Abstract
Background:
Gestational diabetes mellitus (GDM) is a perfect window of opportunity for the prevention of DM in two generations, and its incidence is increasing in our country. Awareness of the condition among antenatal women will translate into prevention and early diagnosis of the disease. This study was done to determine the awareness of GDM among all the antenatal women who attend a Primary Health Center (PHC) for antenatal care.
Materials and Methods:
A pretested questionnaire consisting of details on background characteristics, 12 questions focusing on Type 2 DM and GDM, and a question on the source of knowledge was administered to all women attending the antenatal clinic. Their responses were scored and the women were graded as having good, fair, or poor knowledge about GDM.
Results:
One hundred and twenty antenatal women participated in the study. Mean age of the women was 23.8 years (SD: 2.94). Overall, 17.5% women had good knowledge, 56.7% had fair knowledge, and 25.8% women had poor knowledge about GDM. The major sources of awareness of GDM were reported to be television/radio, neighbors/friends, and family members.
Discussion:
Only a small proportion of rural antenatal women had good knowledge about GDM. The awareness that untreated GDM may pose a risk to the unborn child was high among the study women. Health care workers have to play a greater role in bringing about awareness about GDM among antenatal women.
Keywords: Antenatal women, awareness, gestational diabetes mellitus, source of knowledge
INTRODUCTION
With an estimated 50.8 million people living with diabetes, India has the largest diabetes population in the world and has the dubious distinction of being the diabetes capital of the world.[1] Gestational diabetes mellitus (GDM) is one of the subtypes of diabetes, the prevalence of which is constantly increasing. GDM is defined as glucose intolerance that is first detected during pregnancy.[2] GDM is associated with an increased risk of pre-eclampsia for mothers in the antepartum period and a higher risk for macrosomia, hypoglycemia, jaundice, respiratory distress syndrome, polycythemia, and hypocalcemia in infants.[3] After delivery, though the glucose levels return to normalcy, the mother is at a higher risk for Type 2 DM, and the child of a woman with GDM is at a higher risk for metabolic syndrome.[3]
Diabetes complicates between 1 and 20% of all pregnancies worldwide, which includes pregestational diabetes mellitus (PGDM) and GDM.[4] There are ethnic differences in the prevalence of PGDM and GDM. The South Asian race is at a higher predisposition for both Type 2 DM and GDM.[5,6] In a recent community-based study conducted by Seshiah, et al. in South India, GDM was detected among 17.8% of the women in urban, 13.8% in semiurban, and 9.9% women in rural areas based on the two-hour 75 g postglucose value ≥140 mg/dL.[7]
Most of the available literature pertains to the awareness of diabetes among women in the general population or awareness of GDM among antenatal women diagnosed to have GDM and there has not been any study done on the awareness of GDM among all antenatal women in general, with or without GDM.[8,9] Once the antenatal women are diagnosed to have GDM, they are put into the high-risk category and referred to a higher level of health-care facilities for follow-up care. Knowledge about GDM among antenatal women will translate into adoption of a healthy lifestyle, better healthcare-seeking pattern, better self-care, and thus prevention and early diagnosis of the disease. Hence, this study was done to determine the awareness of GDM among all the antenatal women who attend a Primary ealth Center (PHC) for antenatal care.
MATERIALS AND METHODS
This study was conducted in a PHC in Kanchipuram district in the state of Tamil Nadu. The PHC caters to 49,000 population. Antenatal clinic will be conducted every Tuesday and the average attendance in the antenatal clinic is 25-35. The study was conducted for six weeks during the months of September and October 2008. All women attending the antenatal clinic were included irrespective of the number of conceptions or the period of gestation. The subjects were contacted only once. After obtaining informed consent, a pretested questionnaire was administered by the investigator for collection of data.
The questionnaire was designed to collect information on background characteristics of age, education, occupation, and parity followed by 12 questions focusing on general awareness about DM and GDM, and risk factors, diagnosis, treatment, and consequences of GDM. The source of knowledge of antenatal women regarding GDM was also obtained.
The questions on risk factors assessed the awareness on prepregnancy obesity, family history of diabetes, diabetes during previous pregnancy, and rapid weight gain during current pregnancy. The options provided were yes, no, and don't know. When the mother answered ‘yes’ to the questions, it was considered as the right response.
