Abstract
Aims
To examine sociodemographic associations of transitions from alcohol use to disorders and of remission from disorders in metropolitan China.
Design and Setting
Face-to-face interviewing by trained lay-interviewers on a multi-staged, clustered sample from the general population of Beijing and Shanghai, P.R.C.
Participants
5,201 adults aged 18-70 years and with household registration.
Measurements
World Mental Health version of Composite International Diagnostic Interview.
Findings
Lifetime prevalence estimates for alcohol use, regular use (at least 12 drinks in a year), DSM-IV abuse and dependence with abuse were 65.4%, 39.5% (60.4% of ever-drinkers), 4.6% (11.6% of regular users) and 0.9% (20.4% of lifetime alcohol abusers) respectively. These estimates were higher among respondents from the recent cohort. 64.3% and 36.9% respondents with a history of lifetime abuse and dependence had remitted respectively. The number of sociodemographic associations for the onset of each transitional stage decreased from alcohol use to alcohol dependence. Onset of ever-use was more common in respondents who were male, 18-50 years of age, with middle education level, and never married, but less common among the previously married and students. First onset of regular use among those with ever-use was more common in respondents who were male, less than 50 years of age and never married, but less common in students. Being male and less than 50 years of age was associated with more alcohol abusers among regular users.
Conclusion
This study was the first to reveal in a Chinese population that qualitatively different risk factors might operate during the different stages of progression from alcohol use to disorders. Further research is needed to clarify the mechanisms underlying these differences in order to guide prevention programs.
Keywords: alcohol, abuse, dependence, remission, transitions, China
INTRODUCTION
Alcohol use in China has an ancient history that dated back to 7,000 BC according to the discovery of an early wine jar in the village of Jiahu in Henan province (1). Regular as well as binge drinking are legitimized in a variety of Chinese social circumstances with little perception that alcohol can induce harm. During Maoist China, alcohol drinking was considered bourgeois and largely brought to a halt. Following the country’s economic reform that began in 1978, however, alcohol consumption has continued to rise (2,3). Commercial alcohol production in China has increased more than 50-fold per capita since 1952 (3). Using an identical methodology, two national surveys conducted in 1994 and 2001 found that the volume of annual alcohol consumption per person increased from 3.6 to 4.6 liters, while the incidence rates of acute intoxication increased from 2.6% to 8.3% (4-6). Likewise, recent surveys in metropolitan Wuhan (the capital of Hubei Province) found that the lifetime and 12-month rates of alcohol use increased from 77.78% and 68.20% in 2002 to 80.44% and 73.63% in 2005 (7).
Previous prevalence estimates of alcohol use disorders in China are inconsistent because of variations in methodology, diagnostic criteria, and types of disorders and prevalence reported. The two national surveys mentioned above indicated no change in the point prevalence of alcohol dependence (3.4% and 3.8% respectively) (4-6). By contrast, two national surveys of a wide range of mental disorders, performed in 1982 and 1993 respectively, found that lifetime prevalence of alcohol dependence had increased from 0.009% to 0.068%, thereby moving from the ninth to the third most prevalent mental disorder in China (8,9). Likewise, a regional survey in Shangdong province found that the current prevalence rate of alcohol dependence increased from 0.036 % in 1984 to 0.134 % in 1994 (10). Thus, the overall picture of alcohol dependence in China is one of modest increase over time though the reported rates remained low by Western standard.
The results of previous surveys in China cannot easily be compared with most published work because they did not use internationally standardized methods of assessment. Moreover, all the surveys focused primarily on the prevalence and risk factors of alcohol dependence. They did not take account of transitions regarding the spectrum of problematic alcohol use that ranged from non-drinking to first use, regular use, abuse or/and dependence. However, Western studies that examined differential associations of initiation of alcohol consumption and the transitions to subsequent stages of alcohol use suggested that the targets of intervention might vary by different developmental periods (11-14). Besides, the cohort effect of alcohol use and disorders and the sociodemographic correlates of remission from alcohol use disorders, both of which have been examined in Western studies (13-18), were not investigated in previous Chinese surveys. Therefore, we set out to examine not only the prevalence and risk factors of alcohol use disorders but also the sociodemographic correlates pertaining to different stages of alcohol use and disorders and remission, and their association with cohorts by using an internationally standardized methodology in two of the most rapidly growing cities in China, namely, Beijing and Shanghai.
MATERIALS AND METHODS
This study is a part of the World Mental Health (WMH) Survey Initiative (http://www.hcp.med.harvard.edu/wmh/). The training and assessment of interviewers, sampling, field procedure and quality control of this study were standardized. The key methodological aspects of this study were described below.
Sample
A three-stage clustered area probability sampling strategy according to household register was employed to survey 18-70 year old adults in the metropolitan areas of Beijing and Shanghai (19,20). In first-stage sampling, 4162 neighborhood committees (NCs) in Beijing (containing 2,009,253 households) and 2319 NCs in Shanghai (containing 2,507,416 households) were designated in the sampling pool. According to probabilities proportional to size (PPS) measures, 47 NCs in Beijing and 44 NCs in Shanghai were selected and the field samplers went to these NCs to check their actual residential distribution against the obtained demographic data. In the second stage, a sample of households were selected randomly for each NC according to pre-decided sampling intervals and the random starting point. In the third stage, all eligible members of the selected households were recorded by the field sampler and one eligible person was randomly chosen.
