Abstract
Study Objectives:
To determine the relationship between sleep complaints, primary insomnia, excessive daytime sleepiness, and lifestyle factors in a large community-based sample.
Design:
Cross-sectional study.
Setting:
Blood donor sites in New Zealand.
Patients or Participants:
22,389 individuals aged 16-84 years volunteering to donate blood.
Interventions:
N/A.
Measurements:
A comprehensive self-administered questionnaire including personal demographics and validated questions assessing sleep disorders (snoring, apnea), sleep complaints (sleep quantity, sleep dissatisfaction), insomnia symptoms, excessive daytime sleepiness, mood, and lifestyle factors such as work patterns, smoking, alcohol, and illicit substance use. Additionally, direct measurements of height and weight were obtained.
Results:
One in three participants report < 7-8 h sleep, 5 or more nights per week, and 60% would like more sleep. Almost half the participants (45%) report suffering the symptoms of insomnia at least once per week, with one in 5 meeting more stringent criteria for primary insomnia. Excessive daytime sleepiness (evident in 9% of this large, predominantly healthy sample) was associated with insomnia (odds ratio [OR] 1.75, 95% confidence interval [CI] 1.50 to 2.05), depression (OR 2.01, CI 1.74 to 2.32), and sleep disordered breathing (OR 1.92, CI 1.59 to 2.32). Long work hours, alcohol dependence, and rotating work shifts also increase the risk of daytime sleepiness.
Conclusions:
Even in this relatively young, healthy, non-clinical sample, sleep complaints and primary insomnia with subsequent excess daytime sleepiness were common. There were clear associations between many personal and lifestyle factors—such as depression, long work hours, alcohol dependence, and rotating shift work—and sleep problems or excessive daytime sleepiness.
Citation:
Wilsmore BR; Grunstein RR; Fransen M; Woodward M; Norton R; Ameratunga S. Sleep habits, insomnia, and daytime sleepiness in a large and healthy community-based sample of New Zealanders. J Clin Sleep Med 2013;9(6):559-566.
Keywords: Epidemiology, insomnia, sleep, sleepiness
Sleep disturbance is a common and often underdiagnosed complaint in general medical practice,1 which can persist over many years2 and has been shown to result in health problems, greater functional impairment, lost productivity, and excess health care utilization.3–5 The ability of community health resources to treat sleep-related problems appears limited.6 However, insomnia can be a symptom of other conditions, such as depression,7 substance abuse,8 and sleep disordered breathing.9 Currently, the term “primary insomnia” is used to define insomnia in the absence of such conditions.10 Many epidemiological studies in the past have not accounted for these conditions when determining the prevalence of insomnia.11–13
Despite the well-established significance of insomnia, some studies have suggested sleep dissatisfaction is a more accurate predictor than insomnia of the likelihood of seeking medical help, reporting daytime impaired functioning, and of being diagnosed with a sleep or a mental disorder.14–16 Other sleep conditions related to sleep quantity, quality, and excessive daytime sleepiness have also been associated with negative health consequences,17 including injury18 and memory impairment.19 However, large community-based studies utilizing a detailed questionnaire to explore relationships between sleep disorders and complaints and lifestyle behaviors are scant.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Insomnia, daytime sleepiness and inadequate sleep are common complaints, but have not been accurately quantified in the past. The current study utilised 22,389 relatively healthy New Zealanders with the ability to control for multiple confounders such as depression, sleep disordered breathing and substance abuse, to more accurately determine how common these sleep complaints are, and to identify the relationship between such sleep complaints, primary insomnia, excessive daytime sleepiness, and lifestyle factors.
Study Impact: This study highlights how incredibly common sleep complaints are, even in this relatively young, healthy, nonclinical sample, and identifies some of the common associations such as depression, long work hours, alcohol dependence, and rotating shift work.
The aim of the current analysis was to utilize data from the New Zealand Blood Donors' Health Study (NZBDHS) to determine the association of multiple sleep related variables with personal and lifestyle factors and evaluate the influence of these factors on primary insomnia and excessive daytime sleepiness in a large, diverse, yet predominantly healthy, community-based sample.
METHODS
Recruitment procedures and methodology of the New Zealand Blood Donors' Health Study (NZBDHS) are detailed elsewhere.20,21 In brief, 22,389 people volunteering to donate blood (81% response rate) aged 16 years or older were recruited into the study from April 1998 to October 1999, at blood collection points managed by the Northern Regional Blood Service in the Northland, Auckland, Waikato, and Bay of Plenty regions of New Zealand.22 The criteria for accepting volunteer blood donation in New Zealand are in accordance with international guidelines (www.nzblood.co.nz). In general, the donor must be in good health, have a hemoglobin > 120 g/L (females) or 130 g/L (men), and be free from high-risk behaviors to ensure the safety of both the donor and recipient. The study was approved by regional ethics committees, and all participants provided informed consent.
Height, weight, and neck circumference were measured by study staff. A self-administered questionnaire was used to solicit details regarding the presence of snoring, sleep apnea, sleep complaints (satisfaction, quantity, and insomnia), alcohol consumption, smoking, use of marijuana or other illegal drugs, and depression (Appendix). Detailed instruments used in previous research and the pilot study informed its content.22 Participants were also asked if they had ever been told by a doctor that they have, or have had a heart attack, a stroke, epilepsy, migraine, or diabetes.
The main classification systems for insomnia are the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)10 and International Classification of Sleep Disorders (ICSD).23 The criteria for defining an insomnia complaint in the current study were consistent with these definitions and previous large-scale studies.24 To be considered as having an insomnia complaint a subject had to: (i) report difficulty initiating sleep (DIS) or maintaining sleep (DMS), early morning awakening (EMA) with inability to resume sleep, or a complaint of non-restorative sleep (NRS) in spite of adequate sleep duration, ≥ 4 times per month (i.e., once per week) and (ii) claim to be dissatisfied with the amount of his/her sleep, or take a sleep-enhancing medication. These two conditions had to be present together to conclude the presence of an insomnia complaint. “Primary insomnia” was defined as having an insomnia complaint (meeting criteria above) in the absence of alcohol dependence (CAGE),25–27 regular cannabis or illicit drug use, depression, and sleep apnea. Insomnia rates vary based on different definitions, including insomnia complaints in the absence of sleep dissatisfaction and more frequent symptoms (e.g., more than every other day)28–30; therefore the analysis and reporting is presented with both more liberal and conservative definitions than the DSM-IV and ICSD criteria. Daytime sleepiness was quantified using the Epworth Sleepiness Scale (ESS)31 and dichotomized into presence (score > 10) or absence (score ≤ 10) of excessive daytime sleepiness, based on evidence indicating scores > 10 have an increased propensity to obstructive sleep apnea syndrome, narcolepsy, or idiopathic hypersomnia.31 Sleep quantity was collected as a continuous variable based on the number of nights in which ≥ 7-8 h of sleep were obtained, then categorized for logistic regression. Questions relating to depression were based on the CIDI-SFMD60 and are elaborated in the appendix.
