Fertility preservation is an emerging field in medicine that enables men, women, and children to maintain reproductive health when it is threatened by gonadotoxic treatment or nononcologic malignancies that can impair spermatogenesis and ovogenesis. Established methods include sperm cryopreservation or experimental testicular tissue cryopreservation for males, and oocyte cryopreservation or ovarian tissue cryopreservation for females. Fertility preservation treatments must be addressed through a multidisciplinary approach that involves gynecologists, urologists, oncologists, pediatricians, and professionals in the field of medically assisted reproduction.
Keywords: Cytotoxic agents, Cancer, Cell culture, Cryopreservation
Abstract
Fertility preservation is an emerging field in medicine that enables men, women, and children to maintain reproductive health when it is threatened by gonadotoxic treatment. Patients affected by other nononcologic malignancies that can impair spermatogenesis and ovogenesis can also benefit from fertility preservation treatments. Age-related infertility can also be overcome by cryopreserving gametes or embryos. The only established methods for fertility preservation in male patients are sperm cryopreservation in postpubertal age and experimental testicular tissue cryopreservation in prepubertal age. In adult women, oocyte cryopreservation is the preferred option, whereas ovarian tissue cryopreservation is the only possibility for prepubertal girls. Fertility preservation treatments must be addressed through a multidisciplinary approach that involves gynecologists, urologists, oncologists, pediatricians, and professionals in the field of medically assisted reproduction to work in coordination to provide patients with counseling and comprehensive information about fertility issues.
Introduction
Fertility preservation is an emerging field that provides the opportunity to maintain reproductive health to all those patients who either have to receive gonadotoxic treatment for medical reasons or want to preserve their gametes to postpone childbearing (age-related fertility preservation). The majority of patients who can benefit from fertility preservation techniques are cancer patients. Chemo- and radiotherapy given in cancer therapies have detrimental consequences on male and female gonads that may lead to infertility. Other disorders, such as autoimmune diseases (e.g., lupus) and myelodysplastic syndromes, require medical treatment that can also impair reproductive cells and tissues. The main target of these therapies is the cellular cycle, and the interruption or arrest of the cellular cycle causes severe defects in the DNA replication and transcription mechanisms that could lead to cell death. Nevertheless, the undesirable effects of those therapies depend on various factors, such as the intrinsic characteristics of the patients (age, general health status, genetic disposition, sensitivity of tissues, cell-repair mechanisms), therapy (total dose and irradiated field in radiotherapy, type of chemotherapy agent), and tumor biology [1].
Men and women are affected by gonadotoxic therapies in different ways. The reproductive damage caused in the male is mainly focused on sperm quality and germinal epithelium. Since spermatogenesis is maintained throughout life from puberty, damage caused by gonadotoxic therapies can usually be reversed after treatment. There is evidence of significant recovery of gonadal function in the first 10 years after treatment [2]. In women, radio- and chemotherapy can affect ovaries and uterus, threatening ovarian reserve and uterine vascularization.
Apart from oncological patients, fertility preservation is also indicated in other circumstances where germ cell degeneration is observed. Women affected by premature ovarian failure (POF) may also benefit from fertility preservation. POF etiology is mainly idiopathic, but the origin of POF can also be genetic, as in Turner syndrome mosaicism, X trisomy, and X-fragile syndrome. Twenty percent of patients with POF have an autoimmune-associated disease, such as diabetes mellitus, thyroid dysfunction, Addison syndrome, myasthenia gravis, Crohn's disease, lupus, or rheumatoid arthritis [3]. In men, Klinefelter syndrome affects 1 of 600 male newborns. Germ cell degeneration in affected patients starts in utero and progresses through infancy and adolescence. Sperm cryopreservation in adolescent patients prior to achievement of azoospermia (90% of cases) should be performed as a strategy for fertility preservation [4].