The 180 interviewers consisted of graduate students from several universities in Beijing and Shanghai. They received a seven-day training session according to a standardized training procedure set by the WMH Collection Coordination Center (19,21). The training session covered rationale of the questionnaire design, the content and sequence of questions, interview skills, dealing with refusals, role-play exercise and pilot interviews. During data-collection fieldwork, filled questionnaires were checked and debriefing to interviewers was provided by supervisors on a daily basis. There was also random checking on completed interviews through telephone and in-person visits. From November 2001 and February 2002, a total of 5201 face-to face interviews (including 2633 in Beijing and 2568 in Shanghai) were conducted in the respondents’ home by the trained lay-interviewers. The response rates were 74.8% (Beijing) and 74.6% (Shanghai). The interviews were administered in two parts. All 5201 respondents completed part-1 interview which included the core mental disorders diagnostic assessment, including alcohol use and disorders. All respondents who met criteria for at least one mental disorder during the part-1 interview and a 25% probability sub-sample of other part-1 respondents (n=1628) received part-2 interview which included additional questions about the correlates and disorders of secondary interest, such as chronic physical disorders, time-varying risk factors, and costs of illness. All respondents provided written informed consent prior to the interview.
Measure
The WMH version of Composite International Diagnostic Interview (WMH-CIDI) was a fully structured interview schedule for collecting information about mental disorder and socio-demographic variables of respondents. Mental disorders, including alcohol abuse and dependence, were diagnosed according to the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (14,22,23). Version 3.0 of the WMH-CIDI was translated into Chinese using the standard WHO protocol (19,24). A blind clinical reappraisal study found that substance use disorders diagnosis generated from the Structured Clinical Interview for DSM-IV (SCID) (25,26) had generally good concordance with the WMH-CIDI 3.0 diagnoses. The sensitivity, specificity and area under the receiver operator characteristic curve of the Chinese WMH-CIDI for alcohol use disorders were 87.0%, 98.3% and 92.6% respectively (27).
The alcohol module of the WMH-CIDI began with a screening question about the age of respondents when they first drank an alcoholic beverage (ever-use): “How old were you the very first time you ever drank an alcoholic beverage?” If the respondent reported ever-use, age of onset (AOO) of regular-use and alcohol disorders was asked as “How old were you when you first started drinking at least 12 drinks in a year?” and “How old were you the very first time you had any of these problems?”, using a list of symptoms related to alcohol abuse and dependence. Remission was defined as the cessation of use and the absence of any pre-existing symptom (of abuse and dependence) for at least two years before interview. Among respondents with a history of remitted alcohol abuse and dependence, the most recent age of having any symptom among respondents was assessed by asking the following question - “How old were you the last time you had [this problem/ (either/any) of these problems] because of drinking?”. Additional variables were created to represent the speed of transition between onset of first use and onset of first regular use among lifetime regular users, as well as the speed of transition between onset of first regular alcohol use and onset of abuse.
A number of socio-demographic variables were asked in separate sections of part II of the WMH-CIDI. Age-at-interview was categorized into four groups (18-34 years, 35-49 years, 50-64 years, and ≥ 65 years). Education level was assumed to be orderly and categorized into current students, none or primary (having finished 0-6 years of education), junior high school (7-9 years), senior high school (10-12 years) and university and more (13 years or more). Marital status was categorized into “never married”, “previously married” and “married/cohabitating”. Year of education and year of transition for marital status were also asked and later treated as time-varying covariates for survival analyses.
Statistical Analysis
Statistical analyses of this study were based on the part-2 sample, which over-sampled those having disorders and under-sampled those without. Weighting was used to adjust for this and differential probabilities of selection within households and for residual discrepancies between the sample and official population statistics on the cross-classification of sociodemographic variables. Projected AOO distributions of the cumulative lifetime probability of alcohol use, regular use, abuse and dependence as of age 60 were estimated by the actuarial method implemented in PROC LIFETEST in SAS (version 9.1.3, SAS Institute, Cary, N.C.).
Sociodemographic correlates of transitions across six stages of use and disorders (non-use, ever-use, regular use, abuse, dependence, remission) were analyzed with discrete-time survival models using the person-year as the unit of analysis (28). In this approach, each year in the life of each respondent up to and including the AOO of the outcome disorder was treated as a separate observational record, with years after the AOO deleted from the data file. A regression model was then estimated using a logit of probit link function in which a separate dummy control variable was included for each year of life. The regression coefficients for the substantive predictors can then be interpreted as predictive effects on the conditional odds (logit) or risk (probit) of onset in a given year among respondents with no prior lifetime history of the outcome assuming proportional odds (logit) or hazards (probit). This approach of analysis allows us to model transitions to subsequent stages of alcohol use while accounting for those individuals who might not have passed through the period of risk. The correlates included age-at-interview, gender, education and marital status (the latter two were treated as time-varying correlates), each of which was analysed separately while others were statistically controlled. The person-year data array used in the transition from never-use to first-use included all years before and including their age of having their first drink, while the array for the latter three transitions (ever-use to regular-use, regular-use to abuse, abuse to dependence) included all years beginning from the last year of earlier stage transition and continuing through the year of onset of the next stage or, for respondents who never made the next transition, through their age–at-interview. For the transition from abuse-dependence to remission, the person-year data array was defined as all years beginning from year after the first onset of abuse and continuing either to remission as defined before or until 1 year prior to age–at-interview. In addition, the equations for later stages included additional covariates on the onset and timing of earlier stages. This same process was applied in all equations that included information about multiple earlier transitions. The final models, however, included only those AOO/transition variables that showed consistent associations with the respective transition.
