Abstract
Study Objectives:
Research suggests that rumination may play an important role in insomnia. Whereas some have suggested that rumination mainly relates to depression, the evidence suggests that there may be insomnia-specific rumination. This paper explores insomnia symptom rumination across two distinct samples of varying levels of depressed mood and insomnia symptom severity.
Methods:
The first sample consisted of nonclinical participants (N = 327) with a range of insomnia and depressed mood symptoms, and the second sample consisted of those who met both Major Depressive Disorder and Insomnia diagnoses (N = 66). Rather than relying on a measure developed for those with depression, we developed and tested an insomnia-specific measurement scale based on items from previous rumination studies and the addition of items derived from common daytime insomnia symptoms.
Results:
Internal consistency was highly acceptable across the two samples for the new insomnia-specific rumination measure (Cronbach α was 0.93 and 0.94). In the first study, poor sleepers reported significantly higher levels of daytime symptom rumination than did good sleepers. Across both studies, rumination about daytime insomnia symptoms and depression were signifi-cantly correlated; however, insomnia rumination scores predicted insomnia even after controlling for depression. Moreover, in Study 2, insomnia-specific rumination was related to insomnia, but general depressive rumination was not predictive of insomnia.
Conclusions:
The findings provide support for the use of this insomnia-specific rumination scale; moreover the findings support previous observances regarding rumination about daytime insomnia symptoms that are not exclusive to depression.
Citation:
Carney CE; Harris AL; Falco A; Edinger JD. The relation between insomnia symptoms, mood, and rumination about insomnia symptoms. J Clin Sleep Med 2013;9(6):567-575.
Keywords: Rumination, insomnia, cognition, depression, cognitive risk
Repetitive thought is an important process that pervades across many disorders.1 Rumination is one such repetitive thought process, which is focused on past failure or the cause of current distress and typically occurs within the context of Major Depressive Disorder.2–4 Whereas rumination is most often associated with depression, it likely plays a role in other disorders as well, especially in those disorders that share similar symptomatology with depression. In particular, insomnia has many overlapping symptoms with depression, such as sleep difficulties, low energy, difficulty concentrating, low mood, and suicidality.5 Further, insomnia and depression are highly comorbid with one another.6 Thus, perhaps rumination plays an important role in insomnia.
As is the case with depression, research has supported a role for cognitive processes in maintaining insomnia.7–10 Harvey's Cognitive Model of Insomnia posits that those with sleep difficulties can suffer from repetitive thinking throughout the 24-hour period.7 This negatively toned mental activity usually focuses on worries about not getting enough sleep and whether it will be possible to function adequately during the following day while suffering from daytime symptoms of insomnia (e.g., fatigue, disturbed mood, concentration difficulties). Such repetitive thought can perpetuate further emotional arousal, and this cycle is thought to perpetuate insomnia. While certain repetitive thought processes, such as worry, have been explored in great depth within the context of insomnia,11,12 rumination has not received the same degree of attention with respect to its role in sleep disturbance. In the recent past, rumination and worry were used as interchangeable terms, but the content of these two repetitive thought processes are thought to be different (see Carney13 for discussion). Worry is most often associated with thinking about future consequences, e.g., what is going to happen tomorrow if I feel this way?”; whereas rumination is most often concerned with what is causing the current problem; that is, rumination is most often oriented to the past, e.g., “Why am I feeling this way?” Also, worry is more often associated with anxiety whereas rumination is more likely to occur with dysphoria. Whereas other repetitive thought processes, such as worry, have been shown to be sleep-disruptive factors in insomnia,11 worry and rumination are separate but related factors. For example, our previous study suggested that rumination and worry are distinct constructs since rumination was significantly related to insomnia severity, while worry was not.14 Despite these observations, there have been no previous efforts to develop an insomnia-specific rumination measure.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Insomnia-specific rumination is a process in which there is repetitive thought about the symptoms of insomnia, such as fatigue. A few studies have found that rumination in insomnia is not merely a depressive process. The current study tested an insomnia-specific rumination measure in two distinct samples, including a sample of adults with clinical insomnia, and found similar support for insomnia-specific rumination that is distinct from depressive rumination.
Study Impact: The corroboration of previous findings showing that there is rumination in insomnia, distinct from that found in depression, suggests that rumination-targeted treatments are worthy of investigation in those with insomnia.
Recently, emerging studies have supported the link between rumination and sleep. In an undergraduate sample, there were significant associations between rumination and subjective sleep quality.15 Similarly, Carney and colleagues found a difference between good and poor sleepers on their tendency to ruminate when feeling low, and this difference was not accounted for by dysphoria.13 Good and poor sleepers did not differ on other rumination-related constructs, such as distraction (e.g., distracting yourself from depression by doing something fun with a friend) or self-focused rumination (e.g., asking yourself, “why am I reacting this way?”); they differed on a tendency to ruminate on dysphoric symptoms (e.g., thinking about how hard it is to concentrate) only. Thus, whereas those with depression and other disorders are characterized by increased self-focused rumination, those with poor sleep react with repetitive thought in response to insomnia symptoms. Thus, the construct of rumination and more specifically, symptom-focused rumination appears to be a key concept in insomnia.
The rumination characteristic in insomnia focuses on thinking repeatedly about daytime problems, such as poor concentration, low motivation, and low energy. Although insomnia is typically associated with nighttime pathology, a particularly prominent complaint is the resultant daytime fatigue.16 This daytime pathology, characterized by fatigue, cognitive complaints and low mood, can interfere with daily functioning. Thinking repeatedly about what caused daytime symptoms such as fatigue and poor concentration, can reinforce beliefs of poor sleep self-efficacy, increase anxiety about solving one's sleep problem, and may lead to maladaptive safety behaviors (e.g., spending more time in bed).7 However, the current lack of an instrument to measure the symptom-focused rumination process in insomnia limits our ability to scrutinize the role this process plays in perpetuating this form of sleep disorder. Hence, the current series of two studies reported herein describe our efforts to develop and test an insomnia-specific symptom focused rumination scale that includes the common range of daytime symptoms that preoccupy insomnia sufferers. In Study 1, we describe the item content of the scale and report results of psychometric testing with a large sample of mixed good and poor sleepers. We also report our findings in regard to its relationship with other measures of insomnia controlling for coincident levels of depressed mood. In Study 2, we further tested the psychometric properties and predictive validity of our instrument in a sample of individuals with comorbid insomnia and depressive disorders. Our aim was to test the general hypothesis that daytime symptom focus is independently predictive of insomnia over and above what insomnia symptoms might be predicted from coincident levels of depressive mood.
STUDY 1—METHODS
Participants
The participants consisted of 327 (82% female) undergraduate students enrolled in an introductory psychology course at Ryerson University. Participants ranged in age from 18-49 years (mean = 20.38, SD = 4.60). The students were recruited via SONA, the Psychology Department's online system. Students who were interested in participating in this study volunteered to participate in partial fulfillment of their introductory psychology course requirements.
