Abstract
As robotic assisted surgery is gaining popularity in gynecologic surgery, resident physicians are becoming more experienced in this modality. Many trainees will utilize this technology after residency either in general practice or subspecialty fellowship.
Study Objective
The primary aim of this study was to describe credentialing requirements for newly graduated resident physicians for robotic gynecologic surgery in Alabama.
Design
III
Design Classification
III
Setting
Alabama, USA
Subjects
Credentialing authorities at hospitals in the state of Alabama that currently utilize robotic surgery in the field of gynecology were contacted.
Interventions
Participants completed an online questionnaire regarding credentialing policies.
Measurements and Main Results
Fifteen of the 16 hospitals (94%) in Alabama that utilize robotic technology for gynecologic surgery participated in this survey. All hospitals had a credentialing policy for robotic surgery, but only 9/15 hospitals (60%) had a separate pathway for physicians with recent residency training. This pathway consisted of an attestation letter from a residency program director in all 9 hospitals, a robotic case list in 3/9 (33%), and proctored cases following residency in 2/9 (22%). Five (55%) required a certain number of hysterectomy cases (median 5, range 2–10).
Conclusion
Robotic surgery credentialing requirements in Alabama are variable. Validation of requirements in best practices for robotic surgery by graduating resident physicians is needed.
Introduction
The use of robotic surgery has increased rapidly since the Da Vinci Surgical System (Intuitive Surgical, Sunnyvale, CA, USA) obtained FDA approval for gynecologic surgery in 2005. By 2009, more robotic surgeries were performed for gynecologic indications than all other robotic surgical specialties combined [1]. Gynecologic surgeons utilize the Da Vinci Surgical System for procedures such as hysterectomy, myomectomy, pelvic and paraaortic lymph node dissection, radical hysterectomy, sacrocolpopexy and tubal reanastamoses.
There is ongoing debate regarding the responsibility of hospitals to ensure that surgeons are being trained, credentialed and monitored in an ethical manner to utilize robotic surgery. The American College of Obstetricians and Gynecologists offers no specific recommendation, but comments that “credentialing for robotic-assisted surgery within and across specialties is based on training, experience, and documented current competency” [2]. This issue is attracting increasing attention as there have been recent reports of litigation directed at hospitals resulting from insufficient training and insufficient credentialing for surgeons who are newly trained in robotic surgery [3]. The majority of literature in this area focuses on the training and credentialing of surgeons who are adopting this technology after completing residency. This is appropriate, as the majority of surgeons utilizing this new technology are not newly graduated resident surgeons with experience in robotic surgery. However, residents who have graduated in recent years may have had considerable robotic surgical experience. We are unaware of any recommendations for, or reports of, credentialing practices for newly graduated residents with robotic surgery experience during residency.
The primary aim of this study was to describe regional credentialing requirements for robotic gynecologic surgery for physicians hired directly out of residency. . Our secondary aim was to describe credentialing authorities for robotic surgery in Alabama. We performed a cross-sectional study of hospitals in Alabama to characterize their robotic credentialing practices for newly graduated residents in obstetrics and gynecology.
Materials and Methods
IRB approval was obtained from the University of Alabama at Birmingham. All hospitals in the state of Alabama who were actively performing robotic gynecologic surgery in July of 2010 were identified by contacting the industry representative. The credentialing authority at each institution was identified by the hospital call centers. A cover letter was sent describing the purpose of the study and an on-line survey tool was used to develop a twelve-question survey (Figure 1). The survey was distributed to the robotic credentialing authority at each institution by email on July 28, 2010. The last survey was completed on August 15, 2010. The survey was designed to assess the robotic surgery credentialing practices for newly graduated residents in obstetrics and gynecology. Participants were asked to identify their role in credentialing and whether they had a separate credentialing policy for newly graduated residents who have had robotic experience in residency. Participants were asked to rank (unnecessary, desirable or essential) the following factors: industry sponsored on-site training, industry sponsored on-line training modules, industry sponsored off-site training, number of cases previously performed as primary surgeon, and number of cases previously performed as an assistant or secondary surgeon. Participants were asked to provide the minimum number of hysterectomies or myomectomies that they require in order for a newly graduated resident to obtain credentialing. They were also queried about what proportion of a case would need to be performed by the resident for them to be counted towards credentialing. Finally, participants were asked what documentation they require from the newly graduated OB/GYN resident about their robotic experiences.
Figure 1.
Online Survey of Credentialing Authorities in Alabama
Results
Sixteen hospitals in Alabama were identified who perform robotic assisted gynecologic surgery. Fifteen hospitals (93.8%) participated in this survey and the mean number of years each hospital has performed robotic gynecologic surgery is 2.9 years (range 1–7 years). The credentialing authority at each hospital is the Obstetrics and Gynecology department chair (67%), the chair of general surgery (7%), or the director of robotic surgery (27%). Nine (60%) of the credentialing authorities reported that they perform robotic surgery in their practice.