This approach yielded results that are similar to those obtained using a complementary log-log function and reporting hazard ratios. It was preferred because of easier interpretability. Confidence intervals (CIs) of the Odds Ratios (ORs) were estimated using the Taylor series linearization method (29) through the SUDAAN software package (release 8.0.1, January, 2002; Research Triangle Institute, Research Triangle Park, NC, USA) in order to adjust for the fact that the sample was clustered and the cases were weighted. Multivariate significance was evaluated using Wald χ2 tests based on coefficient variance–covariance matrices that were adjusted for design effects using the Taylor series method. Statistical significance was evaluated using 0.05-level two-sided design-based tests.
RESULTS
Prevalence of Alcohol Ever Use, Regular Use, Abuse and Dependence
More than half of the respondents (65.4%, 95% CI=61.9-68.9%) reported that they had ever drunk at least a sip of alcohol beverage in their life. 39.5% (95% CI= 36.6-42.4%), i.e., 60.4% (95% CI= 56.15-64.7%) among these ever-drinkers, reported using alcohol regularly at some time in their life. Lifetime prevalence estimates of alcohol abuse and alcohol dependence were 4.6% (95% CI= 3.4-5.8%) and 0.9% (95% CI= 0.5-1.3%) respectively. 11.6% (95% CI= 8.7-14.5%) of regular users developed alcohol abuse; 20.4% (95% CI= 13.5-27.3%) of lifetime alcohol abusers turned into alcohol dependence. Among respondents with a history of lifetime abuse and dependence, 64.3% (95% CI= 48.0-80.6%) and 36.9% (95% CI= 17.9-55.9%) of them had remitted.
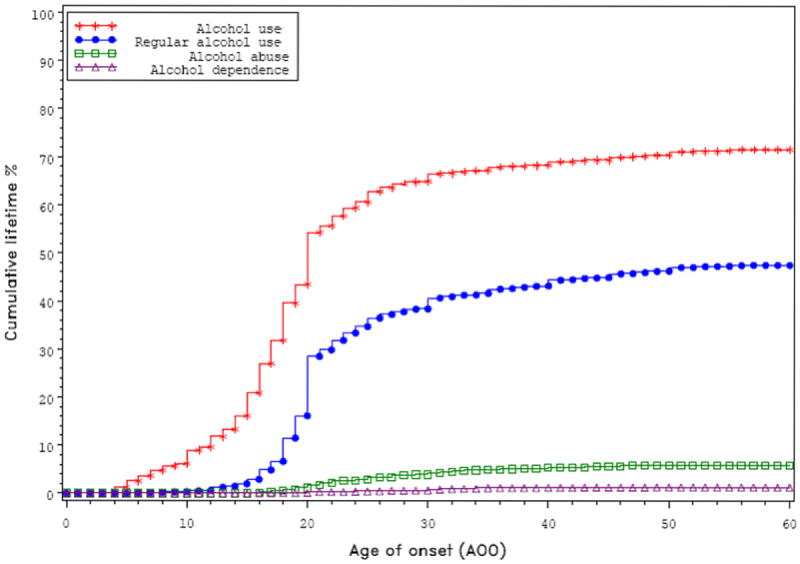
Age-of-Onset of Alcohol Use, Abuse and Dependence
Figure 1 shows the cumulative AOO curves for ever-use, regular-use, alcohol abuse and alcohol dependence. The cumulative incidence of ever-use showed the sharpest increase in adolescence before and including age 20, in which more than half of all projected lifetime users began use in 18-19 years of age. For regular-use, the sharpest increase also occurred in adolescence before and including age 20, with the median AOO in 20-21 years. Alcohol abuse and dependence increased slowly with median AOO in 25-26 and 28-29 years respectively. The majority of first occurrence of lifetime abuse and dependence happened between 20-31 years of age.
Figure 1. Age of onset of alcohol use, regular use, abuse, and dependence of each user in the total part-2 sample.
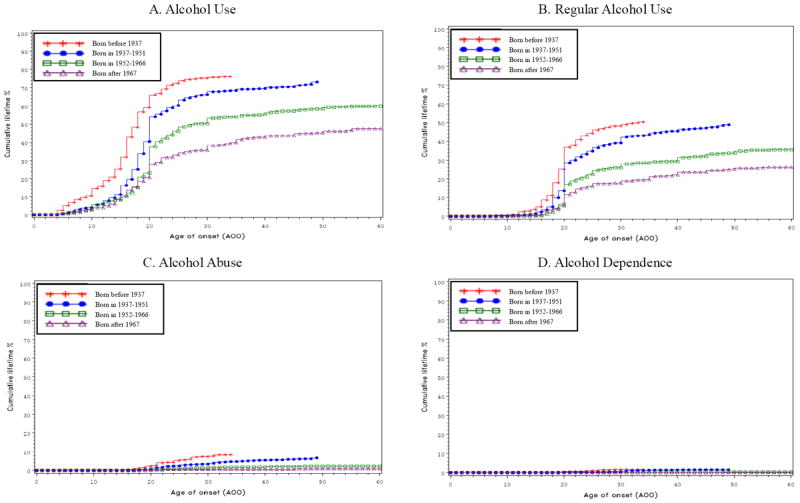
Association between cohort and onset of alcohol use and disorders
All stages of alcohol use and disorders were more common in recent than early cohorts, though the increase of cumulative prevalence of alcohol dependence did not diverge distinctively among cohorts owing to small sample size of those in dependence (Figure 2). From the earliest to the most recent cohorts (born before 1937, in 1937-1951, in 1952-1966 and after 1967), 47.4%, 59.9%, 73.1%, and 76.1% had ever used alcohol respectively; the lifetime prevalences of regular use were 26.1%, 35.5%, 48.9%, 50.3% respectively. Prevalences of lifetime abuse (0.9%, 2.2%, 6.6%, 8.3%) and dependence (0.0%, 0.3%, 1.3%, 1.6%) also increased across cohorts. Moreover, while ever-use and regular-use increased sharply around the age of twenties for all cohorts, the increase was earlier for the most recent cohort than the earlier cohorts.