Their knowledge on diagnosis of GDM was assessed by questions on time for testing and the test employed to detect it. The options provided for time for testing were 12-16 weeks, 18-22 weeks, 24-28 weeks, and during delivery. If the response was 12-16 weeks or 24-28 weeks, it was considered as the correct answer as during the conduct of the study, the debate regarding the appropriate time of testing was still on.[10] The options given for the test employed for GDM were urine test, blood test, or blood test following glucose load. If the woman responded as blood test following glucose load, it was considered as the right answer.
The knowledge on treatment of GDM was assessed by the questions with options as diet and exercise, oral antidiabetic drugs, and insulin injections. If the woman responded as diet and exercises or insulin injections, it was considered as the correct answer.
Their knowledge on course and consequences of GDM was assessed by questions on whether GDM usually disappeared after delivery, posed a risk to the unborn baby if untreated, and whether women diagnosed to have GDM were at an increased risk for future Type 2 diabetes. A ‘yes’ for each of these was considered as a correct response.
Each correct response was given a score of 1 and each woman was scored out of a total of 12. A score of 0-4 was considered as poor knowledge, 5-8 as fair, and 9-12 as good knowledge of GDM. Association between knowledge and age, educational status, and parity of the women was analyzed by test of proportions and the statistical significance was assessed using the Chi-square test.
RESULTS
One hundred and twenty antenatal women participated in the study. Most of them were housewives (90%). Mean age of the women was 23.8 years (SD: 2.94) and the range was 18-33. Majority of the women (63.3%) were in the 21-25 age group and 25.8% were above 25 years of age. With respect to education, 8.3% of the women were illiterates, 9.2% had primary education, 65% had secondary education, and 17.5%, higher education. Half (50%) of the women were primagravid.
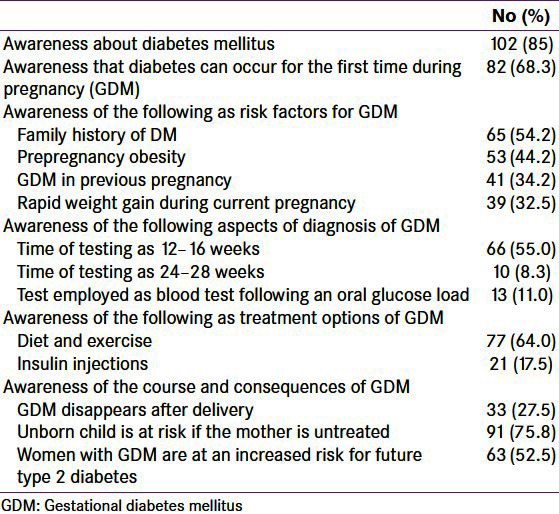
Overall, 17.5% women had good knowledge, 56.7% had fair knowledge, and 25.8% women had poor knowledge about GDM. The median knowledge score was 7. Age, education, and parity were not found to be significantly associated with the level of knowledge of women about GDM (data not shown in table). The awareness of the women on the various aspects of GDM is given in Table 1.
Table 1.
Awareness of antenatal women (n=120) on various aspects of gestational diabetes mellitus
The major sources of awareness of GDM were reported to be television/radio, neighbors/friends, and family members. Doctors, health-care workers, or hospital charts/boards were sources of information among a lesser proportion of women [Figure 1].
Figure 1.
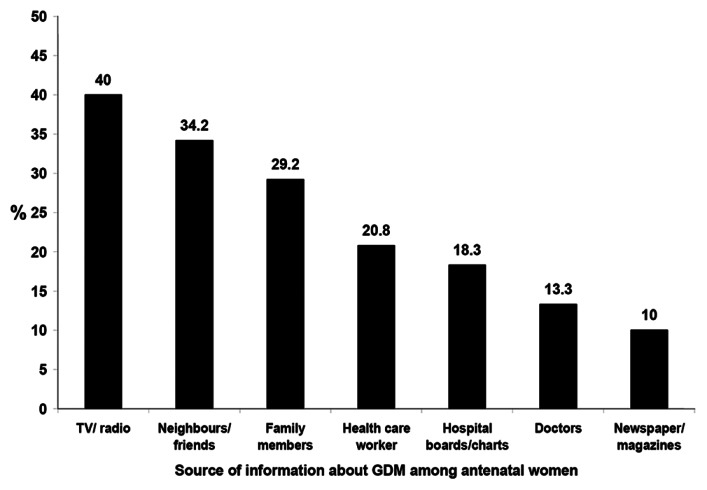
Source of information about gestational diabetes mellitus (GDM) among antenatal women (n = 120)
DISCUSSION
This study shows that only a small proportion of rural antenatal women (17.5%) had good knowledge about GDM. A greater proportion of the women were aware of the conditions of DM and GDM. Awareness about time of diagnosis of GDM, diet, and exercise as a treatment option for GDM, and about the probability of untreated GDM posing a risk to the unborn child was also high among the study women. However, knowledge about the risk factors for GDM and the course of GDM, and that the women diagnosed with GDM are at an increased risk for future Type 2 diabetes was low. For women to take proper precautions and self-care, it is important that they have a good knowledge about the risk factors and the consequences that they may face if they have untreated GDM.