Measures
Daytime Insomnia Symptom Response Scale (DISRS)14
Given the emerging evidence for rumination in insomnia, it was important to develop a sleep-specific measure to assess ruminative tendencies in insomnia populations. The rumination measure used in previous studies of sleep and rumination13,14 was the Symptom-Focused Rumination Subscale (SYM)17 from the Response Styles Questionnaire (RSQ).18 The SYM queries the degree to which one responds to feeling low, with repetitive thinking about: “how hard it is to concentrate” or “feelings of fatigue and achiness.” While these items are associated with depression, they also are common daytime complaints in those with insomnia. Indeed, research has supported that there is substantial overlap between symptoms in depression and those found in insomnia.5 Given that the SYM is a validated subscale from a validated rumination measure and studies suggested that it was particularly useful in those with disrupted sleep, this 8-item subscale served as the starting point for developing the DISRS. All but one of the 8 original SYM items were retained for inclusion in the new scale. The excluded item from the SYM related to anhedonia (e.g., “Think about how you don't seem to feel anything anymore”), a cardinal symptom of depression, and one which discriminates between individuals with and without depression.5 Another item contained in the SYM was a compound item (“Think about your feelings of fatigue and achiness”); this was divided into 2 items (i.e., think about feelings of fatigue” and “think about how achy you feel”) on the DISRS, as these are 2 distinct symptoms of insomnia. Twelve additional items based on daytime symptoms of insomnia were generated by the first author, based on daytime symptoms of insomnia reported elsewhere, including the daytime symptoms listed in Research Diagnostic Criteria for Insomnia.19 The items were sent to an expert in insomnia (J.D.E), who provided feedback and approved the items. The result was a 20-item scale in which people are asked how frequently they engage in the behaviors listed when feeling tired, on a 4-point scale ranging from 1 (Almost Never) to 4 (Almost Always). The scale is scored by adding the items and total scores range from 20 to 80, with higher scores indicating higher levels of rumination.
The Insomnia Severity Index (ISI)
The ISI20 is well validated and commonly recommended self-report measure for assessing the severity of insomnia symptoms.21 It includes 7 items which measure insomnia symptom severity on a 5-point scale ranging from 0 (Not at All) to 4 (Extremely). The ISI score is obtained by adding the individual item scores, resulting in possible values ranging from 0 to 28; within this range, higher scores indicate greater insomnia severity. The ISI has good internal consistency (Cronbach α = 0.91) and test-retest reliability (r = 0.80). The ISI also demonstrates good concurrent validity, as it correlates with sleep diary measures and polysomnography.22 A score ≥ 8 has been shown to differentiate good sleepers from those with insomnia symptoms22 and was used as the division between good and poor sleepers in this study.
The Beck Depression Inventory, Second Edition (BDI-II)
The BDI-II23 is a 21-item self-report measure that assesses common depressive symptoms, such as depressed mood, hopelessness, suicidal ideation, sleep disturbance, and appetite change. Total scores range from 0 to 63, with higher scores indicating a greater degree of depression. The BDI-II has very good internal consistency (split half Pearson = 0.93). It also has well-established content validity and is good at differentiating between depressed and non-depressed individuals.23,24 The BDI-II has been used and validated in insomnia patients; however, there is reason to be cautious in using the BDI-II among those with insomnia because of the high number of non-discriminating items such as those querying insomnia and fatigue.5 For the purposes of this study, the highly overlapping insomnia and fatigue items were removed from the total BDI-II score.
Fatigue Severity Scale (FSS)
The FSS25 is a 9-item scale which is used to measure fatigue symptoms. Items are scored along a 7-point Likert scale ranging from 1 (Strongly Agree) to 7 (Strongly Disagree). The FSS total score is the average of the 9 individual items. The scale has good psychometric properties, as demonstrated by good internal consistency (Cronbach α = 0.94) and good test-retest reliability.25,26
Penn State Worry Questionnaire-Past Week (PSWQ-PW)
The PSWQ-PW27 is an abbreviated version of the original 16-item PSWQ, a common tool which measures the generality, excessiveness, and uncontrollability components of worry. The PSWQ-PW contains 15 items and specifically measures state worry over the past week. Sample items include, “my worries overwhelmed me” and “I worried about projects until they were done.” The PSWQ-PW has good internal consistency (Cron-bach α = 0.91) and is highly correlated with other state measures of worry.27
Procedure
After consenting to participate, participants completed a brief demographic information form, the DISRS, BDI-II, ISI, FSS, and PSWQ.
STUDY 1—RESULTS
To test for multivariate normality, histograms were conducted for each of the DISRS items, and all items showed normal distributions. Outliers were screened by obtaining z values for each of the items, and data points were flagged if they had a value exceeding |3.29|.28 There were no outliers in this sample, and all data points were well within 3 standard deviations of the mean.
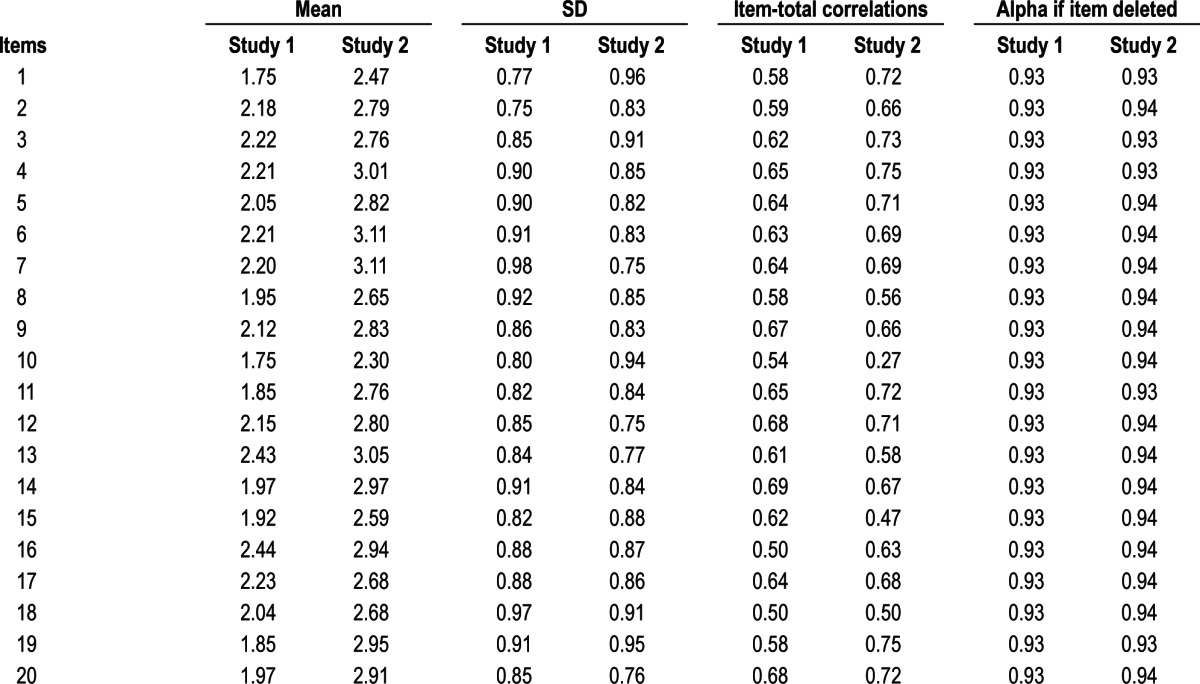
The means and standard deviations for each DISRS item are displayed in Table 1. The mean score on the DISRS in this sample was 41.43, with a standard deviation of 11.42 and a median score of 40. The total scores ranged from 20 to 75 across the sample, with 20 being the minimum possible score and 80 being the highest possible score. The skewness and kurtosis values were 0.30 and -0.48, respectively, well within the |2| and |7| cutoff scores, respectively.29 The internal consistency, as measured by Cronbach α was 0.93. The item-total statistics are displayed in Table 1. The item-total correlations range from 0.50 to 0.69, which indicates that each item is adequately correlated with the total scale. In addition, the Cronbach α if item deleted statistics did not suggest that any DISRS item should be removed.
