Abstract
Aims and Objectives:
To assess the prevalence of metabolic syndrome (MetS) in human immunodeficiency virus (HIV) positive patients. Prevalence of MetS was compared in patients who were not on highly active antiretroviral therapy (HAART) to patients who were on HAART.
Materials and Methods:
Seventy HIV positive cases were studied. Pregnant and lactating women, patients on drugs other than HAART known to cause metabolic abnormalities and those having diabetes or hypertension were excluded. Cases were evaluated for MetS by using National Cholesterol Education Program Adult Treatment Panel-III.
Results:
47 cases were on HAART and 23 cases were not on HAART. Fasting Blood Glucose ≥100 mg/dl was present in 28.6% cases, out of whom 27.7% were on HAART and 30.4% were not on HAART (P = 0.8089). 12.9% cases had BP ≥130/≥85 mm Hg, out of whom 14.9% were on HAART and 8.7% were not on HAART (P = 0.4666). 42.9% cases had TG ≥150 mg/dl, out of whom 44.7% were on HAART and 39.1% were not on HAART (P = 0.6894). HDL cholesterol was low (males <40 mg/dl, females <50 mg/dl) in 50% cases, out of whom 55.3% were on HAART and 39.1% were not on HAART (P = 0.2035).
Conclusions:
Prevalence of MetS was 20%. Majority of patients had only one component of MetS (32.9%). Low HDL was present in 50%, followed by raised triglycerides in 42.9%. Waist circumference was not increased in any of the patients. There was no statistically significant difference between those on HAART and those not on HAART in distribution of risk factors and individual components of MetS.
Keywords: Highly active antiretroviral therapy, human immunodeficiency virus, metabolic syndrome
INTRODUCTION
Metabolic abnormalities including increased lipid levels, abnormal fat distribution, elevated blood pressure, and disturbances in glucose metabolism have frequently been reported in individuals infected with HIV.[1–4] Cross-sectional studies have reported a prevalence of diabetes of 2% to 7% among HIV-infected patients receiving protease inhibitors,[3,5,6] an additional 16% having impaired glucose tolerance. Between 33 and 75% of patients with HIV infection receiving HAART develop lipodystrophy, consisting of elevations in plasma triglycerides, total cholesterol, and apolipoprotein B, as well as hyperinsulinemia and hyperglycemia. Approximately 20% of the patients with HIV-associated lipodystrophy meet the criteria for the MetS. This study was done to assess MetS in HIV-positive patients. Prevalence of MetS was compared in patients who were not on HAART to patients who were on HAART.
MATERIALS AND METHODS
Informed consent was taken from the patients and a thorough clinical and biochemical examination was done to look for metabolic abnormalities. Criteria proposed by the third report of the National Cholesterol Education Program (NCEP) expert panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) were used for evaluation of MetS. Elevated waist circumference (men ≥90 cm, women ≥80 cm), elevated triglycerides (≥150 mg/dL or taking medication), reduced HDL cholesterol or taking medication (men ≤40 mg/dL, women ≤50 mg/dL), elevated blood pressure (≥130/≥85 mm Hg or use of medication for hypertension), elevated fasting glucose (≥100 mg/dL or use of medication for hyperglycemia). Presence of three out of five criteria was taken for diagnosis of MetS. Study was conducted at nodal ART center from July 2010 to July 2011. All HIV positive patients were taken; pregnant and lactating females, patients already diagnosed case of diabetes, hypertension and taking drugs like lipid lowering drugs, oral contraceptive pills, β-blockers, glucocorticoids and diuretics were excluded from the study.
Risk factors mean components of metabolic syndrome (MetS), one risk factor means one component, two risk factor means two components and so on. Cases of 18 years of age and more were studied and most of them were in age group of 30–45 years (82.9%). Variables demonstrating a univariate relationship (P < 0.05) with the outcome variable were included in the logistic regression analysis to assess the effect of independent variables on MetS diagnosis.
RESULTS
Out of 70 cases, 71.4% were males and 28.6% were females. Raised blood pressure was found in 12.9% cases, HDL cholesterol was low in 54% males and 35% females. Triglycerides were raised in 42.9% cases and FBG was elevated in 28.6% cases. Waist circumference was not increased in any case. On studying risk factor distribution, a total of 32.9% cases were found to have one risk factor out of whom 36.2% cases were on HAART and 26.1% were not on HAART (P = 0.3986). Two risk factors were present in 18.6% cases, out of whom 21.3% were on HAART and 13% were not on HAART (P = 0.4055). MetS (≥3 risk factors) was present in 20% cases, out of whom 19.1% were on HAART and 21.7% were not on HAART (P = 0.7991). Total 28.6% cases were those not having any risk factor, out of whom 23.4% were on HAART and 39.1% were not on HAART (P = 0.6394).
