Abstract
The natriuretic system consists of the atrial natriuretic peptide (ANP) and four other similar peptides including the wrongly named brain natriuretic peptide (BNP). Chemically they are small peptide hormones predominantly secreted by the cardiac myocytes in response to stretching forces. The peptide hormones have multiple renal, hemodynamic, and antiproliferative effects through three different kinds of natriuretic receptors. Clinical interest in these peptide hormones was initially stimulated by the use of these peptides as markers to differentiate cardiac versus noncardiac causes of breathlessness. Subsequently work has been done on using these peptides to prognosticate patients with acute and chronic heart failure and those with acute myocardial infraction. Synthetic forms of both atrial- and brain-natriuretic peptides have been studied and approved for use in acute heart failure with mixed results. This review focuses on the biochemistry and physiology of this fascinating hormone system and the clinical application of these hormones.
Keywords: Atrial natriuretic peptide, brain natriuretic peptide, heart failure, natriuretic peptides
INTRODUCTION
The fact that atrial extracts have potent natriuretic and vasodepressor activity was discovered by De Bold et al. in 1981.[1] Ever since the natriuretic system has been considered as a functionally important endocrine system of cardiovascular and renal origin. This lead to the discovery of atrial natriuretic peptide (ANP), and subsequently four other natriuretic peptides: Brain natriuretic peptide (BNP), C-type natriuretic peptide (CNP), dendroaspis natriuretic peptide (DNP), and urodilantin were discovered. Though these molecules are referred to as natriuretic peptides they perform a variety of physiological functions besides natriuresis including vasodilation, antiproliferative effects, vascular remodeling, and modulation of renin–angiotensin–aldosterone systems. The natriuretic system also consists of three receptors namely natriuretic peptide receptor-A (NPR-A or guanylyl cyclase-A), natriuretic receptor-B (NPR-B or guanylyl cyclase-B), and natriuretic peptide receptor-C (NPR-C or clearance receptor).
CHEMISTRY
ANP is a 28 amino acid peptide with a ringed structure formed by intramolecular disulfide linkages. It is synthesized and secreted by the cardiac atria.[1] The ANP gene in humans is located on the short arm of chromosome 1.[2] ANP is synthesized as a 151 amino acid preprohormone (preproANP) and is stored in atrial myocytes as a 126 amino acid prohormone (proANP). When secreted proANP is cleaved yielding N-ANP and the biologically active C-terminal hormone (ANP) in equimolar amounts.[3]
BNP is a 32 amino acid peptide, structurally similar to ANP with a 17 common amino acid sequence. It was first isolated from porcine brain extracts by Sudoh et al.[4] A single-copy gene consisting of 3 exon and 2 introns located on chromosome 1. BNP is stored as a mature hormone in the human heart while ANP is stored as proANP.[5] The cardiomyocytes synthesize a prepropeptide (preproBNP; 134 amino acids) which is split into a signal peptide and a propeptide (proBNP;108 amino acids). During secretion from the cardiomyocytes, proBNP is split at a ratio of 1:1 into the physiologically active BNP (32 amino acids) which corresponds to the C-terminal fragment, and the biologically inactive N-terminal fragment (NTproBNP; 76 amino acids).[6]
CNP, which was first isolated from porcine brain in 1990, consists of 22 amino acids.[7] The ring structure of CNP is highly homologous with ANP and BNP but uniquely lacks the carboxy-terminal extension. The structure of CNP is identical among species. PreproCNP, comprising 126 amino acids, after cleavage of the first 23 amino acids is converted to proCNP, which is further processed to CNP-53 and/or CNP the potencies of which are essentially the same.[8]
DNP was first isolated from the venom of the green mamba snake, Dendroaspis angusticeps.[9] The 38 amino acid natriuretic peptide which contains a 17 amino acid disulfide ring similar to ANP, BNP, and CNP with a 15-residue carboxy terminal extension.
Urodilantin is a nonglycosylated 32 amino acid natriuretic peptide was isolated from human urine.[10] The amino acid sequence of urodilantin is identical to that of ANP except for the presence of 4 additional amino acids in the amino terminal.[11]
Tissue distribution
ANP gene expression is highest in the normal adult atria and much lower in ventricles. The atrium is the major site of ANP synthesis; however, ventricular ANP expression is increased markedly in the failing and hypertrophied heart.[12]
BNP was initially isolated from the brains of pigs and dogs.[4,13] Its name is however a misnomer as the highest expression level of BNP is in the ventricular myocardium. BNP mRNA has also been found in extra cardiac tissues including human brain, bovine adrenal medulla, and human amnion cells.
CNP is distributed throughout the brain in rats and humans and its concentration is 10-fold higher than ANP and BNP in cerebrospinal fluid. CNP is also detectable in the endothelium, kidney adrenal glands, heart, bowel, thymus, uterus, and testes.[14–19]
DNP like immnuoreactivity has been detected in canine and human plasma and human myocardium.[20]
Natriuretic peptide receptors
There are three different subtypes of natriuretic peptide receptors (NPRs), NPR-A, NPR-B, and NPR-C which have been localized to three human chromosomes. The designation however does not correspond to relative affinities for ANP, CNP, and BNP.[21] The biological actions of the hormones are mediated by NPR-A and NPR-B, whereas NPR-C mainly acts like a clearance receptor.[22] The NPRs are transmembrane proteins which belong to the receptor guanylyl cyclase family, found in target tissues of the natriuretic peptides.[23] ANP, BNP, and urodilantin selectively activate NPR-A. ANP has greater affinity for NPR-A than BNP and CNP.[24] CNP binds more selectively with NPR-B.
