was utilized to complete this study.
Interventions
Patients were categorized by whether they initiated CPAP therapy following an individual or group counseling session. Assignment to individual counseling or a group class was not determined by any pre-established criteria, but rather reflected our clinic's procedure at that time. Specifically, placement of patients into one of the two educational programs was based upon the day of the week their overnight polysomnogram was performed. Further, all polysomnographic studies at our institution are scheduled to accommodate the patient's wishes, and there was no difference in the acuity or complexity of studies between the different weeknights. Patients were not aware of this distinction at the time they scheduled their polysomnogram. However, those who did not wish to participate in a group clinic were able to request an individual follow-up appointment.
Patients receiving individual counseling initiated CPAP during a scheduled clinic appointment after their initial sleep clinic consultation and polysomnographic studies were completed. During this appointment they received one-on-one counseling by a board-certified sleep physician regarding the results of their polysomnographic studies, basic information on OSA, its known effects on comorbid conditions, proper sleep hygiene, adjunctive/conservative methods to improve sleep, and the importance of treatment adherence. Patients were also provided specific counseling on the proper use and maintenance of CPAP and underwent personalized, formal mask fitting by a specialized respiratory therapist trained in sleep apnea and CPAP equipment. This format adhered to a standardized approach according to our clinic's procedures. The total time for this method was 45min/patient.
Patients who participated in group classes for CPAP initiation were scheduled for a shared session, generally consisting of 15-20 patients. Consent to participating in a group class was obtained at the time of scheduling, and all personally identifying information was protected during the classes. This session consisted of a 20-min lecture given by a board-certified sleep physician involving basic information regarding OSA, its sequelae, treatment options, and the benefits therapeutic adherence, similar to the information provided during individual counseling sessions. This was followed by a 10- to 15-min lecture from the sleep clinic's registered nurses regarding proper sleep hygiene, adjunctive/conservative methods to improve sleep, and reinforcement of the benefits of adherence. Patients were then instructed on the proper use and maintenance of the CPAP equipment and underwent formal mask fitting by a specialized respiratory therapist To ensure privacy, no personal information was discussed during the group portion of this program. At the completion of the group session, all patients enrolled in the group sessions were seen on an individual basis by one of the board-certified sleep physicians to provide them the opportunity to discuss the details of their respective polysomnograms, to help identify any barriers to therapy they might have, and to address questions or concerns not covered in the shared lectures. The total time for the group sessions was approximately 2-2.5 hours. In comparison, the group educational program was able to initiate CPAP therapy in 15-20 patients in the same time frame as we were able to initiate therapy in 6 patients receiving individual counseling. In other words, the group class facilitated a 3- to 4-fold increase in clinic efficiency in this regard.
Other than the type of educational session, all patients treated with CPAP in our center received similar care. All patients cared for in our clinic had a comprehensive sleep evaluation by one of our sleep medicine physicians prior to undergoing any polysomnographic studies. All individuals received a telephone follow-up during the first 2 weeks of treatment to ensure proper mask fit and to identify any potential barriers to CPAP adherence; all had access to a 24-h support line for problems arising from CPAP therapy. Additionally, all patients were automatically scheduled to undergo a clinical evaluation after the first month of therapy to optimize care. All patients received the same model of CPAP (Respironics System One Auto, Phillips Respironics, Murrysville, PA).
Measured Variables
Age, gender, body mass index (BMI), diagnostic apneahypopnea index (AHI), Epworth Sleepiness Scale (ESS), and Fatigue Analog Scale were recorded for each patient. In addition, objective use of CPAP was measured in all patients during their initial follow-up evaluation after their first month of therapy (Encore Anywhere, Phillips Respironics). Specifically, we recorded the percentage of nights CPAP was used, the mean hours of CPAP use per night for all nights, and the mean hours of CPAP use per night during nights used.