Logistic regression was performed with log odds of insomnia as the dependent variable and adjustment for multiple potential covariates (age, sex, body mass index, neck circumference, sleepiness, sleep quantity, alcohol consumption, smoking, cannabis and illicit drug use, depression, employment status and subsequent primary occupation, hours of work per week, work pattern, education, marital status, and ethnicity). Covariates were kept continuous where possible. Interactions between primary occupation, marital status, insomnia, age, and sex were also assessed. Similar analysis was performed with log odds of excessive daytime sleepiness as the dependent variable. Throughout this paper, OR is used to represent cross-sectional odds ratios. Reported differences are significant at the 0.05 level. All analyses were performed using SPSS version 12.
RESULTS
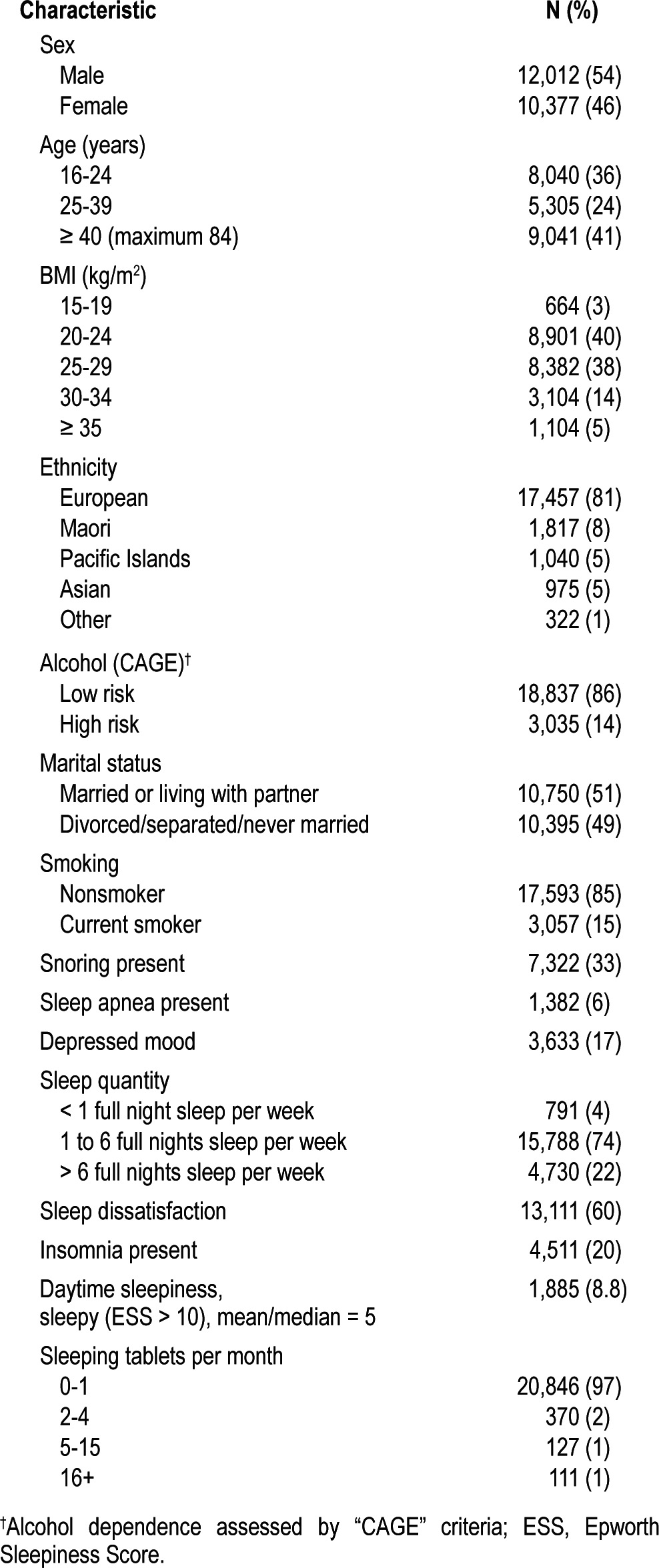
Demographic data and physical measurements were available from all 22,389 NZBDHS participants (Table 1). Questionnaire responses were received from 96% of the NZBDHS participants. Those who returned questionnaires were similar to those who did not in age (mean difference: 0.1 years) and sex (males comprised 46% of those who returned questionnaires and 47% of those who did not). The percentages of self-reported major illnesses were very low (0.2% reporting a history of heart attack, 0.2% a history of stroke, and 0.4% diabetes), compared with the general population as noted in the New Zealand Health Survey in 2002 (10.4% heart disease, 2.1% stroke, 4.3% diabetes).32 This study had a higher proportion of participants aged 16-39 years than the New Zealand Health Survey (60% vs 36%, respectively; Table 1).
Table 1.
Participant characteristics
Sleep Complaints
In this cohort, 7,298 (34%) participants reported not getting at least 7-8 h of sleep 5 or more nights per week. The amount of sleep increased with age (p < 0.001). When asked “How do you feel about the amount of sleep you normally get?” only 7,503 (34%) responded with “Get the right amount” and 1,429 (6%) with “Get plenty.” Therefore dissatisfaction with the amount of sleep was reported by 60% of the cohort. Women reported being dissatisfied with their sleep more than men (Table 2; p < 0.001), and the percentage reporting sleep dissatisfaction decreased with age (p < 0.001; Table 2). Thus, sleep quantity and subsequently sleep satisfaction, increased with age. The more insomnia symptoms reported, the higher the likelihood of sleep dissatisfaction (Table 3).
Table 2.
Primary insomnia, daytime sleepiness, sleep dissatisfaction and poor sleep quantity by age and gender
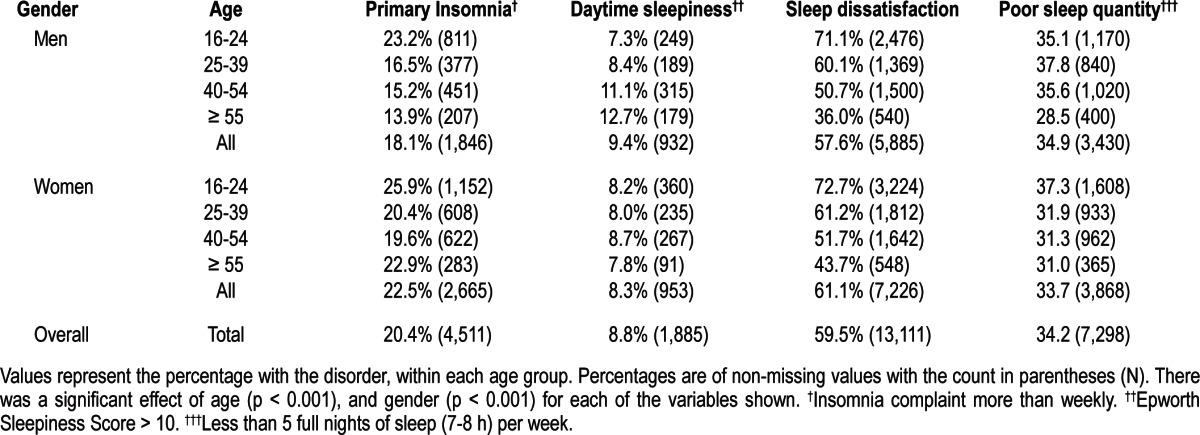
Table 3.