ANP, BNP, and CNP all bind to the NPR-C receptor which functions mainly as a clearance receptor. NPR-C acts through internalization and lysosomal hydrolysis of the natriuretic peptide receptor complex. The number and distribution of NPRs vary widely. NPR-A is mainly expressed in heart lungs, kidney, adrenal glands adipose tissue, eye, and pregnant uterus.[25,26] NPR-B has a similar distribution as NPR-A, but has a lower density to the kidney and a higher density to the brain. NPR-C is the most abundant NPR and its presence has been demonstrated in heart, kidney, brain, endothelium, smooth muscle cells, and adrenal glands.[22,27]
Regulation of natriuretic peptide secretion
ANP and BNP are continuously released from the heart but their synthesis and secretion is regulated by a number of factors. Atrial stretch is the principal stimulus for increase in ANP release from atrial cardiomyocytes. The main stimulus for BNP release appears to be ventricular stretch and increased levels of BNP have been found in patients with increased left ventricular end diastolic pressure, pulmonary artery pressure, and pulmonary artery wedge pressure.[28,29] The transcription of the CNP gene is regulated by many factors like tumor necrosis factor (TNF) and interleukin-1. Blood levels of CNP are elevated in conditions characterized by endothelial damage like sepsis, hypoxia, and chronic renal failure.[30]
Physiologic actions
Renal effects
ANP causes intravascular volume contraction resulting in decreased preload and blood pressure.[31] In low doses, it causes natriuresis but no change in blood pressure.[32]
BNP, like ANP, is natriuretic in both humans and animals.
Hemodynamic effects
Sustained low dose infusion of ANP reduces peripheral vascular resistance and blood pressure whereas higher doses decrease the blood pressure which is accompanied by a rise in the peripheral vascular resistance, which is probably due to activation counter regulatory hormones. BNP causes no significant change in blood pressure or heart rate when administered to hypertensive or normotensive human subjects in doses sufficient to raise plasma concentrations to levels comparable to those seen in heart failure.[33] When administered in higher doses, it causes a decrease in systemic vascular resistance and blood pressure, rise in cardiac index, and reduction in the pulmonary capillary wedge pressure.[34] CNP induces vascular relaxation and inhibits growth of vascular smooth muscle cells and has powerful venodilator effects.[35–37]
Antiproliferative effect
ANP has been shown to be antimitogenic in endothelial and vascular smooth muscle cells and attenuates the growth response to adrenergic stimuli.[36,38] CNP exerts a growth inhibitory action and antagonizes the growth promoting action of angiotensin II.[39]
Modulation of sympathetic nervous system activity
ANP reduces sympathetic tone by dampening of baroreceptors, suppressing the release of catecholamines from autonomic nerve endings and suppressing sympathetic outflow from the CNS. The effects of ANP on the CNS also contribute to fluid and electrolyte balance and hemodynamic regulation. CNP was initially considered to act principally as a neuropeptide and plays a role in prejunctional inhibition of norepinephrine release.[40]
Effects on the renin-angiotensin-aldosterone system
Secretion of renin or aldosterone are markedly inhibited following ANP infusion,[41] while BNP causes a fall or no change in plasma rennin activity.[34] ANP, but not BNP, inhibits the plasma aldosterone response to angiotensin II.[42] Infusion of small doses and BNP inhibits the renin-angiotensin-aldosterone system (RAAS) while CNP does not, unless administered in very high doses.
CLINICAL SIGNIFICANCE OF NATRIURETIC PEPTIDES
Diagnostic uses
Natriuretic peptides have been found to be useful markers in differentiating patients presenting with acute onset of breathlessness and also as prognostic markers in patients with congestive cardiac failure. Plasma levels of ANP and BNP are increased in variety of conditions like heart failure, acute myocardial infarction, hypertension, left ventricular hypertrophy, and pulmonary hypertension.
Heart failure
BNP is a hormone that is secreted mainly by the ventricles and its levels are markedly high in patients with acute and congestive heart failure. Distention and stretching of the left ventricular wall leads to increased synthesis of BNP which produces natriuresis and vasodilatation along with an inhibitory effect on the RAAS and adrenergic system.[43,44] BNP plasma levels are also elevated in patients with acute myocardial infarction and left ventricular dysfunction and this increase persists during the late phase of cardiac remodeling.[45] Determining plasma BNP concentration is an effective diagnostic tool in patients presenting with acute dyspnea. Studies have demonstrated that patients diagnosed with dyspnea secondary to heart failure have significantly elevated plasma BNP concentration compared to noncardiogenic dyspnea (due to respiratory disease).[46,47] BNP values have been found to be directly correlating with NYHA functional class.[48] BNP analysis has also been shown to have a superior diagnostic accuracy in heart failure compared to other parameters like high venous pressure recruitment, increase of LV dimension and interstitial edema detected using chest x-ray. Hence BNP is not only a good marker for the diagnosis of heart failure but is also an excellent indicator of its severity. In patients who present with acute dyspnea, BNP testing is recommended according to prescribed algorithms providing much information to physicians in clinical practice [Figure 1].[49]
Figure 1.
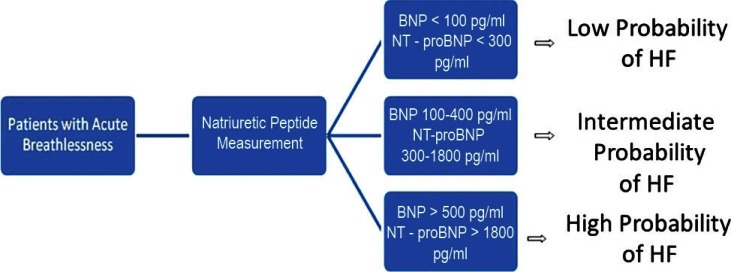
Decisional algorithm for HF (heart failure) diagnosis on the basis of BNP and NT-proBNP measurement
Natriuretic peptide measurements are also important for risk stratification as high levels are associated with recurrent hospitalization and risk of sudden death.[50] Predischarge BNP measurement is a significant predictor for identifying subsequent death or hospital admissions at 6 months.[51,52] Morbidity and mortality in heart failure appear to increase markedly with a proBNP concentration >500 pg/ml. Baseline BNP and proBNP have been found to be similarly related to both mortality and risk of admission with decompensated heart failure independent of echocardiographic variables.[53] For the above reasons BNP analysis has been proposed for the clinical evaluation and therapy guidance of heart failure.[54]
Even in patients with heart failure who have a preserved systolic function proBNP values have been found to have a strong prognostic significance.[55]
Acute coronary syndromes
Plasma ANP levels rise by the time patients with acute myocardial infarction are hospitalized. Plasma BNP levels usually peak 12–24 hours after the onset of infarction, then decline and peak once again 5–7 days later.[56] BNP levels remain significantly elevated during the chronic phase, representing permanent left ventricular dysfunction and/or remodeling but return to normal in patients after successful early coronary reperfusion.[57] In patients with acute coronary syndromes (ACS), BNP is a strong indicator of heart failure.[58] and BNP levels have been significantly found to be higher in patients with multivessel than in those with single-vessel disease.[59]
Hypertension and left ventricular hypertrophy
Several studies have shown that plasma ANP and BNP levels are higher in hypertensive than in normotensive individuals and are higher in hypertensive patients with ventricular hypertrophy (LVH) than in those without LVH.[60]
Cardiac amyloidosis
Limited data show BNP measurement to be important in cardiac amyloidosis, which is a disorder characterized by diastolic dysfunction, and levels are quite elevated in patients with overt heart failure and cardiac amyloidosis.[61]
Restrictive cardiomyopathy and constrictive pericarditis
These two nearly indistinguishable entities pose quite a diagnostic challenge. BNP levels have been found to be markedly elevated in patients with restrictive cardiomyopathy (RCM) presenting in NYHA class 3 or 4 heart failure while clinically similar patients of constrictive pericarditis (CP) have much lower BNP levels.[62] Hence BNP could serve as a useful mechanism to differentiate between these two diseases which have a very similar clinical presentation but whose treatment varies completely.
