Abstract
Purpose
To identify factors associated with attrition in a longitudinal study of cardiovascular prevention.
Methods
Demographic, clinical and psychosocial variables potentially associated with attrition were investigated in 1,841 subjects enrolled in the southwestern Pennsylvania Heart Strategies Concentrating on Risk Evaluation study. Attrition was defined as study withdrawal, loss to follow-up, or missing ≥50% of study visits.
Results
Over four years of follow up, 291 subjects (15.8%) met criteria for attrition. In multivariable regression models, factors that were independently associated with attrition were: Black race (Odds Ratio(OR):2.21, 95%Confidence Interval(CI):1.55, 3.16; P<0.001), younger age (OR per 5-year increment:0.88, 95%CI:0.79, 0.99; P<0.05), male sex (OR: 1.79, 95%CI: 1.27, 2.54; P<0.05), no health insurance (OR:2.04, 95%CI:1.20, 3.47; P<0.05), obesity (OR:1.80, 95%CI:1.07, 3.02; P<0.05), CES-D depression score≥16 (OR:2.02, 95%CI:1.29, 3.19; P<0.05), higher ongoing life events questionnaire score (OR=1.09, 95%CI= 1.04–1.13; P<0.001). Having a spouse/partner participating in the study was associated with lower odds of attrition (OR=0.60 95%CI=0.37–0.97; P<0.05). A synergistic interaction was identified between black race and depression.
Conclusions
Attrition over four years was influenced by sociodemographic, clinical and psychological factors that can be readily identified at study entry. Recruitment and retention strategies targeting these factors may improve participant follow-up in longitudinal cardiovascular prevention studies.
MeSH headings: Cardiovascular Diseases, Cohort Studies, Lost to Follow-Up
Results from longitudinal cohort studies of cardiovascular disease (CVD) have contributed to the decline in age-standardized CVD mortality rates. Decreasing subject participation and retention rates in cohort studies, which have been occurring over the past several decades 1–3, may compromise the integrity of study results by negatively impacting biases of results, statistical power, and generalizability of findings4–6. Participant loss to follow-up (LTFU) and missing study visits are inevitable and are related to length of follow-up and complexity of study protocols 7.
Researchers have been encouraged to report their study’s retention strategies and identify factors that influence subject retention6,8–10. Nevertheless, little information exists about associations of demographic, clinical and psychosocial factors, both individually and in combination, on study attrition. This is particularly relevant to investigations that include underrepresented populations such as minorities and women 11–13. Furthermore, the expense of conducting health care research, low percentages of individuals who enroll in studies and potential risks to subjects make systematic efforts to reduce study attrition an important priority9, 14. Our study aimed to identify characteristics associated with attrition in a middle-age cohort of 1,841 subjects in the Heart Strategies Concentrating on Risk Evaluation (Heart SCORE) study.
METHODS
Heart SCORE is an ongoing study of 2,000 middle aged whites and blacks in southwestern Pennsylvania.15 Heart SCORE aims to improve risk stratification, identify racial disparities and evaluate mechanisms for population differences in CVD. After a baseline evaluation, subjects underwent annual visits which included measurements of traditional and emerging CVD risk factors, tabulation of adverse events and assessments of subclinical atherosclerosis. The present analysis was confined to 1,841 subjects (92% of cohort). Sixty-seven subjects who self-reported race other than black or white were not included because the number of participants in these categories was too small for a meaningful analysis. Participants known to be deceased (n=34) and those in the window for their 4-year visits at the time of analysis (n=58) were excluded in order to accurately evaluate the occurrence of attrition over 4 years. All subjects provided written informed consent approved by the University of Pittsburgh Institutional Review Board.
Data collection
Age, race, sex, education level, annual income and health insurance status were obtained by self-report at baseline. Race was self-identified as “Black or African American”, “White”, “Asian”, “American Indian or Native Alaskan”, “Native Hawaiian or Pacific Islander”, “Other”. Education was categorized as “some college or higher” or “less than college”. Annual income was reported as: “<$10,000”, “10,000-<$20,000”, “$20,000-<$40,000”, “$40,000-<$80,000” and “≥$80,000”. Subjects self-reported any history of CVD (coronary heart disease, heart failure, stroke) and other chronic conditions. At baseline, subjects completed psychosocial scales, including the Center for Epidemiologic Studies Depression Scale (CES-D)16, Cook-Medley Hostility Scale (CMHI)17, State-Trait Anger Inventory (STAI anger)18, State-Trait Anxiety Inventory (STAI anxiety) 19, Cohen Perceived Stress Scale 20, Unfair Treatment Scale 21, Ongoing Life Events Score (OLE) 22, Life Orientation Test (LOT) 23, Life Engagement Score (LES) 24 and Social Network Index 25. Measurements including weight, height, waist circumference and blood pressure were performed at baseline and annually. Fasting venous blood was drawn annually to measure lipids, and glucose. Study coordinators recorded any difficulties with phlebotomy.