Endpoints
The primary outcome measured was the difference in the use of CPAP during the first 4 weeks of therapy between the 2 groups. Differences in the rates of discontinuation of therapy and regular use of CPAP between groups served as secondary outcomes. We defined regular use as the use of CPAP > 4 h/ night on more than 70% of nights. In the event a patient failed to return for follow-up, we assumed therapy had been discontinued, and CPAP use was recorded as zero. The time between the titration polysomnogram and initiation of CPAP therapy was also compared between the two groups.
Statistical Analysis
Data are presented as the mean ± one standard deviation. All tests were two-tailed, and p values < 0.05 were assumed to represent statistical significance. Differences between groups were examined using the independent-samples t-test for continuous variables and the χ2 test for categorical data. Data were analyzed using the PAWP 17.0 (SPSS Inc, Chicago, IL).
RESULTS
During the inclusive time period, 2,158 patients initiated CPAP therapy in our center. Forty-two individuals were excluded from the final analysis (a group setting was considered to be inappropriate by their sleep physician in 24, and 18 did not wish to participate in a group clinic). The final included cohort consisted of 2,116 patients (98.1%). Of the total cohort, 32.7% underwent a split-night study. The remainder (67.3%) participated in a full-night in-lab CPAP titration following their initial diagnostic polysomnogram.
The majority of the cohort were men (76.6%), with a mean age of 48.3 ± 9.2 years, and mean BMI of 29.6 ± 4.6 kg/m2. Most patients had moderate-severe OSA, with a mean AHI of 33.3 ± 24.4 events/h. For the entire cohort, CPAP was used on 64.7% of nights, with a mean nightly use of 3.2 ± 2.8 h on all nights and 4.1 ± 2.0 h on nights CPAP was utilized. Regular use among all patients was 42.8%, and 12.5% discontinued therapy.
Among the cohort, 1,084 (51.2%) received individual counseling and 1,032 (48.8%) participated in a group education clinic. Baseline patient characteristics were similar between the 2 groups (Table 1). Compared to individual counseling, CPAP adherence was greater among those who participated in a group clinic (Table 2). Specifically, group clinic patients used CPAP on 67.2% ± 30.8% of nights, compared with 62.1% ± 37.0% in those receiving individual counseling (p = 0.02). Nightly use of CPAP among group clinic patients was 3.5 ± 1.9 h during all nights compared with 3.1 ± 2.6 h in those receiving individual counseling (p = 0.04). Similarly, during nights CPAP was used, the mean use of CPAP was greater in those undergoing group education (4.3 ± 2.1 versus 3.7 ± 2.8 hours, p = 0.03). Regular use of CPAP tended to be more common in those who participated in a group clinic and was observed in 45.2%, compared with only 40.6% of those receiving individual counseling (p = 0.08). In addition, the time between the CPAP titration polysomnography and initiation of CPAP therapy was considerably shorter among those participating in the group clinic (13.2 ± 3.1 versus 24.6 ± 7.4 days, p < 0.001).
Table 1.
Baseline characteristics of patients receiving individual versus group education
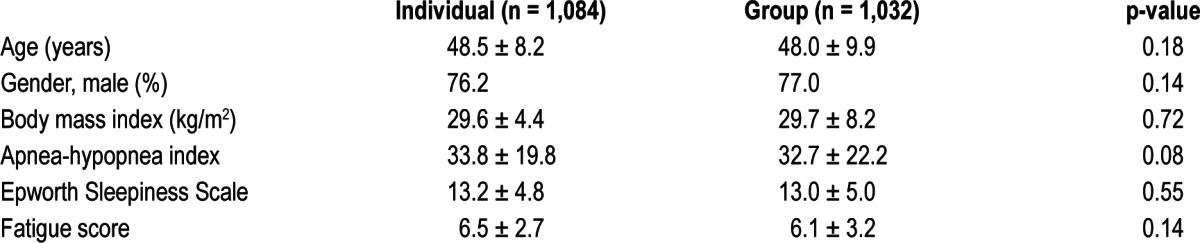
Table 2.