Table 1.
Descriptive and item-total statistics
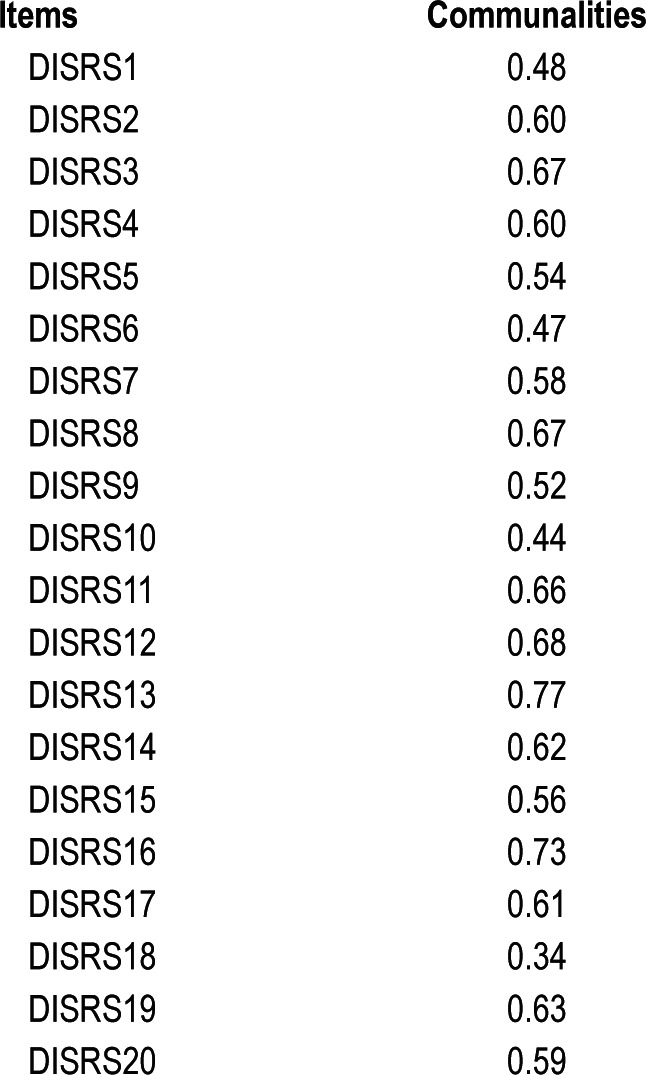
An exploratory factor analysis (EFA) was conducted to examine the factor structure of the DISRS. The communalities ranged from 0.34 to 0.77 (as shown in Table 2), but most were within the 0.5 to 0.6 range (mean = 0.59). The inter-item correlation matrix was examined, and most of the correlations ranged from 0.3 to 0.6. There were no correlations greater than 0.8, indicating that multicollinearity is not likely to be a problem.30 The Kaiser-Meyer-Olkin Measure of Sampling Adequacy was 0.94 suggested that the sample size is adequate.31 Bartlett's test of sphericity [χ2(190) = 3,265.78, p = < 0.001] is significant, indicating that there is a relationship between the variables, and that the correlations are significantly different from zero.30 The EFA was conducted with a principle component extraction method. The rotated factor matrix was obtained using the direct oblimin rotation, a type of oblique rotation, given that all the items, and thus the components, should be correlated with one another, based on previous research.17,18
Table 2.
DISRS communalities for exploratory factor analysis
The EFA revealed a 3-factor solution according to Kaiser's (1960) criteria. The 3 factors together explain 58.12% of the total variance, and all of the Eigenvalues were > 1.32 The factor loadings for the pattern matrix are displayed in Table 3. All of the factor loadings were > 0.4, a level which meets the current recommended criterion.33 The first factor explains 43.38% of the variance (Eigenvalue = 8.77) and appeared to reflect cognitive and motivation complaints. The second factor, which accounts for 8.54% of the variance (Eigenvalue = 1.71), appeared to relate to negatively valenced state symptoms (e.g., lack of energy, achiness, low mood, irritability). The third factor, accounting for 6.21% of the variance (Eigenvalue = 1.24), consisted of items related to feeling tired. Table 4 displays the correlations between each of the 3 factors.
Table 3.
Factor loadings of exploratory factor analysis with oblique rotation of the DISRS
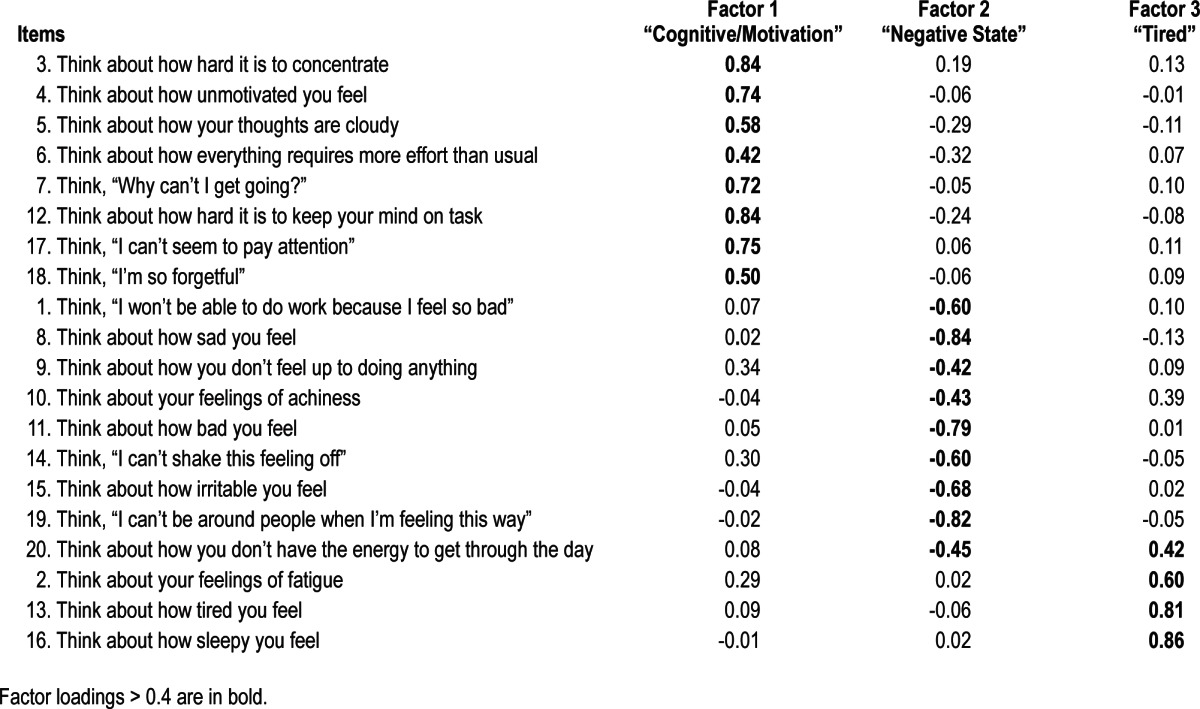
Table 4.