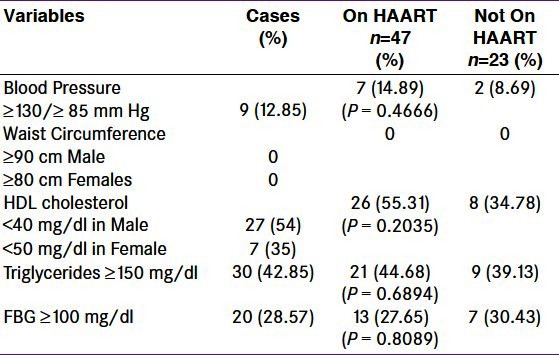
Prevalence of MetS in the present study was 20%. Proportion of HIV positive cases who had FBG ≥100 mg/dl was 28.6%, out of whom 27.7% were on HAART and 30.4% were not on HAART. (P = 0.8089). Total 12.9% cases were having BP ≥130/≥85 mm Hg, out of whom 14.9% were on HAART and 8.7% were not on HAART (P = 0.4666). Total 42.9% cases were having TG ≥150 mg/dl, out of whom 44.7% were on HAART and 39.1% were not on HAART (P = 0.6894). HDL cholesterol values were low in 50% cases, out of whom 55.3% were on HAART and 39.1% were not on HAART (P = 0.2035) [Table 1].
Table 1.
Components of metabolic syndrome of 70 human immunodeficiency virus positive cases
DISCUSSION
Prevalence of MetS in the present study was 20%. Various Indian studies have reported prevalence of MetS in general population between 3% and 25%.[7,8] Jericó et al.[9] reported 17% prevalence of MetS which increased from 5.1% among HIV-infected patients under age 30 years to 27.0% for those aged 50–59 years while Samaras et al.[10] reported the prevalence of MetS to be 18%. Falutz et al.[11] showed prevalence of MetS varying from 19% to 26% depending on the specific definition used, and only a minority of patients (5%) satisfied the criteria for all of the definitions. Total of 601 patients completed the metabolic survey in a study done by Mondy et al.[12] among whom 26% had MetS. Worm et al.[13] demonstrated an increase in the proportion of patients with MetS from 19.4% to 41.6% over 6 years follow up. A study done by Gazzaruso et al.[14] among HIV patients found the prevalence of MetS to be 45.4%.
In the present study, total 32.9% cases were found to have one risk factor, out of whom 36.2% were on HAART and 26.1% were not on HAART. Two risk factors were present in 18.6% cases, out of whom 21.3% were on HAART and 13% were not on HAART. MetS (≥3 risk factors) was present in 20%, out of whom 19.1% were on HAART and 21.7% were not on HAART. Total 28.6% cases did not have any risk factor, out of whom 23.4% were on HAART and 39.1% were not on HAART [Table 2, Figure 1].
Table 2.
Number of metabolic syndrome risk factors in cases
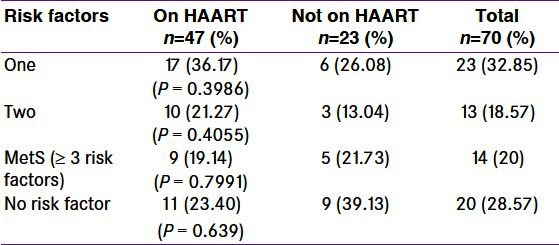
Figure 1.
