Abstract
This study investigated the prevalence and demographic correlates of active and ever-smokers in Beijing and Shanghai. Using a multi-stage household probability sampling method, 5201 participants aged 18–70 underwent face-to-face interviews using the Composite International Diagnostic Interview. 67.1% and 55.5% of male and 7.1% and 5.5% of female respondents were ever-smokers and active smokers respectively. Quitting was less common by proportion among those no longer married or nevered married, middle-aged or working adults. After adjusting for other sociodemographic factors, the oldest age-group (>54 years) showed a significantly negative association with active smoking while those no longer married had significantly positive association with active smoking, among ever-smokers. Although the high prevalence of male smoking in Beijing and Shanghai was expected, the prevalence of female smoking was significantly higher than those found in previous surveys. This pattern of more female smoking not accompanied by an obvious decrease in male smoking defies the expectation of an orderly transition of smoking patterns and may foreshadow smoking patterns in other parts of China.
Keywords: active smoking, quitting, epidemiology, metropolitan China
1. Introduction
In the last two decades, there were three national surveys of smoking in China. They showed that the prevalences of smokers were 61.0%, 66.9% and 66% in males and 7.04%, 4.2% and 3.1% in females respectively (Weng et al., 1986; Yang et al., 1999). Thus, rates of smoking were persistently high in Chinese males and, somewhat unexpectedly, female smokers could be decreasing. These surveys did not report on specific urban or rural areas where the patterns and health consequences of smoking likely vary (Peto, Chen, & Boreham, 2009). Except for the second national survey, Chinese studies on smoking did not analyze patterns of association for continuing to smoke, once smoking had started, in relation to socioeconomic and demographic characteristics (Weng et al, 1986; Yang, Ma, Liu, & Zhou, 2005). However, understanding the mode of transition of smoking in China is essential for policy purposes. According to the 4-stage model of the global impact of the spread of tobacco proposed by Lopez, Collishaw, & Piha (1994), China should currently be in stage II (i.e., persistence of male excess among smokers) and should be moving onto stage III (i.e., converging of the prevalences of smoking among males and females following decline of male smoking and an increase in the proportion of female smokers). Because of China’s uneven pace of development, it is unclear if its change in patterns of smoking will follow such an orderly transition. A study of metropolitan areas such as Beijing and Shanghai may help identify certain epidemiological pattern of smoking that will unfold in the other parts of China.
2. Methods
2.1. Samples
The World Mental Health (WMH) Survey Initiative in Beijing and Shanghai was conducted between November 2001 and February 2002. Respondents were selected from a multi-stage clustered area probability sample with a response rate of 74.8% in Beijing (n=2,633) and 74.6% in Shanghai (n=2,568). The interview was divided into two parts to reduce respondent burden. All 5,201 respondents completed part-1 interview which contained standardized items on personal characteristics and a core diagnostic assessment for selected psychiatric disorders. Those who met criteria for at least one mental disorder and a 25% probability sub-sample of other part-one respondents (n=1628) received part-2 interview which included additional questions about chronic physical disorders, risk factors, and costs of illness. All respondents provided written consent after being informed about the study goals, procedures, data uses and protections, and participant rights. The institutional review board of the participating organizations approved and monitored the compliance of human participant protection. Training and assessment of interviewers, sampling and field procedure were undertaken according to the standardized procedures of the WMH Consortium (Kessler & Üstün, 2008).
2.2. Measures
The survey used the WMH version of the Composite International Diagnostic Interview (WMH-CIDI, Kessler & Üstün, 2008). It was translated into Chinese using the standard WHO protocol, in which a team of survey experts completed the initial translation, a separate team carried out an independent back translation, and any discrepancies were adjusted (Shen et al., 2006). For this study, active smoker and ever-smokers (i.e., active smokers and ex-smokers combined) were identified as those who endorsed the question “Are you a current smoker [active], ex-smoker [former], or have you never smoked?”. Besides gender and age, other demographic correlates included marital status (widowed, separated, or divorced), education level (primary education or lower, finished primary but not yet finished secondary education, finished secondary education, some tertiary education, and finished tertiary education) and employment status (working, student, homemaker, retired and other, including being unemployed).
