Abstract
Background.
It is unclear whether distinct weight-related trajectory classes, differing in course, demographics, and health characteristics, exist in the elderly population.
Methods.
Data came from the 10-year (1986–1996) Duke Established Populations for Epidemiologic Studies of the Elderly study of 3,861 black (54%) and white (46%) participants aged 65–105 years. Latent-class trajectories of body mass index (BMI: kg/m2) based on self-reported weight and height at baseline, 3, 6, and 10 years later were determined using generalized mixture models. Polytomous logistic regression was used to identify baseline demographic and health characteristics that distinguished the trajectories, and 10-year postbaseline data to confirm the findings.
Results.
We identified three trajectories: normal weight (BMI ~24, 27.6% of the sample), overweight (BMI ~26, 65.1%), and obese (BMI ~31, 7.3%). Demographic characteristics distinguished the three trajectories: highest odds of blacks, women, and less education in the obese trajectory, lowest in the normal-weight trajectory. Obese and overweight differed adversely from normal-weight trajectories, but not significantly from each other on cognitive impairment, hypertension, and diabetes. Depressive symptomatology was more prevalent in the obese; they were also younger. There was no association with cancer or heart disease.
Conclusion.
Distinct trajectories and course of BMI were present in this older population. Weight loss increased with increase in BMI class. Although demographic characteristics distinguished all trajectory classes, adverse health characteristics distinguished the overweight and obese classes from the normal-weight class, but not from each other. Problems associated with education and health are present at study entry and should be addressed earlier in life.
Key Words: Body mass index, Trajectory, Elderly.
ALTHOUGH increase in obesity in adults may have plateaued (1), obesity has been occurring at successively younger ages (2), and its impact remains to be fully felt in the older population (3). Obesity is a risk factor for many adverse health conditions (including diabetes, cardiovascular disease, hypertension, stroke, and certain cancers [4]), which are already more prevalent in the older population (5), functional disability (6,7), increased health service use and cost (8), and possibly reduced longevity (9). The extent to which these associations hold in the older population and how weight changes over time in persons aged 65 years and older remain unclear (10–13).
Longitudinal studies have typically used a population averaging approach, which may conceal notable differences within the population. Recently, more sophisticated analytic procedures, such as generalized growth mixture models (GMM [14]), have been used to identify the presence of distinct latent-class trajectories within a population. Such analyses identify classes with unique characteristics, classes that might not otherwise be noticed, and classes that may merit different types of attention. Regarding examination of obesity, latent-class trajectory analyses have only been applied to data from young-to-late middle-aged samples (15–18), but the findings indicate what may be expected in older age. All these studies (sample sizes from ~5,000 to 90,000 participants), used self-reported height and weight to determine body mass index (BMI: weight (kg)/height/[m2]). They followed ages 12–23 (17), 18–49 (18), 19–35 (15), and 25–59 (16), typically identifying four latent-class trajectories, from normal weight to obese, each increasing in BMI over time. An exception was the study of 19- to 35-year-old persons (15), which yielded two classes, and the 25- to 59-year-old persons, where one trajectory (with small representation) showed gain and then loss. In all studies except the latter, which did not look at this issue, heavier weight was associated with poorer health status or adverse outcome. Overall, in these young-to-late middle age representative samples, several latent classes of increasing BMI were present. In only one instance, and for only a small proportion, was decline in BMI found.
Here, we examine BMI over a 10-year period in a community-representative sample of whites and blacks aged 65 and older. We anticipate that multiple latent-class trajectories of BMI will be found. Given conflicting prior findings, we did not predict trajectory direction (BMI increase or decrease), but we did predict that classes reflecting higher BMI would be associated with more adverse circumstances.