Furthermore, in recent decades, a social trend toward delaying childbearing has been observed in women of reproductive age. This delay is due to different factors related to lifestyle (such as development of a professional career or absence of the right partner). As a consequence, these women may be affected by age-related infertility when they decide to conceive, and fertility preservation techniques may also be indicated in this population. Sperm cryopreservation is a well-established technique that enables men who wish to preserve their fertility for social reasons to maintain their gametes stored in liquid nitrogen. Sperm cryopreservation is considered a standard procedure prior to vasectomy. Men exposed to toxins or those whose work conditions can adversely affect spermatogenesis are also candidates for fertility preservation. Fertility preservation has been also required by some individuals who undergo gender reallocation, with cryopreservation of sperm in transsexual women and oocytes in transsexual men.
Male Fertility Preservation
Cancer Patients
Today, two-thirds of patients survive at least 5 years after being diagnosed with cancer. Advances in oncological research and improvement in cancer screening and treatment have increased survival rates and improved the quality of patients' lives [5].
Nonetheless, in some cases, young cancer patients have to face oncological treatments at a childbearing age. Fertility preservation should be considered an important issue when facing the oncological process, and patients should be informed about it as soon as the oncological treatment is indicated.
Effects of Cancer on Male Reproductive Health
Cancer itself has a detrimental impact on male reproductive health because many biological processes, cells, and tissues become affected. The disruption of the hypothalamic-pituitary-gonadal axis induces a breakdown of the spermatogenesis process. In testicular cancer, the malignancy also triggers immunologic and cytotoxic injuries on testicular germinal epithelium that affect testicular environment. Taking into account that neoplasic processes can be considered a systemic illness, the affected individuals can develop some associated somatic disorders, such as fever and malnutrition, and some psychological disorders, such as anxiety and/or depression, that will certainly have a negative impact on reproductive health [6].
Effects of Cancer Treatment on Male Reproductive Health
In male cancer patients, surgery, radiotherapy, and chemotherapy can be followed by transient or permanent infertility by affecting ejaculatory or erectile function, or by impairing spermatogenesis.
Surgery
Bilateral orchiectomy in testicular cancer results in a lack of production of both testosterone and sperm, resulting in permanent infertility. Unilateral orchiectomy reduces the sperm concentration in semen samples. Reduced spermatogenesis is reversible within the first year after surgery in survivors who recover almost normal follicle-stimulating hormone (FSH) levels [7]. Retroperitoneal lymph node dissection, performed mainly in testicular carcinoma, renal cell carcinoma, and upper urinary tract urothelial carcinoma, causes serious disruption of ejaculation. Advances in surgery, such as nerve-sparing techniques, reduce the side effects of the intervention [8]. Prostate cancer patients who have to undergo radical prostatectomy suffer from erectile dysfunction that will impair fertility. Retrograde ejaculation and loss of semen quality have also been described after prostatectomy. Erectile dysfunction can also be produced by surgery for cancer of the rectum [9, 10].
Radiotherapy
Radiotherapy has severe side effects upon male fertility. Irradiation in the G2 phase of the cell cycle induces chromatid aberrations [11]. The chromosomal damage can be individually measured by analyzing the dose/response to radiotherapy of peripheral blood cells. This situation makes it possible to restrict the dose radiation in order to minimize the side effects on healthy tissues [12].
Detrimental effects of radiotherapy depend on dose and irradiation field. A 2-Gy dose of irradiation leads to azoospermia. This situation can be overcome in some cases in approximately 30 months (Table 1). Total body irradiation (TBI) performed in hematological cancers prior to bone marrow transplantation or hematopoietic stem cell transplantation and abdominal or pelvic radiotherapy put patients at high risk of developing permanent infertility. Less than 20% of patients recover gonadal function after TBI. Furthermore, spermatogenesis can be disrupted since radiotherapy combined with chemotherapy increases FSH levels in approximately 70% of patients [13].
Table 1.