All hospitals reported a credentialing policy for robotic surgery, but only 9/15 (60%) had a separate pathway for physicians with recent residency training. Four of 9 (44%) reported that they have hired newly graduated obstetric/gynecology residents who have sought robotic privileges (Table 1). Three of the four hospitals (75%) required additional training for their newly graduated residents, two required a specific number of cases, and one required additional proctored cases regardless of the number of cases performed in residency. Two of the six hospitals without a separate pathway had also hired newly graduated residents who had sought robotic privileges.
Table 1.
Characteristics of Credentialing Authorities for Robotic Gynecologic Surgery in Alabama (n=15)
| Professional Role of Credentialing Authority | ||
| Chair of Obstetrics and Gynecology | 10 | 67% |
| Chair of Robotic Surgery Committee | 4 | 27% |
| Chair of General Surgery | 1 | 7% |
|
| ||
| Robotic Credentialing Policies | ||
| Policy for practicing physicians obtaining privileges | 15 | 100% |
| Separate policy for newly graduated physicians | 9 | 60% |
|
| ||
| Hospital Hiring | ||
| Hired newly graduated physicians with robotic training | 6 | 40% |
Of the 9 hospitals with a separate pathway for newly graduated physicians with recent resident training in robotics, all require an attestation letter from the residency director and one requires a letter from industry. Five (55%) require a certain number of hysterectomy cases be performed in residency (median 5, range 2–10), and three (33%) require a case list. Of the 5 authorities that require a certain number of cases, all require that the resident performed at least one side of the hysterectomy and closure of the vaginal cuff, two require that all vascular pedicles be performed, and one requires that the complete hysterectomy be performed to be counted as a case. Two of 9 (22%) require that all newly graduated residents must be proctored. When asked to comment on how essential industry training is for credentialing, 2/9 (22%) responded that some form of industry-sponsored training is essential and the remaining 7 report that it is desirable (Figure 2).
Figure 2.
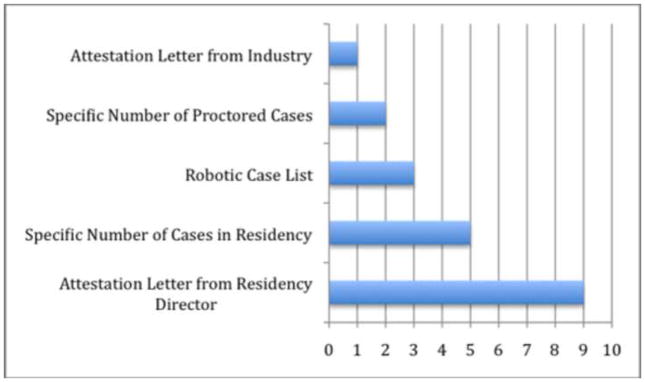
Required Elements in Robotic Surgery Credentialing Policies for Newly Graduation Physicians (n=9)
Of all responding credentialing authorities, 12/15 (80%) felt there was a minimum number of hysterectomies that were necessary to be performed during residency for credentialing a newly graduated resident, ranging from 2–25 (median 5). Three of 15 (20%) responded that regardless of the number of cases performed during residency, new physicians should be proctored.
Discussion
Robotic surgery credentialing requirements at hospitals in Alabama for newly graduated obstetrics and gynecology residents are variable. Forty percent of these hospitals do not have a separate credentialing practice for newly graduated residents to obtain privileges in robotic surgery. All institutions required an attestation from the residency director, and the majority required a minimum number of hysterectomies performed and reported that industry sponsored training was desirable.
The rapid expansion of robotic surgery in gynecology has been described as, “(the) perfect storm of rapidly advancing technology, increasing patient demand, the universal desire for patient safety, and the need to prioritize limited healthcare resources.” [1]. Safe and ethical implementation of this new technology has presented considerable challenges for our specialty. There are no accepted specific recommendations for credentialing in robotic surgery. Lenihan et al recently proposed a model for ethical credentialing and privileging in robotic surgery and they recommended that surgeons applying for privileges who have received initial training and certification elsewhere, should have undergone didactic study, dry laboratory simulation, case observation, live animal model laboratory, and proctored cases (2 minimum), and that they should have their first 5 cases undergo focused review at the new institution [1]. The American Association of Gynecologic Laparoscopists has established an interest group tasked with the establishment of uniform credentialing guidelines [4]. However, in the absence of any specific recommendations from our ACOG, AAGL or AMA credentialing will continue to vary and hospitals will be left to establish their own criteria for robotic surgery.
Surgeons (n=138) were surveyed at the World Robotics Gynecology Congress in 2010 and reported that a mean of 3.29 (range 2 to 10) proctored cases were required at their hospital prior to granting robotic privileges [1]. They also reported that a mean of 13.8 cases were required annually to maintain credentialing at their institution. We report that only 3/15 (20%) credentialing authorities in Alabama require that all new physicians be proctored. This low percentage is in contrast to best credentialing practices that have been reported in urology which reflect that proctoring is very important for acquiring proficiency in robotic surgery; however, surgeons acquiring these skills during residency are proctored by their faculty [5].