Atrial fibrillation
Atrial fibrillation (AF) is common comorbidity in patients with heart failure but BNP levels have also been found to be elevated in heart patients with chronic AF.[63] However this finding has not been found to have much clinical significance.
Valvular heart disease
Natriuretic peptide levels increase with increasing severity of mitral regurgitation (MR) and have been shown to be a marker of poor outcome in patients with organic MR.[64] Positive correlations have been found between BNP levels with severity of mitral stenosis, rise in pulmonary artery pressures and a negative correlation with mitral area.[65] BNP levels are also elevated in patients with aortic regurgitation and aortic stenosis and are linearly related to symptoms.[66]
Cardiac inflammatory and infectious diseases
Release of BNP into the circulation may be a feature of cardiac inflammation. BNP levels have been found to be high in patients with perimyocarditis, infective endocarditis, acute rheumatic fever, and Kawasaki disease.[67–69]
Cardiogenic syncope
High NTproBNP levels have been found in patients with cardiac syncope with high sensitivity and may be helpful in differentiating cardiac from noncardiac syncope.[70]
Sleep apnea and morbid obesity
Elevated BNP levels reflect an increased likelihood of LVH in patients with severe sleep apnea.[71] NTproBNP levels are independently predicted by sleep disordered breathing and insulin resistance according to a cross-sectional study involving 110 morbidly obese healthy young female patients.[72]
Brain natriuretic peptide and pulmonary diseases
Chronic lung disease and respiratory failure: Elevated BNP levels have been found in hypoxemic patients with chronic obstructive pulmonary disease (COPD), particularly in patients with cor pulmonale when compared with patients with COPD alone. BNP levels increase in proportion to the severity of RV dysfunction.[73] While BNP levels are apparently elevated in those with COPD, the levels are not nearly elevated to the degree seen in heart failure.[74]
Pulmonary embolism (PE): Natriuretic peptides are elevated in most patients with acute PE complicated with RV overload or dysfunction. Decline in BNP levels has been shown to be an indicator of efficacy of pharmacological treatment in patients with acute PE.[75]
Pulmonary hypertension: In patients with RV pressure overload due to primary pulmonary hypertension and thromboembolism, plasma BNP levels have been found to be correlated with mean pulmonary pressure and total pulmonary resistance.[76]
Natriuretic peptides and infectious diseases/sepsis
Ventricular dysfunction with reduced ejection fraction and biventricular dilatation is a common finding in a patient with severe sepsis. Plasma ANP, NTproBNP, and BNP levels are significantly elevated in septic shock patients compared to healthy shock subjects. BNP and NTproBNP have prognostic value in the setting of sepsis in the ICU.[77] However; their role in establishing underlying cardiac dysfunction is questionable.
Cirrhosis of the liver
In patients with liver cirrhosis, elevated BNP, and proBNP levels reflect increased cardiac ventricular synthesis of natriuretic peptides thereby indicating the presence of cardiac dysfunction. Hyperdynamic systemic circulation could also be responsible for elevated BNP levels in such patients.[78]
Hyperthyroidism
Serum NTproBNP levels are affected by thyroid functions because of a direct stimulatory effect of thyroid hormones. Multiple linear regression analysis has demonstrated the free T4 and free T3 were independently associated with a high NTproBNP. Patients with hyperthyroidism have been found to have higher NTproBNP and BNP levels compared to hypothyroid patients and normal controls and treatment of thyroid dysfunction could result in their normalization.[79]
Intracranial pathologies
Acute ischemic stroke (AIS): Activation of hypothalamus-pituitary-adrenal axis in patients with AIS is associated with elevated levels of natriuretic peptides which in turn predict long-term mortality after AIS.[80]
Subarachnoid hemorrhage (SAH): Elevated BNP levels along with increased diuresis and natriuresis have been found in patients with SAH.[81] In patients with traumatic SAH, early after SAH, elevated BNP levels are associated with LV dysfunction and pulmonary edema.