Component correlation matrix

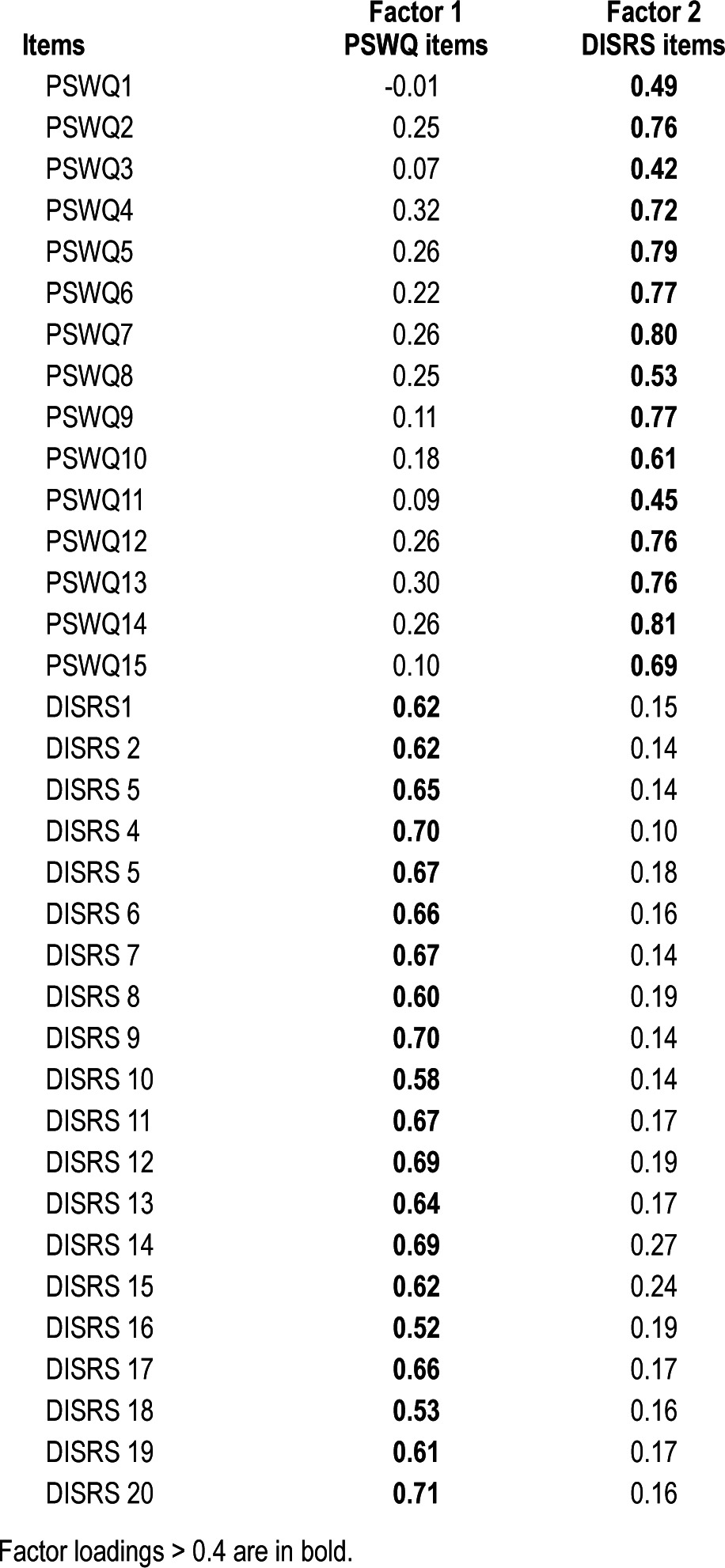
To investigate the relation between the DISRS and constructs that theoretically should relate, Pearson product moment correlation coefficients were calculated. The DISRS positively correlated with insomnia severity (ISI) and fatigue (FSS). The means and standard deviations of these measures are shown in Table 5, along with their correlations with the DISRS. An analysis of variance (ANOVA) confirmed that good sleepers (mean = 36.7, SD = 10.9) had significantly lower DISRS scores than poor sleepers (mean = 44.1, SD = 10.8), F1,323 = 34.69, p < 0.001. Discriminant validity is also of importance, particularly with respect to worry, a construct which is theoretically distinct from that of rumination. In order to determine whether the 2 measures were indeed conceptually distinct from one another, we conducted a factor analysis of the DISRS and PSWQ items using a varimax rotation and extracting 2 factors. The rotated matrix can be seen in Table 6. The varimax rotated factor matrix was obtained using the maximum likelihood extraction method. The 2 factors together explain 47.5% of the total variance, and each of the Eigenvalues were > 1. The first factor explained 12.6% of the variance and contains the DISRS rumi-nation items, which load exclusively on this factor. The second factor, which accounted for 4.0% of the variance, contains the worry items from the PSWQ.
Table 5.