Recovery from azoospermia caused by radiotherapy
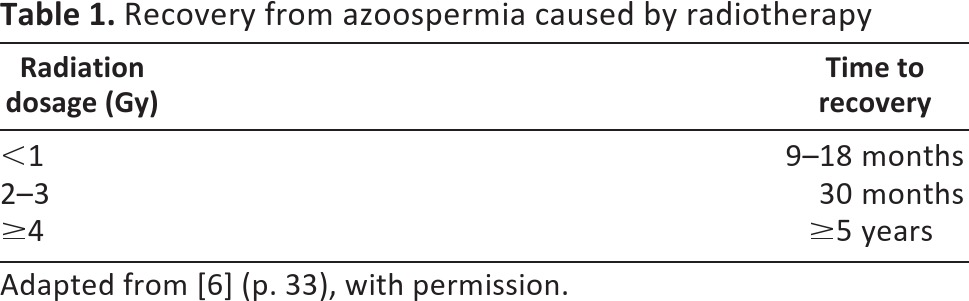
Adapted from [6] (p. 33), with permission.
Chemotherapy
The vast majority of chemotherapeutic agents are gonadotoxic. Alkylating agents seem to present the greater risk of causing infertility, largely due to azoospermia. Other chemotherapeutic agents, such as platinum compounds, can also cause azoospermia in 50% of patients. Besides the decrease in sperm count produced by these oncologic treatments, DNA of spermatozoa can also be impaired. It has been demonstrated that DNA integrity can be recovered after treatment [14]. As not all chemotherapeutic treatments affect male fertility, fertility preservation should be offered only in cases where high risk of azoospermia or DNA damage is suspected.
Strategies for Male Fertility Preservation
Sperm Cryopreservation
Cryopreservation of human spermatozoa was introduced in the 1960s and now constitutes one of the most well-established techniques in assisted reproductive techniques laboratories worldwide. The sperm cryopreservation technique that seems to be more efficient is the rapid freezing protocol. After a short exposure to cryoprotectants (glycerol, DMSO), the sperm sample is loaded into straws or cryotubes and then left in direct contact with nitrogen vapors. Immersion in liquid nitrogen at −196°C allows sperm cryostorage for long periods of time. Survival rates after sperm cryopreservation allow pregnancy rates comparable to the ones obtained with the use of fresh samples [15].
Although some spermatozoa do not survive freezing-thawing procedures, sperm cryopreservation is a useful tool for fertility preservation in adolescent and adult males whenever a sperm sample can be obtained by masturbation and whenever the presence of a certain number of spermatozoa is observed in the ejaculate. Depending on individual sperm quality, the preservation of more than one sample should be addressed. Sperm collection is mostly achieved by masturbation, but some disorders, such as retrograde ejaculation or anejaculation, can be solved by the administration of alpha agonists in the former cases and vibratory stimulation or electro-ejaculation for the latter [6].
Testicular Tissue Cryopreservation
In rare cases where fertility preservation needs to be carried out in obstructive azoospermia adult men, testicular sperm aspiration or testicular sperm extraction (biopsy) is performed. There are several protocols for cryopreservation of surgically retrieved spermatozoa. Whatever the method used, to obtain good results in terms of survival rates, it is important to choose the most suitable cryoprotectants and to perform an accurate thawing protocol.
No fertility preservation options exist for prepubertal boys. In 1994, Brinster and Zimmerman reported the successful transplantation of male germ cells in a rodent model [16]. They proved that spermatogenesis could be induced from the transplanted stem cells in a sterile recipient mouse. This method of spermatogonial stem cell transplantation into the testis shows a potential strategy of fertility preservation in prepubertal boys undergoing a cytotoxic treatment [16]. In a report of recent work performed in a mouse model, Goossens et al. suggest that intratesticular tissue grafting might be best choice for fertility preservation in prepubertal boys because of the maintenance of the stem cell niche and show that its disruption may cause epigenetic problems in germ cells [17].
Female Fertility Preservation
Cancer Patients
Breast, cervical, and colorectal cancers are the leading cancers in women worldwide [18]. Approximately 4% of women with cancer will be younger than 35 years of age at the time of diagnosis [19], and breast cancer is the cancer with the highest incidence in this population [20]. Some of these patients may have disease identified at an early stage and can potentially be cured, with fertility preservation being an important issue at the time of disease diagnosis. Fifty-seven percent of women asked about the possibility of becoming infertile after treatment for breast cancer reported being concerned about fertility issues [21]. Furthermore, the continuous delay of childbearing observed in developed countries will result in an increased proportion of women diagnosed with cancer before their first pregnancy [22].