Relationship between lifestyle factors and sleep dissatisfaction after mutually adjusting for multiple risk factors*
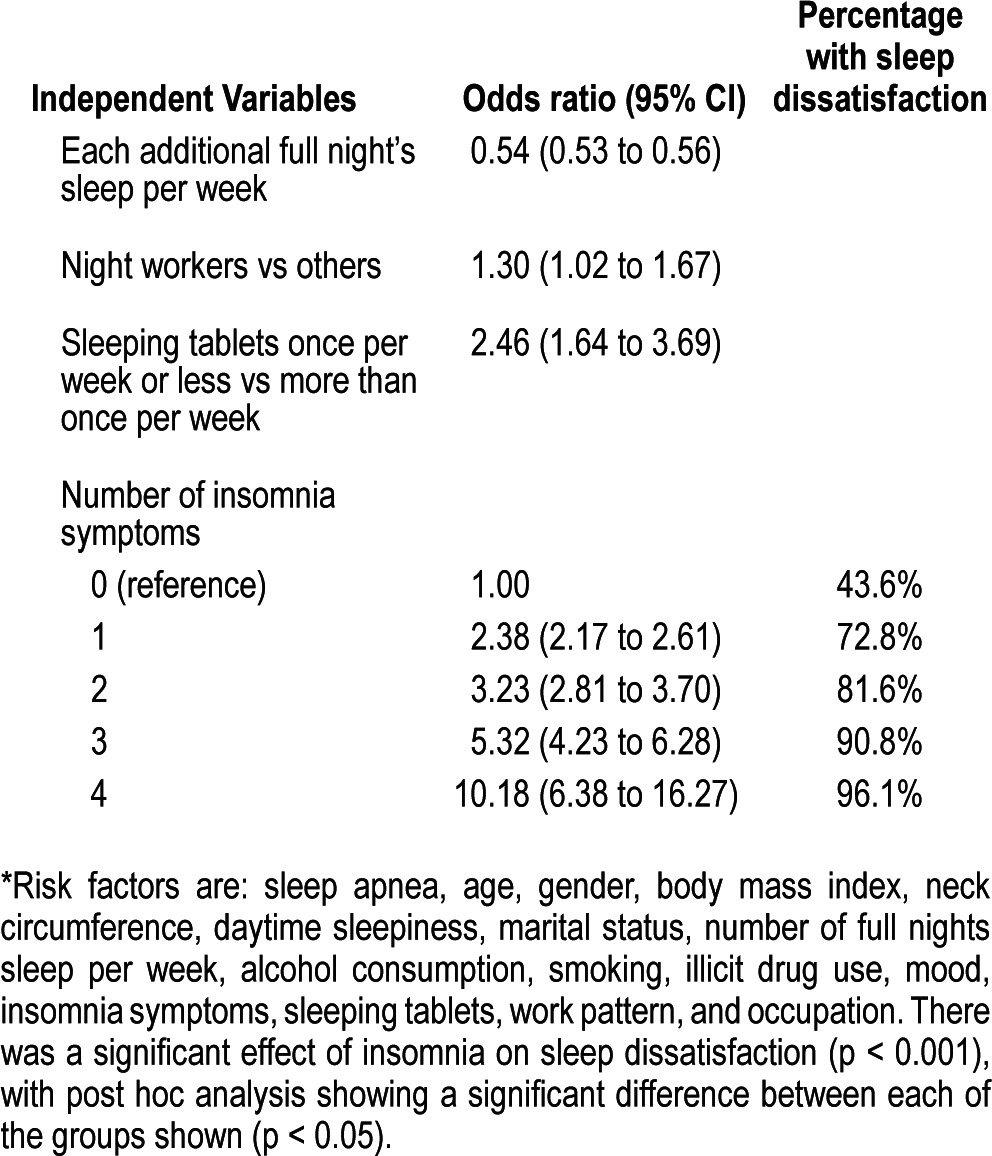
After mutually adjusting for multiple risk factors (sleep apnea, age, gender, body mass index, neck circumference, daytime sleepiness, marital status, number of full nights sleep per week, alcohol consumption, smoking, illicit drug use, mood, insomnia symptoms, sleeping tablets, work pattern, and occupation), non-workers were less likely to be dissatisfied with their sleep (OR 0.79, CI 0.67-0.93). Each full night of sleep almost halved the odds of being dissatisfied (OR 0.54, CI 0.53 to 0.56). Factors that increased the risk of sleep dissatisfaction included: night workers (OR 1.30, CI 1.01 to 1.67), taking sleeping tablets ≤ 1 time per week (OR 2.46, CI 1.64 to 3.69), and having 1 (OR 2.38, CI 2.17 to 2.61), 2 (OR 3.23, CI 2.81 to 3.70), 3 (OR 5.32, CI 4.23 to 6.28), or 4 (OR 10.18, CI 6.38 to 16.27) insomnia symptoms (Table 3). Importantly, with adjustment for these multiple confounders, including the number of full nights sleep per week, those with insomnia still report being less satisfied with their sleep. There was an interaction, such that increasing age increased the risk of sleep dissatisfaction for women (OR 1.010 per year, CI 1.004 to 1.015) but decreased the odds for men (OR 0.991 per year, CI 0.985 to 0.996; p < 0.001). Being divorced, separated, or widowed; smoking; or taking sleeping tablets more than weekly did not affect sleep dissatisfaction.
Sleep Disordered Breathing
Among participants with sleep disordered breathing, a history of depressive symptoms was reported by 7%. After adjusting for multiple potential confounders, snoring was not associated with depressive symptoms (OR 1.05, CI 0.94 to 1.18). However sleep apnea increased the odds of having experienced depressive symptoms (OR 1.28, CI 1.05 to 1.56); not surprisingly, being depressed increased the odds of serious suicidal thoughts (OR 5.80, CI 5.12 to 6.58). Importantly, sleep apnea increased the odds of having had serious thoughts of suicide, even after adjusting for depressive symptoms (OR 1.44, CI 1.15 to 1.80).