There are clear medico-legal risks associated with insufficient credentialing and privileging practices. The claim of negligent credentialing is recognized in at least 32 states [3]. Some have recommended that strict criteria be avoided because there is variation in the number of cases required to achieve competency and plantiff attorneys may use an institution’s own written criteria against them.
The minimum number of cases necessary for robotic credentialing of newly graduated physicians that we report (median = 5) may be a bar that has been set too low. The number of cases required to establish proficiency in robotic surgery has been reported to be as high as 150 to 250 cases [6]. Data available regarding the number of hysterectomies needed to improve operative time ranges from 20–50 cases [7–9]. Furthermore, only 3.6% of 470 obstetrics and gynecology residents surveyed in 2011 reported that they felt equipped to perform robotic surgery without additional training, and only 28% of residency directors whose programs include robotics curriculum have reported that they believe that their program was “effective” or “very effective” [11]. This lack of confidence of residency program directors in their robotic curriculum also calls into question the validity and appropriateness of a letter from the program director to credentialing authorities.
The strengths of this study include that it is a first report on a relevant topic in gynecologic surgery training with a robust response rate. This study is limited by the small number of institutions queried and by the lack of a validated tool, responder anonymity and national representation. Credentialing practices may vary across the country and this study should be repeated on a larger scale.
Newly graduating residents seeking robotic surgery privileges will likely be required to provide an attestation letter from the residency program director. Industry sponsored training is required by some hospitals, but desired by most. In light of the recent focused attention on negligent credentialing litigation, the minimum required number of cases reported here may increase. Future work should focus on the effectiveness of credentialing practices regarding robotic surgery.
Conclusion
Credentialing practices for robotic gynecologic surgery in Alabama vary for newly graduating residents. Further work is warranted to establish validated best practices for safe and ethical implementation of robotic surgery by newly graduated resident physicians.
Acknowledgments
Financial Support or Funding: Partially funded by the National Institute of Diabetes and Digestive and Kidney Diseases 2K24-DK068389 to HER.
Footnotes
Presented at the CREOG & APGO Annual Clinical Meeting, San Antonio, Texas, March 9-12, 2011
Disclaimer/Conflict of Interest: BK Erickson – none; JL Gleason – none ; WK Huh receives funding from Intuitive Surgical; HE Richter – none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lenihan JP. Navigating credentialing, privileging, and learning curves in robotic with an evidence and experienced-based approach. Clin Obstet and Gynecol. 2011;54:382–90. doi: 10.1097/GRF.0b013e31822b47e2. [DOI] [PubMed] [Google Scholar]
- 2.Robot-assisted Surgery. ACOG Technology Assessment in Obstetrics and Gynecology No. 6. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2009;114:1153–55. doi: 10.1097/AOG.0b013e3181c33c4f. [DOI] [PubMed] [Google Scholar]
- 3.Lee YL, Kilic GS, Phelps JY. Medicolegal review of liability risks for gynecologists stemming from lack of training in robot-assisted surgery. J Minim Invasive Gynecol. 2011;18:512–15. doi: 10.1016/j.jmig.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Advincula AP. Roadmap to robotics. AAGL News Scope. 2010;24:9. [Google Scholar]
- 5.Lee JY, Mucksavage P, Sundaram CP, et al. Best practices for robotic surgery training and credentialing. J Urology. 2011;185:1191–97. doi: 10.1016/j.juro.2010.11.067. [DOI] [PubMed] [Google Scholar]
- 6.Barbash GI, Glied SA. New technology and health care costs: the case of robot-assisted surgery. N Eng J Med. 2010;368:701–4. doi: 10.1056/NEJMp1006602. [DOI] [PubMed] [Google Scholar]
- 7.Pitter MC, Anderson P, Blissett A, Pemberton N. Robotic-assisted gynaecological surgery-establishing training criteria; minimizing operative time and blood loss. Int J Med Robot. 2008;4:114–20. doi: 10.1002/rcs.183. [DOI] [PubMed] [Google Scholar]
- 8.Payne TN, Dauterive FR. A Comparison of total laparoscopic hysterectomy to robotically assisted hysterectomy: surgical outcomes in a community practice. J Minim Invasive Gynecol. 2008;15:286–91. doi: 10.1016/j.jmig.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 9.Lenihan JP, Kovanda C, Seshadri-Kreaden U. What is the learning curve for robotic assisted gynecologic surgery? J Minim Invasive Gynecol. 2008;15:589–94. doi: 10.1016/j.jmig.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 10.Gobern JM, Novak CM, Lockrow EG. Survey of robotic surgery training in obstetrics and gynecology residency. J Minim Invasive Gynecol. 2011;18:755–60. doi: 10.1016/j.jmig.2011.08.004. [DOI] [PubMed] [Google Scholar]