Effects of Cancer on Female Reproductive Health
Cancer causes an increased metabolic state and hypothalamic dysfunction that may lead to infertility. It has been reported that oocyte quality is apparently affected by the malignancy and that female carriers of BRCA1 mutation may be low responders to ovarian stimulation [23]. Somatic disorders, such as anxiety and depression associated with the oncologic process, also have a negative impact on reproductive health.
Effects of Cancer Therapies on Female Reproductive Health
Cancer therapies are known to affect reproductive health, although the effects may be unpredictable since the exact apoptotic pathways involved are still unknown. The risk of ovarian failure after chemo- and radiotherapy depends on patient's age, treatment protocol, and type of malignancy. Knowledge of the exact mechanisms involved in ovarian damage is important to try to minimize the detrimental side effects.
Radiotherapy
Ovarian damage caused by radiation depends on the patient's age, the dose, and the field of irradiation. Radiation therapy to the pelvis can have a direct negative impact on ovarian function and on the uterus by altering vascularization and by reducing growth if treatment is received during childhood.
Doses of 4–6 Gy can produce a loss of 50% of the follicular population, whereas total body irradiation represents a high risk of ovarian failure in treated patients (55%–80%). It is also known that younger women (<40 years) are less affected by irradiation damage. Nonpelvic radiation (e.g., cerebral irradiation) can also impair fertility by affecting the hypothalamic-pituitary axis, causing a malfunction in oogenesis [24].
Chemotherapy
Chemotherapeutic agents affect ovarian function by several mechanisms, such as follicular depletion (burn-out mechanism), vascular damage, and cortical fibrosis. The patient's age at treatment and the chemotherapy regimen (type and dose) both influence the risk of premature ovarian failure. Older women have a higher risk of presenting permanent infertility. It has been demonstrated that women younger than 40 years old exposed to chemotherapeutic agents have a 61% risk of developing amenorrhea, and this figure increases to 95% in women older than 40 years. Alkylating drugs such as cyclophosphamide are the most gonadotoxic agents since they are not cell cycle-specific, and they also affect other cells in the ovary [14].
Strategies for Fertility Preservation in Women
Oocyte Cryopreservation
Oocyte cryopreservation is becoming a routine practice in most in vitro fertilization (IVF) centers with the development of the vitrification technique. Difficulties with slow freezing oocyte cryopreservation (ice crystal formation, low survival rates, and poor-quality embryos) in past decades made embryo cryopreservation the first choice for reproductive material cryopreservation. With the methodological improvements achieved with vitrification, clinical pregnancy rates and live birth rates with frozen-thawed oocytes are comparable to those obtained with fresh cycles [25]. Although children born from vitrified oocytes do not present higher rates of congenital anomalies than those born from fresh oocytes, long-term safety is still to be proved [26]. As a consequence, oocyte cryopreservation has become an alternative to embryo freezing in IVF programs and constitutes a real option for fertility preservation.
Oocyte cryopreservation constitutes a strategy of fertility preservation for patients who can postpone oncologic treatment and when controlled ovarian stimulation is not contraindicated. It is a valid option for postpubertal women without a male partner or those who do not accept donor sperm and have moral objections to embryo cryopreservation. Nowadays, age-related fertility preservation is performed mainly by oocyte vitrification. The whole process of oocyte cryopreservation (ovarian stimulation and oocyte retrieval) takes a minimum of 2–3 weeks, depending on patient's menstrual cycle. The use of gonadotropin-releasing hormone (GnRH) antagonists allows a random start of stimulation and provokes luteolysis within 2–4 days, with subsequent follicular development. This is a useful strategy when there are time constraints and the patient is not in the early follicular phase [27]. The exposure to high levels of estradiol may be contraindicated in patients with hormone-dependent tumors. However, there is controversy about this issue, since some authors believe that there is no real risk in having a short-term increase in hormonal levels [28]. Nonetheless, ovarian stimulation protocols with aromatase inhibitors have been described in order to avoid excessive high estradiol levels, and no increase of recurrence rate of breast cancer has been observed with this treatment [29].