Primary Insomnia
A total of 20,516 (93%, after excluding 321 with missing data) participants reported ≥ 1 of the 4 insomnia symptoms at least once per month; 9,843 (45%) reported ≥ 1 of the 4 insomnia symptoms more than once per week (Figure 1). Of these 9,843 individuals, 7,792 (79%) also reported being dissatisfied with their sleep (or reported taking sleeping tablets more than once per week), that is, 35% of the total cohort. After excluding participants who were alcohol dependent (CAGE ≥ 2),25–27,33 regular cannabis or illicit drug users, reported history of depressive symptoms, or suffering sleep apnea, there were 4,511 (20%) of the original cohort subsequently classified as having “primary insomnia”24 defined as at least one insomnia symptom more than once per week, with sleep dissatisfaction, not attributable to alternative medical conditions (Figure 1). Primary insomnia was more commonly reported in women (Table 2).
Figure 1. Flow chart for primary insomnia (values are percentages of non-missing values).
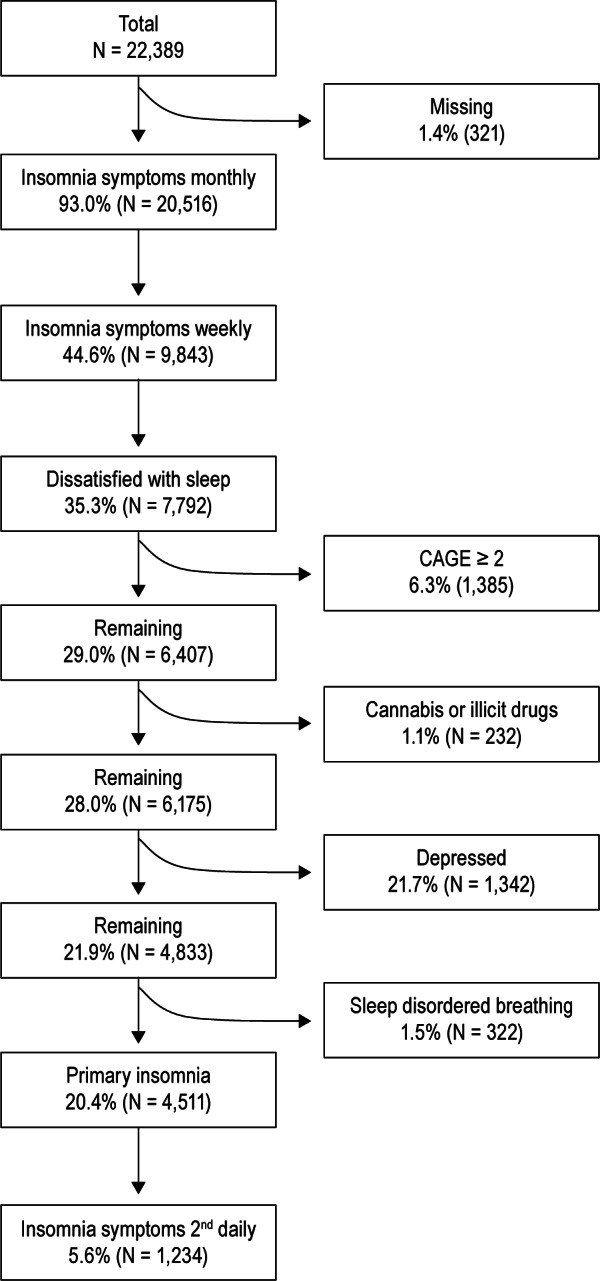
Of the 4,511 participants with primary insomnia, 1,234 (27%), or approximately 6% of the entire cohort, reported suffering at least one symptom of insomnia > 15 times per month. Among the 4,511 participants with primary insomnia, difficulty initiating sleep (DIS) was reported most commonly (44%), followed by difficulty maintaining sleep ([DMS] 36%) and early morning awakenings (EMA) with inability to resume sleep (34%). A single insomnia symptom was reported by 52% of participants with primary insomnia, 2 symptoms by 27%, and 3 or 4 symptoms by 21%.
The percentage of participants reporting primary insomnia (with sleep dissatisfaction) was high in students (23%), retired women (22%), homemakers (20%), and participants in paid employment (20%) recruited to this study. With respect to work patterns, permanent night workers had the highest proportions of primary insomnia (26%), while daytime workers without rotating shifts had the lowest (19%). For marital status, being “never married” had the highest rates of primary insomnia in both sexes (23%). Divorced men had comparatively low rates (13%), while divorced women had much higher rates (24%).
The odds of suffering insomnia was lower among unemployed participants (OR 0.64, CI 0.44 to 0.94) than workers in paid employment. Higher levels of education also reduced the odds of primary insomnia. The OR comparing university education to primary or secondary school only was 0.78, CI 0.70 to 0.86, and comparing university to technical college or similar was 0.90, CI 0.81 to 0.99. After controlling for potential confounders, work patterns and marital status were no longer significantly associated with primary insomnia.
After adjusting for potential confounders (age, sex, body mass index, neck circumference, alcohol consumption, smoking, cannabis and illicit drug use, depression, employment status and subsequent primary occupation, hours of work per week, work pattern, education, marital status, and ethnicity), primary insomnia was associated with excessive daytime sleepiness. The OR for a one-unit increase in ESS was 1.03, CI 1.02 to 1.04 and for ESS > 10 (compared to ≤ 10) OR 1.30, CI 1.14 to 1.48.
Excessive Daytime Sleepiness
Excessive daytime sleepiness (ESS > 10) was evident in 1,885 (9%). These participants were most likely to report a moderate-to-high chance of dozing in the afternoon (42%); however, 2% reported a moderate-to-high chance of dozing while driving a moving car. Excessive daytime sleepiness increased with age in men (p < 0.001) but not women (p = 0.737; Table 2).
Participants with ESS > 10, on average, had a higher BMI (mean difference, 0.6 kg/m2, CI 0.4 to 0.8), worked 4 more hours per week (4.1, CI 3.0 to 5.1), had almost one full night's sleep less per week (mean difference 0.9, CI 0.8 to 1.0), were more likely to report sleep apnea (18%, snore 11%, neither 7%; p < 0.001), smoke (10% v 9%; p = 0.002), be alcohol dependent (12% v 8%; p < 0.001), report having been depressed (15% v 8%; p < 0.001), be dissatisfied with their sleep (11% v 5%; p < 0.001), and work rotating shifts with night shifts (12% v 9%; p = 0.014).