Methods
Sample
Data come from the Duke site of the Established Populations for Epidemiologic Studies of the Elderly, a 10-year longitudinal study of a stratified random sample of community-based residents aged 65 years and older, in five adjacent counties in the Piedmont area of North Carolina (19). At baseline (1986/87), 4,162 sample members (80% of those contacted) enrolled (black: 54% [oversampled to improve statistical precision for this group]; white: 45%; <1% “other race”); 65% were women. We excluded persons of “other race” (N = 26) with proxy respondents at baseline (N = 162) or with BMI missing at all time points (N = 113), yielding an analysis sample of 3,861 participants. The study was approved by the Institutional Review Board of Duke University Medical Center. Consent forms were signed by all participants.
Data Gathering
Sample members were interviewed in-person at home at baseline, 3, 6, and 10 years later. Using structured questionnaires, trained interviewers gathered information at baseline on demographic characteristics, and at each in-person wave on self-reported height, weight, and mental and physical health condition, and survival status. At the third in-person interview, height and weight were also measured.
Dependent variable.—
Our dependent variable is BMI, obtained from self-reported height and weight at each of the four in-person waves. In this sample, there was good agreement between self-reported and measured height, weight, and BMI (intraclass correlation coefficients 0.85, 0.97, and 0.91, respectively [20]). BMI was imputed when information on height or weight was missing to maintain the sample (Statistical Analysis section).
Independent variables.—
Demographic characteristics included race (black and white), age (continuous), sex, and years of education curtailed at 17 years.
Health status.—
For baseline and 10-year postbaseline analysis, we noted self-reported, doctor-diagnosed stroke, heart disease, hypertension, diabetes, and cancer (excluding skin cancer). Cognitive status was measured using the Short Portable Mental Status Questionnaire (21). An error score ≥4 (possible range 0–10) indicated cognitive impairment. A modified Center for Epidemiologic Studies-Depression (CES-D) scale (19,22) measured depressive symptomatology. Each item was scored 0 or 1 (scoring range 0–20 symptoms), and the summed score dichotomized between 8 and 9 (recoded as 0 and 1), corresponding to the original CES-D cut-point of 15 and 16, in agreement with previous work (19).
Statistical Analysis
Imputation for height and weight.—
Depending on wave, missing values ranged from 8.8% to 14.8% for height and from 4.4% to 9.5% for weight. Initial analyses indicated that a respondent’s values of height and weight were highly correlated across waves. First, systematic discrepancy between self-reported and measured height was adjusted by adding to measured height the mean of the difference between measured and self-reported height determined separately by gender within quintiles of measured height (self-reported height tends to be higher than measured height). All available measures of height were then averaged to yield the imputed value for height. Evaluation of this approach by regressing wave 1 height on an imputed height variable yielded R 2 = 0.78. A similar procedure was used for weight. First, mean difference in weight between successive waves (by gender within weight quintiles) was determined, and it was used to adjust upwards available data on weight. It was then averaged to yield imputed weight (R 2 = 0.82). When only height (weight) was absent on all waves, stochastic regression was used to impute height (weight), based on race, gender, education, income, baseline weight (height), and health status (and smoking status in estimating weight). These predictors yielded R 2 = 0.50 for baseline height, and R 2 = 0.29 for weight. The manner of imputation (23) was designed to maximize accuracy at each wave. However, because information from other waves was used to impute missing data at a particular wave, the imputed data to some extent overestimate stability across waves. BMI was estimated for 199 participants (5.15%).
Basic descriptive statistics (N, %, mean, and standard deviation [SD]) were used to characterize the sample, and χ2 was used to examine bivariate differences using SAS 9.2.
The number of trajectory classes of BMI using GMM (24) was determined using M-plus version 5.2 (14). GMM determines subgroups of trajectories in the data set. To determine the form of the curve, we fit the intercept only, linear (ie, with intercept and slope), and quadratic (ie, with intercept, slope, and squared) model to the data. The number of latent classes was determined by sequentially increasing the number of classes and examining fit statistics (Akaike information criteria, Bayesian information criteria [BIC], sample size-adjusted BIC, entropy, and condition number). Lo–Mendell–Rubin sequential test was used to determine if the decrease in likelihood ratio with increase in classes was statistically significant. Model convergence was tested with a number of start values to ensure proper solution. In addition to the Lo–Mendell–Rubin test, bootstrap-based testing, together with theoretical and substantive considerations, was also used to determine the number of classes. Participants were included in the trajectory they best fit, that is, there is no “crisp” separation of people.