2.3. Data analysis
While the data were weighted according to population census, we estimated proportions of ever-smokers in relation to time invariant characteristics such as age and gender as well as potentially modifiable and time-varying characteristics such as employment and marital status. Then we used simple cross-tabulations to estimate their associations with active-smokers. Covariate-adjusted odds ratios (OR) were estimated via the generalized linear model with a logistic link and were used to convey the strength of association with active smoker, against former smoker, and each covariate of interest. To avoid the shrinkage of the sample size making the regression model imprecise and unstable, the education variable, which was only available for the part-two sample, was not included in regression analysis. Standard errors and confidence intervals were estimated using the Taylor series linearization approach in STATA (Stata Corporation, 2005). All significance tests were made using two-sided tests evaluated at the 0.05 level of significance.
3. Results
3.1. Prevalence of ever-smokers and active smokers
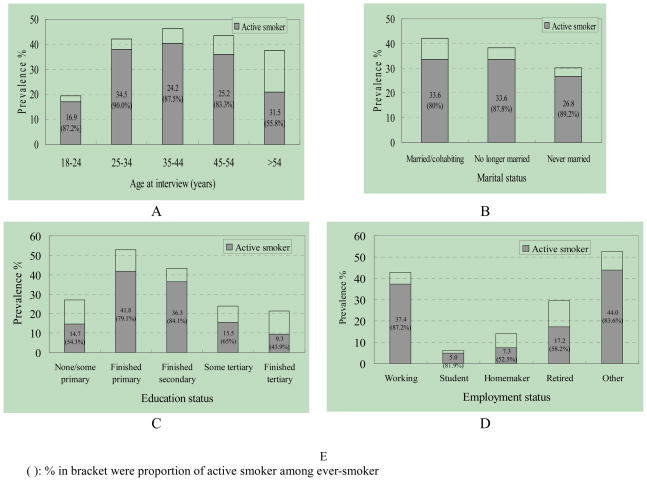
67.1% (SE=1.3%) of male and 7.1% (SE=0.7%) of female respondents were ever-smokers, of whom 82.7% (SE=1.1%) and 77.4% (SE=3.9%) respectively were active smokers. That is, the prevalence of male and female active smokers was 55.5% and 5.5% respectively. As for the distribution of ever-smokers and active smokers among age-groups, their proportions increased with age and reached the highest in middle adulthood (46.2%. SE=1.4%). These then fell off with age (fig. 1).
Fig. 1.
Estimated prevalence of ever-smokers and active smoker by sociodemographics
There was a higher prevalence of ever-smokers among those who were married/cohabiting (42%, SE=1.0%) than those who were never married (30%, SE=2.2%, fig. 1). As for education status, the highest prevalence of ever-smokers and active smokers was found among those finishing primary education (52.9%, SE=3.7%); the lowest was among those who finished tertiary education (21.2%, SE=9.0%, fig. 1). Among employment status subgroups, the largest group difference in the prevalence of ever-smokers and active smokers was between students (6.1%, SE=1.8%) and “other” subgroup which included those unemployed (52.6%, SE=2.7%, fig. 1).
3.2. Active smokers versus quitters
Tabulating the proportion of active smokers among ever-smokers could identify those more likely to quit versus those likely to continue smoking. While this was consistent among most age-groups (83.3%–90%), the proportion in the oldest age-group (>54years) was significantly smaller (55.8%), i.e., close to half had quitted. The never-married subgroup had a larger proportion of active smokers (89.2%, SE=2.1%) than those married/cohabiting (80%, SE=1.2%, fig. 1). The proportion of active smokers was lowest in the group with highest educational level. The working subgroup topped in terms of the proportion of active smokers (87.2%, SE=1.1%, fig. 1), i.e. the working subgroup had the smallest proportion of quitters.
The above preliminary results showed that there were higher proportions of active smokers among young adults, those never-married, and working adults (i.e. less than 20% had quitted). The regression models showed that the oldest age-group (>54 years) was less likely (adjusted OR=0.26, 95% CI=0.08–0.87, p=0.03) to remain as active smokers (and more likely to quit) with reference to the youngest age-group (18–24 years) (Table 1). Those who were no longer married were more likely to remain as active smokers and less likely to quit (adjusted OR=2.58, 95% CI=1.56–4.29, p<0.01) with reference to those who were married or cohabiting. Gender and employment status were not significant covariates in the model.
Table 1.