Descriptive statistics and correlations for convergent validity measures
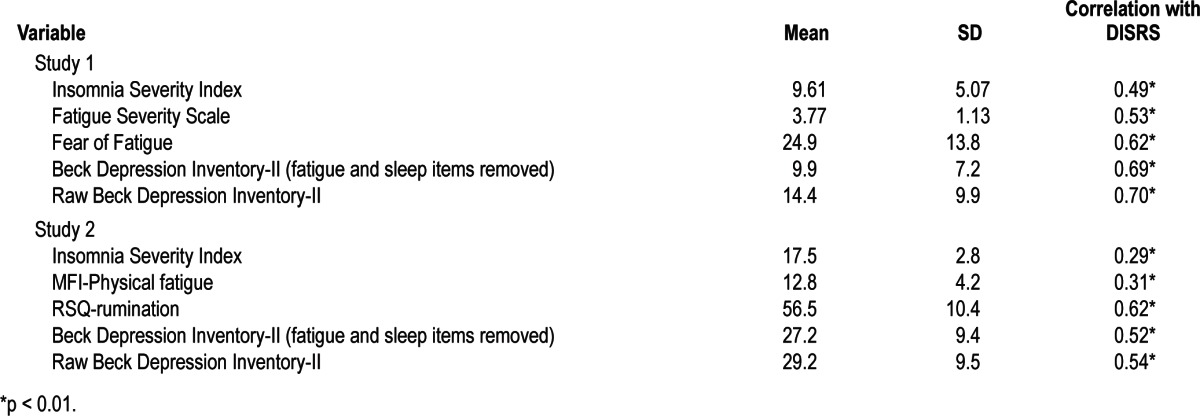
Table 6.
Factor loadings of confirmatory factor analysis with varimax rotation of PSWQ and DISRS items
The multiple regression found that DISRS significantly predicted the ISI (β = 0.493; p < 0.001) and accounted for 24% of the variance. Adding the BDI-II without sleep and fatigue items (β = 0.296; p < 0.001) to the DISRS added marginally to the prediction (R2 change = 0.04; F change score = 0.001); together, depression and rumination accounted for 28% of the variance. The interaction of daytime insomnia symptom rumination and depressed mood was not significant (p = 0.618). That is, the contribution of rumination and depression to insomnia is not cumulative, but rather they each contribute to the variance independently.
Summary
There was good evidence for internal consistency of the measure, as supported by both Cronbach α and the item-total correlations. The factor analysis suggests that rumination in insomnia is multidimensional and reflects three domains: rumination about cognitive and motivation problems, negative emotions, and fatigue. Items from the PSWQ loaded exclusively onto the same factor and rumination items loaded onto a separate factor. There was greater rumination about insomnia in those with higher levels of self-reported sleep disturbance. As predicted, insomnia rumination predicted insomnia severity and was not moderated by depression.
STUDY 2—METHODS
Participants
This study recruited 66 men and women (67% female) aged 20-65 years old (mean = 41.5; SD = 11.8), with complaints of both depression and insomnia (NIH R01-MH076856), solicited from clinics and media advertisements. Sixty-three percent of the sample were Caucasian, 15% did not specify their race/ ethnicity, 13% were African American, and 9% were Asian American. These data were collected as part of the baseline measurement package obtained in a larger clinical trial to treat insomnia and depression. Participants were included if they were in good health (determined by medical and psychiatric history, and a physical examination), had insomnia (i.e., met Research Diagnostic Criteria19 for an Insomnia Disorder on the Duke Structured Interview of Sleep Disorders [DSISD],34 had a score ≥ 15 on the Insomnia Severity Index, showed a mean sleep diary total wake time ≥ 60 min/night and a mean sleep diary sleep efficiency [SE = (total sleep time ÷ time in bed) × 100%] < 85% during a one-week screening period), and met criteria for a Major Depressive Episode (without psychotic features) on the mood module of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID)35 along with a score ≥ 15 on the 17-item Hamilton Rating Scale for Depression (HAMD).36 Those who had conditions thought to interfere with insomnia or depression treatment were excluded (e.g., those with Obsessive Compulsive Disorder with intrusive nighttime rituals, those with frequent nocturnal panic). Additionally, those who met criteria for sleep apnea, restless legs syndrome or Circadian Rhythm Sleep Disorder on the basis of the Duke Structured Interview of Sleep Disorders, and/or those with an apnea-hypopnea index ≥ 15 or periodic limb movement-related arousal index ≥ 15/h of sleep during a screening laboratory polysomnogram were also excluded. Those who were hypnotic dependent (i.e., they reported that they were unwilling or unable to abstain from prescription medications for sleep during an 8-week treatment phase of the study) were also excluded from participation.
Measures
In addition to the DISRS, ISI, and BDI-II, which were used in the previous study, this study used a more comprehensive measure of fatigue, the Multidimensional Fatigue Inventory (MFI), rather than the FSS.
The Multidimensional Fatigue Inventory (MFI)
The MFI is a 20-item scale to assess dimensions of fatigue, including: general, physical, mental, reduced motivation, and reduced activity.37 These 5 dimensions represent distinct sub-scales of the MFI. Responses range on a 5-point scale from (yes, that is true) to (no, that is not true). The MFI has good internal consistency (Cronbach α = 0.84) and adequate convergent validity, as it has been found to be correlated with visual analog scales measuring fatigue.37 Along with the FSS, the MFI is also a recommended self-report measure for the assessment of fatigue in insomnia studies.21 For comparability to the first study, the Physical Fatigue subscale was used for this study.
Procedures
All study procedures were approved by the Ryerson University Research Ethics Board. Study candidates telephoned the Project Coordinator (PC) in response to study advertising (i.e., advertisements, brochures in clinics), and the PC scheduled an in-lab screening interview. At the screening interview, the participants were told about the study and provided informed consent. After the consent process, participants were interviewed by master's or doctoral level psychology students with the Duke Structured Interview for Sleep Disorders (DSISD) and the Structured Clinical Interview for DSM disorders (SCID), and they also completed an ISI. Those who met initial entry criteria for depression on the SCID, and insomnia criteria on the DSISD and ISI (≥ 15) were scheduled for (a) a standard medical evaluation that included a physical examination, as well as a Hamilton Rating Scale for Depression (HAMD-17), (b) one night of PSG monitoring, and (c) one week of sleep log monitoring. Those who met entry criteria completed a battery of questionnaires, including the measures of interest for this study: the BDI-II, ISI, Dysfunctional Beliefs and Attitudes about Sleep (DBAS-16), DISRS, Response Styles Questionnaire (RSQ), and MFI. Those who continued to meet all study selection criteria for the parent study were randomized into treatment groups for an 8-week treatment phase wherein combinations of insomnia and depression treatments were tested. The parent study is ongoing and the study variables might be affected by treatment; thus, the present study reports on the baseline measures only.
Because of the relationship between rumination and depression in the previous studies, a regression analysis was conducted to determine whether daytime insomnia symptom rumination predicted insomnia severity and whether depression added any predictive value. The DISRS was entered as a predictor of ISI in the first step of a multiple regression. The BDI-II was added in the second step. Self-focused rumination (e.g., asking myself “why am I reacting this way?”) (shown in previous studies to relate to depression but not insomnia) was added in the next step, to determine if in a comorbid mood sample this form of daytime symptom-focused rumination is important. In the last step, an interaction term was added to test whether the rumination-specific prediction was accounted for by its interaction with depression.