Polytomous logistic regression was used to compare the trajectories in controlled multivariable models. Baseline characteristics were used to identify differences for all participants present at baseline. To check whether these differences held throughout the years of the study, we repeated the analyses with 10-year postbaseline survivors and 10-year postbaseline data.
Results
The analysis sample consisted of 3,861 participants (65% women, 54% black, and median education 8 years). Details are given in Table 1. Mean (SD) of BMI was 26.04 (4.94). The 199 participants for whom BMI was imputed were, on average, older, more likely to be black, women, with less education, cognitively impaired (each p < .0001), having high depressive symptomatology (p = .008), and reporting stroke (p < .0001) and diabetes (p = .025) (Supplementary Table 1).
Table 1.
Descriptive Characteristics of the Sample at Baseline.
| Total sample (N = 3,861) | Normal (N = 1,066) (27.6%) | Overweight (N = 2,514) (65.1%) | Obese (N = 281) (7.3%) | |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | |
| Demographic characteristics | ||||
| Age (y) | ||||
| 65–74 | 2,437 (63.1) | 700 (65.7) | 1,535 (61.1) | 202 (71.9) |
| 75–84 | 1,173 (30.4) | 301 (28.2) | 799 (31.8) | 73 (26.0) |
| 85+ | 251 (6.5) | 65 (6.1) | 180 (7.2) | 6 (2.1) |
| Race | ||||
| White | 1,762 (45.6) | 630 (59.1) | 1,073 (42.7) | 59 (21.0) |
| Black | 2,099 (54.4) | 436 (40.9) | 1,441 (57.3) | 222 (79.0) |
| Sex | ||||
| Male | 1,366 (35.4) | 439 (41.2) | 870 (34.6) | 57 (20.3) |
| Female | 2,495 (64.6) | 627 (58.8) | 1,644 (65.4) | 224 (79.7) |
| Education (y) | ||||
| 0–8 y | 2,020 (52.3) | 418 (39.2) | 1,409 (56.1) | 193 (68.7) |
| 9–12 y | 1,285 (33.3) | 421 (39.5) | 795 (31.6) | 69 (24.6) |
| >12 y | 556 (14.4) | 227 (21.3) | 310 (12.3) | 19 (6.8) |
| Mental health | ||||
| Cognitive impairment* | 422 (11.0) | 87 (8.2) | 303 (12.1) | 32 (11.5) |
| Depression† | 357 (9.5) | 79 (7.6) | 231 (9.4) | 47 (17.0) |
| Physical health conditions | ||||
| Stroke | 324 (8.4) | 63 (5.9) | 230 (9.2) | 31 (11.0) |
| Heart attack | 581 (15.1) | 151 (14.2) | 391 (15.6) | 39 (14.0) |
| Hypertension | 2,220 (57.5) | 521 (49.0) | 1,498 (59.6) | 201 (71.5) |
| Diabetes | 773 (20.1) | 145 (13.6) | 545 (21.7) | 83 (29.5) |
| Cancer (excluding skin) | 362 (9.4) | 101 (9.5) | 234 (9.3) | 27 (9.6) |
Note: Percentages may not total 100 because of rounding.
*Cognitive impairment indicated by Short Portable Mental Status Questionnaire error score ≥4.
†Depression indicated by modified Center for Epidemiologic Studies-Depression scale score ≥9.