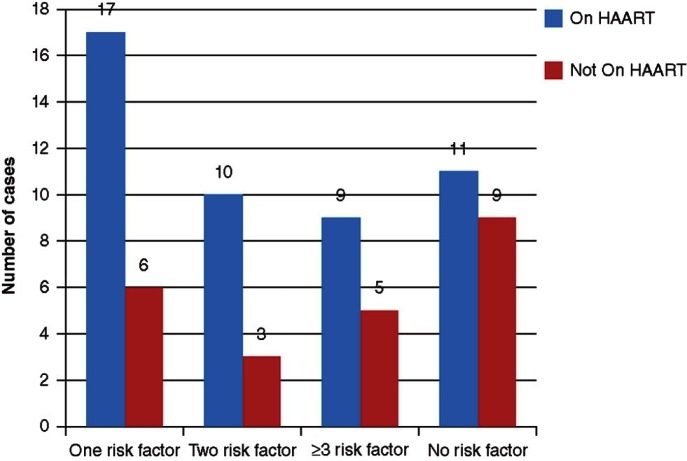
Distribution of risk factors
Jericó et al.[9] showed presence of one or more features of MetS in 69.3% patients, two or more in 35.8%, three or more in 17%, four or more in 4.5%, and five features in 0.1%, thus yielding a prevalence of 17% (95%, CI 14–20%). 47% of the HIV-infected patients satisfied at least one definition for MetS and a minority of the patients (5%) satisfied the criteria for all of the definitions in a study done by Falutz et al.[11] Many patients (49%) had at least two features of MetS but were not classified as having MetS. MetS was more common in those currently receiving protease inhibitors (P = 0.04). Gazzaruso et al.[14] showed one risk factor was present in 19.5% patients, two in 17.2%, three in 26.4%, four in 12.1%, and five in 6.9%. Of the subjects, 17.9% showed no risk factors.
In the present study FBG ≥100 mg/dl was present in 28.6% cases, out of whom 27.7% were on HAART and 30.4% were not on HAART (P = 0.8089) [Table 1]. Jericó et al.[9] reported raised FBG in 11.5% of the cases while Gazzaruso et al.[14] reported the same in 24.0% of the cases.
In the present study, 12.9% cases had BP ≥130/≥85 mm Hg, out of whom 14.9% were on HAART and 8.7% were not on HAART (P = 0.4666) [Table 1]. Jericó et al.[9] showed raised blood pressure was present in 26.3% cases. Worm et al.[13] stated the proportion of patients with hypertension increased from 15.9% at entry level to 54.5% of those under follow up over 6 years. Hypertension was present in 31.4% in HIV-infected cohort studied by Mondy et al.,[12] while Gazzaruso et al.[14] reported hypertension among 42.3% HIV patients.
In the present study, 42.9% cases had TG ≥150 mg/dl, out of whom 44.7% were on HAART and 39.1% were not on HAART (P = 0.6894) [Table 1]. Raised triglycerides were reported in 43.1%, 44% and 59.3% cases by Jericó et al.,[9] Mondy et al.[12] and Gazzaruso et al.,[14] respectively. In the present study HDL cholesterol values were low in 50% cases, out of whom 55.3% were on HAART and 39.1% were not on HAART (P = 0.2035) [Table 1]. Jericó et al.[9] demonstrated low HDL levels in 35.63% cases while Mondy et al.[12] reported 43.5% cases to have low HDL, while 52.4% of HIV-infected patients were shown to have low HDL by Gazzaruso et al.[14]
In the present study, none of the cases had increased waist circumference. However, increased waist circumference was reported in 12.5% of cases by Jericó et al.[9] Presence of increased waist circumference was seen in 30.7% and 37.8% of cases in studies conducted by Mondy et al.[12] and Gazzaruso et al.,[14] respectively.
CONCLUSIONS
Prevalence of MetS was 20% among HIV-infected patients, which is not different from that in HIV negative patients. Majority of patients had only one component of MetS (32.85%). Low HDL was present in 50% of patients followed by raised triglycerides in 42.85%. Waist circumference was not increased in any of the patients. There was no statistically significant difference between those on HAART and those not on HAART in distribution of risk factors and individual components of MetS. MetS is an important risk factor for cardiovascular disease. Timely identification, lifestyle modification and treatment are important to prevent complications.
Limitations of the study
Due to the constraints of a time bound study and a small sample size, the results in the present study are subject to type II error and hence cannot be generalized.