Study Recruitment
Subjects were recruited through mass mailings, advertisements and referrals from the general community, other participants, and physicians. Minority recruitment was enriched through community-based health screening events conducted in partnership with the Pittsburgh Theological Seminary and Urban League of Greater Pittsburgh. Subjects recruited at community events, in physician offices, through community sources, or by other participants were considered “proactively” recruited, in contrast to those who were recruited through mass mailings or advertisements.
Retention strategies
Multiple strategies are used to maximize retention and timeliness of follow-up visits: (1) Subject contact and scheduling- the University of Pittsburgh Graduate School of Public Health call center schedules annual visits. A reminder letter is sent five weeks before the subject’s scheduled follow-up visit; phone calls are made one week and one day prior to visits. During these calls, contact information is updated and subjects are instructed to complete annual questionnaires. (2) Annual study visit- Annual visits (≈45 minutes) include a limited physical examination and blood specimen collection. Subjects are offered nutritional counseling. Beverages and parking validation are provided. (3) Educational benefits- semi-annual newsletters are mailed to provide information about CVD topics, results of analyses, examples of subject experiences implementing lifestyle changes, and healthy recipes. Educational seminars are offered twice yearly. (4) Other research opportunities- Ancillary studies are periodically offered. For example, subjects were given an opportunity to enroll in a study of a portable home monitoring to investigate the link between sleep apnea and CVD. (5) Missed visits and disenrollment procedures- when a subject misses a visit, call center staff initiate repeated attempts at telephone contact until the subject is reached and the visit is rescheduled. If phone contact is unsuccessful, a letter is mailed to ask the subject to call the scheduling office. A Pennsylvania Department of Health database is searched periodically to query vital status on subjects who fail to respond to this letter. If a subject is not identified as deceased, his/her secondary contacts are called to request that the subject contact the study office. Subjects who fail to complete an annual visit are given a 6-month window to show up or complete a mailing package. “Off-study” forms are completed for subjects who withdraw from the study.
Definition of attrition variables
A “missed visit” is assigned when a subject does not show up or return the mailing package corresponding to his/ her annual visit within the expected date plus a 6-month window but is subsequently seen or returns mailing information. Subjects who fail to show up for their visit and do not return mailings for their last three annual visits for any reason other than death are classified as “lost to follow-up” (LTFU). Two categories of study subjects were defined: (1) “Attrition group,” which included LTFU, subjects who withdrew from the study and those who missed ≥2 of 4 annual visits; (2) “Stayers,” which is the complement of attrition (i.e., subjects who missed zero or one annual visit).
Statistical analyses
Baseline characteristics were compared between stayers and the attrition group. Continuous variables were described by means(standard deviations) and compared by t-tests. Categorical variables were described by percentages and compared by chi-square tests. Univariable logistic regression models were used to assess the association between baseline demographic, clinical and psychosocial variables and study attrition. Variables that had P-values<0.10 and those judged to be clinically relevant were included in multivariable models. Multiplicative and additive interactions between the significant predictors of attrition were explored. Multiplicative terms were included in the models and three measures for additive interaction and their 95%Confidence intervals(CI) were calculated26: relative excess risk of interaction (RERI), attributable proportion of interaction, and synergy index. If there are no interactions, RERI and the attributable proportions of interaction are both 0 and the synergy index is 1. All data analyses were performed using SPSS statistical package version 19.0 (SPSS, Inc., Chicago, IL). Two-sided P-values<.05 were considered statistically significant.
RESULTS
Demographic characteristics
Analyses were confined to 1,841 subjects who self-reported race as either black (43%) or white and who completed the timeframe for their 4-year follow-up visit. Baseline characteristics are presented in Table 1. Mean age was 59.1±7.5 years and 73.4% of subjects were <65 years old. A majority of individuals (81.4%) had at least some college education and 57.7% had at least an associate degree. More than half reported an annual income ≥$40,000 and 20.1% reported an annual income ≥$80,000.
Table 1.
Sociodemographic and Clinical Characteristics for the Total Cohort and by Categories of Study Retention. Heart SCORE Study, Southwestern Pennsylvania, 2007–2011.