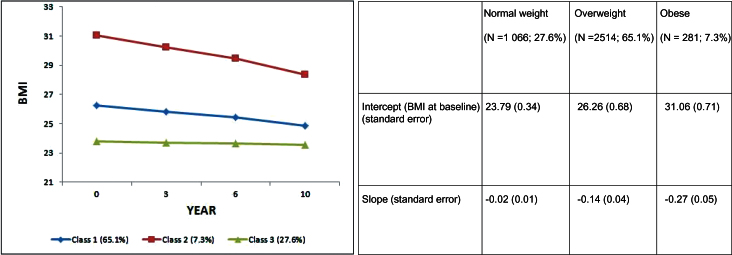
Analysis indicated that three trajectories of BMI best fit the data (Figure 1). They were a high normal class (baseline BMI = 23.8, n = 1,066, and 27.6% of the sample), consistent over time (BMI 23.7, 23.7, 23.6; 3, 6, and 10 years later; p < .094); a mildly overweight class (baseline BMI = 26.3, n = 2,514, and 65.1%), which declined by 1.4 BMI units over 10 years (BMI 25.8, 25.4, 24.9; 3, 6, and 10 years later; p < .000); and an obese class (baseline BMI = 31.1, n = 281, and 7.3%), which declined by 2.7 BMI units over 10 years (BMI: 30.2, 29.4, 28.4; 3, 6, and 10 years later; p < .000). We compared the distribution across the three trajectory classes of those for whom BMI was immediately calculable with those for whom it was imputed. Specifically (nonimputed BMI precedes imputed BMI): normal-weight class—28.1% (18.1%), overweight—64.5% (76.4%), and obese class—7.4% (5.5%). The differences in distribution reflect the health characteristics of the imputed group and were appropriate to class assignment (characteristics of the latent-class trajectories are described later). These health characteristics were not included in the imputation procedure, suggesting that imputation was appropriate.
Figure 1.
Latent class trajectories of BMI.
Unadjusted comparison of the three trajectories (Table 1) indicated a higher proportion of blacks, women, and younger persons in the obese class and higher proportion of whites and men in the normal-weight class. Cognitive impairment was more common in the overweight and least common in the normal-weight trajectory, whereas depression was most common in the obese class. Heart attack and cancer were comparable across classes, but stroke, hypertension, and diabetes were most prevalent in the obese class and least prevalent in the normal-weight class.
Fully controlled polytomous logistic regressions (reference: normal-weight group) (Table 2) found that with increase in weight class, there was an increased representation of blacks, women, and people with less education. There was a fourfold increased odds of blacks and a threefold increased odds of women in the obese trajectory compared with 64% increase and 37% increase, respectively, in the overweight trajectory. Members of both the obese and overweight trajectories had less education than those in the normal-weight trajectory, with the difference between the obese and overweight trajectories just missing significance. Uniquely, members of the obese trajectory were more likely to be younger (5% for each year of age) than those in the normal-weight trajectory.
Table 2.
Fully Controlled Polytomous Logistic Regression (Reference: Normal-Weight Trajectory Class), Baseline Data.
| Overweight | Obese | |||
|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | |
| Age | 1.01 (0.99, 1.02) | 0.243 | 0.95 (0.92, 0.97) | <.0001 |
| Race (black) | 1.57 (1.34, 1.84)* | <0.0001 | 4.05 (2.88, 5.70)* | <.0001 |
| Sex (female) | 1.35 (1.15, 1.58)* | 0.001 | 3.14 (2.23, 4.42)* | <.0001 |
| Education (y) | 0.93 (0.91, 0.95)† | <0.0001 | 0.88 (0.85, 0.92)† | <.0001 |
| Cognitive impairment‡ | 1.52 (1.14, 2.04)† | 0.005 | 1.77 (1.08, 2.91)† | 0.023 |
| Depression§ | 1.02 (0.77, 1.34) | 0.916 | 1.77 (1.16, 2.70)† | 0.008 |
| Stroke | 1.28 (0.93, 1.75) | 0.132 | 1.44 (0.87, 2.40) | 0.158 |
| Heart | 1.02 (0.82, 1.27) | 0.835 | 0.92 (0.61, 1.39) | 0.692 |
| Hypertension | 1.32 (1.13, 1.54)† | 0.001 | 1.74 (1.28, 2.38)† | 0.001 |
| Diabetes | 1.57 (1.27, 1.93)† | <0.0001 | 1.75 (1.25, 2.46)† | 0.001 |
| Cancer (excluding skin) | 1.02 (0.78, 1.32) | 0.909 | 1.28 (0.80, 2.06) | 0.303 |
Note: Unmarked values = not significantly different from normal-weight class.