Comparison of CPAP use between individual versus group education
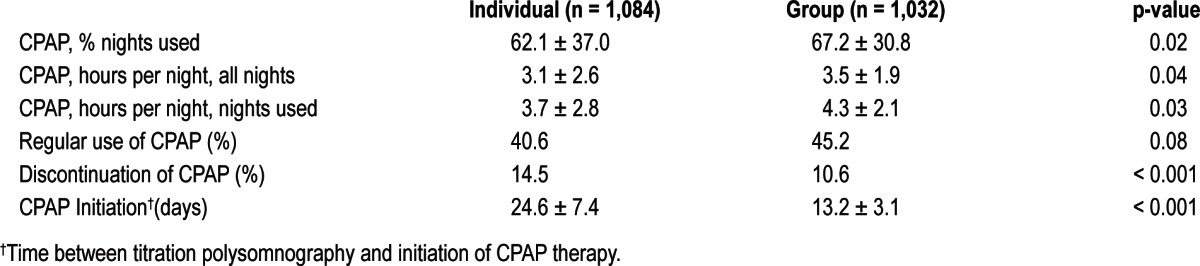
Overall, 256 patients (12.6%) discontinued therapy during the first month of treatment. Discontinuation of therapy was significantly less common in the group patients, occurring in 10.6%, compared with 14.5% among those receiving individual counseling (p < 0.001). Patients who discontinued CPAP were more likely to have a lower AHI (23.2 ± 25.8 vs. 31.3 ± 27.3 events/h, p = 0.06), a higher ESS (16.7 ± 5.9 vs. 12.7 ± 2.1, p = 0.02), weighed more (32.0 ± 5.0 vs. 30.4 ± 4.7 kg/m2, p = 0.09), and were more likely to be women (35.3% vs. 18.1%, p = 0.01). Furthermore, of those who discontinued therapy, 198 patients (77.3%) had received individual counseling (p < 0.001).
DISCUSSION
Despite less time allocated per patient, we found that a group educational strategy resulted in improved acceptance of and adherence to CPAP therapy. Using a group educational setting yielded a three to four-fold increase in the number of patients per unit of time. Further, we did not observe any detriment in subsequent adherence. In fact, objective measures of CPAP use, rates of regular use of CPAP, and discontinuation of therapy were all improved. In addition, group clinics decreased the time between polysomnography and initiation of therapy
The improvement in CPAP adherence observed in those initiating therapy through a group clinic is likely multifactorial. Both strategies provided the same CPAP device, same clinical evaluations and follow-up care, and similar education regarding OSA and the proper use of CPAP. Given this, it appears that the type of the educational program was the basis for the differences in CPAP use between. Group sessions followed a relatively standard approach to education and shared similar content. While these groups were conducted by different staff physicians, they were based on agreed-upon content and format. Individual sessions, on the other hand, were likely less standardized and may have included variable counseling regarding the effects of non-treatment or emphasis on the benefits of CPAP. Further, group clinics involved participation by a clinic nurse. While the overall content and information provided was similar, having an additional provider likely facilitated a greater emphasis on key points. Regardless, both formats provided similar content, were delivered by the same core group of providers, and all patients received formalized mask selection and fitting, and the same CPAP platform and follow-up care. The dynamic setting of the educational program was the only significant difference and, as such, likely had the greatest impact on our observed outcomes. These improvements may, in part, be a result of reinforcement of the importance of CPAP adherence and strategies for promoting proper usage by several providers. However, we believe it is also largely due to external validation that occurs within a small group environment. Within this setting, patients are encouraged to express concerns, reservations regarding therapy, and personal challenges with their medical condition. In turn, this creates an environment of peer reinforcement of their shared experience and realization that other similar people also have their condition. While this form of external validation and peer support can benefit the acceptance of many disease processes, it is likely more pronounced in disorders like OSA where misconceptions, biases, and images regarding the demographics of apneic patients remain prevalent.