Logistic regression of active smokers among ever-smokers by sociodemographic
| factors | OR(95%CI) | t (p) |
|---|---|---|
| Gender | ||
| Male | 1 | - |
| Female | 0.98 (0.56–1.72) | −0.07 (0.947) |
| Age | ||
| 18–24 | 1 | - |
| 25–34 | 1.42 (0.51–3.94) | 0.71 (0.485) |
| 35–44 | 1.15 (0.35–3.74) | 0.24 (0.811) |
| 45–54 | 0.85 (0.28–2.55) | −0.30 (0.766) |
| 55–70 | 0.25 (0.08–0.87) | −2.29 (0.031) |
| Marital Status | ||
| Married / Cohabited | 1 | - |
| Never married | 1.31 (0.63–2.72) | 0.75 (0.462) |
| No longer married | 2.58 (1.56–4.29) | 3.86 (0.001) |
| Employment Status | ||
| Working | 1 | - |
| Student | 0.57 (0.11–3.03) | −0.69 (0.495) |
| Homemakers | 0.62 (0.14–2.66) | −0.67 (0.506) |
| Retired | 0.69 (0.36–1.35) | −1.12 (0.272) |
| Other | 0.74 (0.46–1.20) | −1.27 (0.216) |
4. Discussion
4.1. Limitations
We did not assess several aspects of smoking topology that may be relevant to studying exposure to tobacco, such as quantity or frequency of smoking, the type of tobacco smoked, and the route of administration. Respondents who were self-identified as ever smokers might include a heterogeneous group of individuals with different levels of exposure. Since the study was restricted to a metropolitan sample, our findings are not generalizable to other parts of China.
4.2. Main findings
Our findings on the overall prevalence of smoking were similar to those of the previous national surveys in several aspects. Male smokers greatly over-numbered female smokers, while the prevalence estimates of male ever and active smoker were comparable (Yang et al., 2005). This confirmed that besides an ever smoking prevalence approaching those of high income countries, the relative proportion of male versus female smokers was much higher in China than in most other countries (World Health Organization, 1997). The prevalence of smokers by age group, which concentrated in middle adulthood, was also similar. That prevalence declined further in the oldest age group was an expected finding (Hyland et al, 2004; Weng et al, 1986; Yang et al., 1999, 2005 & 1999). Besides, people with low education were more likely to smoke (Yang et al., 1999, 2005). These similarities apart, our estimates for female ever and current smokers (7.1% and 5.5% respectively) were more than twice of those found in the latest national survey (3.1% and 2.6% respectively, Yang et al., 2005).
Regarding active smokers among ever-smokers, the overall proportion of active smokers among ever smokers was the highest among all the countries of the WMH Consortium (Storr et al., resubmitted). Although female smoking remained low, the proportion of female active-smokers among ever-smokers was comparable to that of males. Expectedly, those no longer married were more likely to remain active-smokers and less likely to quit than those who were married or cohabiting (Nystedt, 2006). Those with higher education exhibited a lower percentage of smokers and a higher proportion of quitters among ever-smokers, suggesting that educated individuals possessed more knowledge about the harm of smoking. Finally, there was a higher proportion of active smokers among never-married working young- and middle-aged adults.
4.3. Female Smoking
Cigarette smoking is said to be a gender discriminator that “encourages men to smoke as a sign of masculinity and discourages women lest they be regarded as dissolute” in China (Xiao & Kohrman, 2008). Although the overall rate of female smoking in China is still low globally (WHO, 1997), we found a much higher prevalence (7.1%) of smoking among females than in the last two national surveys. The proportion of active smokers among ever smokers among females was one of the two highest among countries of the WMH Consortium (Storr et al., resubmitted). Women in Beijing and Shanghai were likely to be influenced by values about modern womanhood and tobacco-related marketing to a greater extent than their counterparts in the rest of the country. It is possible that their pattern of smoking may foreshadow what will occur in other parts of China where female smoking is presently rare.
4.4. Staging Smoking in China
Regarding the application of their 4-stage model to different geographical regions, Lopez and colleagues (1994) remarked that it is unlikely that “the principal defining characteristics of each phase would alter” (p.242). Our finding of a likely pattern of more females becoming active smokers that was not accompanied by a decrease in high rates of male smoking suggested that the stage of smoking in metropolitan China (as represented by Beijing and Shanghai) was somehow closer and yet not corresponding to stage III. Although active smoking among ever smokers was persistently high among males and even higher among females, the current prevalence of female smoking was still lower than what would normally occur in stage II. The prevalence of active smoking is expected to be lower among middle-aged men as many of them should have become ex-smokers, but our findings showed that the proportion of active smokers among ever smokers for the 35–55 age–group was the highest.