STUDY 2—RESULTS
There were no outliers, and all data points were within 3 standard deviations of the mean. The DISRS mean was 56.2 (SD = 11.6), the median was 55.5, and scores ranged from 29-78. Cronbach α was 0.94. The skewness and kurtosis values (-0.13 and -0.63, respectively) were both within published acceptable cutoff scores.29 To investigate construct validity, we calculated the bivariate (i.e., Pearson product moment) correlation between the DISRS and daytime fatigue severity, as well as with sleep, general rumination, and depressed mood. The DISRS positively correlated with all of these related measures. The means, standard deviations, and correlations are shown in Table 5. The multiple regression found that the DISRS significantly predicted the ISI (Adjusted R Square = 0.07, β = 0.285; p = 0.02). Adding the BDI-II without sleep and fatigue items to the DISRS did not add to the prediction over and above rumination alone (F change 1,63 = 0.114, p = 0.74). Adding a depression-specific rumination scale (i.e., self-focused rumination) did not predict insomnia (F change 1,62 = 0.854, p = 0.36). The interaction of daytime insomnia symptom rumination and depressed mood was not statistically significant (F change 1,61 = 2.849, p = 0.10).
Summary
There was evidence of good internal consistency in this sample. In support of its validity, there were significant correlations with related constructs such as fatigue, mood disturbance, and general rumination. As expected, self-focused rumination, a form of rumination found in previous studies to be depression-specific, was not predictive of insomnia severity. Insomnia rumination was a predictor of insomnia severity and this was not accounted for by the interaction of depressed mood severity and rumination.
DISCUSSION
Symptom-focused rumination was characteristic of those with disturbed sleep; a finding consistent with several other earlier studies.13,14 Evidence for rumination in those with sleep disturbance also is consistent with Harvey's cognitive model.7 The model asserts that the repetitive thought process seen at night (e.g., worry about not sleeping) can occur during the day (e.g., thinking repeatedly about why one is feeling so tired). Namely, that the activation of thoughts and emotions relevant to the insomnia process, e.g., reflecting on the level of daytime fatigue after a poor night's sleep and feeling upset about it increases subsequent, selective monitoring for evidence of consequences of poor sleep. Such a process increases the likelihood of perceiving such daytime symptoms, which is presumed to lead to increase distress about the insomnia problem and further perpetuates sleep problems. This heightened level of distress may also stimulate activation of the sympathetic nervous system, due to the perceived threat to well being. This, in turn, could lead to increased arousal, as demonstrated in the chronic hyper-arousal model of insomnia38 and the caffeine model of insomnia.39 This study was not designed to test the paths of all these components, but the data are supportive of aspects of these purported processes. Perhaps the best articulated description of this process in insomnia is seen in Espie's Attention-Intention Effort model.40 That is, as one increases attention for daytime threats (e.g., fatigue or concentration problems) associated with the sleep problem, there is resultant effort in trying to “solve” the sleep problem. Rumination is commonly conceptualized as an (ineffective) problem-solving attempt41; future studies could more definitively test whether rumination in insomnia can be conceptualized as an example of sleep effort. In these samples, there were increased ruminative tendencies associated with increased sleep disturbance and mood problems, and Espie and colleagues have reported increased sleep effort in those with comorbid mood problems as compared to those with insomnia only.42 This is particularly worrisome as rumination has been shown to be a difficult process to stop and is an important predictor of depression.43 It is a repetitive thought process that limits the processing of outside, disconfirming information; that is, someone with a propensity to think negatively would have difficulty integrating more positive information that might disconfirm their deeply ingrained negative beliefs. The current study suggests that those with sleep problems respond to the daytime sequelae of insomnia by thinking about how much it bothers them and this tendency predicts insomnia severity. It has been well established that insomnia increases the risk for episodes of depression44; perhaps this common risk factor (i.e., rumination) may be one route by which insomnia increases depressive risk. The possibility of a shared cognitive risk pathway between insomnia and depression could be evaluated in future studies.
While insomnia severity and rumination were correlated in both studies, the size of the relationship between rumination and sleep was smaller in the clinical comorbid sample. Perhaps this may be related to the presence of depression in this sample. However, in the depressed sample, the unique contribution of insomnia symptom rumination to insomnia symptom severity is interesting. Other forms of rumination, namely self-focused rumination, were not related to insomnia severity, thus the content of the rumination was the same as it is in insomnia populations, even when there was a comorbid major depressive disorder. This supports Watkins' idea suggesting that the repetitive thought process may be trans-diagnostic, albeit the content of the rumination may differ across axis I disorders.45 Another possible explanation is that those with a comorbid mood problem may have a different array of perpetuating mechanisms that explain their insomnia. Psychological variables appear to relate differently to sleep in those with comorbid insomnias as opposed to those with insomnia only.46 Future research should continue to explore the role of rumination in those with primary diagnoses of insomnia and depression, in addition to the comorbid populations. Another important finding in the current paper is the support for an insomnia-specific measure. The Daytime Insomnia Symptom Response Scale exhibited similarly reliable characteristics across the two samples, as measured by an internal consistency estimate (Cronbach alphas were > 0.9). Further, the item-total correlations and the alphas if item deleted analyses in Study 1, suggest that there are no items that are considered poor. As such, the internal reliability of the DISRS for use in those with a range of sleep and mood problems is highly acceptable. The confirmatory factor analysis of DISRS and PSWQ items re-confirms that insomnia-based rumination and worry are indeed distinct constructs with respect to content.14 Correlations between the DISRS and other related measures, along with the finding that the DISRS predicts insomnia severity, supports the convergent validity of the scale for use in those with a range of insomnia symptoms. Given that the DISRS was evaluated against other validated questionnaires in order to establish convergence, future research could evaluate the DISRS with other tests that do not share method variance, i.e., without relying solely on self-report questionnaires.
While these constructs demonstrate appropriate degrees of convergent validity, the correlation between rumination and depression (r = 0.71) was high in those with preclinical levels of depression and insomnia, and was moderately high in those with clinical insomnia and MDD (r = 0.52). Given that rumination is a construct implicated in the etiology of depression, and that some of the items were taken from a depression-specific rumination scale (i.e., the symptom-focused rumination scale of the RSQ), it is not surprising that insomnia-symptom rumi-nation is correlated with depression. This may be a nosologic rather than a psychometric issue, as the daytime symptoms of insomnia overlap substantially with symptoms of depression, and depression inventories are confounded by insomnia symptom items.5 Nonetheless the prediction of insomnia by insomnia rumination was not moderated by depression, so rumination in insomnia is not a mere vestige of mood pathology.
Alternatively, one could consider refining the DISRS by removing four items on theoretical grounds (i.e., from a face-validity perspective, some may be more closely related to depression). The following items may have the highest association with depression: Items 8 (“Think about how sad you feel”), 11 (“Think about how bad you feel”), 14 (“Think ‘I can't shake this feeling off’”), and 19 (“Think, ‘I can't be around people when I'm feeling this way’”). Although there are no items that should be removed on empirical grounds, these four items have the highest correlations with the BDI-II, of 0.56, 0.56, 0.57 and 0.55, respectively. The internal consistency of the scale with these items removed was the same as the full scale (Cronbach α = 0.92; mean = 33.87, SD = 9.17). Ultimately, in order to determine whether the omission of these items is beneficial, this shortened 16-item scale would have to be administered to and validated in another sample. Although these two studies provided psychometric support for this scale, more research is needed.