Therapeutic uses
Natriuretic peptides have been shown to have therapeutic potential for various pathological conditions. Synthetic forms of both ANP and BNP have been approved in some countries for the treatment of heart failure.[82]
Synthetic atrial natriuretic peptide (anaritide and carperitide)
Anaritide, also called ANF 1V, is a 25 amino acid peptide lacking the first three amino terminal residues of the 28 amino acid mature form of ANP. ANP improves cardiac function by altering loading conditions for the left ventricle and ANP infusion has been shown to significantly decrease pulmonary capillary wedge pressure and systemic vascular resistance.[83] In Japan a synthetic full-length ANP (carperitide) has been approved for the treatment of acute decompensated heart failure in 1995. ANP treatment has also been shown to act as an effective adjunctive therapy in patients with acute MI.[84] Anaritide has been investigated for its ability to prevent radio-contrast-induced nephropathy with conflicting results.[85,86]
Synthetic brain natriuretic peptide (nesiritide)
Nesiritide has been approved for the treatment of acute decompensated heart failure in the United States since 2001. Twenty-hour infusion of Nesiritide in patients with congestive heart failure has been shown to have both preload and after load reducing actions resulting in an increase in stroke volume.[87] However in a recent trial involving nearly 7000 patients Nesiritide was shown not to be associated with an increase or decrease in the rate of death and rehospitalization and had a nonsignificant effect on dyspnea. There was also an increase in the rates of hypotension but there was no association with worsening renal failure. On the basis of this trial, Nesiritide cannot be recommended for routine use in the broad population of patients with acute heart failure.[88]
INDIAN PERSPECTIVE
A recent study done in India compared BNP levels with transmitral Doppler flow velocities as a marker of diastolic dysfunction, and systolic parameters pre-and post-pericardiectomy in patients of CP. There was a significant decrease in the mean values of BNP post-pericardiectomy in these patients suggesting that BNP can be used as a marker of left ventricular diastolic dysfunction in place of conventional transmitral Doppler studies. This however requires further research for validation of the same.[89]
CONCLUSION
Elevated natriuretic peptides have shown predictive value in various diseases that have direct or indirect influences on cardiac function. BNP and NTproBNP testing have a clear and a valuable role in the diagnosis of heart failure in patients presenting to the emergency with dyspnea. The strength of BNP testing is in its ability to rule out heart failure in this setting. In patients with heart failure, natriuretic peptide has a strong correlation with its severity. In patients of heart failure in ACS with or without ST elevation natriuretic peptides appear to predict severity of coronary disease and ischemic area extension. Potential clinical applications of natriuretic peptides have expanded but currently the only reasonable clinical use for routine practice is limited to differentiation of acute dyspnea, monitoring of therapeutic responses, and determining prognosis of acute or decompensated heart failure.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.De Bold AL, Borenstein HB, Veress AT, Sonnenberg H. A rapid and potent natriuretic response to intravenous injection of atrial myocardial extract in rats. Life Sci. 1981;28:89–94. doi: 10.1016/0024-3205(81)90370-2. [DOI] [PubMed] [Google Scholar]
- 2.Yandle TG. Biochemistry of natriuretic peptides. J Intern Med. 1994;235:561–76. doi: 10.1111/j.1365-2796.1994.tb01263.x. [DOI] [PubMed] [Google Scholar]
- 3.Mathisen P, Hall C, Simonsen S. Comparative study of atrial peptides ANF (1-98) and ANF(99-126) as diagnostic markers of atrial distention in patients with cardiac disease. Scand J Clin Lab Invest. 1993;53:41–9. doi: 10.1080/00365519309092530. [DOI] [PubMed] [Google Scholar]
- 4.Sudoh T, Kangawa K, Minamino N, Matsuo H. A new natriuretic peptide in porcine brain. Nature. 1988;332:78–81. doi: 10.1038/332078a0. [DOI] [PubMed] [Google Scholar]
- 5.Minamino N, Horio H, Nishikimi T. Natriuretic peptides in the cardiovascular system. In: Kastin AJ, editor. The handbook of biologically active peptides. 1st ed. New York/London: Academy Press; 2006. pp. 1217–25. [Google Scholar]
- 6.Levin ER, Gardner DG, Samson WK. Natriuretic peptides. N Engl J Med. 1998;339:321–8. doi: 10.1056/NEJM199807303390507. [DOI] [PubMed] [Google Scholar]
- 7.Sudoh T, Maekawa K, Kojima M, Minamino N, Kangawa K, Matsuo H. Cloning and sequence analysis of cDNA encoding a precursor for human brain natriuretic peptide. Biochem Biophys Res Commun. 1989;159:1427–34. doi: 10.1016/0006-291x(89)92269-9. [DOI] [PubMed] [Google Scholar]
- 8.Minamino N, Makino Y, Tateyama H, Kangawa K, Matsuo H. Characterization of immunoreactive human C-type natriuretic peptide in brain and heart. Biochem Biophys Res Commun. 1991;179:535–42. doi: 10.1016/0006-291x(91)91404-z. [DOI] [PubMed] [Google Scholar]
- 9.Schweitz H, Vigne P, Moinier D, Frelin C, Lazdunski M. A new member of the natriuretic peptide family is present in the venom of the Green Mamba (Dendroaspis angusticeps) J Biol Chem. 1992;267:13928–32. [PubMed] [Google Scholar]
