In a multicenter, prospective phase II study without controls, no-option critical limb ischemia (CLI) patients were subjected to intra-arterial infusion of autologous bone marrow and followed for 12 months after the treatment. Patients showed improvement in objective and subjective measures of perfusion and improved amputation-free survival rates at 12 months after the treatment. This study provides evidence that autologous bone marrow transplantation is well tolerated by CLI patients without adverse effects, confirming the feasibility and safety of the procedure.
Keywords: Adult human bone marrow, Adult stem cells, Angiogenesis, Autologous stem cell transplantation, Bone marrow transplant, Stem/progenitor cell, Transplantation, Vascular development
Abstract
Critical limb ischemia (CLI) is a vascular disease affecting lower limbs, which is going to become a demanding challenge because of the aging of the population. Despite advances in endovascular therapies, CLI is associated with high morbidity and mortality. Patients without direct revascularization options have the worst outcomes. To date, 25%–40% of CLI patients are not candidates for surgical or endovascular approaches, ultimately facing the possibility of a major amputation. This study aimed to assess the safety and efficacy of autologous bone marrow (BM) transplantation performed in “no-option” patients, in terms of restoring blood perfusion by collateral flow and limb salvage. A multicenter, prospective, not-controlled phase II study for no-option CLI patients was performed. Patients were subjected to intra-arterial infusion of autologous bone marrow and followed for 12 months after the treatment. Variation of blood perfusion parameters, evaluated by laser Doppler flowmetry or transcutaneous oximetry, was set as the primary endpoint at 12 months after treatment and amputation-free survival as the secondary endpoint. Sixty patients were enrolled and treated with BM transplantation, showing improvement in objective and subjective measures of perfusion. Furthermore, survival analysis demonstrated improved amputation-free survival rates (75.2%) at 12 months after the treatment. This study provides further evidence that autologous bone marrow transplantation is well tolerated by CLI patients without adverse effects, demonstrating trends toward improvement in perfusion and reduced amputation rate, confirming the feasibility and safety of the procedure.
Introduction
Peripheral arterial disease (PAD) is a common circulatory problem. In 2010 almost 18 million U.S. citizens suffered from PAD. Reflecting the aging population, this number is projected to increase to 21 million by 2020. Critical limb ischemia (CLI), the most severe and deadly form of the disease, currently affects 2.8–3.5 million of those with PAD. By 2020, the U.S. prevalence of CLI is forecast to grow to between 3.6 and 4.5 million. Among PAD patients, approximately 1%–3% will develop CLI [1].
The clinical course of PAD patients without CLI is generally stable; on the other hand, the prognosis of CLI is poor: according to the TASC II Guidelines [2], after 1 year 30% of patients with CLI will lose a leg and 25% will die. Approximately 25%–40% of CLI patients are not candidates for either surgical or endovascular approaches because of high operative risk or unfavorable vascular involvement, thus leaving a large percentage of patients without any valid therapeutic option. Therefore, new strategies are needed to offer a viable therapy to this increasing number of patients.
Several years ago, a step forward was taken in understanding the mechanisms for neovascularization. In 1997, Asahara et al. [3] and Shi et al. [4] identified a class of bone marrow-derived circulating endothelial progenitor cells that contribute to angiogenesis and/or vasculogenesis in ischemic tissue. Since then, numerous studies have reported the capability of stem and progenitor cell types, delivered locally into ischemic tissue, to reduce ischemic damage effects [5, 6].
Subsequently, the use of progenitor cell-based therapies in patients affected by PAD and/or CLI emerged as a new approach for the treatment of ischemic conditions [7]. Encouraging results of several clinical studies have rapidly demonstrated the beneficial effect of autologous bone marrow mononuclear cell (BM-MNC) transplantation to patients affected by CLI. Clinical benefits were reported from these trials, showing improvement in objective and subjective measures of perfusion (i.e., transcutaneous oximetry [TcPO2], laser Doppler flowmetry [LDF], pain reduction, increase of total walking distance [TWD], and decreased rate of amputation) [7–44].
However, the majority of these studies were case series, with few randomized and controlled trials. Robust trials for cellular therapy in CLI are complicated by ethical reasons, severe comorbidities, challenges of blinding, inclusion criteria, and choice of outcome measures. The primary objective of our trial was to further assess the safety of intra-arterial autologous bone marrow transplantation in CLI patients and the efficacy of this treatment in terms of perfusion parameters and amputation-free survival.
Materials and Methods
Study Design
The Naples and Pietra Ligure Evaluation of Stem Cells (NAPLES) study was designed as a multicenter, prospective, nonrandomized phase II trial. Patients enrolled in this trial were affected by Rutherford category 3, 4, or 5 PAD (disabling intermittent claudication or CLI with or without tissue loss) who were not candidates for surgical or endovascular revascularization or who had had failed attempts at revascularization.
We decided to set a nonrandomized phase II trial because the majority of enrolled subjects were “no-option” patients, in whom the progression of the disease is well-defined and amputation is the only treatment option available, as previously reported [2]. Therefore, on the basis of observations done by us and others, we believed that an untreated control group was unnecessary.
The protocol was approved by the ethics committees of the participating hospitals, the Seconda Università di Napoli and the Azienda Ospedaliera S. Corona di Pietra Ligure, and registered at the European Trials Registration (EudraCT 2008-003218-83). Written informed consent for participation was obtained from all patients. The patients treated in Naples are referred to as group 1 (group evaluated with LDF) and the patients treated in Pietra Ligure as group 2 (group evaluated with TcPO2).
Eligibility Criteria
Eligibility criteria are listed in Table 1.
Table 1.