Though it is encouraging to see the role played by mass media in creating awareness about the condition, it is of great concern that the health-care providers were quoted as a source of information by only a fifth of the women. The doctors have to educate the health-care workers and both the doctors and the health-care workers have to play a greater role in creating awareness among antenatal women. The topic of GDM should be included as a part of the routine health-care education programs organized for antenatal women.
The state government of Tamil Nadu has taken up universal screening for GDM by means of a single blood glucose test 2 hours post 75 g of glucose in all the three trimesters. This initiative was hailed as the first of its kind in the world at the conference on diabetes and pregnancy in Istanbul, Turkey in 2007.[11] Along with screening, more efforts are necessary at the program level to improve the awareness about risk factors, course, and effects of GDM on the woman, as a higher level of awareness will surely improve pregnancy outcomes.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Magon N. Gestational diabetes mellitus: Get, set, go from diabetes capital of the world to diabetes care capital of the world. Indian J Endocrinol Metab. 2011;15:161–9. doi: 10.4103/2230-8210.83398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Metzger BE, Coustan DR. Summary and recommendations of the fourth international workshop-conference on gestational diabetes mellitus.The Organizing Committee. Diabetes Care. 1998;21:B161–7. [PubMed] [Google Scholar]
- 3.Kjos SL, Buchanan TA. Gestational diabetes mellitus. N Engl J Med. 1999;341:1749–56. doi: 10.1056/NEJM199912023412307. [DOI] [PubMed] [Google Scholar]
- 4.Seshiah V, Balaji V, Balaji MS, Sanjeevi CB, Green A. Gestational diabetes mellitus in India. J Assoc Physicians India. 2004;52:707–11. [PubMed] [Google Scholar]
- 5.Chowdhury TA, Grace C, Kopelman PG. Preventing diabetes in south Asians. BMJ. 2003;327 (7423):1059–60. doi: 10.1136/bmj.327.7423.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Makgoba M, Savvidou MD, Steer PJ. An analysis of the interrelationship between maternal age, body mass index and racial origin in the development of gestational diabetes mellitus. BJOG. 2012;119:276–82. doi: 10.1111/j.1471-0528.2011.03156.x. [DOI] [PubMed] [Google Scholar]
- 7.Seshiah V, Balaji V, Balaji MS, Paneerselvam A, Arthi T, Thamizharasi M, et al. Prevalence of gestational diabetes mellitus in South India (Tamil Nadu)–A community based study. J Assoc Physicians India. 2008;56:329–33. [PubMed] [Google Scholar]
- 8.Afridi JB, Khan MJ, Iman NU. Diabetes in females: Knowledge, attitude and practices. J Med Sci. 2010;18:40–4. [Google Scholar]
- 9.Carolan M, Steele C, Margetts H. Knowledge of gestational diabetes among a multi-ethnic cohort in Australia. Midwifery. 2010;26:579–88. doi: 10.1016/j.midw.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 10.Seshiah V, Sahay BK, Das AK, Shah S, Banerjee S, Rao PV, et al. Gestational diabetes mellitus–Indian guidelines. [Last Accessed on 2010 Aug 27];J Indian Med Assoc. 2009 107:799–802. 804, 6. Available from: http://www.abcofobg.com/GDM_New/Gestational Diabetes Mellitus-Indian Guidelines.pdf . [PubMed] [Google Scholar]
- 11.Anantharaman A. Lifeline for mother and child. Spectrum The Tribune, Sunday, July 1. 2007. [Last Accessed on 2008 Oct 20]. Available from: http://www.tribuneindia.com/2007/20070701/spectrum/society.htm .