*Overweight and obese trajectory classes are significantly different from each other and from normal-weight class.
†Overweight and obese trajectory classes differ significantly from normal-weight class, but not from each other.
‡Cognitive impairment indicated by Short Portable Mental Status Questionnaire error score ≥4.
§Depression indicated by modified Center for Epidemiologic Studies-Depression scale score ≥9.
Members of both obese and overweight trajectories were more likely than normal-weight trajectory members to be cognitively impaired, but only members of the obese trajectory were more likely to have substantial depressive symptomatology. Only hypertension and diabetes discriminated the normal weight from the overweight and obese trajectories. Although odds for each condition were higher for the obese class, the differences between the overweight and obese trajectory classes were not statistically significant.
The characteristics that distinguished the trajectories at baseline held 10 years later for 10-year postbaseline data, except that for the obese trajectory, stroke was now significant but depression lost significance (on average, members were now overweight).
Overall, 49.3% of participants died during the study. Death was most likely in the overweight class (53.8%) and least likely in the normal weight (40.8%) and obese (41.3%) classes (chi square, 2 df =58.34, p < .0001). At the final wave, 9.3% of the survivors dropped out (refusals, lost, moved, etc.): normal weight: 9.4%; overweight: 9.4%; obese: 8.5% (chi square, 2 df = 7.71, p < .025).
Discussion
The vast majority of longitudinal studies of BMI have used a population-averaging approach which, while identifying general trends over time, conceals potential differences within the population examined. To our knowledge, this is the first longitudinal study of BMI in an older population that, using a latent-class trajectory approach, determines whether there are notable differences within an elderly sample, their distinguishing characteristics, and differences in course.
Using a GMM approach, we identified three latent-class trajectories of BMI—normal weight, overweight, and obese—in a biracial, representative community-resident sample aged 65 and older. The characteristics of these classes were shown to be comparable 10 years later. The presence of distinct trajectories of BMI in the older population complements findings of multiple trajectories for younger adults: two latent-class trajectories were identified in one analysis (15) and four latent-class trajectories in three others (16–18). However, whereas the studies of young adults typically showed increase in BMI over time, this study of an older sample showed stability (the normal-weight class), minor decline (overweight class), or more marked decline (the obese class). So, unlike previous studies that used a population-averaging approach and identified general weight decline in older age (10–12), this study, which identifies three classes within this sample, indicates that weight decline is focused and is more likely for the overweight and particularly for the obese. Weight decline is unlikely to have been due to dropout or death. Dropout was least in the obese class, which had death rates comparable to the normal-weight class.
Although previous reports suggest a gradation of demographic, mental, and physical health characteristics with increase in BMI (3,15,18,25–28), in our study, this was found uniformly only for demographic characteristics. It did not hold for mental or physical health characteristics. Stroke (possibly because of low prevalence), heart disease (the definition of which may have been too restrictive), and cancer (where only certain cancers have been found to be associated with BMI) did not distinguish among the three latent-class trajectories. Agreeing with some studies, but not with others (29–31), there was a greater odds of cognitive impairment in the overweight and the obese classes, which did not differ significantly from each other. The same held for hypertension and diabetes, although point estimates suggested increased odds of disadvantage in the obese class. Depressive symptomatology was an exception, distinguishing only the obese class from the normal-weight class. Interestingly, depression, which may have a bidirectional association with obesity (32,33), was no longer associated with the obesity trajectory 10 years later, when the level of obesity had declined. Unlike previous studies (34), we did not find that overweight was protective for mortality, perhaps because this was the oldest class.