Eligibility criteria of the Naples and Pietra Ligure Evaluation of Stem Cells study
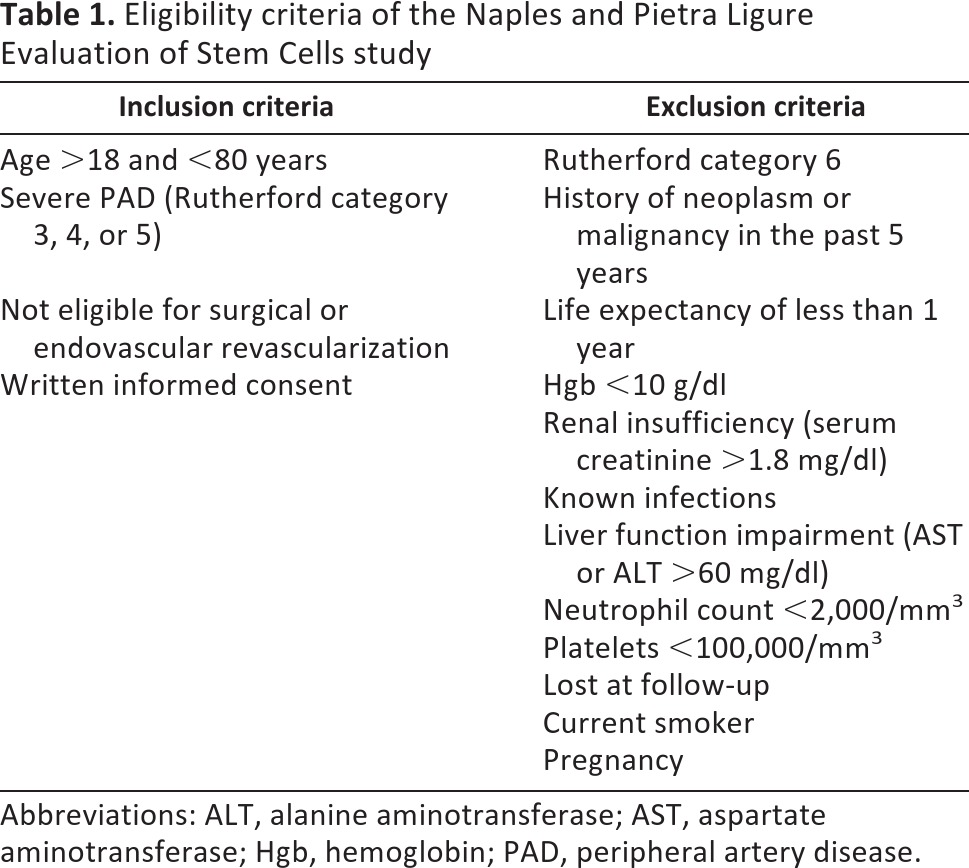
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; Hgb, hemoglobin; PAD, peripheral artery disease.
Treatment Procedure
A total volume of 105 ml of bone marrow (BM) aspirate was obtained from all patients from posterior iliac crest puncture with a 15-gauge needle, under local anesthesia and smooth conscious sedation. Five milliliters of BM aspirate was kept for research purposes. The remaining BM aspirate (100 ml) was immediately added to sodium heparin (2,000 units) in 20 ml of normal saline and filtered (bone marrow collection kit 4R2104; Fenwal Inc., Lake Zurich, IL, http://www.fenwalinc.com) to remove large particulate matter, such as fat, bone chips, and clots. The BM aspirate was then ready for intra-arterial direct infusion ipsilateral to the affected leg through a 4 French introducer placed through common femoral artery into external iliac artery under the control of a peristaltic pump at 150 ml/hour or slowly by direct hand injection. Forty-five days later all the patients underwent a second procedure exactly like the first one.
Patients were discharged on the first postoperative day; scheduled for 3, 6, 12, and 24 months follow-up; and given oral l-arginine, 3 g/day, to take for 4 months after the first transplant. Follow-up consisted of clinical evaluation and laser Doppler flowmetry (Periflex PF2B; Perimed AB, Stockholm, Sweden, http://www.perimed-instruments.com) in group 1 patients or transcutaneous oximetry (TCM400; Radiometer Medical ApS, Brønshøj, Denmark, http://www.radiometer.com) in group 2 patients.
LDF and TcPO2 were used as noninvasive techniques for assessing microvascular blood flow and tissue oxygen tension after autologous bone marrow transplantation. LDF was performed at a stable room temperature (25°C) after 30 minutes of acclimatization in a supine position at rest. We started the measurements at least 5 minutes after placement of the probe to ensure a stable flux measurement. The probe was positioned on the third distal dorsum of the foot of the affected limb, which underwent the infusion of BM. TcPO2 was evaluated in patients at rest in a supine position and at a stable room temperature, considering the values obtained 15 minutes after the beginning of the measurement. The probe position was marked with a dermographic pen or was photographed to place the probe in the same position during the subsequent controls. Each measurement was performed three times and averaged. Baseline measurements were determined before transplantation, and the follow-up was performed at intervals of 6 and 12 months after the treatment.
Endpoints
Because no gold-standard endpoints have been established for such clinical trials, we decided to set as the primary endpoint the variation of blood perfusion parameters measured by LDF (group 1) or TcPO2 (group 2) at 6 and 12 months after transplantation. Amputation-free survival at 12 months among patients affected by CLI was set as a secondary endpoint.
Data Management and Statistical Analysis
Data were collected using paper-based case-report forms and computer database sheets. We calculated that a sample of 60 patients was required to detect an effect size of 0.55 between the study groups (α = 0.05 and β = 0.70). We performed an analysis of variance with repeated measures to determine differences in within-subject effects over time, using the Bonferroni test. All reported p values are based on two-sided tests. Survival probability was evaluated with the Kaplan-Meier test. Data were analyzed with nQuery Advisor 7.0 (Statistical Solutions, Sagus, MA, http://www.statistical-solutions-software.com) and SPSS software (SPSS, Chicago, http://www.spss.com).