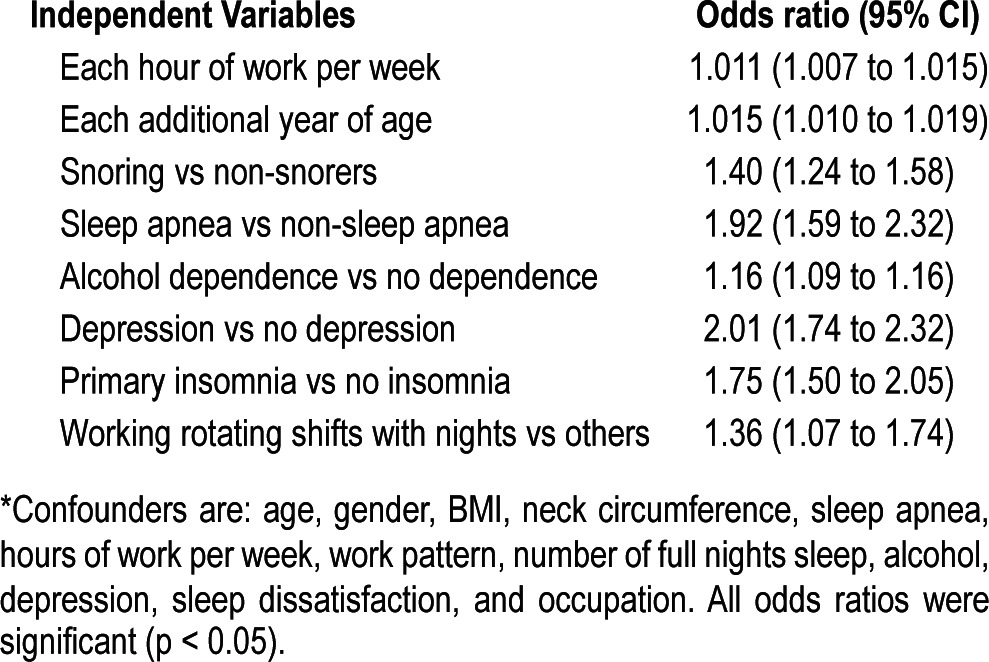
After mutually adjusting for all these potential confounders, each hour of paid work per week increased the odds of reporting excessive daytime sleepiness (OR 1.011, CI 1.007 to 1.015), as did each additional year of age (1.015, CI 1.010 to 1.019). In addition, snoring (1.40, CI 1.24 to 1.58), sleep apnea (1.92, CI 1.59 to 2.32), depression (2.01, CI 1.74 to 2.32), alcohol dependence (1.16, CI 1.09 to 1.16), primary insomnia (1.75, CI 1.50 to 2.05), and working rotating shifts with nights (1.36, CI 1.07 to 1.74) all remained significantly associated with an increased odds of excessive daytime sleepiness (Table 4).
Table 4.
Relationship between lifestyle factors and excessive daytime sleepiness, after mutually adjusting for multiple potential confounders*
DISCUSSION
The current study involving a cohort of people presenting to volunteer blood donor sites, was unique in its size and ability to adjust for the effects of secondary causes of insomnia (such as depression, sleep disordered breathing, illicit drug use, and alcohol dependence) to more accurately isolate primary insomnia. Additionally, the substantial heterogeneity in distribution of sleep-related factors, personal demographics, and lifestyle behaviors provided the opportunity to determine associations that have received only limited attention previously. Consequently, we have been able to show one in three report insomnia symptoms at least weekly, with sleep dissatisfaction. One in three reported not getting at least 7-8 hours of sleep five or more nights per week, and one in ten suffer excessive daytime sleepiness. Sleep dissatisfaction, a well-established factor associated with seeking medical help, impaired daytime functioning, and mental disorders, was reported by 60% of participants even in this relatively young healthy sample.
Insomnia is associated with lost productivity, greater functional impairment, more days of disability due to health problems, and excess health care utilization.4 After excluding participants with confounding conditions to specifically identify primary insomnia, one in five were considered to be suffering from primary insomnia with symptoms at least weekly, and 6% at least every other night. This finding is similar to the prevalence rates previously reported in other large-scale observational studies utilizing DSM-IV criteria (6% to 7%).16,28 However, the prevalence of insomnia varies with the criteria used to define insomnia. Studies defining symptoms of insomnia as “often” or at least three times per week, report prevalence rates between 6% and 15%,34–37 while studies with criteria based on “major complaints of insomnia,” “being bothered by insomnia,” and “having a great or a very great problem with insomnia” reported prevalence rates between 7% and 12%.38–40 Difficulty initiating sleep has been the most commonly reported symptom in all studies to date.28
Our findings are consistent with previous studies which have shown higher rates of insomnia in women,24,41 separated/divorced/widowed individuals, and night workers.14 In our study sample, high proportions of students also reported insomnia. However, after controlling for potential confounders, we found insomnia only increases with age in women. Much of the increased prevalence of insomnia with increasing age in previous studies24 is likely to be associated with increased prevalence of mental and physical conditions associated with insomnia. In the current study and similar studies where primary insomnia has been isolated, the effect of aging has not been so evident.42
The reporting of significant sleep dissatisfaction was high, with 14% of participants getting “nowhere near enough” or “could do with a lot more” sleep, a finding also within the range of previous similar studies (7% to 18%).11,14,16,24,28,43-45 Each full night of sleep halved the odds of reporting sleep dissatisfaction. While other studies have tended to show increased sleep dissatisfaction with increasing age,14,16,28 this was only evident for women in the current project. The discrepancy may reflect the effect of controlling for multiple potential confounders in a larger, more diverse, and relatively healthy cohort, but the possible effect of a non-representative sample cannot be excluded. Almost two of every three participants would like more sleep, and one in three participants do not get 7 to 8 hours sleep five or more nights per week, with a higher BMI associated with less sleep.46 Reporting the symptoms of insomnia had a substantial effect on sleep satisfaction independent of the amount of sleep obtained. This supports previous studies indicating an altered perception of sleep quality and quantity in people with insomnia.47
Excessive daytime sleepiness was evident in 9% of this large, healthy cohort. This finding is similar to the control subjects in the original study defining the criteria for excessive daytime sleepiness when developing the Epworth scale,31 and within the range of other studies utilizing the Epworth sleepiness score on school aged students,48 middle-aged bus drivers,49 and middle-aged Polish adults.50 Other studies using less well-validated criteria tend to report a higher prevalence of daytime sleepiness (12% in Irish men,51 15% in middle-aged men,52 and 17% aged > 18 years53); however, many of these previous studies have studied specific population subgroups. We have taken a large, diverse group of people and been able to demonstrate that insomnia, depression, suicidal ideation, and sleep disordered breathing are associated with excessive daytime sleepiness, with long work hours, alcohol dependence, and rotating work shifts further increasing the odds of excessive daytime sleepiness.