Figure 2. Age of onset of alcohol stages in the total part-2 sample according to cohort.
Sociodemographic associations of alcohol use, abuse and dependence in transition and remission
Table 1 shows the results from discrete-time survival analyses for sociodemographic associations of stage transitions from alcohol use to disorder. Generally speaking, from alcohol use to alcohol dependence, the number of sociodemographic associations for onset of each stage decreased. Gender and age at interview were always significantly associated with transition from non-use to ever-use, ever- use to regular-use, and regular-use to abuse. All these transitions were more common in male respondents and respondents below 50 years old (especially from 18 to 34 years of age). Educational level and marital status at the time of onset exhibited significant associations for the first and to a lesser extent the second stage, but not the subsequent stages. Ever-use was significantly more common in those never-married, and significantly less common among students and those previously married. Regular-use among ever-users was significantly more common only among those never married, and significantly less common among students. Stronger risk estimates, as indicated by the average ORs, were shown in later-stage transitions (especially in the transition from regular use to abuse) for gender and age, but for education and marital status they were shown in the earlier stage transitions (especially in the transition from none use to ever use).
Table 1.
Sociodemographic associations for transition to discrete stages of alcohol-related outcome
| Socio-demographic | Sociodemographic Category | Ever-use among Part-2 Sample (n=1628) | Regular-use among Ever-users (n=1063) | Abuse among regular -users (n=673) | Dependence among abusers (n=116) | ||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | ||
| Age at interview | 18-34 | 2.86 | (2.07 - 3.96) | 1.73 | (1.11 - 2.70) | 5.57 | (2.20 - 14.11) | 2.04 | (0.42 - 9.79) |
| 35-49 | 1.77 | (1.42 - 2.21) | 1.36 | (0.90 - 2.04) | 2.64 | (1.21 - 5.73) | 2.07 | (0.36 - 11.80) | |
| 50-64 | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | |
| 65+ | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | |
| Sex | Female | 0.52 | (0.43 - 0.62) | 0.24 | (0.17 - 0.35) | 0.25 | (0.09 - 0.73) | 0.89 | (0.12 - 6.92) |
| Male | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | |
| Education at the time of onset | Student | 0.42 | (0.30 - 0.59) | 0.52 | (0.30 - 0.90) | 0.92 | (0.29 - 2.92) | 1.19 | (0.11 - 12.35) |
| None or primary | 0.80 | (0.52 - 1.22) | 1.05 | (0.54 - 2.05) | 1.42 | (0.31 - 6.53) | 0.40 | (0.01 - 10.88) | |
| Junior high school | 1.29 | (0.92 - 1.80) | 0.90 | (0.58 - 1.39) | 1.00 | (0.43 - 2.32) | 1.29 | (0.33 - 5.14) | |
| Senior high school | 1.40 | (0.96 - 2.04) | 1.45 | (0.92 - 2.30) | 0.85 | (0.36 - 1.98) | 1.03 | (0.32 - 3.31) | |
| College and more | 1.0 | -- | 1.0 | -- | 1.0 | -- | 1.0 | -- | |
| Marital status at the time of onset | Never married | 5.32 | (3.21 - 8.83) | 1.68 | (1.09 - 2.59) | 0.94 | (0.41 - 2.12) | 0.7 | [0.945] |
| Previously married | 0.38 | (0.15 - 0.94) | 1.29 | (0.42 - 3.92) | 1.55 | (0.51 - 4.72) | 0.70 | (0.19 - 2.61) | |
| Married/Cohabiting | 1.0 | -- | 1.0 | -- | 1.0 | -- | 0.42 | (0.03 - 5.10) | |
| Age of onset | of first alcohol use | --- | --- | 1.01 | (0.98 - 1.04) | 0.97 | (0.91 - 1.04) | --- | --- |
| of regular alcohol use | --- | --- | --- | --- | --- | --- | 1.13 | (0.99 - 1.28) | |
Results are based on multivariate discrete-time survival model with person-year as the unit of analysis. OR indicates odds ratio; CI, confidence interval.
Remission of alcohol abuse with/without dependence was associated with age at interview, education and onset age of alcohol abuse. Remission was more common among student abusers and abusers with older age of onset, but less common among abusers in middle age (35-49 years and 50-64 years) compared to the oldest age group (60+ age-group)(Table 2).
Table 2.
Sociodemographic associations for remission of alcohol use disorders
| Socio-demographic | Sociodemographic Category | Remission of alcohol use disorders (abuse/dependence) (n=116)
|
|
|---|---|---|---|
| OR | (95% CI) | ||
| Age at interview | 18-34 | 0.09 | (0.00 - 3.11) |
| 35-49 | 0.03 | (0.00 - 1.01) | |
| 50-64 | 0.01 | (0.00 - 0.33) | |
| 65+ | 1.0 | -- | |
| Sex | Female | 2.11 | (0.83 - 5.35) |
| Male | 1.0 | -- | |
| Education when last with abuse/dependence | Student | 11.70 | (1.33 - 102.87) |
| None or primary | 0.90 | (0.04 - 18.99) | |
| Junior high school | 1.38 | (0.41 - 4.68) | |
| Senior high school | 1.32 | (0.41 - 4.30) | |
| College and more | 1.0 | -- | |
| Marital status when last with abuse/dependence | Never married | 2.58 | (0.70 - 9.59) |
| Previously married | 0.98 | (0.25 - 3.79) | |
| Married/Cohabiting | 1.0 | -- | |
| Age of onset | of first alcohol abuse | 1.22 | (1.11 - 1.34) |
Results are based on multivariate discrete-time survival model with person-year as the unit of analysis. OR indicates odds ratio; CI, confidence interval.