Embryo Cryopreservation
To date, embryo cryopreservation is the most standardized procedure of fertility preservation. High survival rates and cumulative pregnancy rates of 60% support the fact that it constitutes a clinically well-established technique. The need of a male partner or sperm donor for embryo cryopreservation is a requirement that not always can be fulfilled. The ethical implications of the increasing number of embryos stored in IVF clinics make oocyte vitrification the preferred option for fertility preservation.
Ovarian Tissue Cryopreservation
Ovarian tissue cryopreservation may be still considered an experimental technique. To date, approximately 20 children have been born worldwide after ovarian tissue cryopreservation. Ovarian tissue is obtained by laparoscopy, and it is frozen or vitrified in thin slides [30]. Primordial follicles are located in ovarian cortex, and they are relatively resistant to cryoinjury. Nonetheless, after ovarian tissue thawing and grafting, a massive loss of follicles is observed during the ischemic period until revascularization is established. Revascularization of tissue graft results in some living follicles that grow and develop mature oocytes [31]. Because of the lack of a worldwide registry, the effectiveness of the technique is unknown, but this constitutes the only option for prepubertal girls and for women who cannot delay cancer treatment or cannot undergo controlled ovarian stimulation.
One of the concerns regarding thawed ovarian tissue transplantation is the risk of reseeding malignant cells. Transplantation of thawed ovarian tissue is contraindicated in patients with leukemia because of the high risk of relapse [32]. Some authors have reported that there seems to be no risk of reintroducing malignant cells for women with Hodgkin's disease or at early stages of breast cancer [33]. Transplantation of ovarian cortical fragments can be done either orthotopically (in the peritoneal cavity) or heterotopically (forearm or anterior abdominal wall, probably associated with poorer oocyte quality due to inadequate environment). Neoangiogenesis after ovarian tissue transplantation is still the limiting factor as it takes 5 days and leads to 60% loss of primordial follicles. Pregnancies reported to date have been both spontaneous and after IVF [34]. Transplantation of the whole ovary with its vascular pedicle still remains an experimental procedure in humans [35].
Hormonal Protection by Ovarian Activity Suppression
Ovarian protection from gonadotoxic treatment with GnRH agonists is still controversial. The idea of maintaining the ovarian metabolism quiescent to avoid any damage caused by oncologic treatment is still to be confirmed, and there are doubts about whether GnRH agonist administration has a potential beneficial effect on ovarian tissue because of the lack of FSH receptors on primordial follicles [6].
Ovarian Transposition
The surgical procedure of ovarian transposition intends to move ovaries outside the irradiation field. Laparoscopic ovarian transposition consists of releasing the ovary from its pelvic attachments and placing it behind the uterus or in the paracolic gutter. This strategy is especially useful in patients with cervical cancer who require only radiotherapy for cancer treatment [36].
In Vitro Maturation of Human Oocytes
Retrieval of immature oocytes followed by oocyte in vitro maturation (IVM) is one of the strategies in cases in which ovarian stimulation is not possible. Oocyte retrieval is usually performed prior to ovulation, but immature oocytes can also be recovered during both the follicular and luteal phases [37]. Oocyte cryopreservation after IVM can be performed using vitrification or slow freezing techniques. Vitrification of IVM oocytes has resulted in a live-birth rate of 20%; nonetheless, survival and fertilization rates of IVM oocytes are lower than those of in vivo-matured ones. Vitrification of in vitro matured oocytes combined with ovarian tissue cryopreservation represents a strategy for fertility preservation when ovarian stimulation is contraindicated [38].
Follicular Culture
In vitro follicular culture has been proposed as an alternative to ovarian tissue transplantation to avoid the risk of reintroducing malignant cells. The aim of this technique is to develop an in vitro system that allows the growth of primordial and primary follicles to antral stages in order to obtain mature oocytes [39]. Given the complexity of follicle genesis in vivo, much research in culture conditions is still necessary in order to achieve results that can be applied in clinical practice.
Ethical Aspects of Fertility Preservation
The emerging trend of fertility preservation in clinical practice is bringing new treatment options that may imply ethical dilemmas. Fertility preservation in patients experiencing malignancies and fertility preservation in women who are free from disease and wish to avoid age-related fertility loss are sometimes controversial because of the uncertainty of using the cryopreserved material in the future and the doubtful benefit to the patients.