Footnotes
Source of Support: Nil
Conflict of Interest: No
REFERENCES
- 1.Dube MP, Johnson DL, Currier JS, Leedom JM. Protease inhibitor associated hyperglycemia. Lancet. 1997;350:713–4. doi: 10.1016/S0140-6736(05)63513-1. [DOI] [PubMed] [Google Scholar]
- 2.Dever LL, Oruwari PA, Figueroa WE, O’Donovan CA, Eng RH. Hyperglycemia associated with protease inhibitors in an urban HIV-infected minority patient population. Ann Pharmacotherapy. 2000;34:580–4. doi: 10.1345/aph.19231. [DOI] [PubMed] [Google Scholar]
- 3.Carr A, Samaras K, Thorisdottir A, Kaufmann GR, Chisholm DJ, Cooper DA. Diagnosis, prediction, and natural course of HIV-1 protease-inhibitor-associated lipodystrophy, hyperlipidemia, and diabetes mellitus; a cohort study. Lancet. 1999;353:2093–9. doi: 10.1016/S0140-6736(98)08468-2. [DOI] [PubMed] [Google Scholar]
- 4.Currier J, Boyd F, Kawabata H. Diabetes mellitus in HIV infected individuals [abstract 677-T] Presented at the th Conference on Retrovirus and Opportunistic Infections, Seattle. 2002 Feb [Google Scholar]
- 5.Hammer SM, Squires KE, Hughes, Grimes JM, Demeter LM, Currier JS, et al. A controlled trial of two nucleoside analogues plus indinavir in persons with human immunodeficiency virus infection and CD4 cell counts of 200 per cubic millimeter of less. N Engl J Med. 1997;337:725–32. doi: 10.1056/NEJM199709113371101. [DOI] [PubMed] [Google Scholar]
- 6.Vigouroux C, Gharakhanian S, Salhi Y, Nguyen TH, Chevenne D, Capeau J, et al. Diabetes, insulin resistance and dyslipidaemia in lipodystrophic HIV-infected patients on highly active antiretroviral therapy (HAART) Diabetes Metab. 1999;25:225–32. [PubMed] [Google Scholar]
- 7.Deepa R, Shantiram CS, Premlalitha G, Shanti NG, Mohan V. Prevalence of insulin resistance syndrome in a selected south Indian population-the Chennai urban population study-7 [CUPS-7] Indian J Med Res. 2002;115:118–27. [PubMed] [Google Scholar]
- 8.Gupta A, Gupta R, Sarna M, Rastogi S, Gupta VP, Kothari K, et al. Prevalence of diabetes, impaired fasting glucose and insulin resistance syndrome in an urban Indian population. Diab Res Clin Pract. 2003;61:69–76. doi: 10.1016/s0168-8227(03)00085-8. [DOI] [PubMed] [Google Scholar]
- 9.Jericó C, Knobel H, Montero M, Ordoñez-Llanos J, Guelar A, Gimeno JL, et al. MetS among HIV-Infected Patient. Diabetes Care. 2005;28:144–9. doi: 10.2337/diacare.28.1.132. [DOI] [PubMed] [Google Scholar]
- 10.Samaras K, Wand H, Law M, Emery S, Cooper D, Carr A, et al. Prevalence of metabolic syndrome in HIV-infected patients receiving highly active antiretroviral therapy using International Diabetes Foundation and Adult Treatment Panel III criteria: associations with insulin resistance, disturbed body fat compartmentalization, elevated C-reactive protein, and [corrected] hypoadiponectinemia. Diabetes Care. 2007;30:113–9. doi: 10.2337/dc06-1075. [DOI] [PubMed] [Google Scholar]
- 11.Falutz J, Rosenthall L. HIV and MetS (Met-Syn): Characteristics of patients and limitations of current diagnostic classifications. Program and abstracts of the 16th International AIDS Conference; August 13-18, 2006; Toronto, Canada. Abstract WEPE0145 [Google Scholar]
- 12.Mondy K, Overton ET, Grubb J, Tong S, Seyfried W, Powderly W, et al. Metabolic syndrome in HIV-infected patients from an Urban, Midwestern US outpatient population. Clin Infect Dis. 2007;44:726–34. doi: 10.1086/511679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Worm SW, Friis-Møllera N, Bruyandd M, D’Arminio Monfortee A, Rickenbachf M, Reiss P, et al. High prevalence of the Metabolic syndrome in HIV-infected patients: Impact of different definitions of the Metabolic syndrome. AIDS. 2010;24:427–35. doi: 10.1097/QAD.0b013e328334344e. [DOI] [PubMed] [Google Scholar]
- 14.Gazzaruso C, Sacchi P, Garzaniti A, Fratino P, Bruno R, Filice G. Prevalence of metabolic syndrome among HIV patients. Diabetes Care. 2002;25:1253–4. doi: 10.2337/diacare.25.7.1253. [DOI] [PubMed] [Google Scholar]