DISCUSSION
This is the first study in China to examine sociodemographic associations in each stage of alcohol use and disorders and the pattern of association with cohorts. Our main findings included a strong cohort association in the transition from non-use to ever-use, and a decreasing number of sociodemographic correlates in the transition from use to disorders.
Previous studies in China indicated that male gender was a consistent risk factor and older age was usually a risk factor for alcohol use and disorders (8,10,30-33). They also generally found that lower education and divorced status were correlates (10,30,31,34). By examining the spectrum of alcohol use and disorders, the present study found that the number of sociodemographic associations for the onset of each stage decreased from alcohol use to use disorders. Younger age and male gender were always associated with transition from non-use to ever-use, ever-use to regular-use, and regular-use to alcohol use disorders. Educational level and marital status, which are more related to socio-environmental factors than age and gender, exhibited associations for the first and to a lesser extent the second stage of transition but not the subsequent stages. Moreover, the transitional pattern of risk estimates according to ORs was noteworthy. The decreasing sample number from none use to use and use to disorders notwithstanding, stronger risk estimates were shown in later-stage transitions (especially from regular use to abuse) for gender and age, but for education and marital status, the stronger risks were in the earlier stage transitions (especially from none use to ever use). These findings suggested that qualitatively different risk factors might operate during the different stages of progression of alcohol use. They could indicate that environmental or cultural variables played a greater role in earlier phases of use, while transition to alcohol use disorders was more influenced by biological factors. As suggested by twin studies and prospective studies, genetic and familial factors had more influence on the development of heavy drinking and alcohol dependence than early stages of alcohol use (35,36). According to research in molecular genetics, genetic polymorphism related to alcohol metabolic pathways might protect a large proportion of Chinese people from heavy drinking (37-39). From these perspectives, alcohol disorders in China may not reach the level found in Western countries even if the rate of use is similar. Indeed, the prevalences of alcohol use in the present study (lifetime: 65.4%, 12-month: 40.2%) resembled those of the U.S. in 1997 (lifetime: 66.0%, 12-month: 44.4%) (13), but the prevalences of dependence (lifetime: 0.9%, 12-month: 0.6%) were much lower than in the U.S. (life time: 13.3%, 12-month: 4.4%) (13). However, because of the complex gene-environment interactions that may occur with social change, the prevalence of dependence may rise in China as the younger cohorts of regular users grow old.
The association with cohort in the present study resembled Western studies which found that alcohol use, abuse and dependence were more common among people born after World War II (13,14,18). We found that alcohol use and disorders were more common in younger than older cohorts and the most recent cohort started to drink and regular drink at an especially early age. This may be explained by recent decades of socioeconomic change in China. Prior to 1978, alcohol was not easily available in the country for both political and economic reasons. But subsequent economic reform has steadily improved people’s standard of living and facilitated rapid expansion of the drinking industry. The latter is shown by the emergence of numerous Western style pubs and bars that did not exist in Chinese cities previously. Along with the fact that there are few legal regulations on purchase, consumption and selling of alcohol (2,3), use of alcohol has grown rapidly. Unsurprisingly, the national production of alcoholic beverages increased markedly from 3.7 million tons in 1980 to over 50 million tons in 2007 (40,41). Younger cohorts of Chinese people who have lived through China’s economic boom are therefore more likely to use alcohol and develop early-onset disorders. This suggests that alcohol use disorders are likely to rise in future.
Few Western studies have simultaneously examined how risk factors and AOO differentially predict transitions across the different stages of alcohol use, disorders and remission. The one exception is a study based on data from the National Comorbidity Survey – Replication (NCS-R) which used the same instrument as ours (14). Both studies found that young age was associated with transitions to alcohol use and disorders (14). This is different from previous studies on alcohol dependence in China, which indicated that older age was a risk factor (10,31-33). Previous Western studies generally found a positive association between early AOO and disorder severity (42-44), suggesting that a later AOO of alcohol abuse increased the chance of remission. Accordingly, we found as in the U.S. study that AOO of abuse was positively associated with remission from abuse and dependence. But unlike the US study (14), we found that middle age at interview (35-64 years) was negatively associated with remission. Future research should examine whether this was related to the popularity of binge-drinking for social and business reasons in China (2,3,45), as a result of which drinkers might not quit alcohol till they were retired or exhibited significant deterioration in physical health. Unlike the US study (14) too, we found that students were less likely to start ever-use and regular-use, and more likely to remit from alcohol use disorders. This might partly arise from very strict school regulations against alcohol use in China.