- 10.Schulz-Knappe P, Forssmann K, Herbert F, Hock D, Pipkorn R, Forssmann WG. Isolation and structural analysis of “urodilantin,” a new peptide of the cardiodilantin-(ANP)-family, extracted from human urine. Klin Wochenschr. 1988;66:752–9. doi: 10.1007/BF01726570. [DOI] [PubMed] [Google Scholar]
- 11.Forssmann WG, Richter R, Meyer M. the endocrine heart and natriuretic peptides: Histochemistry, cell biology, and functional aspects of the renal urodilantin system. Histochem Cell Biol. 1998;110:335–57. doi: 10.1007/s004180050295. [DOI] [PubMed] [Google Scholar]
- 12.Ogawa Y, Itoh H, Nakao K. Molecular biology and biochemistry of natriuretic peptide family. Clin Exp pharmacol Physiol. 1995;22:49–53. doi: 10.1111/j.1440-1681.1995.tb01918.x. [DOI] [PubMed] [Google Scholar]
- 13.Itoh H, Nakao K, Saito Y, Yamada T, Shirakami G, Mukoyama M, et al. Radioimmnuoasssay for brain natriuretic peptide (BNP) detectioin of BNP in canine brain. Biochem Biophys Res Commun. 1989;158:120–8. doi: 10.1016/s0006-291x(89)80186-x. [DOI] [PubMed] [Google Scholar]
- 14.Chen HH, Burnett JC., Jr C-type natriuretic peptide: The endothelial component of the natriuretic peptide system. J Cardiovasc Pharmacol. 1998;32:S22–8. [PubMed] [Google Scholar]
- 15.Mattingly MT, Brandt RR, Heubin DM, Wei CM, Nir A, Burnett JC., Jr Presence of C-type natriuretic peptide in human kidney and urine. Kidney Int. 1994;46:744–7. doi: 10.1038/ki.1994.329. [DOI] [PubMed] [Google Scholar]
- 16.Stingo AJ, Clavell AL, Heublin DM, Wei CM, Pittelkow MR, Burnett JC., Jr Presence of C-type natriuretic peptide incultured human endothelial cells and plasma. Am J Physiol. 1992;263:H1318–21. doi: 10.1152/ajpheart.1992.263.4.H1318. [DOI] [PubMed] [Google Scholar]
- 17.Vollmar AM, Wolf R, Schulz R. Coexpression of the natriuretic peptides (ANP, BNP, CNP) and their receptors in normal and acutely involved rat thymus. J Neuroimmunol. 1995;57:117–27. doi: 10.1016/0165-5728(94)00171-j. [DOI] [PubMed] [Google Scholar]
- 18.Stepan H, Faber R, Stegemann S, Schultheiss HP, Walther T. Expression of C-type natriurtic peptide in human placenta and myometrium in normal pregnancies and pregnancies complicated by intrauterine growth retardation. Preliminary results. Fetal Diagn Ther. 2002;17:37–41. doi: 10.1159/000048004. [DOI] [PubMed] [Google Scholar]
- 19.Middendorff R, Muller D, Paust HJ, Davidoff MF, Mukhopadhyay AK. Natriuretic peptides in the human testis: Evidence for a potential role of C-type natriurtic peptide in Leydig cells. J Clin Endocrinol Metab. 1996;81:4324–8. doi: 10.1210/jcem.81.12.8954035. [DOI] [PubMed] [Google Scholar]
- 20.Schirger JA, Heusblin DM, Chen HH, Lisy O, Jougasaki M, Wennverg PW, et al. Presence of Dendroaspis natriuretic peptide - like immunoreactivity in human plasma and its increase during human heart failure. Mayo Clin Proc. 1999;74:126–30. doi: 10.4065/74.2.126. [DOI] [PubMed] [Google Scholar]
- 21.Lowe DG, Klisak I, Sparkles RS, Mohandas T, Goeddel DV. Chromosomal distribution of the members of the human natriuretic peptide receptor/guanylyl cyclase family. Genomics. 1990;8:304–12. doi: 10.1016/0888-7543(90)90286-4. [DOI] [PubMed] [Google Scholar]
- 22.Maack T, Okolicany J, Koh GY, Price DA. Functional properties of atrial natriuretic factor receptors. Semin Nephrol. 1993;13:50–60. [PubMed] [Google Scholar]
- 23.Koller KJ, Goeddel DV. Molecular biology of the natriuretic peptides and their receptors. Circulation. 1992;86:1081–8. doi: 10.1161/01.cir.86.4.1081. [DOI] [PubMed] [Google Scholar]
- 24.Suga S, Nakao K, Hosoda K, Mukoyama M, Ogawa Y, Shirakami G, et al. Receptor selectivity of natriuretic peptide family, atrial natriretic peptide, brain natriuretc peptide and C-type natriuretic peptide. Endocrinology. 1992;130:229–339. doi: 10.1210/endo.130.1.1309330. [DOI] [PubMed] [Google Scholar]
- 25.Itoh H, Sagawa N, Hasegawa M, Nanno H, Kobayashi F, Ihara Y, et al. Expression of biologically active receptors for natriuretic peptide in human uterus during pregnancy. Biochem Biophys Res Commun. 1994;203:602–7. doi: 10.1006/bbrc.1994.2225. [DOI] [PubMed] [Google Scholar]
- 26.Nakao K, Ogawa Y, Suga S, Imura H. Molecular biology and biochemistry of the natriuretic peptide system. II: Natriuretic peptide receptors. J Hypertens. 1992;10:1111–4. doi: 10.1097/00004872-199210000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Espiner EA, Richards AM, Yandle TG, Nicholls MG. Natriuretic hormones. Endocrinol Metab Clin North Am. 1995;24:481–509. [PubMed] [Google Scholar]
- 28.Richards AM, Crozier IG, Espiner EA, Yandle TG, Nicholls MG. Plasma brain natriuretic peptide and endopeptidase 24.11 inhibition in hypertension. Hypertension. 1993;22:231–6. doi: 10.1161/01.hyp.22.2.231. [DOI] [PubMed] [Google Scholar]
- 29.Kohno M, Horio T, Yokokawa K, Akioka K, Ikeda M, Takeda T. Pulmonary arterial brain natriuretic peptide concentration and cardiopulmonary hemodynamics during exercise in patients with essential hypertension. Metabolism. 1992;41:1273–5. doi: 10.1016/0026-0495(92)90095-r. [DOI] [PubMed] [Google Scholar]
- 30.Hama N, Itoh H, Shirakami G, Suga S, Komatsu Y, Yoshimasa T, et al. Detection of C-type natriuretic peptide in human circulation and marked increase of plasma CNP level in septic shock patients. Biochem Biophys Res Commun. 1994;198:1177–82. doi: 10.1006/bbrc.1994.1166. [DOI] [PubMed] [Google Scholar]