Our findings must also be interpreted in light of limitations that particularly relate to the recruitment strategy, and the reliance on self-reporting of many lifestyle behaviors and sleep disorders. Most importantly, the study sample was not designed to be representative of the general population or blood donors in New Zealand. The study opportunistically recruited self-selected volunteers reporting to blood donation sites in the study region between 1998 and 1999, some of whom did not meet criteria for blood donation on the day. However, the participants comprise a diverse, nonclinical, community-dwelling sample; and the observed associations between sleep-related factors and other variables of interest in this are likely to be general-izable to other community-based settings. The current survey also had a high response rate (81%) compared with previous studies on the prevalence of insomnia.11,24,38 In addition, we are unlikely to have completely excluded all potential confounding effects when attempting to isolate primary insomnia, such as chronic pain, cardiovascular disease, narcolepsy, delirium, and rarer general medical conditions. However, the possible influence of these factors would be minimal in this relatively young and healthy cohort. The results should also be interpreted in the context of having been collected between 1998 and 1999. Finally, although self-reporting of sleep disorders is likely to underestimate the true magnitude when compared to some direct measurement of sleep quantity and sleep quality, self-report has established accuracy,54–56 allows identification of areas for more detailed investigation, and is the only feasible method of measuring sleep variables in very large observational studies such as the NZBDHS.17,57–59 These potential limitations are offset by accessing the largest cohort examining sleep and insomnia with a high response rate, direct physical measurements, and incorporating a detailed well-validated questionnaire covering multiple personal demographics and lifestyle behaviors.
Even in a large, relatively young and healthy sample, sleep dissatisfaction, inadequate sleep duration, insomnia, and excessive daytime sleepiness are common. The associations of these factors with each other as well as with depression, emphasize the importance of promoting better sleep habits to reduce the risk of adverse health outcomes.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Grunstein has received research supplies from Philips Respironics, ResMed, SomnoMed, and Cephalon. The other authors have indicated no financial conflicts of interest. Data analysis and reporting was performed at Woolcock Institute of Medical Research.
APPENDIX
Self-Administered Questionnaire
Sleep disorders (Yes/No)
Have you ever been told that you snore loudly?
Have you ever been told that you stop breathing while you sleep?
Have you even been told that you appear to choke while you sleep?
Sleep apnea was defined as either stopping breathing or choking whilst asleep.
Sleep complaints
- Sleep satisfaction
- How do you feel about the amount of sleep you normally get?
- Nowhere near enough
- Could do with a lot more
- Could do with a bit more
- Get the right amount
-
Get plentyResponses were dichotomised into dissatisfied (1,2,3) and satisfied (4, 5).
- Sleep quantity
- On average, how many nights during a week do you get a full night's sleep (i.e. at least 7 to 8 hours)?
- Responses were categorized as 0 nights per week; 1-6 nights per week; 7 nights per week. For logistic regression categories were < 5 nights per week; and 5-7 nights per week.
- Insomnia
- Please indicate how often (0, 1, 2-4, 5-15, 16-30 times per month) you experience each of the following:
- o Have trouble falling asleep.
- o Wake up during the night and have difficulty getting back to sleep.
- o Wake up too early in the morning and be unable to get back to sleep.
- Primary insomnia was defined as having at least one of these sleep complaints at least weekly, and being dissatisfied with sleep, in the absence of depression, alcohol dependence, sleep apnea, or illicit substance use.
Alcohol
- Do you currently drink alcohol once a month or more? Yes/No
- If yes, how often do you drink alcohol?
- 6-7 days a week
- 4-5 days a week
- 2-3 days a week
- Once a week
- Once every 2 weeks
- Once a month
- On an average day when you drink alcohol, how many drinks would you usually have in total?
- Alcohol consumption was dichotomized into high and low risk based on the CAGE questionnaire.37 Two positive answers have a sensitivity exceeding 85% and a specificity approaching 90% for the diagnosis of alcohol abuse or dependence.
Smoking
Do you smoke cigarettes (not cigars/pipe) now? Yes/No
How many manufactured cigarettes do you usually smoke each day?
Non-smokers were assigned ‘0’ where smokers were assigned a value based on the number of cigarettes smoked per day.
Marijuana
- During the past 12 months how often did you use marijuana (also know as grass, pot, cannabis, hashish, hash oil)?
- Did not use
- Less than once a month Once a month
- Once every 2 weeks
- Once a week or more often
Other illegal drugs
- During the past 12 months how often did you use other illegal drugs? That is, drugs not prescribed by your doctor or bought from a chemist, such as cocaine, LSD, amphetamines or speed, heroin, morphine.
- Did not use
- Less than once a month Once a month
- Once every 2 weeks
- Once a week or more often
Health
- Have you ever been told by a doctor that you have, or have had:
-
a) a heart attack “coronary”if yes, were you admitted to hospital?
- b) a stroke
- c) a migraine
- d) epilepsy
-
Mood
Have you ever had two weeks or more when you felt sad or depressed nearly every day? Yes/No
Did it interfere a lot with you life, work or activities? Yes/No
Subjects who responded positively to both of these questions constituted one group (high risk for depression), all others constituted the other group. Questions relating to depression were based on the CIDI-SFMD.60
Suicidal ideation was determined by the question: Have you ever seriously thought of committing suicide (that is, taking some action to end your life)? Yes/No
REFERENCES