In a similar study, Golay and associates demonstrated improvements in treatment adherence in existing OSA patients on CPAP therapy who underwent additional group educational interventions after an initial period of CPAP use.9 While the study reported preliminary results, utilized a small cohort, and lacked a control group, it nonetheless demonstrated improvements in the both duration of CPAP use and subjective sleepiness at three months. Likewise, Likar and colleagues observed improvements in CPAP among patients with OSA who participated in group clinics for continuity of care and follow-up assessments at regular time intervals (6 months) over a two-year period.10
Group educational strategies have been demonstrated to improve outcomes in several other disease processes. Rickheim et al. showed that group educational programs improved outcomes in the management of diabetes mellitus.7 Specifically, they observed greater improvements in HbA1c among those who underwent group versus individualized education. Likewise, Barlow and associates demonstrated that group educational clinics positively impacted the management of rheumatoid arthritis and showed improvements in arthritis symptom severity, self-efficacy, and psychological well-being at three- and six-month follow-up assessments.8
Our study has several potential limitations. First, our results reflect observations from a performance improvement initiative and not a prospective, randomized trial. Similar to retrospective studies, our study design limits the validity of our findings. However, we included a large number of consecutive patients, which minimizes the potential for bias. In addition, patients were not assigned to either intervention based on any predetermined criteria, which mitigates the potential for selection biases. Patients had the option of not participating in a group setting, which could also create selection bias. However, this occurred in only 1.3% of those initially designated for a group clinic. Second, both interventions received considerable education, which likely diminished the differences observed between the two groups that could have underestimated the value of this educational model. Overall, regular use of CPAP was low among the cohort. While not dissimilar from other reports, it does highlight the ongoing challenges related to CPAP adherence and emphasizes the need to explore any potentially positive interventions, especially those that are not associated with an increase in costs or resources. Third, while the individual educational counseling adhered to a standardized curriculum endorsed by our clinic, some variations in the educational experience may have occurred. However, in an attempt to minimize this, the physicians responsible for providing the individual educational counseling also co-developed and conducted the group educational program. Further, both educational programs had identical respiratory therapy components conducted by the same specialized respiratory therapists. As such, this impact should have been minimal. We did not include data regarding race or educational level, as our primary focus was the impact of our proposed educational model of adherence, and we limited the information gathered to those items specifically related to sleep and sleep disordered breathing. The impact of these factors on adherence has been explored in prior studies. However, none have been consistently shown to influence adherence. It is possible that we would have identified some additional confounding factor, especially given the size of our study. Finally, while long-term use of CPAP is often predicted by short-term adherence patterns, we only measured CPAP adherence during the first month of therapy. It is, therefore, uncertain if these improvements will be sustained.
As the prevalence of OSA and the demand for CPAP continue to increase, fewer resources will likely be available for patients. Through the initiation of a group educational strategy, we were able to decrease the time to therapy while promoting better acceptance of and adherence to therapy. In our institution, group clinics also facilitated a more rapid initiation of therapy and reduced delays in treatment. In addition, group clinics decrease the use of clinic appointments for CPAP initiation which allows for more new and follow-up evaluations. Our results suggest that a group educational setting to initiate patients on CPAP therapy appears to be an effective and productive use of resource that increases clinic availability and therapeutic adherence. The role of this form of educational strategy warrants additional consideration and may be a viable alternative to traditional, individual physician-directed counseling. Further investigation in a prospective randomized trial is needed to validate these findings.
DISCLOSURE STATEMENT
The views expressed in this manuscript are solely those of the authors and do not reflect those of the Department of the Army or Department of Defense. This study received no financial support. Dr. Lettieri serves on the speaker's bureau for Cephalon (now Teva Pharmaceuticals). The other author has indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Dorothy Clinton, N.P. for her invaluable assistance in the administration of the group educational program and data collection for this analysis.