- 31.Charles CJ, Espiner EA, Richards AM. Cardiovascular actions of ANF: Contributions of renal, neurohumoral, and hemodynamic factors in sheep. Am J Physiol. 1993;264:R533–8. doi: 10.1152/ajpregu.1993.264.3.R533. [DOI] [PubMed] [Google Scholar]
- 32.Richards AM, Crozier IG. Physiological role of atrial natri-uretic peptide. Int J Cardiol. 1989;25:141–3. doi: 10.1016/0167-5273(89)90178-2. [DOI] [PubMed] [Google Scholar]
- 33.Stephenson SL, Kenny AJ. The hydrolysis of alpha-human atrial peptide by pig kidney microvillar membranes is initiated by endopeptidases-24.11. Biochem J. 1987;243:183–7. doi: 10.1042/bj2430183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoshimura M, Yasue H, Morita E, Sakaino N, Jouqasaki M, Mukoyama S, et al. Hemodynamic, renal, and hormonal responses to brain natriuretic peptide infusion in patients with congestive heart failure. Circulation. 1999;84:1581–8. doi: 10.1161/01.cir.84.4.1581. [DOI] [PubMed] [Google Scholar]
- 35.Drewett JG, Fendly BM, Garbers DL, Lowe DG. Natriuretic peptide receptor-B (guanylyl cyclase-B) mediates C-type natriuretic peptide relaxation of of recontracted rat aorta. J Biol Chem. 1995;270:4668–4674. doi: 10.1074/jbc.270.9.4668. [DOI] [PubMed] [Google Scholar]
- 36.Itoh H, Pratt RE, Dzau VJ. Atrial natriuretic polypeptide inhibits hypertrophy of vascular smooth muscle cells. J Clin Invest. 1990;86:1690–7. doi: 10.1172/JCI114893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Doi K, Itoh H, Ikeda T, Hosada K, Oqawa Y, Iqaki T, et al. Adenovirus-mediated gene transfer of C-type natriureticc peptide causes G1 growth inhibition of cultured vascular smooth cells. Biochem Biophys Res. 1997;239:889–94. doi: 10.1006/bbrc.1997.7576. [DOI] [PubMed] [Google Scholar]
- 38.Horio T, Nishikimi T, Yoshihara F, Matsuo H, Takishita S, Kanqawa K. Inhibitory regulation of hypertrophy of endogenous atrial natriuretic peptide in cultured cardiac myocytes. Hypertension. 2000;35:19–24. doi: 10.1161/01.hyp.35.1.19. [DOI] [PubMed] [Google Scholar]
- 39.Itoh H, Nakao K. Antagonism between the vascular renin-angiotensin and natriuretic peptide systems in vascular remodelling. Blood Press Suppl. 1994;5:49–53. [PubMed] [Google Scholar]
- 40.Trachte GJ, Drewett JG. C-type natriuretic peptide neuromodulates independently of guanylyl cyclase activation. Hypertension. 1994;23:38–43. doi: 10.1161/01.hyp.23.1.38. [DOI] [PubMed] [Google Scholar]
- 41.Burnett JC, Jr, Granger JP, Opgenorth TJ. Effects of synthetic atrial natriuretic factor on renal function and renin release. Am J Physiol. 1984;247:F863–6. doi: 10.1152/ajprenal.1984.247.5.F863. [DOI] [PubMed] [Google Scholar]
- 42.Hunt PJ, Espiner EA, Nicholls MG, Richards AM, Yandle TG. Differing biological effects of equimolar atrial and brain natriuretic peptide infusions in normal man. J Clin Endocrinol Metab. 1996;81:3871–6. doi: 10.1210/jcem.81.11.8923831. [DOI] [PubMed] [Google Scholar]
- 43.Kannel WB. Incidence and epidemiology of heart failure. Heart Fail Rev. 2000;5:167–73. doi: 10.1023/A:1009884820941. [DOI] [PubMed] [Google Scholar]
- 44.Cheung BM, Kumana CR. Natriur etic peptides- relevance in cardiac disease. JAMA. 1998;280:1983–4. doi: 10.1001/jama.280.23.1983. [DOI] [PubMed] [Google Scholar]
- 45.Hirayama A, Kusuoka H, Yamamoto H, Sakata Y, Asakura M, Higuchi Y, et al. Serial changes in plasma brain natriuretic peptide concentration at the infarct and non-infarct sites in patients with left ventricular remodeling after myocardial infarction. Heart. 2005;91:1573–7. doi: 10.1136/hrt.2004.049635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dao Q, Krishnaswamy P, Kazanegra R, Harrison A, Amirnovin R, Lenert L, et al. Utility of B-type natriuretic peptide in the diagnosis of congestive heart failure in an urgent care setting. J Am Coll Cardiol. 2001;37:379–85. doi: 10.1016/s0735-1097(00)01156-6. [DOI] [PubMed] [Google Scholar]
- 47.Morrison LK, Harrison A, Krishnaswamy P, Kazanegra R, Clopton P, Maisel A. utilty of a rapid B-natriuretic peptide assay in differentiating congestive heart failure from lung disease in patients presenting with dyspnoea. J Am Coll Cardiol. 2001;39:202–9. doi: 10.1016/s0735-1097(01)01744-2. [DOI] [PubMed] [Google Scholar]
- 48.Maisel AS, Krishnaswamy P, Nowak RM, Mccord J, Hollander J, Duc P, et al. Breathing Not Properly Multinational Study Investigators: Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347:161–7. doi: 10.1056/NEJMoa020233. [DOI] [PubMed] [Google Scholar]
- 49.Baggish A, Cameron R, Anwaruddin S, Chen AA, Krauser DG, Tunq R, et al. A clinical and biochemical critical pathway for the evaluation of patients with suspected acute congestive heart failure: The ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE) algorithm. Crit Pathways Cardiol. 2004;3:171–6. doi: 10.1097/01.hpc.0000145817.68289.a2. [DOI] [PubMed] [Google Scholar]
- 50.Harrison A, Morrison LK, Krishnaswamy P, Kazaneqra R, Clopton P, Dao Q, et al. B-type natriuretic peptide predicts future cardiac events in patients presenting to the emergency departement with dyspnea. Ann Emerg Med. 2002;39:131–8. doi: 10.1067/mem.2002.121483. [DOI] [PubMed] [Google Scholar]
- 51.Bettencourt P, Azevedo A, Pimenta J, Friões F, Ferreira S, Ferreira A. N-terminal-probrain natriuretic peptide predicts outcome after hospital discharge in heart failure patients. Circulation. 2004;110:2168–74. doi: 10.1161/01.CIR.0000144310.04433.BE. [DOI] [PubMed] [Google Scholar]