| Characteristic | Total (n=1841) |
Stayers group (n=1550) |
Attrition group (n=291) |
p |
|---|---|---|---|---|
| Age, mean (SD) | 59.1 (7.5) | 59.4 (7.4) | 57.7 (7.9) | <0.001 |
| Race, % | ||||
| White | 57.0 | 60.5 | 38.1 | <0.001 |
| Black | 43.0 | 39.5 | 61.9 | |
| Female, % | 65.8 | 66.4 | 62.2 | 0.22 |
| Education level (Some college or more), % | 81.4 | 82.1 | 77.6 | 0.07 |
| Annual income, % | <0.001 | |||
| <$20,000 | 17.2 | 15.2 | 28.0 | |
| $20,000-< $40,000 | 28.3 | 28.3 | 28.4 | |
| $40,000-< $80,000 | 34.4 | 35.3 | 29.5 | |
| ≥$80,000 | 20.1 | 21.2 | 14.0 | |
| No insurance or self pay, % | 5.5 | 4.4 | 11.5 | <0.001 |
| Having spouse or partner in the study, % | 25.7 | 27.4 | 16.5 | <0.001 |
| BMI, Kg/m2, mean (SD) | 30.1 (6.3) | 29.8(6.1) | 31.9(7.2) | <0.001 |
| Metabolic status (ATP-3), % | <0.001 | |||
| Normal | 68.0 | 70.0 | 57.5 | |
| Metabolic syndrome | 21.1 | 20.9 | 21.8 | |
| Diabetes | 10.9 | 9.0 | 20.7 | |
| Having been proactively recruited for the study, % | 30.9 | 29.9 | 36.7 | 0.02 |
| Having experienced blood drawn difficulty at baseline study visit, % | 16.8 | 16.0 | 20.9 | 0.05 |
SD=standard deviation; BMI=Body mass index, ATP-3=Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)
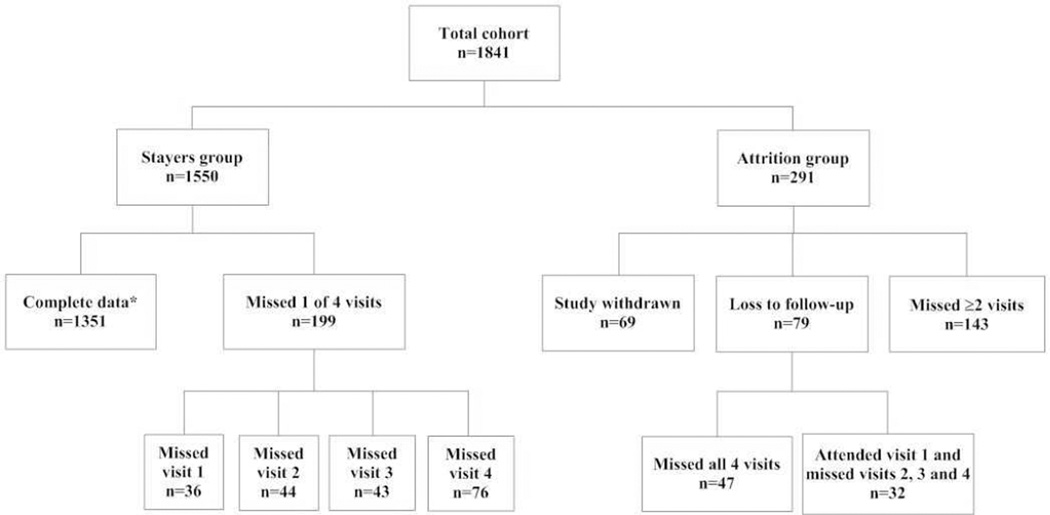
Figure 1 depicts the distribution of subjects according to categories of retention and illustrates that 1,351(73.4%) subjects had complete data (i.e., no missed visits) and 199(10.8%) missed only one visit over four years. Sixty-nine(3.7%), 79(4.3%), and 143(7.8%) subjects withdrew, were LTFU, and missed ≥50% of their annual visits, respectively. In total, 291 subjects(15.8%) met the definition of study attrition.
Figure 1.
Distribution of participants according to categories of study retention. Heart SCORE study, southwestern Pennsylvania, 2007–2011.
*Complete data: No missed visits (1 to 4)
As shown in Table 1, in comparison with stayers (n=l,550), the 291 individuals in the attrition group were younger [57.7(7.9) versus 59.4(7.4) years; P<0.001], more likely to be black (61.9% versus 39.5%; P<0.001), and had a higher mean body mass index(BMI) [31.9(7.2) versus 29.8(6.l)kg/m2; P<0.001]. The attrition group had a significantly greater percentage of individuals who reported income <$40,000 (56.4% versus 43.5%; P<0.00l) and were uninsured (11.5% versus 4.4%, P<0.001). The percentage of subjects who had a spouse or partner participating in the study was significantly lower in the attrition group (16.5 versus 27.4%, P<0.001). Having been “proactively recruited” for the study was more frequent among those in the attrition group (36.7% versus 29.9%, P=0.02). The percentage of subjects who reported any difficulty or discomfort during phlebotomy at their baseline visit was nominally higher in the attrition group (20.9% versus 16%, P=0.05).
Psychosocial variables
Table 2 shows the percentage of individuals with a CES-D score≥16, which is indicative of at least mild depression 27, as well as mean scores for continuous psychosocial scales by categories of retention. Subjects in the study attrition group had significantly higher scores on depression, hostility, anger, anxiety, stress, unfair treatment, OLE and LOT scales. Life engagement (purpose in life) and social network (diversity and number of social contacts) scores were similar between the two groups. Additional analyses showed that black race was significantly associated with higher scores for depression, hostility, unfair treatment and ongoing life events (data not shown).