The present study has several limitations that are worthy of note. Given that China still consists of about 70% of rural regions and even its urban areas are heterogeneous, our findings cannot be generalized to other parts of the country. Thus, a previous survey of nine Chinese cities showed that the current prevalence of alcohol dependence ranged widely from 1.6% to 8.0% (34). The rather low lifetime prevalence of alcohol dependence (0.9%) found in the present study made the sample size of dependence not large enough to investigate reliable sociodemographic correlates of transition from abuse to dependence and remission from alcohol dependence. It was not only lower than suggested by other Chinese surveys (5,6,46,47) but also low relative to the prevalence of abuse (4.6%). The latter might be due to both methodological and substantive factors. The prevalence estimate of dependence could be attenuated because the DSM-IV system requires a greater number of criteria to diagnose dependence than abuse. Such attenuation was also found in the NCS-R, which found that the lifetime prevalence for alcohol abuse and dependence was 13.2% and 5.4% respectively (14). Moreover, the version of WMH-CIDI we used did not diagnose dependence if there was no abuse symptom because of previous findings that dependence without abuse was very rare (48). This is a limitation that will be addressed in future versions of the CIDI. The lower lifetime prevalence of dependence might also reflect the cultural pattern of alcohol use pattern in China. This is because Chinese norms discourage daily solitary drinking but encourage social and celebratory drinking (2,3,45), thereby reducing the risk of developing dependence. Additionally, our sampling excluded migrant laborers who frequently changed work place and did not possess household registration in Beijing and Shanghai, but previous studies showed that they exhibited a higher prevalence of alcohol use and disorders, particularly dependence, than the general population (33,49,50).
To aid recall of AOO, we provided respondents with information necessary for distinguishing AOO for each of the stages of alcohol use. There were also a series of probes for respondents who could not recall the exact age. One of the probes was “was it before your twenties?” and if the respondents answered “yes”, the upper end of the range (20 years of age) was used in analysis to give a consistently conservative, lower-bound estimate. Nonetheless, the validity of this retrospective AOO recall method in the WMH-CIDI has not been examined. Thus, our finding of a sharp increase around the age of 20 might partly result from the above-mentioned methodological aid. Another limitation of our study was that more memory decay could occur among older respondents, especially those who were infrequent lifetime users. Bias might also occur because of the tendency of respondents to report experiences closer in time to the interviews. However, as the estimates of AOO tend to increase with age, there is no indication that the rank ordering for the different events is affected (14). In the Chinese context of rapid socio-cultural change and increasing consumption of alcohol beverage in recent decades, our finding of the most recent cohort starting to drink and regularly drink earlier in life was plausible. This observed cohort effect should be examined in prospective longitudinal research which will also overcome the problem of comparability of cross-sectionally identified cohorts, especially as population mobility related to internal migration is common in China nowadays.
The combinations of transitions from one stage to other stages can be complex. Dependence can arise from abuse or heavy solitary use, and can go onto abstinence at one time and relapse at another. The present study has not examined this transitional complexity. Finally, the decreasing numbers from ever use to dependence might lead to decreased statistic powers for analysis at later stages of transition. This might partly contribute to the decreased number of significant associations from use to disorders. Nonetheless, the findings of increased (gender and age) as well as decreased (marital and education status) risk elevations towards later stages of transition suggested that decreasing number of significant associations was not simply a consequence of decreasing sample size across stages. The NCS-R which had a large sample size and used an identical method of analysis reported similar findings (14).
These limitations apart, our study provided preliminary information about the stages at which different individual characteristics might confer risks to the development of alcohol disorders in a Chinese population. Given that there is little organized alcohol treatment and prevention service throughout China, such information, if enriched by further studies, will help identify high-risk individuals and potentially improve the precision and affordability of prevention programs.
Acknowledgments
The Chinese WMH Survey Initiative is supported by the Pfizer Foundation in conjunction with the World Health Organization WMH Survey Initiative. We thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis. These activities were supported by the United States National Institute of Mental Health (R01MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864 and R01 DA016558), the Fogarty International Center (FIRCA R01-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, Inc., Glaxo-SmithKline, Bristol–Myers Squibb and Sanofi Aventis. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/
Contributor Information
Sing Lee, Department of Psychiatry, The Chinese University of Hong Kong, HKSAR, PRC.
Wan-jun Guo, Department of Psychiatry, The Chinese University of Hong Kong, HKSAR, PRC.
Adley Tsang, Hong Kong Mood Disorders Center, The Chinese University of Hong Kong, HKSAR, PRC.
Yan-ling He, Shanghai Mental Health Center, PRC.
Yue-qin Huang, Institute of Mental Health, Peking University, PRC.
Ming-yuan Zhang, Shanghai Mental Health Center, PRC.
Zhao-rui Liu, Institute of Mental Health, Peking University, PRC.
Yu-cun Shen, Institute of Mental Health, Peking University, PRC.
Ronald C. Kessler, Department of Health Care Policy, Harvard Medical School, MA, USA.