It is important to consider that this scale was designed to measure a specific construct. That is, the instructions ask about the pervasiveness of the tendency to engage in repetitive thought behaviors in response to the state of “feeling tired.” These instructions were chosen based on a prevailing operational definition of rumination, which conceptualizes rumination as the process through which individuals respond to particular disorder-relevant states by focusing on them and searching for possible causes of the state/symptoms.47 The relevant cue for rumination in depression is dysphoria, and dysphoria is not a pervasive state in insomnia; thus, using depression scales is inappropriate in this population. Fatigue is the most common symptom complaint in insomnia48 and the state most related to rumination in insomnia.13,14 Therefore, it is important to have a qualifier relevant to insomnia rather than depression to differentiate this state from other states, such as depressed mood, which is relevant to many of the items in the DISRS. Thus, we are not interested in general repetitive thought, or repetitive thoughts relevant to other disorders, and instead are orienting respondents to the specific state of fatigue.
The factor structure suggests that when faced with daytime insomnia symptoms, people with poor sleep tend to increase their thinking about: (1) their thoughts and motivation level, (2) their negative state (e.g., how badly they feel), and (3) tiredness. It is possible that there are other content areas not assessed with this measure, as these three domains accounted for less than two-thirds of the variance. The factor analysis was conducted to understand the construct only. Given that only three items load on the tiredness factor and that the latter two factors do not account for a substantive part of the variance, the use of these factors as subscales is not advisable; instead the total summed score should be used. However, insofar as the factor analysis helps us to further understand the construct, it would also be interesting to see whether and how the factor structure might differ when administering the scale to a clinical sample
The psychometric properties of this scale in a clinical sample suffering from uncomplicated insomnia without notable comorbidities are yet to be determined. Future studies could evaluate this measure to ensure it is valid in such a population. It is notable that this scale was derived from a smaller set of items shown to be useful in those with clinical insomnia.14 This study specifically examined those with a range of mood and sleep symptoms to show that rumination is not a mere artifact of mood problems. Comorbid insomnia is the rule rather than the exception in clinical practice,49,50 so arguably validation efforts in comorbid insomnia groups are equally if not more important than testing them in those suffering from isolated forms of insomnia. In sum, the present study found evidence in support of an insomnia-specific measure of rumination, and also confirmed previous studies' findings of symptom focused rumination, in both nonclinical and clinical groups with a range of sleep and mood pathology. In addition to the theoretical implications for understanding perpetuating factors in insomnia and also for models of the risk that insomnia may confer for depression, there also may be clinical implications. The front-line recommended treatment for chronic insomnia is cognitive behavior therapy for insomnia (CBT-I),51 and this treatment has little to offer with regard to rumination-specific strategies. It is also a treatment that de-emphasizes daytime focused strategies. Future studies could test whether addressing the tendency to respond to daytime symptoms would improve clinical outcomes, or whether improving CBT-I's effects on daytime symptoms would reduce rumination.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Edinger has received loaner equipment for research from Philips/Respironics; he has also received medications for research provided by Forest Pharmaceuticals. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This study was supported by grant R01- MH076856. Authors' Note: Those interested in using the scale mentioned in this paper can contact Dr. Carney for permission.
REFERENCES
- 1.Harvey AG, Watkins E, Mansell W, Shafran R. Oxford: Oxford University Press; 2004. Cognitive behavioural processes across psychological disorders: A transdiagnostic approach to research and treatment. [Google Scholar]
- 2.Nolen-Hoeksema S, Morrow J, Fredrickson BL. Response styles and the duration of episodes of depressed mood. J Abnorm Psychol. 1993;102:20–8. doi: 10.1037//0021-843x.102.1.20. [DOI] [PubMed] [Google Scholar]
- 3.Watkins E. Appraisals and strategies associated with rumination and worry. Pers Indiv Differ. 2004;37:679–94. [Google Scholar]
- 4.Watkins E, Moulds M, Mackintosh B. Comparisons between rumination and worry in a non-clinical population. Behav Res Ther. 2005;43:1577–85. doi: 10.1016/j.brat.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 5.Carney C, Ulmer C, Edinger JD, Krystal AD, Knauss F. Assessing depression symptoms in those with insomnia: An examination of the Beck Depression Inventory Second Edition (BDI-II) J Psychiat Res. 2009;43:576–82. doi: 10.1016/j.jpsychires.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ohayon MM, Caulet M, Lemoine P. Comorbidity of mental and insomnia disorders in the general population. Compr Psychiatry. 1998;39:185–97. doi: 10.1016/s0010-440x(98)90059-1. [DOI] [PubMed] [Google Scholar]
- 7.Harvey AG. A cognitive model of insomnia. Behav Res Ther. 2002;40:869–93. doi: 10.1016/s0005-7967(01)00061-4. [DOI] [PubMed] [Google Scholar]
- 8.Jones BT, Macphee LM, Broomfield NM, Jones BC, Espie CA. Sleep-related attentional bias in good, moderate, and poor (Primary Insomnia) sleepers. J Abnorm Psychol. 2005;114:249–58. doi: 10.1037/0021-843X.114.2.249. [DOI] [PubMed] [Google Scholar]
- 9.Tang NK, Harvey AG. Effects of cognitive arousal and physiological arousal on sleep perception. Sleep. 2004;27:69–78. doi: 10.1093/sleep/27.1.69. [DOI] [PubMed] [Google Scholar]
- 10.Tang NK, Schmidt DA, Harvey AG. Sleeping with the enemy: Clock monitoring in the maintenance of insomnia. J Behav Ther Exp Psychiatry. 2006;38:40–55. doi: 10.1016/j.jbtep.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 11.Gross R, Borkovec T. Effects of cognitive intrusion manipulation on the sleep onset latency of good sleepers. Behav Ther. 1982;13:112–6. [Google Scholar]
- 12.Hall M, Buysse DJ, Reynolds CF, Kupfer DJ, Baum A. Stress-related intrusive thoughts disrupt sleep onset and contiguity. J Sleep Res. 1996;25:163. [Google Scholar]
- 13.Carney C, Edinger J, Meyer B, Lindman L, Istre T. Symptom-focused rumination and sleep disturbance. Behav Sleep Med. 2006;4:228–41. doi: 10.1207/s15402010bsm0404_3. [DOI] [PubMed] [Google Scholar]