- 1.Backhaus J, Junghanns K, Mueller-Popkes K, et al. Short-term training increases diagnostic and treatment rate for insomnia in general practice. Eur Arch Psychiatry Clin Neurosci. 2002;252:99–104. doi: 10.1007/s00406-002-0361-x. [DOI] [PubMed] [Google Scholar]
- 2.Mendelson WB. Long-term follow-up of chronic insomnia. Sleep. 1995;18:698–701. doi: 10.1093/sleep/18.8.698. [DOI] [PubMed] [Google Scholar]
- 3.National Institutes of Health State of the Science Conference statement on Manifestations and Management of Chronic Insomnia in Adults, June 13-15, 2005. Sleep. 2005;28:1049–57. doi: 10.1093/sleep/28.9.1049. [DOI] [PubMed] [Google Scholar]
- 4.Simon GE, VonKorff M. Prevalence, burden, and treatment of insomnia in primary care. Am J Psychiatry. 1997;154:1417–23. doi: 10.1176/ajp.154.10.1417. [DOI] [PubMed] [Google Scholar]
- 5.Godet-Cayre V, Pelletier-Fleury N, Le Vaillant M, Dinet J, Massuel MA, Leger D. Insomnia and absenteeism at work. Who pays the cost? Sleep. 2006;29:179–84. doi: 10.1093/sleep/29.2.179. [DOI] [PubMed] [Google Scholar]
- 6.U.S. lacks adequate capacity to treat people with sleep disorder, IOM reports. Hosp Health Netw. 2006;80:74. [PubMed] [Google Scholar]
- 7.Buysse DJ, Reynolds CF, 3rd, Kupfer DJ, et al. Clinical diagnoses in 216 insomnia patients using the International Classification of Sleep Disorders (ICSD), DSM-IV and ICD-10 categories: a report from the APA/NIMH DSM-IV Field Trial. Sleep. 1994;17:630–7. doi: 10.1093/sleep/17.7.630. [DOI] [PubMed] [Google Scholar]
- 8.Brower KJ, Aldrich MS, Robinson EA, Zucker RA, Greden JF. Insomnia, self-medication, and relapse to alcoholism. Am J Psychiatry. 2001;158:399–404. doi: 10.1176/appi.ajp.158.3.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stradling JR, Crosby JH. Predictors and prevalence of obstructive sleep apnoea and snoring in 1001 middle aged men. Thorax. 1991;46:85–90. doi: 10.1136/thx.46.2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fourth edition, text revision: DSM-IV-TR. Fourth ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 11.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention?[see comment] JAMA. 1989;262:1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 12.Ohayon MM, Caulet M. Insomnia and psychotropic drug consumption. Prog Neuropsychopharmacol Biol Psychiatry. 1995;19:421–31. doi: 10.1016/0278-5846(94)00023-b. [DOI] [PubMed] [Google Scholar]
- 13.Ganguli M, Fox A, Gilby J, Belle S. Characteristics of rural homebound older adults: a community-based study. J Am Geriatr Soc. 1996;44:363–70. doi: 10.1111/j.1532-5415.1996.tb06403.x. [DOI] [PubMed] [Google Scholar]
- 14.Ohayon MM, Caulet M, Priest RG, Guilleminault C. DSM-IV and ICSD-90 insomnia symptoms and sleep dissatisfaction. Br J Psychiatry. 1997;171:382–8. doi: 10.1192/bjp.171.4.382. [DOI] [PubMed] [Google Scholar]
- 15.Chiu HF, Leung T, Lam LC, et al. Sleep problems in Chinese elderly in Hong Kong. Sleep. 1999;22:717–26. doi: 10.1093/sleep/22.6.717. [DOI] [PubMed] [Google Scholar]
- 16.Ohayon MM, Zulley J. Correlates of global sleep dissatisfaction in the German population. Sleep. 2001;24:780–7. [PubMed] [Google Scholar]
- 17.Enright PL, Newman AB, Wahl PW, Manolio TA, Haponik EF, Boyle PJ. Prevalence and correlates of snoring and observed apneas in 5,201 older adults. Sleep. 1996;19:531–8. doi: 10.1093/sleep/19.7.531. [DOI] [PubMed] [Google Scholar]
- 18.Lindberg E, Carter N, Gislason T, Janson C. Role of snoring and daytime sleepiness in occupational accidents. Am J Respir Crit Care Med. 2001;164:2031–5. doi: 10.1164/ajrccm.164.11.2102028. [DOI] [PubMed] [Google Scholar]
- 19.Jennum P, Sjol A. Self-assessed cognitive function in snorers and sleep apneics. An epidemiological study of 1,504 females and males aged 30-60 years: the Dan-MONICA II Study. Eur Neurol. 1994;34:204–8. doi: 10.1159/000117039. [DOI] [PubMed] [Google Scholar]
- 20.Ameratunga SN, Norton RN, Whitlock G, et al. The New Zealand Blood Donors' Health Study: baseline findings of a large prospective cohort study of injury. Inj Prev. 2002;8:66–9. doi: 10.1136/ip.8.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilsmore BR, Grunstein RR, Fransen M, Woodward M, Norton R, Ameratunga S. Sleep, blood pressure and obesity in 22,389 New Zealanders. Intern Med J. 2012;42:634–41. doi: 10.1111/j.1445-5994.2012.02753.x. [DOI] [PubMed] [Google Scholar]
- 22.Ameratunga SN, Norton RN, MacMahon SW, et al. A prospective cohort study of blood donors: methodological issues in the investigation of injuries and chronic diseases. Aust N Z J Public Health. 1998;22:578–82. doi: 10.1111/j.1467-842x.1998.tb01442.x. [DOI] [PubMed] [Google Scholar]
- 23.American Academy of Sleep Medicine. The international classification of sleep disorders, revised: diagnostic and coding manual (ICSD) Chicago, IL: American Academy of Sleep Medicine; 2001. [Google Scholar]
- 24.Ohayon MM. Prevalence of DSM-IV diagnostic criteria of insomnia: distinguishing insomnia related to mental disorders from sleep disorders. J Psychiatr Res. 1997;31:333–46. doi: 10.1016/s0022-3956(97)00002-2. [DOI] [PubMed] [Google Scholar]
- 25.Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131:1121–3. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- 26.Bush B, Shaw S, Cleary P, Delbanco TL, Aronson MD. Screening for alcohol abuse using the CAGE questionnaire. Am J Med. 1987;82:231–5. doi: 10.1016/0002-9343(87)90061-1. [DOI] [PubMed] [Google Scholar]
- 27.Kitchens JM. Does this patient have an alcohol problem? JAMA. 1994;272:1782–7. [PubMed] [Google Scholar]
- 28.Ohayon MM, Smirne S. Prevalence and consequences of insomnia disorders in the general population of Italy. Sleep Med. 2002;3:115–20. doi: 10.1016/s1389-9457(01)00158-7. [DOI] [PubMed] [Google Scholar]
- 29.Tani P, Lindberg N, Nieminen-von Wendt T, et al. Insomnia is a frequent finding in adults with Asperger syndrome. BMC Psychiatry. 2003;3:12. doi: 10.1186/1471-244X-3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rocha FL, Guerra HL, Lima-Costa MF. Prevalence of insomnia and associated socio-demographic factors in a Brazilian community: the Bambui study. Sleep Med. 2002;3:121–6. doi: 10.1016/s1389-9457(01)00119-8. [DOI] [PubMed] [Google Scholar]
- 31.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 32.Health Mo. Wellington: Ministry of Health; 2004. A portrait of health: key results of the 2002/03 New Zealand health survey. [Google Scholar]