As a result of more effective treatments, the long-term survival rate of childhood and young adult cancer patients has raised over the past few decades. Almost 80% of children diagnosed with malignancy will recover from the illness [40]. Infertility is an issue that is important to cancer patients and their families and that must be addressed. Realistic information about the new advances in fertility preservation and chances for the future should be given in order to ensure appropriate counseling and treatment.
Fertility preservation in girls during childhood due to nononcological conditions (repeated ovarian surgery, genetic disorders) may be controversial because of the uncertainty of predicting which patients are at risk for POF; which are the fertility preservation methods available for girls; and the feasibility, safety, and efficacy of these methods [41].
Conclusion
Fertility preservation is a multidisciplinary field that requires the collaboration and coordination of professionals from different specialties. Oocyte, sperm, embryo, and ovarian tissue cryopreservation offers patients real options of preserving fertility. It is important that individuals under threat of fertility loss are offered appropriate fertility preservation options.
Acknowledgments
This work was performed under the auspices of the Catedra d'Investigació en Obstetricia, Ginecología i Reproducció of the Department of Obstetrics and Gynaecology, USP-Institut Universitari Dexeus, Universitat Autònoma de Barcelona.
Author Contributions
C.G.: collection and assembly of data, manuscript writing; M.B. and M.D.: manuscript writing; A.V.: conception and design, final approval of manuscript.
Disclosure of Potential Conflicts of Interest
The authors indicate no potential conflicts of interest.
References
- 1.Simon B, Lee SJ, Partridge AH, et al. Preserving fertility after cancer. CA Cancer J Clin. 2005;55:211–228. doi: 10.3322/canjclin.55.4.211. [DOI] [PubMed] [Google Scholar]
- 2.Howell SJ, Radford JA, Ryder WD, et al. Testicular function after cytotoxic chemotherapy: Evidence of Leydig cell insufficiency. J Clin Oncol. 1999;17:1493–1498. doi: 10.1200/JCO.1999.17.5.1493. [DOI] [PubMed] [Google Scholar]
- 3.Gidoni Y, Holzer H, Tulandi T, et al. Fertility preservation in patients with non-oncological conditions. Reprod Biomed Online. 2008;16:792–800. doi: 10.1016/s1472-6483(10)60144-7. [DOI] [PubMed] [Google Scholar]
- 4.Stahl PJ, Stember DS, Hsiao W, et al. Indications and strategies for fertility preservation in men. Clin Obst Gynecol. 2010;53:815–827. doi: 10.1097/GRF.0b013e3181f980b3. [DOI] [PubMed] [Google Scholar]
- 5.Vogelzang NJ, Benowitz SI, Adams S, et al. Clinical cancer advances 2011: Annual Report on Progress Against Cancer from the American Society of Clinical Oncology. J Clin Oncol. 2012;30:88–109. doi: 10.1200/JCO.2011.40.1919. [DOI] [PubMed] [Google Scholar]
- 6.Woodruff TK, Snyder KA. Oncofertility: Fertility Preservation for Cancer Survivors. 1st ed. New York, NY: Springer; 2007. [Google Scholar]
- 7.Jacobsen KD, Theodorsen L, Fosså SD. Spermatogenesis after unilateral orchiectomy for testicular cancer in patients following surveillance policy. J Urol. 2001;165:93–96. doi: 10.1097/00005392-200101000-00023. [DOI] [PubMed] [Google Scholar]
- 8.Peschel R, Gettman MT, Neururer R, et al. Laparoscopic retroperitoneal lymph node dissection: Description of the nerve-sparing technique. Urology. 2002;60:339–343. doi: 10.1016/s0090-4295(02)01827-7. [DOI] [PubMed] [Google Scholar]
- 9.Albaugh JA. Addressing and managing erectile dysfunction after prostatectomy for prostate cancer. Urol Nurs. 2010;30:167–177. [PubMed] [Google Scholar]