Latent-class trajectory analysis offers a more nuanced approach and a more accurate depiction of obesity in this population, providing an opportunity to better design and in particular target interventions to classes at risk. We agree with previous findings on the association of demographic and health characteristics with BMI (indicating the validity of present findings), while providing information not previously presented and highlighting information to which too little attention has been paid. First, older people are not uniform—three different trajectory classes of BMI are present in this older, community representative sample. Second, change in weight is not uniform. Weight is stable over 10 years in older people of normal weight and declines minimally in the overweight and more markedly in the obese. Although most studies indicate that the overweight have the lowest mortality, in this study this was not the case, perhaps because the overweight were the oldest. Although the overweight did not have increased depressive symptomatology, their morbidity was otherwise not significantly different from that of the obese class—any additional weight appears to have health consequences. Finally, we must remain aware of the interrelationships among and between BMI, and the demographic, mental, and physical health characteristics examined (31,33,35–40). This provides alternative opportunities to intervene with the intent of improving health. Because this is an integrated system, any particular intervention may affect multiple potential outcomes.
This study has limitations. Most information is self-reported, although self-report is reasonably reliable (41). Information on cognition and depressive symptomatology was gathered using validated, reliable measures, but are not clinical diagnoses. The accuracy of self-reported height and weight, and hence BMI, has been determined for this sample and is substantial (20). To maintain sample characteristics and size, BMI was imputed where relevant, the procedure used could have increased the stability of the trajectory classes that were found. Imputation, however, appears to have been appropriate. Although health characteristics were not included in the BMI imputation procedures, those for whom imputation was needed had health characteristics in common with the overweight (and obese) class trajectories to which they were disproportionately assigned, suggesting that imputation was reasonably accurate. Imputation allowed inclusion of participants who were more demographically challenged and sicker and so increased the representativeness of the findings. Our data come from the south-eastern United States, where obesity is highest. In consequence, our findings may indicate the status of older persons in other geographical areas which are now reaching the levels of additional weight found here. Finally, present findings need to be replicated.
People enter older age with the impact of the demographic characteristics and health conditions accumulated up to that time. Their weight does not have a uniform course, which has implications for well-being (42). As the present analysis shows, we need to understand the diversity present, so that we can tailor response accordingly.
Funding
This work was supported by the National Institute on Aging at the National Institutes of Health (contract number N01-AG12102; grant numbers R01 AG12765, R01 AG17559, and 5P30 AG028716), National Institute of Mental Health (grant 2P50-MH60451), and by National Center for Research Resources at the National Institutes of Health Clinical and Translational Science Awards grant 5UL1 RR024128-04. The content of this publication is solely the responsibility of the authors and does not necessarily reflect the views or policies of the U.S. Department of Health and Human Services, National Institute of Health, National Institute of Mental Health, or the National Institute on Aging. The information presented here was previously presented at the annual scientific meeting of the Gerontological Society of America, Atlanta, GA, 2009.
Supplementary Material
Supplementary material can be found at: http://biomedgerontology.oxfordjournals.org/.
References
- 1. Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010; 303: 235–241 [DOI] [PubMed] [Google Scholar]
- 2. Lee JM, Pilli S, Gebremariam A, et al. Getting heavier, younger: trajectories of obesity over the life course. Int J Obes (Lond). 2010; 34: 614–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang Y, Beydoun MA. The obesity epidemic in the United States – gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007; 29: 6–28 [DOI] [PubMed] [Google Scholar]
- 4. National Heart, Lung, and Blood Institute [NHLBI] Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. NIH Publication No. 98-4083, September 1998 http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.htm Accessed November 2, 2011.