ABBREVIATIONS
- CPAP
continuous positive airway pressure
- OSA
obstructive sleep apnea
- BMI
body mass index
- AHI
apnea-hypopnea index
- ESS
Epworth Sleepiness Scale
REFERENCES
- 1.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5:173. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aloia MS, Arnedt JT, Stanchina M, Millman RP. How early in treatment is PAP adherence established? Revisiting night-to-night variability. Behav Sleep Med. 2007;5:229–40. doi: 10.1080/15402000701264005. [DOI] [PubMed] [Google Scholar]
- 3.Pépin JL, Krieger J, Rodenstein D, et al. Effective compliance during the first 3 months of continuous positive airway pressure. A European prospective study of 121 patients. Am J Respir Crit Care Med. 1999;160:1124–9. doi: 10.1164/ajrccm.160.4.9802027. [DOI] [PubMed] [Google Scholar]
- 4.Popescu G, Latham M, Allgar V, et al. Continuous positive airway pressure for sleep apnoea/hypopnoea syndrome: usefulness of a 2 week trial to identify factors associated with long term use. Thorax. 2001;56:727–33. doi: 10.1136/thorax.56.9.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stepnowsky CJ, Marler MR, Ancoli-Israel S. Determinants of nasal CPAP compliance. Sleep Med. 2002;3:239–47. doi: 10.1016/s1389-9457(01)00162-9. [DOI] [PubMed] [Google Scholar]
- 6.Stepnowsky CJ, Marler MR, Palau J, et al. Social-cognitive correlates of CPAP adherence in experienced users. Sleep Med. 2006;7:350–6. doi: 10.1016/j.sleep.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 7.Rickheim PL, Weaver TW, Flader JL, Kendall DM. Assessment of group versus individual diabetes education: a randomized study. Diabetes Care. 2002;25:269–74. doi: 10.2337/diacare.25.2.269. [DOI] [PubMed] [Google Scholar]
- 8.Barlow JH, Barefoot J. Group education for people with arthritis. Patient Educ Couns. 1996;27:257–67. doi: 10.1016/0738-3991(95)00844-6. [DOI] [PubMed] [Google Scholar]
- 9.Golay A, Girard A, Grandin S, et al. A new educational program for patients suffering from sleep apnea syndrome. Patient Educ Couns. 2006;60:220–7. doi: 10.1016/j.pec.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 10.Likar LL, Panciera TM, Erickson AD, Rounds S. Group education sessions and compliance with nasal CPAP therapy. Chest. 1997;111:1273–7. doi: 10.1378/chest.111.5.1273. [DOI] [PubMed] [Google Scholar]
- 11.Hoy CJ, Vennelle M, Kingshott RN, Engleman HM, Douglas NJ. Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome? Am J Respir Crit Care Med. 1999;159:1096–100. doi: 10.1164/ajrccm.159.4.9808008. [DOI] [PubMed] [Google Scholar]
- 12.Chervin RD, Theut S, Bassetti C, Aldrich MS. Compliance with nasal CPAP can be improved by simple interventions. Sleep. 1997;20:284–9. doi: 10.1093/sleep/20.4.284. [DOI] [PubMed] [Google Scholar]
- 13.Aloia MS, Dio LD, Ilniczky MA, Perlis ML, Greenblatt DW, Giles DE. Improving compliance with nasal CPAP and vigilance in older adults with OSAHS. Sleep Breath. 2001;5:13–21. doi: 10.1007/s11325-001-0013-9. [DOI] [PubMed] [Google Scholar]
- 14.Meurice JC, Ingrand P, Portier F, et al. A multicentre trial of education strategies at CPAP induction in the treatment of severe sleep apnoea-hypopnoea syndrome. Sleep Med. 2007;8:37–42. doi: 10.1016/j.sleep.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 15.Hui DS, Chan JK, Choy DK, et al. Effects of Augmented continuous positive airway pressure education and support on compliance and outcome in a Chinese population. Chest. 2000;117:1410–6. doi: 10.1378/chest.117.5.1410. [DOI] [PubMed] [Google Scholar]
- 16.Kushida CA, Littner MR, Morgenthaler T, et al. Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep. 2005;28:499–521. doi: 10.1093/sleep/28.4.499. [DOI] [PubMed] [Google Scholar]