Table 2.
Psychosocial Measures for the Total Cohort and by Categories of Study Retention. Heart SCORE Study, Southwestern Pennsylvania, 2007–2011.
| Total (n=1841) | Stayers group (n=1550) |
Attrition group (n=291) |
p | |
|---|---|---|---|---|
| Depression (CES-D score ≥16), % | 11.6 | 10.0 | 22.9 | <0.001 |
| CMHI hostility, mean (SD) | 8.1 (4.4) | 7.9(4.3) | 9.2 (4.7) | <0.001 |
| STAI anger, mean (SD) | 5.3 (3.6) | 5.1 (3.5) | 6.1 (4.3) | <0.001 |
| STAI anxiety, mean (SD) | 6.2 (4.8) | 6.0 (4.6) | 7.5 (5.7) | <0.001 |
| Cohen stress score, mean (SD) | 4.3 (3.0) | 4.1 (2.9) | 5.4(3.5) | <0.001 |
| Unfair treatment, mean (SD) | 7.2(4.5) | 7.0 (4.4) | 9.0 (4.9) | <0.001 |
| Ongoing life events score, mean (SD) | 5.5 (4.2) | 5.2 (4.0) | 7.3 (5.1) | <0.001 |
| Life orientation test, mean (SD) | 23.2 (4.0) | 23.3 (3.9) | 22.4 (4.6) | 0.008 |
| Life engagement score, mean (SD) | 26.7 (5.3) | 26.8 (5.2) | 26.2 (5.4) | 0.09 |
| Social network diversity, mean (SD) | 5.5(1.8) | 5.5(1.8) | 5.4 (2.0) | 0.23 |
| Number of social contacts, mean (SD) | 27.7 (24.2) | 27.6 (24.3) | 28.5 (23.4) | 0.62 |
CES-D: Center for Epidemiologic Studies Depression Scale; CMHI: Cook-Medley Hostility Scale; STAI anger: State-Trait Anger Inventory; STAI anxiety: State-Trait Anxiety Inventory.
Uni- and multivariable analyses
Socio-demographic and clinical characteristics found to be significantly associated with study attrition in univariable logistic regression models were: Black race, younger age, annual income<$20,000, no health insurance, working status other than currently working or retired, not living with spouse/partner, not having a spouse/partner in the study, proactively recruited, obesity (BMI≥30 kg/m2) and difficulty during phlebotomy at baseline study visit. The percentage of subjects with ≥3 chronic medical conditions was not significantly higher for the attrition group (29.4% versus 24.8%, P=0.13). With the exception of life engagement score and social network variables, all studied psychological variables were univariably associated with attrition.
Multivariable logistic regression models identified black race, no health insurance, male sex, obesity, and a CES-D≥16 as the strongest factors independently associated with attrition (Table 3). Having a spouse/partner in the study was independently associated with a lower odds of attrition after adjusting for demographic, clinical and psychosocial variables (Odds Ratio(OR):0.60, 95%CI: 0.37, 0.97; ,P=0.04). Marital status did not play a confounding role on the association between having a spouse/partner in the study and attrition (data not shown). Having been proactively recruited for the study was associated with attrition after adjusting for race, age, sex, health insurance status and body weight status (Models 1 and 2, Table 3), but this was not significant in the presence of psychological predictors (Model 3, Table 3). In comparison with whites and after adjustment for age, sex, health insurance status, having spouse/partner in the study, recruitment strategy, body weight status, depression score and OLE score, blacks had more than twice the odds of study attrition (OR:2.21, 95%CI:1.55, 3.16; P<0.001). Being obese conferred 80% higher odds of study attrition in the fully adjusted model. Additional analyses indicated that each kg/m2 of BMI was associated with an estimated 3% increase in the odds of study attrition (OR: 1.03, 95%CI: 1.01, 1.06; P=0.004). Not having health insurance and a CES-D score≥16 were independently associated with two-fold odds for attrition. Education and income levels were not independent predictors of attrition.
Table 3.
Adjusted Associations of Sociodemographic, Clinical and Psychological Factors on Study Attrition. Heart SCORE Study, Southwestern Pennsylvania, 2007–2011.