Results
Patient and Demographics
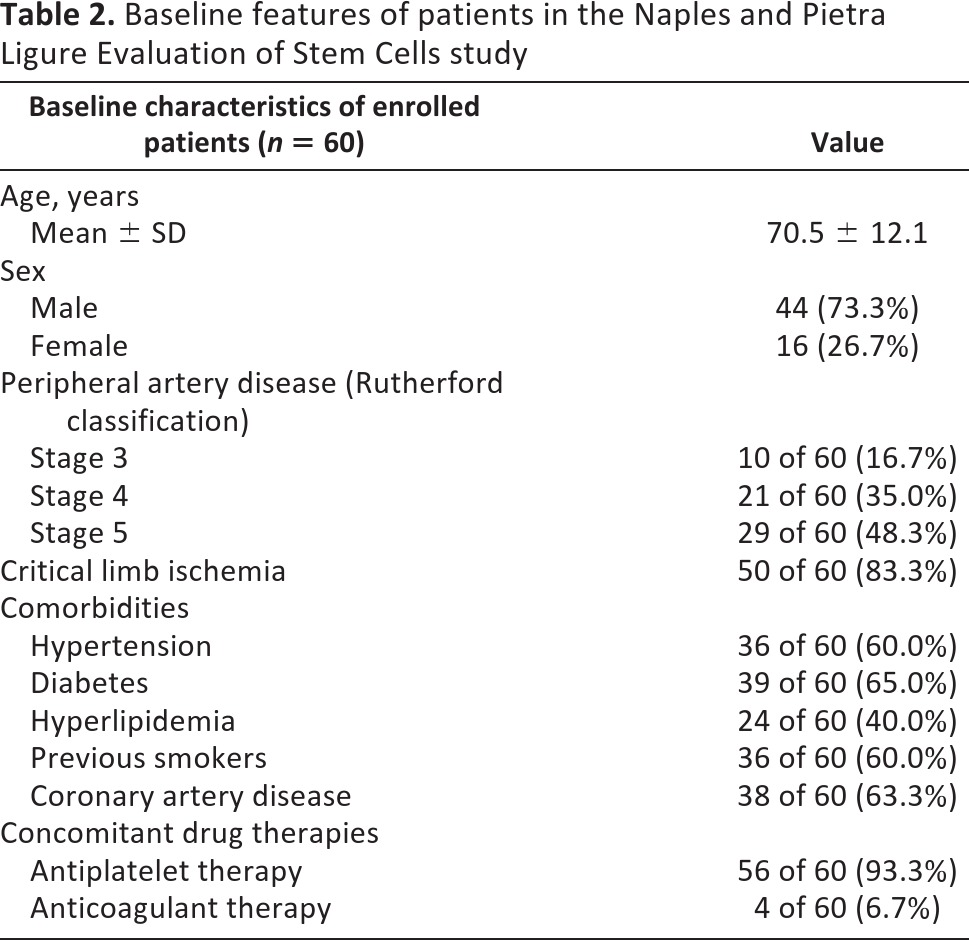
Seventy-six patients were enrolled from October 2008 to December 2010. Sixteen patients were discarded, leaving 60 patients for evaluation. The study enrollment diagram is shown in Figure 1, and the baseline features of claudicants and CLI patients are summarized in Table 2. Comorbidities and concomitant drug therapies did not differ significantly between the groups. All patients received antiplatelet or anticoagulant drugs throughout the study period.
Figure 1.
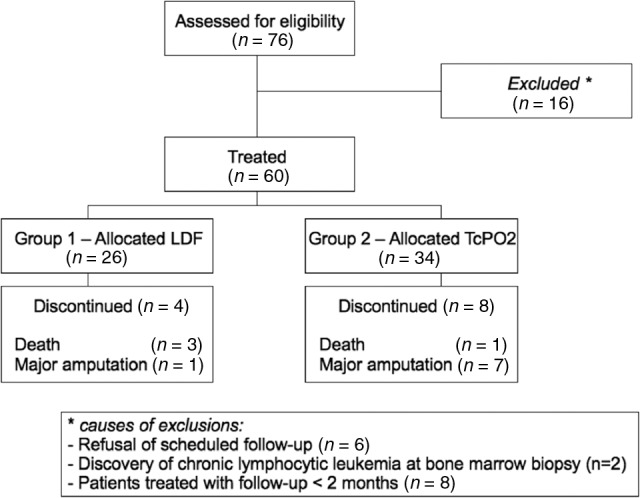
Study enrollment diagram of the Naples and Pietra Ligure Evaluation of Stem Cells study. Abbreviations: LDF, laser Doppler flowmetry; TcPO2, transcutaneous oximetry.
Table 2.
Baseline features of patients in the Naples and Pietra Ligure Evaluation of Stem Cells study
Procedural and Safety Results
Marrow aspiration and injection were accomplished in the operating room on a single visit under local anesthesia. Patients tolerated the procedure well, and transient smooth sedation was used to facilitate the BM collection. There were no complications on the day of treatment, and there were no deaths or severe procedure-related adverse events after 1 month from the procedure. No local complications at the iliac crest puncture or reinjection site of common femoral artery were observed. No local or systemic infective complications occurred. One patient in group 2 with previous history of myocardial ischemia and coronary artery bypass graft developed a nonfatal myocardial infarction 2 months after the procedure. Because of the history of the patient, the event was not considered related to the cell infusion. The patient is still alive and well 24 months after the procedure. Two patients in group 2 needed a humeral approach because of the presence of heavy scar and/or heavy calcifications at the level of Scarpa's triangle, without complications.