- 10.Doeksen A, Gooszen JA, van Duijvendijk P, et al. Sexual and urinary functioning after rectal surgery: A prospective comparative study with a median follow-up of 8.5 years. Int J Colorectal Dis. 2011;26:1549–1557. doi: 10.1007/s00384-011-1288-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Terzoudi GI, Jung T, Hain J, et al. Increased G2 chromosomal radiosensitivity in cancer patients: The role of cdk1/cyclin-B activity level in the mechanisms involved. Int J Radiat Biol. 2000;76:607–615. doi: 10.1080/095530000138268. [DOI] [PubMed] [Google Scholar]
- 12.Huber R, Braselmann H, Geinitz H, et al. Chromosomal radiosensitivity and acute radiation side effects after radiotherapy in tumour patients: A follow-up study. Radiat Oncol. 2011;6:32. doi: 10.1186/1748-717X-6-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huddart RA, Norman A, Moynihan C, et al. Fertility, gonadal and sexual function in survivors of testicular cancer. Br J Cancer. 2005;93:200–207. doi: 10.1038/sj.bjc.6602677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jensen JR, Morbeck DE, Coddington CC., III Fertility preservation. Mayo Clin Proc. 2011;86:45–49. doi: 10.4065/mcp.2010.0564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Di Santo M, Tarozzi N, Nadalini M, et al. Human sperm cryopreservation: Update on techniques, effect on DNA integrity, and implications for ART. Adv Urol. 2012;2012:854837. doi: 10.1155/2012/854837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brinster R, Zimmermann J. Spermatogenesis following male germ-cell transplantation. Proc Natl Acad Sci USA. 1994;91:11298–11302. doi: 10.1073/pnas.91.24.11298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goossens E, Bilgec T, Van Saen D, et al. Mouse germ cells go through typical epigenetic modifications after intratesticular tissue grafting. Hum Reprod. 2011;26:3388–3400. doi: 10.1093/humrep/der334. [DOI] [PubMed] [Google Scholar]
- 18.GLOBOCAN 2008: Fast stats. World. Most frequent cancers: Women. [Accessed May 2, 2012]. Available at http://globocan.iarc.fr/factsheets/populations/factsheet.asp?uno=900#WOMEN.
- 19.Lee SJ, Schover LR, Partridge AH, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24:2917–2931. doi: 10.1200/JCO.2006.06.5888. [DOI] [PubMed] [Google Scholar]
- 20.Jeruss JS, Woodruff TK. Preservation of fertility in patients with cancer. N Engl J Med. 2009;360:902–911. doi: 10.1056/NEJMra0801454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Partridge AH, Gelber S, Peppercorn J, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004;22:4174–4183. doi: 10.1200/JCO.2004.01.159. [DOI] [PubMed] [Google Scholar]
- 22.Eskander RN, Randall LM, Berman ML, et al. Fertility preserving options in patients with gynecologic malignancies. Am J Obstet Gynecol. 2011;205:103–110. doi: 10.1016/j.ajog.2011.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Friedler S, Koc O, Gidoni Y, et al. Ovarian response to stimulation for fertility preservation in women with malignant disease: A systematic review and meta-analysis. Fertil Steril. 2012;97:125–133. doi: 10.1016/j.fertnstert.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 24.Meirow D, Nugent D. The effects of radiotherapy and chemotherapy on female reproduction. Hum Reprod Update. 2001;7:535–543. doi: 10.1093/humupd/7.6.535. [DOI] [PubMed] [Google Scholar]
- 25.Cobo A, Kuwayama M, Pérez S, et al. Comparison of concomitant outcome achieved with fresh and cryopreserved donor oocytes vitrified by the Cryotop method. Fertil Steril. 2008;89:1657–1664. doi: 10.1016/j.fertnstert.2007.05.050. [DOI] [PubMed] [Google Scholar]