- 14.Carney CE, Harris AL, Moss T, Edinger JD. Distinguishing rumination from worry in clinical insomnia. Behav Res Ther. 2010;48:540–6. doi: 10.1016/j.brat.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomsen DK, Mehlsen MY, Christensen S, Zachariae R. Rumination - relationship with negative mood and sleep quality. Pers Indiv Differ. 2003;34:1293–301. [Google Scholar]
- 16.Hossain JL, Ahmad P, Reinish RW, Kayumov L, Hossain NK, Shapiro CM. Subjective fatigue and subjective sleepiness: Two independent consequences of sleep disorders? J Sleep Res. 2005;14:245–53. doi: 10.1111/j.1365-2869.2005.00466.x. [DOI] [PubMed] [Google Scholar]
- 17.Bagby RM, Rector NA, Bacchichi JR, McBride C. The stability of the Repsonse Styles Questionnaire scale in a sample of patients with major depression. Cognitive Ther Res. 2004;28:527–38. [Google Scholar]
- 18.Nolen-Hoeksema S, Morrow J. A prospective study of depression and post-traumatic stress symptoms after a natural disaster: The 1989 Loma Prieta earthquake. J Pers Soc Psychol. 1991;61:115–21. doi: 10.1037//0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- 19.Edinger JD, Bonnet M, Bootzin RR, et al. Derivation of research diagnostic criteria for insomnia: Report on an American Academy of Sleep Medicine work group. Sleep. 2004;27:1567–96. doi: 10.1093/sleep/27.8.1567. [DOI] [PubMed] [Google Scholar]
- 20.Morin CM. Insomnia: Psychological assessment and management. New York: Guilford Press; 1993. [Google Scholar]
- 21.Buysse DJ, Ancoli-Israel S, Edinger J D, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29:1155–73. doi: 10.1093/sleep/29.9.1155. [DOI] [PubMed] [Google Scholar]
- 22.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 23.Beck AT, Steer RA, Brown GK. San Antonio, TX: The Psychological Association; 1996. Manual for the Beck Depression Inventory, Second Edition (BDI-II) [Google Scholar]
- 24.Richter P, Werner J, Heerlein A, Kraus A, Sauer H. On the validity of the Beck Depression Inventory: A review. Psychopathology. 1998;31:160–8. doi: 10.1159/000066239. [DOI] [PubMed] [Google Scholar]
- 25.Krupp LB, LaRocca NG, Muir-Nash J, Sternberg AD. The Fatigue Severity Scale: Application to patients with multiple sclerosis and systemic lupus erythemasis. Arch Neurol. 1989;46:1121–3. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 26.Valko PO, Bassetti CL, Bloch KE, Held U, Baumann C. Validation of the fatigue severity scale in a Swiss cohort. Sleep. 2008;31:1601–7. doi: 10.1093/sleep/31.11.1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stöber J, Bittencourt J. Weekly assessment of worry: an adaptation of the Penn State Worry Questionnaire for monitoring changes during treatment. Behav Res Ther. 1998;36:645–56. doi: 10.1016/s0005-7967(98)00031-x. [DOI] [PubMed] [Google Scholar]
- 28.Tabachnick BG, Fidell LS. Using multivariate statistics. 4th ed. Needham Heights, MA: Allyn & Bacon; 2001. [Google Scholar]
- 29.West SG, Finch JF, Curran PJ. Structural equation models with nonnormal variables: Problems and remedies. In: Hoyle RH, editor. Structural equation modeling: Concepts, issues, and applications. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- 30.Field A. Discovering statistics using SPSS. 3rd ed. London: Sage; 2009. [Google Scholar]
- 31.Hutcheson G, Sofroniou N. The multivariate social scientist. London: Sage; 1999. [Google Scholar]
- 32.Kaiser HF. A second generation little jiffy. Psychometrika. 1970;35:401–15. [Google Scholar]
- 33.Stevens JP. Applied multivariate statistics for the social sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1992. [Google Scholar]
- 34.Edinger JD, Olsen MK, Stechuchak KM, et al. Reliability and validity of the Duke Structured Interview for Sleep Disorders for Insomnia Screening. Sleep. 2009;32:A265. [Google Scholar]
- 35.First MB, Spitzer RL, Gibbon M, Williams JBW. New York: Biometrics Research, New York State Psychiatric Institute; 2002. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) [Google Scholar]
- 36.Hamilton M. A rating scale for depression. J Neurol Neurosur Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smets EMA, Garssen B, Bonke B, De Haes CJM. The Multidimensional Fatigue Inventory (MFI) Psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995;39:315–25. doi: 10.1016/0022-3999(94)00125-o. [DOI] [PubMed] [Google Scholar]
- 38.Riemann D, Spiegelhalder K, Feige B, et al. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14:19–31. doi: 10.1016/j.smrv.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 39.Bonnet MH, Arand DL. Caffeine use as a model of acute and chronic insomnia. Sleep. 1992;15:526–6. [PubMed] [Google Scholar]
- 40.Espie CA, Broomfield NM, MacMahon KMA, Macphee LM, Taylor LM. The attention-intention-effort pathway in the development of psychophysiologic insomnia: A theoretical review. Sleep Med Rev. 2006;10:215–45. doi: 10.1016/j.smrv.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 41.Hong RY. Worry and rumination: Differential associations with anxious and depressive symptoms and coping behaviors. Behav Res Ther. 2007;45:277–90. doi: 10.1016/j.brat.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 42.Kohn L, Espie CA. Sensitivity and specificity of measures of the insomnia experience: A comparative study of psychophysiologic insomnia, insomnia associated with mental disorder and good sleepers. Sleep. 2005;29:104–12. doi: 10.1093/sleep/28.1.104. [DOI] [PubMed] [Google Scholar]
- 43.Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. J Abnorm Psychol. 2000;109:504–11. [PubMed] [Google Scholar]
- 44.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disorders. 2011;135:10–9. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 45.Ehring T, Watkins ER. Repetitive negative thinking as a transdiagnostic process. Int J Cognit Ther. 2008;1:192–205. [Google Scholar]
- 46.Sánchez-Ortuño MM, Carney CE, Edinger JD, Harris AL. Moving beyond average values: assessing the night-to-night instability of sleep and arousal in DSMIV-TR insomnia subtypes. Sleep. 2011;34:531–9. doi: 10.1093/sleep/34.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. J Abnorm Psychol. 1991;100:569–82. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- 48.Morin CM, LeBlanc M, Daley M, Gregoire JP, Mérette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7:123–30. doi: 10.1016/j.sleep.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 49.Buysse DJ, Reynolds CF, Hauri P, et al. Diagnostic concordance for DSMIV disorders: A report form the APA NIMH DSM-IV field trial. Am J Psychiatry. 1994;151:1351–60. doi: 10.1176/ajp.151.9.1351. [DOI] [PubMed] [Google Scholar]
- 50.Edinger JD, Hoelscher TJ, Webb MD, Marsh GR, Radtke RA, Erwin CW. Polysomnographic assessment of DIMS: empirical evaluation of its diagnostic value. Sleep. 1989;12:315–22. [PubMed] [Google Scholar]
- 51.National Institutes of Health State of the Science Conference Statement. Manifestations and management of chronic insomnia in adults. Sleep. 2005;28:1049–57. doi: 10.1093/sleep/28.9.1049. [DOI] [PubMed] [Google Scholar]