Viability and Features of Infused Cells
From each harvest, a small aliquot of cells was analyzed by cytofluorimeter to assess cell viability. Cell viability of infused cells (mean ± SD of all samples collected) was 94.1 ± 4.7%. We also tested BM-derived blood for CD34+ and CD146+ markers. The mean number of CD34+ infused cells was 4.7 × 106 ± 3.1 × 106, corresponding to 0.52 ± 0.28% of all BM-MNCs. CD146+ infused cells were found to be 0.0022% of all BM-MNCs (International Society for Hematotherapy and Graft Engineering protocol enumeration in a single platform).
Primary Endpoints
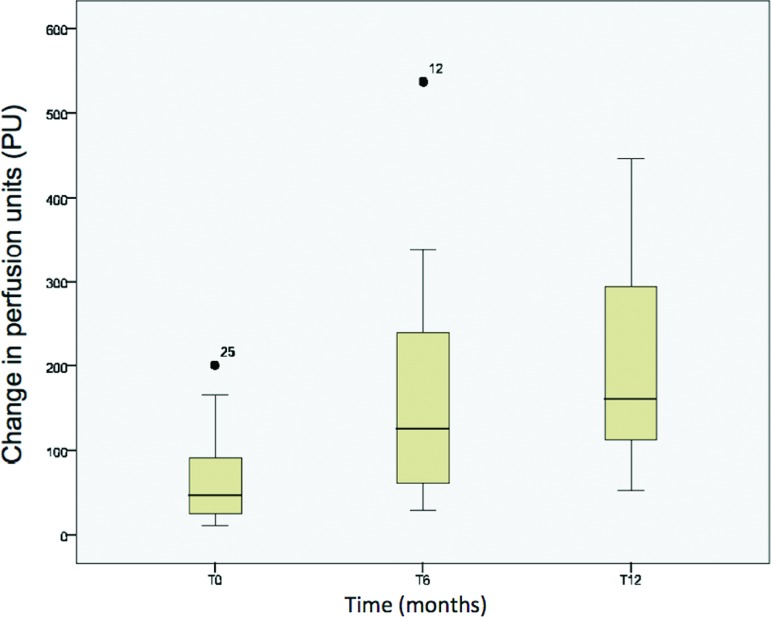
Almost all patients reported improvements of clinical symptoms, such as pain and TWD, with positive impact on their quality of life. Quantitative analysis of the laser Doppler imaging of the group 1 revealed a significant increase of blood flow at rest in ischemic limbs at 12 months (T12) (laser Doppler basal oxygenation: T0 65.095 ± 53.3 vs. T12 205.03 ± 114.39; p = .008 with adjustment for multiple comparisons; Fig. 2). Restoration of perfusion has also been evident from the blood flow measured for the lowered leg (laser Doppler basal poststimulus [LDBP]: T0 86.552 ± 91.22 vs. T12 109.83 ± 75.21; p = .035 with adjustment for multiple comparisons). The significance of this measure was lower; however, we should take into account that the increase of LDBP is abnormal in a healthy patient, whereas it is considered a compensatory mechanism in a patient affected by vasculopathy. Therefore, the increase of LDBP confirmed the beneficial effect of infusion.
Figure 2.
Change in perfusion parameters in group 1: laser Doppler basal oxygenation flowmetry measurements at T0 (before transplantation), T6, and T12 (after transplantation) visualized as a box plot, including the median, the minimum, and the maximum data values (p = .008; repeated-measures analysis of variance). The black dots are the two outliers (patients 12 and 25), representing the minimum and the maximum of perfusion measurements. Abbreviations: PU, perfusion units; T, time in months.
Next, we considered the response in hyperemia conditions. Increasing local skin temperature leads to an increase in blood flow, avoiding the myogenic vessel tone, providing an effective method by which to assess the presence of microcirculatory modifications. A significant increase in these conditions was observed (laser Doppler with probe at 44°C: T0 169.11 ± 145.73 vs. T12 216.66 ± 145.91; p = .04 with adjustment for multiple comparisons).
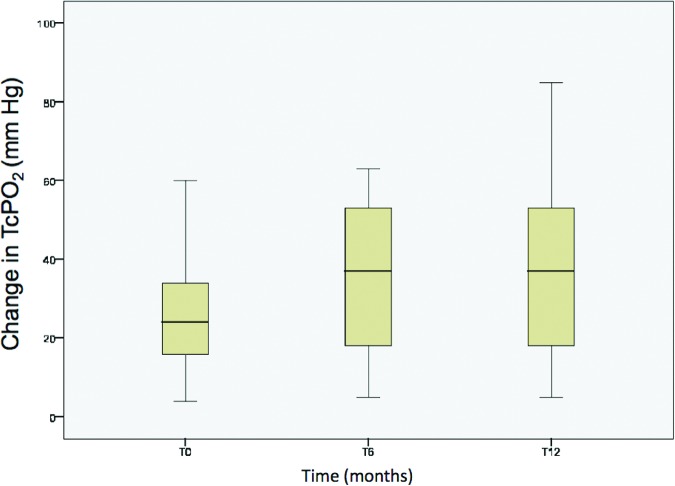
TcPO2 of the patients in group 2 showed a significant increase in TcPO2 at 12 months in ischemic limbs after the treatment (T0 26.96 ± 15.83 vs. T12 36.13 ± 22.47; p = .008 with adjustment for multiple comparisons; Fig. 3). The results of measurement with LDF and TcPO2 in claudicants and CLI patients are not presented separately because of the small number of claudicants (n = 10), although all patients showed similar perfusion responses to cell infusion.