- 5. Schneider KM, O’Donnell BE, Dean D. Prevalence of multiple chronic conditions in the United States’ Medicare population. Health Qual Life Outcomes. 2009; 7: 82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Houston DK, Ding J, Nicklas BJ, et al. The association between weight history and physical performance in the Health, Aging and Body Composition study. Int J Obes (Lond). 2007; 31: 1680–1687 [DOI] [PubMed] [Google Scholar]
- 7. Alley DE, Chang VW. The changing relationship of obesity and disability, 1988-2004. JAMA. 2007; 298: 2020–2027 [DOI] [PubMed] [Google Scholar]
- 8. Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Aff (Millwood). 2009; 28: w822–w831 [DOI] [PubMed] [Google Scholar]
- 9. Olshansky SJ, Passaro DJ, Hershow RC, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005; 352: 1138–1145 [DOI] [PubMed] [Google Scholar]
- 10. Cornoni-Huntley JC, Harris TB, Everett DF, et al. An overview of body weight of older persons, including the impact on mortality. The National Health and Nutrition Examination Survey I–Epidemiologic Follow-up Study. J Clin Epidemiol. 1991; 44: 743–753 [DOI] [PubMed] [Google Scholar]
- 11. Stevens J, Knapp RG, Keil JE, Verdugo RR. Changes in body weight and girths in black and white adults studied over a 25 year interval. Int J Obes. 1991; 15: 803–808 [PubMed] [Google Scholar]
- 12. Kahng SK, Dunkle RE, Jackson JS. The relationship between the trajectory body mass index and health trajectory among older adults: multilevel modeling analyses. Res Aging. 2004; 26: 31–61 [Google Scholar]
- 13. Botoseneanu A, Liang J. The effect of stability and change in health behaviors on trajectories of body mass index in older Americans: a 14-year longitudinal study. J Gerontol A Biol Sci Med Sci. 2012; 67: 1075–1084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Muthén B, Muthén L. M-plus User’s Guide. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- 15. Clarke PJ, O’Malley PM, Schulenberg JE, Johnston LD. Midlife health and socioeconomic consequences of persistent overweight across early adulthood: findings from a national survey of American adults (1986-2008). Am J Epidemiol. 2010; 172: 540–548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jun HJ, Corliss HL, Nichols LP, Pazaris MJ, Spiegelman D, Austin SB. Adult body mass index trajectories and sexual orientation: the Nurses’ Health Study II. Am J Prev Med. 2012; 42: 348–354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nonnemaker JM, Morgan-Lopez AA, Pais JM, Finkelstein EA. Youth BMI trajectories: evidence from the NLSY97. Obesity (Silver Spring). 2009; 17: 1274–1280 [DOI] [PubMed] [Google Scholar]
- 18. Ostbye T, Malhotra R, Landerman LR. Body mass trajectories through adulthood: results from the National Longitudinal Survey of Youth 1979 Cohort (1981-2006). Int J Epidemiol. 2011; 40: 240–250 [DOI] [PubMed] [Google Scholar]
- 19. Blazer D, Burchett B, Service C, George LK. The association of age and depression among the elderly: an epidemiologic exploration. J Gerontol. 1991; 46: M210–M215 [DOI] [PubMed] [Google Scholar]
- 20. Fillenbaum GG, Kuchibhatla MN, Whitson HE, et al. Accuracy of self-reported height and weight in a community-based sample of older African Americans and whites. J Gerontol A Biol Sci Med Sci. 2010; 65: 1123–1129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975; 23: 433–441 [DOI] [PubMed] [Google Scholar]
- 22. Radloff L. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psych Meas. 1977; 1: 385–401 [Google Scholar]
- 23. Landerman LR, Land KC, Pieper CF. An empirical evaluation of the predictive mean matching method for imputing missing values. Sociol Method Res. 1997; 26: 3–34 [Google Scholar]
- 24. Muthén B. Second-generation structural equation modeling with a combination of categorical and continuous latent variables: new opportunities for latent class/latent growth modeling. In: Collins LM, Sayer A, eds. New Methods for the Analysis of Change. Washington, DC: American Psychological Association; 2001: 291–322 [Google Scholar]