- 52.Aspromonte N, Valle R, Peacock WF, Vanderheyden M, Maisel A. Inpatient monitoring and prognostic importance of B-type natriuretic peptide. Congest Heart Fail. 2008;14:30–4. doi: 10.1111/j.1751-7133.2008.tb00008.x. [DOI] [PubMed] [Google Scholar]
- 53.Masson S, Latini R, Anand IS, Vago T, Angelici L, Barlera S, et al. Direct comparison of B-type natriuretic peptide (BNP) and amino-terminal proBNP in a large population of patients with chronic and symptomatic heart failure: The Valsartan Heart Failure (Val-HeFT) data. Clin Chem. 2006;52:1528–38. doi: 10.1373/clinchem.2006.069575. [DOI] [PubMed] [Google Scholar]
- 54.Faggiano P, Valle R, Aspromonte N, D'Aloia A, Di Tano G, Barro S, et al. How often we need to measure brain natriuretic peptide (BNP) blood levels in patients admitted to the hospital for acute severe heart failure. Role of serial measurements to improve short-term prognostic stratification? Int J Cardiol. 2010;140:88–94. doi: 10.1016/j.ijcard.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 55.Bettencourt P, Azevedo A, Fonseca L, Araújo JP, Ferreira S, Almeida R, et al. Prognosis of decompensated heart failure patients with preserved systolic function is predicted by NT-proBNP variations during hospitalization. Int J Cardiol. 2007;117:75–9. doi: 10.1016/j.ijcard.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 56.Morita E, Yasue H, Yoshimura M, Ogawa H, Jougasaki M, Matsumura T, et al. Increased plasma levels of brain natriuretic peptide in patients with acute myocardial infarction. Circulation. 1993;88:82–91. doi: 10.1161/01.cir.88.1.82. [DOI] [PubMed] [Google Scholar]
- 57.Nagaya N, Goto Y, Nishikimi T, Uematsu M, Miyao Y, Kobayashi Y, et al. Sustained elevation of plasma brain natriuretic peptide levels associated with progressive ventricular remodelling after acute myocardial infarction. Clin Sci (Lond) 1999;96:129–36. [PubMed] [Google Scholar]
- 58.Sinclair H, Paterson M, Walker S, Beckett G, Fox KA. Predicting outcome in patients with acute coronary syndrome: Evaluation of B-type natriuretic peptide and the global registry of acute coronary events (GRACE) risk score. Scott Med J. 2007;52:8–13. doi: 10.1258/rsmsmj.52.3.8. [DOI] [PubMed] [Google Scholar]
- 59.Palazzuoli A, Rizzello V, Calabrò A, Gallotta M, Martini G, Quatrini I, et al. Osteoprotegerin and B-type natriuretic peptide in non-ST elevation acute coronary syndromes: Relation to coronary artery narrowing and plaques number. Clin Chim Acta. 2008;391:74–9. doi: 10.1016/j.cca.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 60.Yamamoto K, Burnett JC, Jr, Jougasaki M, Nishimura RA, Bailey KR, Saito Y, et al. Superiority of brain natriuretic peptide as a hormonal marker of ventricular systolic and diastolic dysfunction and ventricular hypertrophy. Hypertension. 1996;28:988–94. doi: 10.1161/01.hyp.28.6.988. [DOI] [PubMed] [Google Scholar]
- 61.Palladini G, Campana C, Klersy C, Balduini A, Vadacca G, Perfetti V, et al. Serum N- terminal pro-brain natriuretic peptide is a sensitive marker of myocardial dysfunction in AL amyloidosis. Circulation. 2003;107:2440–5. doi: 10.1161/01.CIR.0000068314.02595.B2. [DOI] [PubMed] [Google Scholar]
- 62.Leya F, Arab D, Joyal D, Shioura KM, Lewis BE, Steen LH, et al. The efficacy of brain natriuretic peptide levels in differentiating constrictive pericarditis from restrictive cardiomyopathy. J Am Coll Cardiol. 2005;45:1900–2. doi: 10.1016/j.jacc.2005.03.050. [DOI] [PubMed] [Google Scholar]
- 63.Silvet H, Young-Xu Y, Walleigh D, Ravid S. Brain natriuretic peptide is elevated in outpatients with atrial fibrillation. Am J Cardiol. 2003;92:1124–7. doi: 10.1016/j.amjcard.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 64.Moe GW, Howlett J, Januzzi JL, Zowall H. Canadian Multicenter Improved Management of Patients With Congestive Heart Failure (IMPROVE-CHF) Study Investigators. N-terminal pro- B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: Primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation. 2007;115:3103–10. doi: 10.1161/CIRCULATIONAHA.106.666255. [DOI] [PubMed] [Google Scholar]
- 65.Iltumur K, Karabulut A, Yokus B, Yavuzkir M, Taskesen T, Toprak N. N-terminal proBNP plasma levels correlate with severity of mitral stenosis. J Heart Valve Dis. 2005;14:735–41. [PubMed] [Google Scholar]
- 66.Gerber I, Stewart R, Legget M, West TM, French RL, Sutton TM, et al. Increased plasma natriuretic peptide levels reflect symptom onset in aortic stenosis. Circulation. 2003;107:1884–90. doi: 10.1161/01.CIR.0000060533.79248.0C. [DOI] [PubMed] [Google Scholar]
- 67.Kahveci G, Bayrak F, Mutlu B, Bitigen A, Karaahmet T, Sonmez K, et al. Prognostic value of N-terminal pro-B-type natriuretic peptide in patients with active infective endocarditis. Am J Cardiol. 2007;99:1429–33. doi: 10.1016/j.amjcard.2006.12.071. [DOI] [PubMed] [Google Scholar]
- 68.Bayram E, Kocatürk H, Yücel O, Atalay C, Colak MC, Atesal S. The role of adrenomedullin and brain natriuretic peptide levels in acute rheumatic fever in adults. Anadolu Kardiyol Derg. 2008;8:188–91. [PubMed] [Google Scholar]
- 69.Zhang QY, Du JB, Chen YH, Li WZ. Change in plasma Nterminal pro-brain natriuretic peptide in children with Kawasaki disease and its value in clinical practice. Zhonghua Er Ke Za Zhi. 2006;44:886–90. [PubMed] [Google Scholar]