- 33.Buchsbaum DG, Buchanan RG, Centor RM, Schnoll SH, Lawton MJ. Screening for alcohol abuse using CAGE scores and likelihood ratios. Ann Intern Med. 1991;115:774–7. doi: 10.7326/0003-4819-115-10-774. [DOI] [PubMed] [Google Scholar]
- 34.Olson LG. A community survey of insomnia in Newcastle. Aust N Z J Public Health. 1996;20:655–7. doi: 10.1111/j.1467-842x.1996.tb01083.x. [DOI] [PubMed] [Google Scholar]
- 35.Hetta J, Broman JE, Mallon L. Evaluation of severe insomnia in the general population--implications for the management of insomnia: insomnia, quality of life and healthcare consumption in Sweden. J. Psychopharmacol (Oxf) 1999;13:S35–6. doi: 10.1177/026988119901304S10. [DOI] [PubMed] [Google Scholar]
- 36.Doi Y, Minowa M, Okawa M, Uchiyama M. Prevalence of sleep disturbance and hypnotic medication use in relation to sociodemographic factors in the general Japanese adult population. J Epidemiol. 2000;10:79–86. doi: 10.2188/jea.10.79. [DOI] [PubMed] [Google Scholar]
- 37.Leger D, Guilleminault C, Dreyfus JP, Delahaye C, Paillard M. Prevalence of insomnia in a survey of 12,778 adults in France. J Sleep Res. 2000;9:35–42. doi: 10.1046/j.1365-2869.2000.00178.x. [DOI] [PubMed] [Google Scholar]
- 38.Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment. Prevalence and correlates. Arch Gen Psychiatry. 1985;42:225–32. doi: 10.1001/archpsyc.1985.01790260019002. [DOI] [PubMed] [Google Scholar]
- 39.Liljenberg B, Almqvist M, Hetta J, Roos BE, Agren H. The prevalence of insomnia: the importance of operationally defined criteria. Ann Clin Res. 1988;20:393–8. [PubMed] [Google Scholar]
- 40.Weyerer S, Dilling H. Prevalence and treatment of insomnia in the community: results from the Upper Bavarian Field Study. Sleep. 1991;14:392–8. [PubMed] [Google Scholar]
- 41.Quintana-Gallego E, Carmona-Bernal C, Capote F, et al. Gender differences in obstructive sleep apnea syndrome: a clinical study of 1166 patients. Respir Med. 2004;98:984–9. doi: 10.1016/j.rmed.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 42.Ohayon MM, Hong SC. Prevalence of insomnia and associated factors in South Korea. J Psychosom Res. 2002;53:593–600. doi: 10.1016/s0022-3999(02)00449-x. [DOI] [PubMed] [Google Scholar]
- 43.Ohayon MM, Caulet M, Guilleminault C. How a general population perceives its sleep and how this relates to the complaint of insomnia. Sleep. 1997;20:715–23. doi: 10.1093/sleep/20.9.715. [DOI] [PubMed] [Google Scholar]
- 44.Yeo BK, Perera IS, Kok LP, Tsoi WF. Insomnia in the community. Singapore Med J. 1996;37:282–4. [PubMed] [Google Scholar]
- 45.Kageyama T, Kabuto M, Nitta H, et al. Prevalence of use of medically prescribed hypnotics among adult Japanese women in urban residential areas. Psychiatry Clin Neurosci. 1998;52:69–74. doi: 10.1111/j.1440-1819.1998.tb00975.x. [DOI] [PubMed] [Google Scholar]
- 46.Vorona RD, Winn MP, Babineau TW, Eng BP, Feldman HR, Ware JC. Over-weight and obese patients in a primary care population report less sleep than patients with a normal body mass index. Arch Intern Med. 2005;165:25–30. doi: 10.1001/archinte.165.1.25. [DOI] [PubMed] [Google Scholar]
- 47.Trinder J. Subjective insomnia without objective findings: a pseudo diagnostic classification? Psychol Bull. 1988;103:87–94. doi: 10.1037/0033-2909.103.1.87. [DOI] [PubMed] [Google Scholar]
- 48.Shin C, Joo S, Kim J, Kim T. Prevalence and correlates of habitual snoring in high school students. Chest. 2003;124:1709–15. doi: 10.1378/chest.124.5.1709. [DOI] [PubMed] [Google Scholar]
- 49.Hui DS, Chan JK, Ko FW, et al. Prevalence of snoring and sleep-disordered breathing in a group of commercial bus drivers in Hong Kong. Intern Med J. 2002;32:149–57. doi: 10.1046/j.1444-0903.2001.00196.x. [DOI] [PubMed] [Google Scholar]
- 50.Zielinski J, Zgierska A, Polakowska M, et al. Snoring and excessive daytime somnolence among Polish middle-aged adults. Eur Respir J. 1999;14:946–50. doi: 10.1034/j.1399-3003.1999.14d36.x. [DOI] [PubMed] [Google Scholar]
- 51.Nugent AM, Gleadhill I, McCrum E, Patterson CC, Evans A, MacMahon J. Sleep complaints and risk factors for excessive daytime sleepiness in adult males in Northern Ireland. J Sleep Res. 2001;10:69–74. doi: 10.1046/j.1365-2869.2001.00226.x. [DOI] [PubMed] [Google Scholar]
- 52.Goncalves MA, Paiva T, Ramos E, Guilleminault C. Obstructive sleep apnea syndrome, sleepiness, and quality of life. Chest. 2004;125:2091–6. doi: 10.1378/chest.125.6.2091. [DOI] [PubMed] [Google Scholar]
- 53.Hara C, Lopes Rocha F, Lima-Costa MF. Prevalence of excessive daytime sleepiness and associated factors in a Brazilian community: the Bambui study. Sleep Med. 2004;5:31–6. doi: 10.1016/j.sleep.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 54.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–84. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- 55.Teculescu D, Guillemin F, Virion JM, et al. Reliability of the Wisconsin Sleep Questionnaire: a French contribution to international validation. J Clin Epidemiol. 2003;56:436–40. doi: 10.1016/s0895-4356(03)00029-5. [DOI] [PubMed] [Google Scholar]
- 56.Hoffstein V, Mateika S, Anderson D. Snoring: is it in the ear of the beholder? Sleep. 1994;17:522–6. doi: 10.1093/sleep/17.6.522. [DOI] [PubMed] [Google Scholar]
- 57.Olson LG, King MT, Hensley MJ, Saunders NA. A community study of snoring and sleep-disordered breathing. Prevalence. Am J Respir Crit Care Med. 1995;152:711–6. doi: 10.1164/ajrccm.152.2.7633731. [DOI] [PubMed] [Google Scholar]
- 58.Ohayon MM, Guilleminault C, Priest RG, Caulet M. Snoring and breathing pauses during sleep: telephone interview survey of a United Kingdom population sample.[see comment] BMJ. 1997;314:860–3. doi: 10.1136/bmj.314.7084.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Franklin KA, Gislason T, Omenaas E, et al. The influence of active and passive smoking on habitual snoring. Am J Respir Crit Care Med. 2004;170:799–803. doi: 10.1164/rccm.200404-474OC. [DOI] [PubMed] [Google Scholar]
- 60.Kessler RC, Andrews G, Mroczek D, Üstün TB, Wittchen H-U. The World Health Organization Composite International Diagnostic Interview Short Form (CIDISF) Int J Methods Psychiatr Res. 1998;7:171–85. [Google Scholar]