- 26.Noyes N, Porcu E, Borini A. Over 900 oocyte cryopreservation babies born with no apparent increase in congenital anomalies. Reprod Biomed Online. 2009;18:769–776. doi: 10.1016/s1472-6483(10)60025-9. [DOI] [PubMed] [Google Scholar]
- 27.Nayak SR, Wakim AN. Random-start gonadotropin-releasing hormone (GnRH) antagonist-treated cycles with GnRH agonist trigger for fertility preservation. Fertil Steril. 2011;96:e51–e54. doi: 10.1016/j.fertnstert.2011.04.079. [DOI] [PubMed] [Google Scholar]
- 28.Kim SS, Klemp J, Fabian C. Breast cancer and fertility preservation. Fertil Steril. 2011;95:1535–1543. doi: 10.1016/j.fertnstert.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oktay K, Buyuk E, Libertella N, et al. Fertility preservation in breast cancer patients: A prospective controlled comparison of ovarian stimulation with tamoxifen and letrozole for embryo cryopreservation. J Clin Oncol. 2005;23:4347–4353. doi: 10.1200/JCO.2005.05.037. [DOI] [PubMed] [Google Scholar]
- 30.Hirshfeld-Cytron J, Grobman WA, Milad MP. Fertility preservation for social indications: A cost-based decision analysis. Fertil Steril. 2012;97:665–670. doi: 10.1016/j.fertnstert.2011.12.029. [DOI] [PubMed] [Google Scholar]
- 31.Friedman O, Orvieto R, Fisch B, et al. Possible improvements in human ovarian grafting by various host and graft treatments. Hum Reprod. 2012;27:474–482. doi: 10.1093/humrep/der385. [DOI] [PubMed] [Google Scholar]
- 32.Dolmans MM, Marinescu C, Saussoy P, et al. Reimplantation of cryopreserved ovarian tissue from patients with acute lymphoblastic leukemia is potentially unsafe. Blood. 2010;116:2908–2914. doi: 10.1182/blood-2010-01-265751. [DOI] [PubMed] [Google Scholar]
- 33.Sánchez-Serrano M, Novella-Maestre E, Rosello-Sastre E, et al. Malignant cells are not found in ovarian cortex from breast cancer patients undergoing ovarian cortex cryopreservation. Hum Reprod. 2009;24:2238–2243. doi: 10.1093/humrep/dep196. [DOI] [PubMed] [Google Scholar]
- 34.Donnez J, Silber S, Andersen CY, et al. Children born after autotransplantation of cryopreserved ovarian tissue: A review of 13 live births. Ann Med. 2011;43:437–450. doi: 10.3109/07853890.2010.546807. [DOI] [PubMed] [Google Scholar]
- 35.Martinez-Madrid B, Donnez J. Cryopreservation of intact human ovary with its vascular pedicle-or cryopreservation of hemiovaries? Hum Reprod. 2007;22:1795. doi: 10.1093/humrep/dem047. [DOI] [PubMed] [Google Scholar]
- 36.Leitao MM, Chi DS. Fertility-sparing options for patients with gynecologic malignancies. Oncologist. 2005;10:613–622. doi: 10.1634/theoncologist.10-8-613. [DOI] [PubMed] [Google Scholar]
- 37.Demirtas E, Elizur SE, Holzer H, et al. Immature oocyte retrieval in the luteal phase to preserve fertility in cancer patients. Reprod Biomed Online. 2008;17:520–523. doi: 10.1016/s1472-6483(10)60239-8. [DOI] [PubMed] [Google Scholar]
- 38.González C, Devesa M, Boada M, et al. Combined strategy for fertility preservation in an oncologic patient: Vitrification of in vitro matured oocytes and ovarian tissue freezing. J Assist Reprod Genet. 2011;28:1147–1149. doi: 10.1007/s10815-011-9628-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Telfer EE, McLaughlin M. In vitro development of ovarian follicles. Semin Reprod Med. 2011;29:15–23. doi: 10.1055/s-0030-1268700. [DOI] [PubMed] [Google Scholar]
- 40.Ginsberg JP. New advances in fertility preservation for pediatric cancer patients. Curr Opin Pediatr. 2011;23:9–13. doi: 10.1097/MOP.0b013e3283420fb6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jadoul P, Dolmans MM, Donnez J. Fertility preservation in girls during childhood: Is it feasible, efficient and safe and to whom should it be proposed? Hum Reprod Update. 2010;16:617–630. doi: 10.1093/humupd/dmq010. [DOI] [PubMed] [Google Scholar]