| Regression Model 1 | Regression Model 2 | Regression Model 3 | ||||
|---|---|---|---|---|---|---|
| OR | Confidence Interval |
OR | Confidence Interval |
OR | Confidence Interval |
|
| Race (black vs white) | 2.75* | 2.01,3.77 | 2.35* | 1.70,3.26 | 2.21* | 1.55,3.16 |
| Age (5-year increment) | 0.85** | 0.77,0.95 | 0.86** | 0.77,0.95 | 0.88** | 0.79,0.99 |
| Sex (male vs female) | 1.46** | 1.07, 1.99 | 1.48** | 1.07,2.03 | 1.79** | 1.27,2.54 |
| No insurance or self-pay (vs. insurance) | 2.54* | 1.59,4.07 | 2.54* | 1.58,4.09 | 2.04** | 1.20,3.47 |
| Having spouse or partner in the study (vs. not) | 0.61** | 0.40,0.93 | 0.61** | 0.40, 0.94 | 0.60** | 0.37,0.97 |
| Having been Proactively recruited for the study | 1.40** | 1.03, 1.90 | 1.39** | 1.02, 1.90 | 1.22*** | 0.86, 1.72 |
| Category of body weight (vs normal) | ||||||
| Overweight | 1.21*** | 0.73,2.03 | 1.05*** | 0.60, 1.83 | ||
| Obese | 2.05** | 1.26,3.34 | 1.80** | 1.07,3.02 | ||
| CES-D (≥16 vs <16) | 2.02** | 1.29–3.19 | ||||
| Ongoing life events score | 1.09* | 1.04–1.13 | ||||
CES-D: Center for Epidemiologic Studies Depression Scale
p<0.001,
p<0.05,
Non significant
Note: Regression Model 1 included race, age, sex, health insurance, having spouse or partner in the study and having been proactively recruited for the study. Regression Model 2 included variables in Model 1 plus categories of body weight. Regression Model 3 included variables in Model 2 plus CES-D and Ongoing life events score.
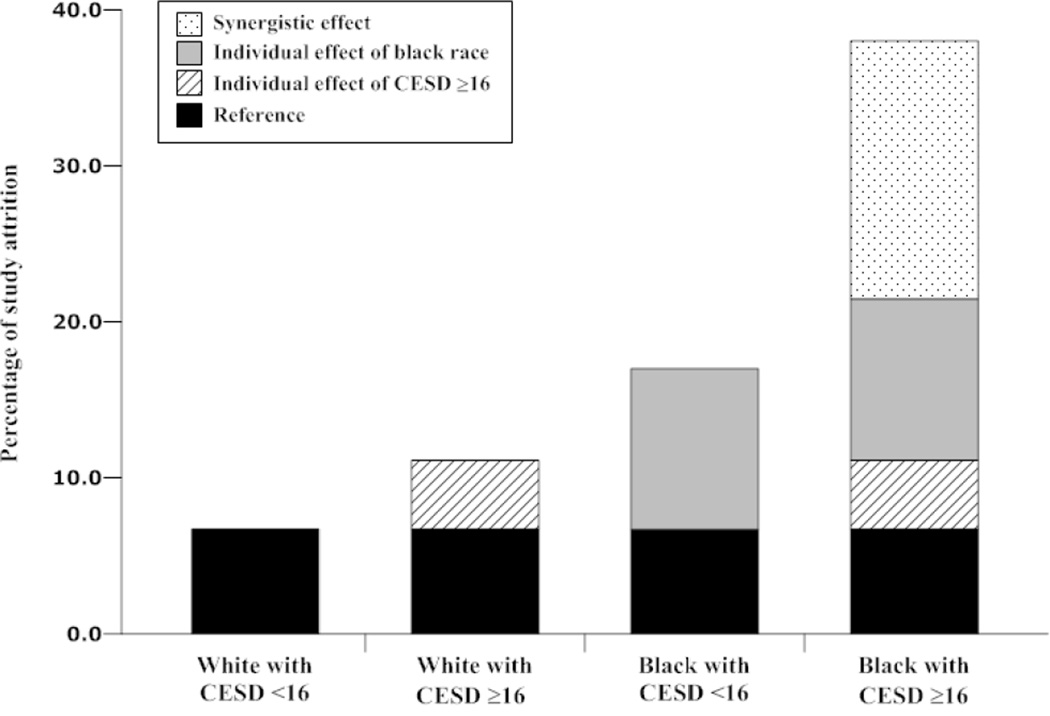
Interactions among variables
Compared with whites with a CES-D score<16, study attrition was significantly higher in blacks and subjects with a CES-D≥16. After adjustment for other predictors, the 3 interaction measures on the additive scale showed significantly higher values than the null (RERI:3.29, 95%CI:0.46, 6.12; attributable proportion of interaction:0.63, 95%CI:0.37, 0.88; synergy index:4.37, 95%CI:1.31, 14.57), indicating a synergistic association of black race and depression on study attrition (Figure 2). Additive interactions between race and sex, health insurance status and obesity were explored, but no significant interactions were found. All multiplicative interaction terms including race, sex, health insurance status, obesity and CES-D score failed to reach statistical significance in multivariable models.
Figure 2.
Individual and joint associations between race, CES-D depression score ≥16 and study attrition. Heart SCORE study, southwestern Pennsylvania, 2007–2011.
CES-D: Center for Epidemiologic Studies Depression Scale
DISCUSSION
The Heart SCORE study of CVD risk enrolled 2,000 subjects in southwestern Pennsylvania. Over four years of follow up, we found that study attrition was highest among blacks, males, younger individuals, subjects without health insurance, obese subjects, and those with at least mild depression or a higher ongoing life events score. Having a spouse/partner participating in the study was associated with lower study attrition.