References
- 1.McGovern Patrick E. Ancient Wine: The Search for the Origins of Viniculture. Vol. 314 Princeton: Princeton University Press; 2003. [Google Scholar]
- 2.Hao W, Chen H, Su Z. China: alcohol today. Addiction. 2005;100:737–741. doi: 10.1111/j.1360-0443.2005.01036.x. [DOI] [PubMed] [Google Scholar]
- 3.Cochrane J, Chen H, Conigrave KM, Hao W. Alcohol use in China. Alcohol Alcohol. 2003;38:537–542. doi: 10.1093/alcalc/agg111. [DOI] [PubMed] [Google Scholar]
- 4.Su Z, Hao W, Chen H. Alcohol Consumption and Alcohol - Related Problems in Five Areas in China. Alcohol Pattern, Alcohol Consumption and Alcohol-Related Problems in Five Areas in China: 1. Alcohol Patterns and Annual Consumption. Chinese Mental Health Journal. 2003;17:536–539. [Google Scholar]
- 5.Su Z, Hao W, Chen H. Collaborate Group for 2nd Survey on Alcohol Drinking in Five Areas in China. Alcohol Pattern, Alcohol Consumption and Alcohol-Related Problems in Five Areas in China: 3. Problems Related to Alcohol Use in General Population. Chinese Mental Health Journal. 2003;17:544–546. [Google Scholar]
- 6.Wei H, Derson Y, Xiao S, Li L, Zhang Y. Alcohol consumption and alcohol-related problems: Chinese experience from six area samples, 1994. Addiction. 1999;94:1467–1476. doi: 10.1046/j.1360-0443.1999.941014673.x. [DOI] [PubMed] [Google Scholar]
- 7.Zhang J, Casswell S, Cai H. Increased drinking in a metropolitan city in China: a study of alcohol consumption patterns and changes. Addiction. 2008;103:416–423. doi: 10.1111/j.1360-0443.2007.02088.x. [DOI] [PubMed] [Google Scholar]
- 8.Twelve Region Psychiatric Epidemiological Study Work Group. A national 12-region psychiatric epidemiological study – methodology and results. Chinese Journal of Neurology and Psychiatry. 1986;19:65–69. [PubMed] [Google Scholar]
- 9.Zhang W, Shen Y, Li S, Cheng C, Huang Y, Wang J, et al. Epidemiological investigation on mental disorders in 7 areas of China. Chin J Psychiatry. 1998;31:69–71. [Google Scholar]
- 10.Liu Z, Zhang J, Weng Z. A ten-year survey of patients with dependence on alcohol in Shandong Province. Chinese Journal of Behavioral Medical Science. 1999;8:293–295. [Google Scholar]
- 11.Jackson KM, Sher KJ, Gotham HJ, Wood PK. Transitioning into and out of large-effect drinking in young adulthood. J Abnorm Psychol. 2001;110:378–91. doi: 10.1037//0021-843x.110.3.378. [DOI] [PubMed] [Google Scholar]
- 12.Guo J, Collins LM, Hill KG, Hawkins JD. Developmental pathways to alcohol abuse and dependence in young adulthood. J Stud Alcohol. 2000;61:799–808. doi: 10.15288/jsa.2000.61.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grant BF. Prevalence and correlates of alcohol use and DSM-IV alcohol dependence in the United States: results of the National Longitudinal Alcohol Epidemiologic Survey. J Stud Alcohol. 1997;58:464–473. doi: 10.15288/jsa.1997.58.464. [DOI] [PubMed] [Google Scholar]
- 14.Kalaydjian A, Swendsen J, Chiu W-T, Dierker L, Degenhardt L, Glantz M, et al. Sociodemographic predictors of transitions across stages of alcohol use, disorders and remission in the National Comorbidity Survey-Replication. Comprehensive Psychiatry. 2009 doi: 10.1016/j.comppsych.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001-2002. Addiction. 2005;100:281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- 16.Dawson DA, Grant BF, Stinson FS, Chou PS. Estimating the effect of help-seeking on achieving recovery from alcohol dependence. Addiction. 2006;101:824–834. doi: 10.1111/j.1360-0443.2006.01433.x. [DOI] [PubMed] [Google Scholar]
- 17.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 19.Shen YC, Zhang MY, Huang YQ, He YL, Liu ZR, Cheng H, et al. Twelve-month prevalence, severity, and unmet need for treatment of mental disorders in metropolitan China. Psychol Med. 2006;36:257–267. doi: 10.1017/S0033291705006367. [DOI] [PubMed] [Google Scholar]
- 20.Heeringa SG, Wells JE, Hubbard F, Mneimneh ZN, Chiu WT, Sampson NA, et al. Sample designs and sampling procedures. In: Kessler RC, Üstün TB, editors. The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. New York: Cambridge University Press; 2008. pp. 14–32. [Google Scholar]
- 21.Pennell BE, Mneimneh ZN, Bowers A, Chardou S, Wells JE, Viana MC, et al. Implementation of the World Mental Health Surveys. In: Kessler RC, Üstün TB, editors. The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. New York: Cambridge University Press; 2008. pp. 33–57. [Google Scholar]
- 22.Kessler RC, Üstün TB. The World Health Organization Composite International Diagnostic Interview. In: Kessler RC, Üstün TB, editors. The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. New York: Cambridge University Press; 2008. pp. 58–90. [Google Scholar]
- 23.Kessler RC, Abelson J, Demler O, Escobar JI, Gibbon M, Guyer ME, et al. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMH-CIDI) Int J Methods Psychiatr Res. 2004;13:122–139. doi: 10.1002/mpr.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harkness J, Pennell BE, Villar A, Gebler N, Aguilar-Gaxiola S, Bilgen I. Translation procedures and translation assessment in the World Mental Health Survey Initiative. In: Kessler RC, Üstün TB, editors. The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. New York: Cambridge University Press; 2008. pp. 91–113. [Google Scholar]
- 25.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) New York: Biometrics Research, NewYork State Psychiatric Institute; 2002. [Google Scholar]