Figure 3.
Change in perfusion parameters in group 2: transcutaneous oximetry measurements at T0 (before transplantation), T6, and T12 (after transplantation) visualized as a box plot, including the median, the minimum, and the maximum data values (p = .008; repeated-measures analysis of variance). Abbreviations: T, time in months; TcPO2, transcutaneous oximetry.
With regard to the 10 patients affected by Rutherford category 3 PAD, there was a subjective improvement of TWD beginning approximately 3 months after transplantation, increasing at least threefold at 6 months in 80% of them (8 of 10). This finding is not meaningful, based on the small number of patients and on the subjective evaluations.
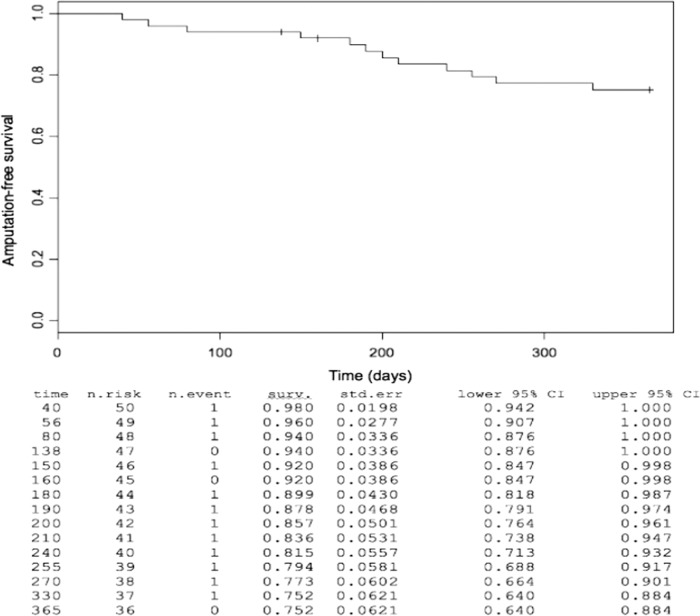
Secondary Endpoint
CLI patients were followed up until death or until amputation occurred over the time. There were eight major amputations (16.6%) and four deaths (8.3%) in the period considered. We then calculated the amputation-free survival longitudinally and generated a Kaplan-Meier plot. As shown, the amputation-free survival in CLI patients (n = 50) was 75.2% at 12 months after the treatment (Fig. 4), indicating that the risk of death and/or major amputation decreased in transplanted patients compared with natural evolution of the disease, in which 30% of patients will face amputation and 25% will die after 1 year, as already reported in above-mentioned TASC II Guidelines.
Figure 4.
Amputation-free survival. The Kaplan-Meier curve describes the amputation-free survival after 12 months among all critical limb ischemia subjects enrolled (n = 50). Abbreviations: CI, confidence interval; std. err, standard error; surv, survival.
Discussion
With the aging of Western population, PAD in general and CLI in particular are going to become more demanding problems for health care programs. Many patients unfit for surgery and/or an endovascular approach will face major amputation, further increasing social costs of the disease. This phase II multicenter clinical study confirmed the long-term beneficial effects of cellular therapy in patients with PAD. In fact, ischemia is a potent stimulus to increase the oxygen delivery via a network of collateral vessels and to stimulate angiogenesis [45, 46], but this natural capability is impaired in CLI patients [47, 48].
Intra-arterial infusion of BM-derived stem cells seems to be a safe procedure, confirming the findings of other studies [12], and it is also a promising tool in the hands of vascular specialists. No malignant tumor was clinically identified during the study period, and this outcome confirms data from other studies [39, 49].
Considering the perfusion analysis, the improvement of peripheral perfusion was confirmed both by LDF and TcPO2 measurements, and it seemed to persist for at least 12 months after the treatment. Looking at the trend after 18 months, a decrease of the values after that time was observed and could be due to the progression of the disease (data not shown). This decrease has been already stated by others [49]. Thus, the option to re-treat those patients showing a negative trend of the perfusion after 18 months can be taken into account.
The 75% amputation-free survival recorded at 1 year among no-option CLI patients in our study appears to be promising compared with the natural evolution of CLI disease and the mean survival probability in this class of patients, and it is similar to the findings of a recent study in PAD patients treated with intramuscular BM-MNC infusion [12].
The procedure seems also to have beneficial effects on claudicants (Rutherford category 3), because the majority of enrolled patients of this category reported a marked increase in their TWD, although these data are based on subjective reports. We can hypothesize in the future a more active role of this therapy in claudicants, since this option does not exclude the possibility of resorting to subsequent surgical or endovascular approaches. We decided to not include the record of the ankle-brachial index for two reasons: (a) the measurements are operator-biased, and (b) the tibial vessels are incompressible in many diabetic patients.
Conclusion
The NAPLES study revealed that intra-arterial transplantation of BM-derived stem cells is beneficial in PAD patients, increasing the percentage of amputation-free survival in CLI patients at 1 year. Although both subjective and objective parameters of limb ischemia noticeably improved following cells transplantation, the real efficacy needs to be evaluated in larger groups. However, we have to take in account that robust cellular trials in CLI patients are complicated by severe comorbidities.
For what concerns new strategies of the research, a promising tool could come from the use of superparamagnetic iron oxide nanoparticles (SPIONs) or carbon nanotubes (CNTs). In fact, researchers have shown that SPION- or CNT-labeled stem cells can be addressed to target tissue if submitted to magnetic gradients, increasing the number of stem cells within target tissues [50, 51]. Bone marrow transplantation in CLI patients is to our knowledge a safe procedure, improves tissue perfusion, and obtains high amputation-free survival rates.