Our findings indicate that study attrition is a nonrandom event that is dependent on characteristics that can be readily identified at study entry. This concept has important implications on the design and analyses of other research studies. For example, our finding that black race is a strong independent predictor of attrition should prompt investigators to consider novel and culturally-sensitive methods to over-recruit and retain blacks in observational studies. Targeted strategies can address reported observations that blacks, as compared to whites, have a lower perceived benefit of study participation 28 and place a lower priority on health promotion and disease prevention 29. Other addressable issues are transportation difficulties, inconvenient clinic hours, challenges related to literacy levels, lost wages, family concerns about research and child-care difficulties 30. Investigators can also dispel the belief that researchers are more interested in research than in patient well-being 30,31.
Similar considerations should be given to males and younger individuals, who were more likely to be in our “study attrition” group. These findings are consistent with reports indicating that younger age is associated with higher loss to follow-up, which may be explained by greater geographical mobility among younger study subjects 32,33. Younger individuals may also perceive less disease susceptibility and less benefit from ongoing participation in long-term studies. Similar concepts may explain our finding that being proactively recruited was associated with higher attrition. In contrast, individuals who were recruited through mailings or advertisements were more likely to be retained, indicating that these methods may recruit a group with less geographic mobility and greater self-interest in and commitment to long-term participation in protocols.
New retention strategies can capitalize on other noted observations. Obesity emerged as a strong independent predictor of study attrition. Given the increasing prevalence of obesity and the importance of enrolling obese patients in CVD study cohorts, study designs should consider retention methods that are relevant to obese individuals such as providing transportation and addressing co-morbidities that may preclude long-term study commitment. In contrast, our finding that having a spouse/partner who was a study subject was independently associated with a lower rate of attrition needs to be interpreted cautiously. While this might be used as a marker for lower risk of attrition, we do not suggest the enrollment of couples in longitudinal research studies as a strategy to improve retention, since this might reduce independence of observations, thus creating biases and analytic complexity.
We initially postulated that a lack of health insurance would be associated with increased study retention because participation in Heart SCORE provided regular CVD risk assessments at no cost to subjects. However, our results demonstrated that a lack of health insurance was associated with increased attrition, which has been previously reported in prevention-oriented research studies30,34. Being uninsured remained a significant predictor of attrition even after adjustment for relevant demographic, clinical, and psychosocial factors, which reinforces the application of this easily obtainable information as a risk marker for study attrition.
To the best of our knowledge, ours is the first study to examine the association between a comprehensive set of psychosocial variables and attrition in a cardiovascular prevention cohort study. Ongoing life events and depression were significant independent predictors of attrition. Ongoing life events score is indicative of subject’s life changes and has been associated with the development of chronic diseases, including CVD 35. Our observation that subjects with depression symptoms had increased odds of attrition is consistent with the literature36,37. Providing psychological counseling or referrals for depression treatment might be considered a novel strategy to improve retention. Furthermore, our study identified an additive synergistic interaction between black race and a CES-D score≥16 on study attrition. It has been argued that interaction on an additive scale is more meaningful than that on a multiplicative scale for assessing biologic significance of associations and is more relevant to disease prevention and intervention 38,39. From a study design perspective, the identification of the joint association of black race and depression on attrition provides insight into characterization of a subset of individuals with disproportionally high risk for study withdrawal, loss to follow-up, or missing data and who may benefit from targeted retention strategies.
Limitations
First, our findings from an urban-based study of racial disparities of CVD in Southwestern Pennsylvania may not generalize to cohorts with different socio-demographic characteristics or from different geographic regions. Second, we employed an array of retention strategies across different themes9, resulting in a high percentage of subjects with complete data or having missed only one study visit over 4 years. This may limit the application of our findings to other studies with higher attrition rates. Third, the small number of individuals who withdrew from our study or who were LTFU precluded analysis of individual components of our definition of attrition. Fourth, identified predictors of attrition, such as race, may be surrogates for unmeasured factors (e.g., perceived benefit of study participation, mistrust of research studies)30,40. Fifth, our results may not apply to clinical trials, which may entail more frequent contact with trial subjects. Finally, our analyses examined study attrition after four years of follow-up. CVD studies, especially those investigating primary prevention, frequently require longer-term follow-up. However, our results are relevant to longer-term studies because attrition is generally highest during the early follow-up intervals41.
Conclusions
Sociodemographic, clinical and psychological factors associated with attrition from a CVD prevention study were identified. These factors can be used to inform enrollment goals, subject recruitment methods and novel targeted retention efforts for other longitudinal CVD studies. Further investigations are required to assess the influence of the factors reported in our study over longer follow-up periods and the effectiveness of new retention strategies that incorporate these factors.