- 70.Pfister R, Diedrichs H, Larbig R, Erdmann E, Schneider CA. NTpro- BNP for differential diagnosis in patients with syncope. Int J Cardiol. 2009;133:51–4. doi: 10.1016/j.ijcard.2007.11.082. [DOI] [PubMed] [Google Scholar]
- 71.Usui Y, Tomiyama H, Hashimoto H, Takata Y, Inoue Y, Asano K, et al. Plasma B-type natriuretic peptide level is associated with left ventricular hypertrophy among obstructive sleep apnoea patients. J Hypertens. 2008;26:117–23. doi: 10.1097/HJH.0b013e3282f06eb4. [DOI] [PubMed] [Google Scholar]
- 72.Ybarra J, Planas F, Pou JM. Aminoterminal pro-brain natriuretic peptide (NT-proBNP) and sleep-disordered breathing in morbidly obese females: A cross-sectional study. Diab Vasc Dis Res. 2008;5:19–24. doi: 10.3132/dvdr.2008.004. [DOI] [PubMed] [Google Scholar]
- 73.Yap LB, Mukerjee D, Timms PM, Ashrafian H, Coghlan JG. Natriuretic peptides, respiratory disease, and the right heart. Chest. 2004;126:1330–6. doi: 10.1378/chest.126.4.1330. [DOI] [PubMed] [Google Scholar]
- 74.McCullough PA, Hollander JE, Nowak RM, Storrow AB, Duc P, Omland T, et al. Uncovering heart failure in patients with a history of pulmonary disease: Rationale for the early use of B-type natriuretic peptide in the emergency department. Acad Emerg Med. 2003;10:198–204. doi: 10.1111/j.1553-2712.2003.tb01990.x. [DOI] [PubMed] [Google Scholar]
- 75.Enea I, Ceparano G, Mazzarella G, Di Sarno R, Cangiano G, Busino CA. Biohumoral markers and right ventricular dysfunction in acute pulmonary embolism: The answer to thrombolytic therapy. Ital Heart J Suppl. 2004;5:29–35. [PubMed] [Google Scholar]
- 76.Yap LB, Mukerjee D, Timms PM, Ashrafian H, Coghlan JG. Natriuretic peptides, respiratory disease, and the right heart. Chest. 2004;126:1330–6. doi: 10.1378/chest.126.4.1330. [DOI] [PubMed] [Google Scholar]
- 77.Charpentier J, Luyt C, Fulla Y, Vinsonneau C, Cariou A, Grabar S, et al. Brain natriuretic peptide: A marker of myocardial dysfunction and prognosis during severe sepsis. Crit Care Med. 2004;32:660–5. doi: 10.1097/01.ccm.0000114827.93410.d8. [DOI] [PubMed] [Google Scholar]
- 78.Henriksen JH, Gotze JP, Fuglsang S, Christensen E, Bendtsen F, Moller S. Increased circulating pro-brain natriuretic peptide (proBNP) and brain natriuretic peptide (BNP) in patients with cirrhosis: Relation to cardiovascular dysfunction and severity of disease. Gut. 2003;52:1511–7. doi: 10.1136/gut.52.10.1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ozmen B, Ozmen D, Parildar Z, Mutaf I, Bayindir O. Serum Nterminal- pro-B-type natriuretic peptide (NT-pro-BNP) levels in hyperthyroidism and hypothyroidism. Endocr Res. 2007;32:1–8. doi: 10.1080/07435800701670047. [DOI] [PubMed] [Google Scholar]
- 80.Anne M, Juha K, Timo M, Mikko T, Olli V, Kyösti S, et al. Neurohormonal activation in ischemic stroke: Effects of acute phase disturbances on long-term mortality. Curr Neurovasc Res. 2007;4:170–5. doi: 10.2174/156720207781387169. [DOI] [PubMed] [Google Scholar]
- 81.Berendes E, Walter M, Cullen P, Prien T, Van Aken H, Horsthemke J, et al. Secretion of brain natriuretic peptide in patients with aneurysmal subarachnoid haemorrhage. Lancet. 1997;349:245–9. doi: 10.1016/s0140-6736(96)08093-2. [DOI] [PubMed] [Google Scholar]
- 82.Gardner DG. Natriuretic peptides: Markers or modulators of cardiac hypertrophy? Trends Endocrinol Metab. 2003;14:411–6. doi: 10.1016/s1043-2760(03)00113-9. [DOI] [PubMed] [Google Scholar]
- 83.Saito Y, Nakao K, Nishimura K, Sugawara A, Okumura K, Obata K, et al. Clinical applications of atrial natriuretic polypeptide in patients with congestive heart failure: Beneficial effects on left ventricular function. Circulation. 1987;76:115–24. doi: 10.1161/01.cir.76.1.115. [DOI] [PubMed] [Google Scholar]
- 84.Hayashi M, Tsutamoto T, Wada A, Fujii M, Ohno K, Sakai H, et al. Intravenous atrial natriuretic peptide prevents left ventricular remodeling in patients with first anterior acute myocardial infarction. J Am Coll Cardiol. 2001;37:1820–6. doi: 10.1016/s0735-1097(01)01233-5. [DOI] [PubMed] [Google Scholar]
- 85.Barrett BJ, Parfrey PS. Prevention of nephrotoxicity induced by radiocontrast agents. N Engl J Med. 1994;331:1449–50. doi: 10.1056/NEJM199411243312111. [DOI] [PubMed] [Google Scholar]
- 86.Kurnik BR, Allgren RL, Genter FC, Solomon RJ, Bates ER, Weisberg LS. Prospective study of atrial natriuretic peptide for the prevention of radiocontrast-induced nephropathy. Am J Kidney Dis. 1998;31:674–80. doi: 10.1053/ajkd.1998.v31.pm9531185. [DOI] [PubMed] [Google Scholar]
- 87.Mills RM, LeJemtel TH, Horton DP, Liang C, Lang R, Silver MA, et al. Sustained hemodynamic effects of an infusion of nesiritide (human b-type natriuretic peptide) in heart failure: A randomized, double blind, placebo controlled clinical trial. Natrecor Study Group. J Am Coll Cardiol. 1999;34:155–62. doi: 10.1016/s0735-1097(99)00184-9. [DOI] [PubMed] [Google Scholar]
- 88.O'Connor CM, Starling RC, Hernandez AF, Armstrong PW, Dickstein K, Hasselblad V, et al. Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med. 2011;365:32–43. doi: 10.1056/NEJMoa1100171. [DOI] [PubMed] [Google Scholar]
- 89.Kapoor PM, Aggarwal V, Chowdhury U, Chowdhury M, Singh SP, Kiran U. Comparison of B-type natriuretic peptide and left ventricular dysfunction in patients with constrictive pericarditis undergoing pericardiectomy. Ann Card Anaesth. 2010;13:123–9. doi: 10.4103/0971-9784.62942. [DOI] [PubMed] [Google Scholar]