- 25. Kerwin DR, Zhang Y, Kotchen JM, et al. The cross-sectional relationship between body mass index, waist-hip ratio, and cognitive performance in postmenopausal women enrolled in the Women’s Health Initiative. J Am Geriatr Soc. 2010; 58: 1427–1432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 2007; 29: 29–48 [DOI] [PubMed] [Google Scholar]
- 27. Rokholm B, Baker JL, Sørensen TI. The levelling off of the obesity epidemic since the year 1999–a review of evidence and perspectives. Obes Rev. 2010; 11: 835–846 [DOI] [PubMed] [Google Scholar]
- 28. Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull. 1989; 105: 260–275 [DOI] [PubMed] [Google Scholar]
- 29. Isaac V, Sim S, Zheng H, Zagorodnov V, Tai ES, Chee M. Adverse Associations between visceral adiposity, brain structure, and cognitive performance in healthy elderly. Front Aging Neurosci. 2011; 3: 12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kerwin DR, Gaussoin SA, Chlebowski RT, et al. Interaction between body mass index and central adiposity and risk of incident cognitive impairment and dementia: results from the Women’s Health Initiative Memory Study. J Am Geriatr Soc. 2011; 59: 107–112 [DOI] [PubMed] [Google Scholar]
- 31. Sturman MT, de Leon CF, Bienias JL, Morris MC, Wilson RS, Evans DA. Body mass index and cognitive decline in a biracial community population. Neurology. 2008; 70: 360–367 [DOI] [PubMed] [Google Scholar]
- 32. de Wit L, Luppino F, van Straten A, Penninx B, Zitman F, Cuijpers P. Depression and obesity: a meta-analysis of community-based studies. Psychiatry Res. 2010; 178: 230–235 [DOI] [PubMed] [Google Scholar]
- 33. Needham BL, Epel ES, Adler NE, Kiefe C. Trajectories of change in obesity and symptoms of depression: the CARDIA study. Am J Public Health. 2010; 100: 1040–1046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Durazo-Arvizu R, Cooper RS, Luke A, Prewitt TE, Liao Y, McGee DL. Relative weight and mortality in U.S. blacks and whites: findings from representative national population samples. Ann Epidemiol. 1997; 7: 383–395 [DOI] [PubMed] [Google Scholar]
- 35. Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001; 24: 1069–1078 [DOI] [PubMed] [Google Scholar]
- 36. Fillenbaum GG, Pieper CF, Cohen HJ, Cornoni-Huntley JC, Guralnik JM. Comorbidity of five chronic health conditions in elderly community residents: determinants and impact on mortality. J Gerontol A Biol Sci Med Sci. 2000; 55: M84–M89 [DOI] [PubMed] [Google Scholar]
- 37. Flint AJ, Hu FB, Glynn RJ, et al. Excess weight and the risk of incident coronary heart disease among men and women. Obesity (Silver Spring). 2010; 18: 377–383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Oreopoulos A, McAlister FA, Kalantar-Zadeh K, et al. The relationship between body mass index, treatment, and mortality in patients with established coronary artery disease: a report from APPROACH. Eur Heart J. 2009; 30: 2584–2592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Paeratakul S, Lovejoy JC, Ryan DH, Bray GA. The relation of gender, race and socioeconomic status to obesity and obesity comorbidities in a sample of US adults. Int J Obes Relat Metab Disord. 2002; 26: 1205–1210 [DOI] [PubMed] [Google Scholar]
- 40. van den Berg E, Kloppenborg RP, Kessels RP, Kappelle LJ, Biessels GJ. Type 2 diabetes mellitus, hypertension, dyslipidemia and obesity: A systematic comparison of their impact on cognition. Biochim Biophys Acta. 2009; 1792: 470–481 [DOI] [PubMed] [Google Scholar]
- 41. Baumeister H, Kriston L, Bengel J, Härter M. High agreement of self-report and physician-diagnosed somatic conditions yields limited bias in examining mental-physical comorbidity. J Clin Epidemiol. 2010; 63: 558–565 [DOI] [PubMed] [Google Scholar]
- 42. Arnold AM, Newman AB, Cushman M, Ding J, Kritchevsky S. Body weight dynamics and their association with physical function and mortality in older adults: the Cardiovascular Health Study. J Gerontol A Biol Sci Med Sci. 2010; 65: 63–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.