Acknowledgments
The authors thank Amy Beto, Mary Catherine Coast, Jowanda Green, Andrea Dinga, Janet Bonk, Jennifer Rush, Margaret Gabriel, Catherine Thornton and Linda Dobosh for conducting study visits and for their ongoing subject retention efforts. The authors also thank Dr. Jaime Cerda from the Department of Public Health, Pontificia Universidad Católica de Chile, for his valuable comments on an earlier version of this manuscript.
Funding Sources
This study was funded by the Pennsylvania Department of Health (ME-02-384) and National Institutes of Health (R01HL089292).
List of abbreviations
- BMI
Body mass index
- CI
Confidence interval
- CES-D
Center for Epidemiologic Studies Depression Scale
- CMHI
Cook-Medley Hostility Scale
- CVD
Cardiovascular disease
- Heart SCORE
Heart Strategies Concentrating on Risk Evaluation
- LES
Life Engagement Score
- LOT
Life Orientation Test
- LTFU
Loss to follow-up
- OLE
Ongoing Life Events Score
- OR
Odds ratio
- RERI
Relative excess risk of interaction
- STAI anger
State-Trait Anger Inventory
- STAI anxiety
State-Trait Anxiety Inventory
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
None.
REFERENCES
- 1.Hartge P. Participation in population studies. Epidemiology. 2006;17:252–254. doi: 10.1097/01.ede.0000209441.24307.92. [DOI] [PubMed] [Google Scholar]
- 2.Morton LM, Cahill J, Hartge P. Reporting participation in epidemiologic studies: A survey of practice. American Journal of Epidemiology. 2006;163:197–203. doi: 10.1093/aje/kwj036. [DOI] [PubMed] [Google Scholar]
- 3.Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol. 2007;17:643–653. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 4.Goldberg M, Luce D. Selection effects in epidemiological cohorts: Nature, causes and consequences. Rev Epidemiol Sante Publique. 2001;49 477e492. [PubMed] [Google Scholar]
- 5.Szklo M, Nieto F. Epidemiology - beyond the basics. Boston, MA: Jones and Bartlett Publishers; 2004. [Google Scholar]
- 6.Marcellus L. Are we missing anything? Pursuing research on attrition. The Canadian journal of nursing research = Revue canadienne de recherche en sciences infirmieres. 2004;36:82–98. [PubMed] [Google Scholar]
- 7.Kristman V, Manno M, Cote P. Loss to follow-up in cohort studies: How much is too much? European journal of epidemiology. 2004;19:751–760. doi: 10.1023/b:ejep.0000036568.02655.f8. [DOI] [PubMed] [Google Scholar]
- 8.Chatfield MD, Brayne CE, Matthews FE. A systematic literature review of attrition between waves in longitudinal studies in the elderly shows a consistent pattern of dropout between differing studies. Journal of clinical epidemiology. 2005;58:13–19. doi: 10.1016/j.jclinepi.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Robinson KA, Dennison CR, Wayman DM, et al. Systematic review identifies number of strategies important for retaining study participants. Journal of clinical epidemiology. 2007;60:757–765. doi: 10.1016/j.jclinepi.2006.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zook PM, Jordan C, Adams B, et al. Retention strategies and predictors of attrition in an urban pediatric asthma study. Clinical trials. 2010;7:400–410. doi: 10.1177/1740774510373798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institutes of Health. [Accessed November 12, 2012];Inclusion of women and minorities as participants in research involving human subjects. ( http://grants.nih.gov/grants/funding/women_min/women_min.htm)
- 12.Corbie-Smith GM, Durant RW, St George DM. Investigators' assessment of nih mandated inclusion of women and minorities in research. Contemporary clinical trials. 2006;27:571–579. doi: 10.1016/j.cct.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 13.Ding EL, Powe NR, Manson JE, et al. Sex differences in perceived risks, distrust, and willingness to participate in clinical trials: A randomized study of cardiovascular prevention trials. Archives of internal medicine. 2007;167:905–912. doi: 10.1001/archinte.167.9.905. [DOI] [PubMed] [Google Scholar]
- 14.Cotter RB, Burke JD, Stouthamer-Loeber M, et al. Contacting participants for follow-up: How much effort is required to retain participants in longitudinal studies? Evaluation and Program Planning. 2005;28:15–21. [Google Scholar]
- 15.Bambs C, Kip KE, Dinga A, et al. Low prevalence of “ideal cardiovascular health” in a community-based population: The heart strategies concentrating on risk evaluation (heart score) study. Circulation. 2011;123:850–857. doi: 10.1161/CIRCULATIONAHA.110.980151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Radloff LS. The ces-d scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 17.Cook WW, Medley DM. Proposed hostility and pharisaic-virtue scales for the mmpi. Journal of Applied Psychology. 1954;38:414–418. [Google Scholar]
- 18.Spielberger CD, Jonhson EH, Rusell SF, et al. The experience and expression of anger. New York: Hemisphere/McGraw Hill; 1985. [Google Scholar]