Lopez’s model was based on developed countries where the economy and health services have evolved more steadily and evenly. Cultural factors, rapid economic development, and under-developed anti-tobacco policy may render the model not readily applicable for describing the pattern of progression of smoking in China. It has been noted that the pattern of smoking in China in the 1980s was similar to that of the U.S. in the 1950s (Yu et al., 1990). In the absence of effective policy and programs, however, China may not evolve into stage IV with a beneficial decline in smoking-related mortality and morbidity as in the U.S. A study of the smoking characteristics of U.S. workers in 1978–1980 showed few differences in prevalence of smoking among men and women for specific occupations (Brackbill, Frazier, & Shilling, 1988). This is hardly true of the recent situation of workers in China.
Acknowledgments
The Chinese WMH Survey Initiative is supported by the Pfizer Foundation in conjunction with the World Health Organization WMH Survey Initiative. We thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis. These activities were supported by the United States National Institute of Mental Health (R01MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864 and R01 DA016558), the Fogarty International Center (FIRCA R01-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, Inc., Glaxo-SmithKline, Bristol–Myers Squibb and Sanofi Aventis. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Brackbill R, Frazier T, Shilling S. Smoking characteristics of US workers, 1978–1980. American Journal of Industrial Medicine. 1988;13(1):5–41. doi: 10.1002/ajim.4700130103. [DOI] [PubMed] [Google Scholar]
- Hyland A, Li Q, Bauer JE, Giovino GA, Steger C, Cummings KM. Predictors of cessation in a cohort of current and former smokers followed over 13 years. Nicotine Tobacco Research. 2004;6:S363–369. doi: 10.1080/14622200412331320761. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Üstün TB. The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. New York: Cambridge University Press; 2008. [Google Scholar]
- Lopez AD, Collishaw NE, Piha T. A descriptive model of the cigarette epidemic in developed countries. Tobacco Control. 1994;3:242–247. [Google Scholar]
- Nystedt P. Marital life course events and smoking behaviour in Sweden: 1980–2000. Social Science and Medicine. 2006;62:1427–1442. doi: 10.1016/j.socscimed.2005.08.009. [DOI] [PubMed] [Google Scholar]
- Peto R, Chen ZM, Boreham J. Tabacco: the growing epidemic in China. CVD Prevention and Control. 2009 doi: 10.1016/j.cvdpc.2008.12.001. [DOI] [Google Scholar]
- Shen YC, Zhang MY, Huang YQ, He YL, Liu ZR, Cheng H, Tsang A, Lee S, Kessler RC. Twelve-month prevalence, severity, and unmet need for treatment of mental disorders in metropolitan China. Psychological Medicine. 2006;36:257–267. doi: 10.1017/S0033291705006367. [DOI] [PubMed] [Google Scholar]
- Stata Corporation. Stata statistical software: Release 9. College Station, TX: Stata Corporation; 2005. [Google Scholar]
- Weng XZ, Hong SG, Chen DY, Chen BZ, Tian BC. National smoking survey of a random sample of half a million persons in 1984. Journal of Cardiovascular and Pulmonary Diseases. 1986;4:44–48. (in Chinese) [Google Scholar]
- World Health Organization. Tobacco or health: A Global Status Report. Geneva, Switzerland: WHO; 1997. [Google Scholar]
- Xiao SY, Kohrman M. Anthropology in China’s health promotion and tobacco. Lancet. 2008;372(9650):1617–1618. doi: 10.1016/S0140-6736(08)61361-6. [DOI] [PubMed] [Google Scholar]
- Yang G, Fan L, Tan J, Qi G, Zhang Y, Samet JM, Taylor CE, Becker K, Xu J. Smoking in China: findings of the 1996 National Prevalence Survey. Journal of American Medical Association. 1999;282:1247–1253. doi: 10.1001/jama.282.13.1247. [DOI] [PubMed] [Google Scholar]
- Yang GH, Ma JM, Liu N, Zhou LN. Smoking and passive smoking in Chinese, 2002. Chinese Journal of Epidemiology. 2005;26:77–83. (in Chinese) [PubMed] [Google Scholar]
- Yu JJ, Mattson ME, Boyd GM, Mueller MD, Shopland DR, Pechacek TF, Cullen JW. A comparison of smoking patterns in the People’s Republic of China with the United States: An impending health catastrophe in the middle kingdom. Journal of American Medical Association. 1990;264:1575–1579. [PubMed] [Google Scholar]