Acknowledgments
We are grateful to the Fondazione Luigi Califano, Fondazione Banco Napoli, and Istituto Superiore di Sanità, which gave us the support needed to perform the research. Special thanks go to Paola Mantovano and Giuseppe Sica, who helped us in coordinating the clinical trial.
Author Contributions
A. Schiavetta and G.C.: conception and design, data assembly, interpretation and manuscript writing, final approval of manuscript; C.M., C.B., G.M., A.G., L.L., S.P.: data collection and assembly, data analysis and interpretation, final approval of manuscript; S.L. and A. Silvestroni: provision and treatment of patients and data collection, final approval of manuscript; G.S.: data analysis, conception and design, final approval of manuscript; V.S.: conception and design, financial support, final approval of manuscript.
Disclosure of Potential Conflicts of Interest
The authors indicate no potential conflicts of interest.
References
- 1.Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): A collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society For Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients with Peripheral Arterial Disease): Endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; Transatlantic Inter-society Consensus; and Vascular Disease Foundation. Circulation. 2006;113:e463–e654. doi: 10.1161/CIRCULATIONAHA.106.174526. [DOI] [PubMed] [Google Scholar]
- 2.Norgren L, Hiatt WR, Dormandy JA, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) J Vasc Surg. 2007;45(suppl S):S5–S67. doi: 10.1016/j.jvs.2006.12.037. [DOI] [PubMed] [Google Scholar]
- 3.Asahara T, Murohara T, Sullivan A, et al. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997;275:964–967. doi: 10.1126/science.275.5302.964. [DOI] [PubMed] [Google Scholar]
- 4.Shi Q, Rafii S, Wu MH, et al. Evidence for circulating bone marrow-derived endothelial cells. Blood. 1998;92:362–367. [PubMed] [Google Scholar]
- 5.Asahara T, Masuda H, Takahashi T, et al. Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res. 1999;85:221–228. doi: 10.1161/01.res.85.3.221. [DOI] [PubMed] [Google Scholar]
- 6.Crosby JR, Kaminski WE, Schatteman G, et al. Endothelial cells of hematopoietic origin make a significant contribution to adult blood vessel formation. Circ Res. 2000;87:728–730. doi: 10.1161/01.res.87.9.728. [DOI] [PubMed] [Google Scholar]
- 7.Sprengers RW, Lips DJ, Moll FL, et al. Progenitor cell therapy in patients with critical limb ischemia without surgical options. Ann Surg. 2008;247:411–420. doi: 10.1097/SLA.0b013e318153fdcb. [DOI] [PubMed] [Google Scholar]
- 8.Kalka C, Masuda H, Takahashi T, et al. Transplantation of ex vivo expanded endothelial progenitor cells for therapeutic neovascularization. Proc Natl Acad Sci USA. 2000;97:3422–3427. doi: 10.1073/pnas.070046397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamaguchi J, Kusano KF, Masuo O, et al. Stromal cell-derived factor-1 effects on ex vivo expanded endothelial progenitor cell recruitment for ischemic neovascularization. Circulation. 2003;107:1322–1328. doi: 10.1161/01.cir.0000055313.77510.22. [DOI] [PubMed] [Google Scholar]
- 10.Tateishi-Yuyama E, Matsubara H, Murohara T, et al. Therapeutic angiogenesis for patients with limb ischaemia by autologous transplantation of bone-marrow cells: A pilot study and a randomised controlled trial. Lancet. 2002;360:427–435. doi: 10.1016/S0140-6736(02)09670-8. [DOI] [PubMed] [Google Scholar]
- 11.Lu D, Chen B, Liang Z, et al. Comparison of bone marrow mesenchymal stem cells with bone marrow-derived mononuclear cells for treatment of diabetic critical limb ischemia and foot ulcer: A double-blind, randomized, controlled trial. Diabetes Res Clin Pract. 2011;92:26–36. doi: 10.1016/j.diabres.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 12.Walter DH, Krankenberg H, Balzer JO, et al. Intraarterial administration of bone marrow mononuclear cells in patients with critical limb ischemia: A randomized start, placebo-controlled pilot trial (PROVASA) Circ Cardiovasc Interv. 2011;4:26–37. doi: 10.1161/CIRCINTERVENTIONS.110.958348. [DOI] [PubMed] [Google Scholar]
- 13.Kawamoto A, Katayama M, Handa N, et al. Intramuscular transplantation of G-CSF mobilized CD34(+) cells in patients with critical limb ischemia: A phase I/IIa, multicenter, single-blinded, dose-escalation clinical trial. Stem Cells. 2009;27:2857–2864. doi: 10.1002/stem.207. [DOI] [PubMed] [Google Scholar]
- 14.Ozawa T, Kato K, Sanada H, et al. Marked decrease of plasma VEGF after implantation of autologous bone marrow mononuclear cells in a patient with critical limb ischemia: A case report. Angiology. 2006;57:235–239. doi: 10.1177/000331970605700216. [DOI] [PubMed] [Google Scholar]
- 15.Saigawa T, Kato K, Ozawa T, et al. Clinical application of bone marrow implantation in patients with arteriosclerosis obliterans, and the association between efficacy and the number of implanted bone marrow cells. Circ J. 2004;68:1189–1193. doi: 10.1253/circj.68.1189. [DOI] [PubMed] [Google Scholar]