- 19.Spielberger CD. Theory and research on anxiety. New York: Academic Press; 1966. [Google Scholar]
- 20.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of health and social behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- 21.Williams DR, Yan Y, Jackson JS, et al. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of health psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 22.Bromberger JT, Matthews KA. A longitudinal study of the effects of pessimism, trait anxiety, and life stress on depressive symptoms in middle-aged women. Psychology and aging. 1996;11:207–213. doi: 10.1037//0882-7974.11.2.207. [DOI] [PubMed] [Google Scholar]
- 23.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the life orientation test. Journal of personality and social psychology. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 24.Scheier MF, Wrosch C, Baum A, et al. The life engagement test: Assessing purpose in life. Journal of behavioral medicine. 2006;29:291–298. doi: 10.1007/s10865-005-9044-1. [DOI] [PubMed] [Google Scholar]
- 25.Cohen S, Doyle WJ, Skoner DP, et al. Social ties and susceptibility to the common cold. JAMA : the journal of the American Medical Association. 1997;277:1940–1944. [PubMed] [Google Scholar]
- 26.Andersson T, Alfredsson L, Kallberg H, et al. Calculating measures of biological interaction. European journal of epidemiology. 2005;20:575–579. doi: 10.1007/s10654-005-7835-x. [DOI] [PubMed] [Google Scholar]
- 27.McDowell I, Newell C. Measuring health, a guide to rating scales and questionnaires. New York: Oxford University Press; 1996. [Google Scholar]
- 28.Smith YR, Johnson AM, Newman LA, et al. Perceptions of clinical research participation among african american women. Journal of women's health. 2007;16:423–428. doi: 10.1089/jwh.2006.0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gettleman L, Winkleby MA. Using focus groups to develop a heart disease prevention program for ethnically diverse, low-income women. Journal of community health. 2000;25:439–453. doi: 10.1023/a:1005155329922. [DOI] [PubMed] [Google Scholar]
- 30.Brown DR, Fouad MN, Basen-Engquist K, et al. Recruitment and retention of minority women in cancer screening, prevention, and treatment trials. Ann Epidemiol. 2000;10:S13–S21. doi: 10.1016/s1047-2797(00)00197-6. [DOI] [PubMed] [Google Scholar]
- 31.Shavers VL, Lynch CF, Burmeister LF. Racial differences in factors that influence the willingness to participate in medical research studies. Ann Epidemiol. 2002;12:248–256. doi: 10.1016/s1047-2797(01)00265-4. [DOI] [PubMed] [Google Scholar]
- 32.Russell C, Palmer JR, Adams-Campbell LL, et al. Follow-up of a large cohort of black women. American Journal of Epidemiology. 2001;154:845–853. doi: 10.1093/aje/154.9.845. [DOI] [PubMed] [Google Scholar]
- 33.Oleske DM, Kwasny MM, Lavender SA, et al. Participation in occupational health longitudinal studies: Predictors of missed visits and dropouts. Ann Epidemiol. 2007;17:9–18. doi: 10.1016/j.annepidem.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 34.Ahluwalia JS, Richter K, Mayo MS, et al. African american smokers interested and eligible for a smoking cessation clinical trial: Predictors of not returning for randomization. Ann Epidemiol. 2002;12:206–212. doi: 10.1016/s1047-2797(01)00305-2. [DOI] [PubMed] [Google Scholar]
- 35.Troxel WM, Matthews KA, Bromberger JT, et al. Chronic stress burden, discrimination, and subclinical carotid artery disease in african american and Caucasian women. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2003;22:300–309. doi: 10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]
- 36.Mirowsky J. Age, depression, and attrition in the national survey of families and households. Sociological Methods & Research. 2000;28:476–504. [Google Scholar]
- 37.de Graaf R, Bijl RV, Smit F, et al. Psychiatric and sociodemographic predictors of attrition in a longitudinal study: The netherlands mental health survey and incidence study (nemesis) American Journal of Epidemiology. 2000;152:1039–1047. doi: 10.1093/aje/152.11.1039. [DOI] [PubMed] [Google Scholar]
- 38.Rothman KJ, Greenland S, Walker AM. Concepts of interaction. American Journal of Epidemiology. 1980;112:467–470. doi: 10.1093/oxfordjournals.aje.a113015. [DOI] [PubMed] [Google Scholar]
- 39.Szklo M, Nieto FJ. Epidemiology: Beyond the basics. Sudbury, MA: Jones and Bartlett Publishers; 2006. [Google Scholar]
- 40.Herman AA. Toward a conceptualization of race in epidemiologic research. Ethnicity & disease. 1996;6:7–20. [PubMed] [Google Scholar]
- 41.Deeg DJ, van Tilburg T, Smit JH, et al. Attrition in the longitudinal aging study amsterdam The effect of differential inclusion in side studies. Journal of clinical epidemiology. 2002;55:319–328. doi: 10.1016/s0895-4356(01)00475-9. [DOI] [PubMed] [Google Scholar]