- 26.Haro JM, ArbabzadehBouchez S, Brugha TS, Girolamo Gd, Guyer ME, Jin R, et al. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res. 2006;15:167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang YQ, Liu ZR, Zhang MY, Shen YC, Tsang A, He YL, et al. Mental Disorders and Service Use in China. In: Kessler RC, Ustun TS, editors. World Health Organization World Mental Health Survey Series Volume One – Patterns of mental illness in the WMH Surveys. Yew York: Cambridge University Press; 2008. pp. 447–473. [Google Scholar]
- 28.Efron B. Logistic regression, survival analysis, and the Kaplan-Meier curve. J Am Stat Assoc. 1988;83:414–25. [Google Scholar]
- 29.Wolter KM. Introduction to variance estimation. New York: Springer-Verlag; 1985. [Google Scholar]
- 30.Wu B, Mao ZF, Rockett IR, Yue Y. Socioeconomic status and alcohol use among urban and rural residents in China. Subst Use Misuse. 2008;43:952–966. doi: 10.1080/10826080701204961. [DOI] [PubMed] [Google Scholar]
- 31.Wang LH, Zhu ZH, Li ZB. An epidemiological research of alcohol dependence and its related fators. Chin Bull Drud Depend. 1994;3:22–29. 21. [Google Scholar]
- 32.Jiafang Z, Jiachun W, Yunxia L, Xiaoxia Q, Ya F. Alcohol abuse in a metropolitan city in China: a study of the prevalence and risk factors. Addiction. 2004;99:1103–1110. doi: 10.1111/j.1360-0443.2004.00799.x. [DOI] [PubMed] [Google Scholar]
- 33.Guo W, Lanzi G, Luobu O, Ma X, Zhen P, Ji Y, et al. An epidemiological survey of alcohol use disorders in a Tibetan population. Psychiatry Res. 2008;159:56–66. doi: 10.1016/j.psychres.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 34.Collaborative Research Group on Alcoholism and Related Problems. Epidemiological survey on alcohol dependence in populations of four occupations in nine cities of China (I) methodology and prevalence. Chinese Mental Health Journal. 1992;6:112–115. 142. [Google Scholar]
- 35.Sartor CE, Lynskey MT, Heath AC, Jacob T, True W. The role of childhood risk factors in initiation of alcohol use and progression to alcohol dependence. Addiction. 2007;102:216–225. doi: 10.1111/j.1360-0443.2006.01661.x. [DOI] [PubMed] [Google Scholar]
- 36.Whitfield JB, Zhu G, Madden PA, Neale MC, Heath AC, Martin NG. The genetics of alcohol intake and of alcohol dependence. Alcohol Clin Exp Res. 2004;28:1153–1160. doi: 10.1097/01.alc.0000134221.32773.69. [DOI] [PubMed] [Google Scholar]
- 37.Dick DM, Foroud T. Candidate genes for alcohol dependence: a review of genetic evidence from human studies. Alcohol Clin Exp Res. 2003;27:868–879. doi: 10.1097/01.ALC.0000065436.24221.63. [DOI] [PubMed] [Google Scholar]
- 38.Higuchi S, Matsushita S, Kashima H. New findings on the genetic influences on alcohol use and dependence. Curr Opin Psychiatry. 2006;19:253–265. doi: 10.1097/01.yco.0000218595.54054.7a. [DOI] [PubMed] [Google Scholar]
- 39.Zintzaras E, Stefanidis I, Santos M, Vidal F. Do alcohol-metabolizing enzyme gene polymorphisms increase the risk of alcoholism and alcoholic liver disease? Hepatology. 2006;43:352–361. doi: 10.1002/hep.21023. [DOI] [PubMed] [Google Scholar]
- 40.Wang YC. Work report of the fifth Session of the third Council meeting of China Alcoholic Drinks Industry association; Wuhan. 2008. [Google Scholar]
- 41.Huang SM, editor. China Annals of food industries: 2000. Beijing: Chinese statistic press; 2001. [Google Scholar]
- 42.Hasin DS, Glick H. Severity of DSM-III-R alcohol dependence: United States, 1988. Br J Addict. 1992;87:1725–1730. doi: 10.1111/j.1360-0443.1992.tb02685.x. [DOI] [PubMed] [Google Scholar]
- 43.Pitkanen T, Lyyra AL, Pulkkinen L. Age of onset of drinking and the use of alcohol in adulthood: a follow-up study from age 8-42 for females and males. Addiction. 2005;100:652–661. doi: 10.1111/j.1360-0443.2005.01053.x. [DOI] [PubMed] [Google Scholar]
- 44.Hingson RW, Heeren T, Winter MR. Age at drinking onset and alcohol dependence: age at onset, duration, and severity. Arch Pediatr Adolesc Med. 2006;160:739–746. doi: 10.1001/archpedi.160.7.739. [DOI] [PubMed] [Google Scholar]
- 45.Kim JH, Lee S, Chow J, Lau J, Tsang A, Choi J, Griffiths SM. Prevalence and the factors associated with binge drinking, alcohol abuse, and alcohol dependence: a population-based study of Chinese adults in Hong Kong. Alcohol Alcohol. 2008;43:360–370. doi: 10.1093/alcalc/agm181. [DOI] [PubMed] [Google Scholar]
- 46.Pan G, Jiang C, Yang X, Na J, Fu Z, Yu Q, et al. Epidemiological survey of mental disorders in urban and rural areas of Liaoning province. Chin J Public Health. 2006;22:830–842. [Google Scholar]
- 47.Huang J, Li K, Liu D, Cui L, Gao Y, Li G. Epidemiological survey of alcohol abuse and dependence in Hebei Province. Chinese Journal of Drug Abuse Prevention and Treatment. 2008;14:33–34. 58. [Google Scholar]
- 48.Degenhardt L, Bohnert K, Anthony JC. Case ascertainment of alcohol dependence in general population surveys: “gated” versus “ungated” approaches. Int J Methods Psychiatr Res. 2007;16(3):111–23. doi: 10.1002/mpr.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hao W, Young DS, Xiao SY, Wang SJ, Deng JL, Biao MZ, et al. Alcohol drinking and related problems in six areas in China: Part IV. The risk factors for alcohol dependence. Chinese Journal of Clinical Psychology. 1999;7:4–8. [Google Scholar]
- 50.Lin D, Li X, Yang H, Fang X, Stanton B, Chen X, et al. Alcohol intoxication and sexual risk behaviors among rural-to-urban migrants in China. Drug Alcohol Depend. 2005;79:103–112. doi: 10.1016/j.drugalcdep.2005.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]