- 16.Lenk K, Adams V, Lurz P, et al. Therapeutical potential of blood-derived progenitor cells in patients with peripheral arterial occlusive disease and critical limb ischaemia. Eur Heart J. 2005;26:1903–1909. doi: 10.1093/eurheartj/ehi285. [DOI] [PubMed] [Google Scholar]
- 17.Amann B, Luedemann C, Ratei R, et al. Autologous bone marrow cell transplantation increases leg perfusion and reduces amputations in patients with advanced critical limb ischemia due to peripheral artery disease. Cell Transplant. 2009;18:371–380. doi: 10.3727/096368909788534942. [DOI] [PubMed] [Google Scholar]
- 18.Burt RK, Testori A, Oyama Y, et al. Autologous peripheral blood; CD133+ cell implantation for limb salvage in patients with critical limb ischemia. Bone Marrow Transplant. 2010;45:111–116. doi: 10.1038/bmt.2009.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cobellis G, Silvestroni A, Lillo S, et al. Long-term effects of repeated autologous transplantation of bone marrow cells in patients affected by peripheral arterial disease. Bone Marrow Transplant. 2008;42:667–672. doi: 10.1038/bmt.2008.228. [DOI] [PubMed] [Google Scholar]
- 20.De Vriese AS, Billiet J, Van Droogenbroeck J, et al. Autologous transplantation of bone marrow mononuclear cells for limb ischemia in a Caucasian population with atherosclerosis obliterans. J Intern Med. 2008;263:395–403. doi: 10.1111/j.1365-2796.2007.01899.x. [DOI] [PubMed] [Google Scholar]
- 21.Durdu S, Akar AR, Arat M, et al. Autologous bone-marrow mononuclear cell implantation for patients with Rutherford grade II–III thromboangiitis obliterans. J Vasc Surg. 2006;44:732–739. doi: 10.1016/j.jvs.2006.06.023. [DOI] [PubMed] [Google Scholar]
- 22.Gu YQ, Zhang J, Guo LR, et al. Transplantation of autologous bone marrow mononuclear cells for patients with lower limb ischemia. Chin Med J. 2008;121:963–967. [PubMed] [Google Scholar]
- 23.Hernández P, Cortina L, Artaza H, et al. Autologous bone-marrow mononuclear cell implantation in patients with severe lower limb ischaemia: A comparison of using blood cell separator and Ficoll density gradient centrifugation. Atherosclerosis. 2007;194:e52–e56. doi: 10.1016/j.atherosclerosis.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 24.Horie T, Onodera R, Akamastu M, et al. Long-term clinical outcomes for patients with lower limb ischemia implanted with G-CSF-mobilized autologous peripheral blood mononuclear cells. Atherosclerosis. 2010;208:461–466. doi: 10.1016/j.atherosclerosis.2009.07.050. [DOI] [PubMed] [Google Scholar]
- 25.Kajiguchi M, Kondo T, Izawa H, et al. Safety and efficacy of autologous progenitor cell transplantation for therapeutic angiogenesis in patients with critical limb ischemia. Circ J. 2007;71:196–201. doi: 10.1253/circj.71.196. [DOI] [PubMed] [Google Scholar]
- 26.Kawamura A, Horie T, Tsuda I, et al. Clinical study of therapeutic angiogenesis by autologous peripheral blood stem cell (PBSC) transplantation in 92 patients with critically ischemic limbs. J Artif Organs. 2006;9:226–233. doi: 10.1007/s10047-006-0351-2. [DOI] [PubMed] [Google Scholar]
- 27.Koshikawa M, Shimodaira S, Yoshioka T, et al. Therapeutic angiogenesis by bone marrow implantation for critical hand ischemia in patients with peripheral arterial disease: A pilot study. Curr Med Res Opin. 2006;22:793–798. doi: 10.1185/030079906X1000078. [DOI] [PubMed] [Google Scholar]
- 28.Lara-Hernandez R, Lozano-Vilardell P, Blanes P, et al. Safety and efficacy of therapeutic angiogenesis as a novel treatment in patients with critical limb ischemia. Ann Vasc Surg. 2010;24:287–294. doi: 10.1016/j.avsg.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 29.Matoba S, Tatsumi T, Murohara T, et al. TACT Follow-up Study Investigators. Long-term clinical outcome after intramuscular implantation of bone marrow mononuclear cells (Therapeutic Angiogenesis by Cell Transplantation [TACT] trial) in patients with chronic limb ischemia. Am Heart J. 2008;156:1010–1018. doi: 10.1016/j.ahj.2008.06.025. [DOI] [PubMed] [Google Scholar]
- 30.Miyamoto K, Nishigami K, Nagaya N, et al. Unblinded pilot study of autologous transplantation of bone marrow mononuclear cells in patients with thromboangiitis obliterans. Circulation. 2006;114:2679–2684. doi: 10.1161/CIRCULATIONAHA.106.644203. [DOI] [PubMed] [Google Scholar]
- 31.Moriya J, Minamino T, Tateno K, et al. Long-term outcome of therapeutic neovascularization using peripheral blood mononuclear cells for limb ischemia. Circ Cardiovasc Interv. 2009;2:245–254. doi: 10.1161/CIRCINTERVENTIONS.108.799361. [DOI] [PubMed] [Google Scholar]
- 32.Motukuru V, Suresh KR, Vivekanand V, et al. Therapeutic angiogenesis in Buerger's disease (thromboangiitis obliterans) patients with critical limb ischemia by autologous transplantation of bone marrow mononuclear cells. J Vasc Surg. 2008;48(suppl 6):53S–60S. doi: 10.1016/j.jvs.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 33.Saito Y, Sasaki K, Katsuda Y, et al. Effect of autologous bone-marrow cell transplantation on ischemic ulcer in patients with Buerger's disease. Circ J. 2007;71:1187–1192. doi: 10.1253/circj.71.1187. [DOI] [PubMed] [Google Scholar]
- 34.Wester T, Jørgensen JJ, Stranden E, et al. Treatment with autologous bone marrow mononuclear cells in patients with critical lower limb ischaemia. Scand J Surg. 2008;97:56–62. doi: 10.1177/145749690809700108. [DOI] [PubMed] [Google Scholar]
- 35.Huang P, Li S, Han M, et al. Autologous transplantation of granulocyte colony-stimulating factor-mobilized peripheral blood mononuclear cells improves critical limb ischemia in diabetes. Diabetes Care. 2005;28:2155–2160. doi: 10.2337/diacare.28.9.2155. [DOI] [PubMed] [Google Scholar]
- 36.Huang PP, Yang XF, Li SZ, et al. Randomised comparison of G-CSF-mobilized peripheral blood mononuclear cells versus bone marrow-mononuclear cells for the treatment of patients with lower limb arteriosclerosis obliterans. Thromb Haemost. 2007;98:1335–1342. doi: 10.1160/th07-02-0137. [DOI] [PubMed] [Google Scholar]
- 37.Procházka V, Gumulec J, Jalůvka F, et al. Cell therapy, a new standard in management of chronic critical limb ischemia and foot ulcer. Cell Transplant. 2010;19:1413–1424. doi: 10.3727/096368910X514170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kolvenbach R, Kreissig C, Cagiannos C, et al. Intraoperative adjunctive stem cell treatment in patients with critical limb ischemia using a novel point-of-care device. Ann Vasc Surg. 2010;24:367–372. doi: 10.1016/j.avsg.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 39.Iafrati MD, Hallett JW, Geils G, et al. Early results and lessons learned from a multicenter, randomized, double-blind trial of bone marrow aspirate concentrate in critical limb ischemia. J Vasc Surg. 2011;54:1650–1658. doi: 10.1016/j.jvs.2011.06.118. [DOI] [PubMed] [Google Scholar]
- 40.Bartsch T, Brehm M, Zeus T, et al. Transplantation of autologous mononuclear bone marrow stem cells in patients with peripheral arterial disease (the TAM-PAD study) Clin Res Cardiol. 2007;96:891–899. doi: 10.1007/s00392-007-0569-x. [DOI] [PubMed] [Google Scholar]
- 41.Van Tongeren RB, Hamming JF, Fibbe WE, et al. Intramuscular or combined intramuscular/intra-arterial administration of bone marrow mononuclear cells: A clinical trial in patients with advanced limb ischemia. J Cardiovasc Surg (Torino) 2008;49:51–58. [PubMed] [Google Scholar]
- 42.Gu Y, Zhang J, Qi L. A clinical study on implantation of autologous bone marrow mononuclear cells after bone marrow stimulation for treatment of lower limb ischemia [in Chinese] Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2006;20:1017–1020. [PubMed] [Google Scholar]
- 43.Sprengers RW, Moll FL, Teraa M, et al. Rationale and design of the JUVENTAS Trial for repeated intra-arterial infusion of autologous bone-marrow derived mononuclear cells in patients with critical limb ischemia. J Vasc Surg. 2010;51:1564–1568. doi: 10.1016/j.jvs.2010.02.020. [DOI] [PubMed] [Google Scholar]
- 44.Powell RJ, Comerota AJ, Berceli SA, et al. interim analysis results from the RESTORE-CLI, a randomized, double-blind multicenter phase II trial comparing expanded autologous bone marrow-derived tissue repair cells and placebo in patients with critical limb ischemia. J Vasc Surg. 2011;54:1032–1041. doi: 10.1016/j.jvs.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 45.Kilian JG, Keech A, Adams MR. Coronary collateralization: Determinants of adequate distal vessel filling after arterial occlusion. Coron Artery Dis. 2002;13:155–159. doi: 10.1097/00019501-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 46.Wahlberg E. Angiogenesis and arteriogenesis in limb ischemia. J Vasc Surg. 2003;38:198–203. doi: 10.1016/s0741-5214(03)00151-4. [DOI] [PubMed] [Google Scholar]
- 47.Cetrulo CL, Jr., Knox KR, Brown DJ, et al. Stem cells and distraction osteogenesis: Endothelial progenitor cells home to the ischemic generate in activation and consolidation. Plast Reconstr Surg. 2005;116:1053–1064. doi: 10.1097/01.prs.0000178403.79051.70. discussion 1065–1067. [DOI] [PubMed] [Google Scholar]
- 48.De Vivo S, Palmer-Kazen U, Kalin B, et al. Risk factors for poor collateral development in claudication. Vasc Endovascular Surg. 2005;39:519–524. doi: 10.1177/153857440503900609. [DOI] [PubMed] [Google Scholar]
- 49.Idei N, Soga J, Hata T, et al. Autologous bone-marrow mononuclear cell implantation reduces long-term major amputation risk in patients with critical limb ischemia: A comparison of atherosclerotic peripheral arterial disease and Buerger disease. Circ Cardiovasc Interv. 2011;4:15–25. doi: 10.1161/CIRCINTERVENTIONS.110.955724. [DOI] [PubMed] [Google Scholar]
- 50.Kyrtatos PG, Lehtolainen P, Junemann-Ramirez M, et al. Magnetic tagging increases delivery of circulating progenitors in vascular injury. JACC Cardiovasc Interv. 2009;2:794–802. doi: 10.1016/j.jcin.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 51.Vittorio O, Quaranta P, Raffa V, et al. Magnetic carbon nanotubes: A new tool for shepherding mesenchymal stem cells by magnetic fields. Nanomedicine (Lond) 2011;6:43–54. doi: 10.2217/nnm.10.125. [DOI] [PubMed] [Google Scholar]