Abstract
Social anxiety and eating disorders are highly comorbid. Social appearance anxiety (i.e., fear of negative evaluation of one's appearance), general fear of negative evaluation, and perfectionism have each been proposed as risk factors for both social anxiety disorder and the eating disorders. However, no research to date has examined all three factors simultaneously. Using structural equation modeling in two diverse samples (N = 236; N = 136) we tested a model in which each of these risk factors were uniquely associated with social anxiety and eating disorder symptoms. We found support for social appearance anxiety as a shared risk factor between social anxiety and eating disorder symptoms, whereas fear of negative evaluation was a risk factor only for social anxiety symptoms. Despite significant zero-order relationships, two facets of perfectionism (high standards and maladaptive perfectionism) did not emerge as a risk factor for either disorder when all constructs were considered. These results were maintained when gender, body mass index, trait negative affect, and depression were included in the model. It is possible that treating negative appearance evaluation fears may reduce both eating disorder and social anxiety symptoms.
Keywords: social anxiety, disordered eating, social appearance anxiety, perfectionism, fear of negative evaluation, structural equation modeling, eating disorders
Social Anxiety and Eating Disorder Comorbidity
Eating and anxiety disorders are highly comorbid, with some studies finding up to 83 percent of individuals with an eating disorder also meeting criteria for an anxiety disorder (Godart, Flament, Lecrubier, & Jeammet, 2000; Pallister & Waller, 2008). Social anxiety disorder (SAD) has the highest occurrence of all anxiety disorders in individuals with eating disorders and is significantly more common among individuals with eating disorders than in control groups (Godart et al., 2003; Godart et al., 2000). Further, individuals with SAD are more likely to report disordered eating than controls, and, in individuals with SAD, it has been reported that 20% meet criteria for an eating disorder (Becker, DeViva, & Zayfert, 2004; Godart et al., 2003). The lifetime prevalence of SAD has been reported to be between 23 and 71.4% among individuals with anorexia nervosa (AN)(Godart et al., 2000; Halmi et al., 1991; Hinrichsen, Waller, & van Gerko, 2004) and between 23 and 67.8% among individuals with bulimia nervosa (BN) (Brewerton et al., 1995; Hinrichsen et al., 2004; Laessle & Schulz, 2009) whereas the lifetime prevalence rate of SAD in the general public is significantly lower at approximately 12% (Ruscio et al., 2008).
Clearly, the comorbidity between SAD and eating disorders goes above and beyond SAD being a common mental disorder, suggesting that there may be shared vulnerabilities that confer risk for both SAD and eating disorders. This risk is concerning because within individuals with EDs, SAD is a barrier for help-seeking, a negative prognostic factor for treatment outcomes, and decreases treatment engagement (Buckner, Eggleston, & Schmidt, 2006; Goodwin & Fitzgibbon, 2002). Understanding the nature of this comorbidity may therefore improve treatment success for eating disorders.
Risk Factors for SAD and eating disorders
Research suggests that all mental disorders represent clusters of illness with overlapping genetic and non-genetic risk factors and that these overlapping risk factors may contribute to the high comorbidity rates between disorders (e.g., Fyer & Brown, 2009; Hyman, 2003). To prevent mental disorders and treat individuals with comorbid SAD and eating disorders, it is important to identify the risk factors contributing to these disorders. Given strong but incomplete comorbidity between these disorders (i.e., not every individual with an eating disorder has social anxiety disorder), it seems plausible that there are both specific risk factors (i.e., risk factors that contribute to only one disorder) and shared risk factors between the disorders. Several risk factors have been proposed to contribute to both SAD and eating disorders, and those that have received the most attention to date are perfectionism, fear of negative evaluation, and social appearance anxiety. We will review each of the proposed risk factors below.
Maladaptive and Adaptive Perfectionism
Both socially anxious individuals and those with eating disorders have elevated levels of at least some types of perfectionism as compared with controls (Antony, Purdon, Huta, & Swinson, 1998; Bardone-Cone et al. 2007; Bastiani, Rao, Weltzin, & Kaye, 1995). Perfectionism is posited to contribute to the maintenance of social anxiety (Hope, Heimberg, & Klein, 1990) by priming socially anxious individuals to assume that social interactions will be negative because of their failure to meet a perfect standard (Heimberg, Juster, Hope, & Mattia, 1995). Similarly, several systematic reviews suggest that perfectionism is a risk factor for eating disorders (Bardone-Cone et al., 2007; Jacobi, Hayward, de Zwaan, Kraemer, & Agras, 2004; Stice, 2002).
Research suggests that there are two dimensional aspects of perfectionism (Hewitt, Flett, Turnbull-Donovan, & Mikail, 1991): An adaptive type (e.g., high standards), related to healthy functioning (DiBartolo, Frost, Chang, LaSota, & Grills, 2004) and a maladaptive type (e.g., evaluative perfectionism), related to negative outcomes such as anxiety and depression (DiBartolo, Li, & Frost, 2008). Research has found that maladaptive perfectionism has a strong positive relationship with social anxiety, whereas high standards have a weaker, inverse relationship with social anxiety (Shumaker & Rodebaugh, 2009). Maladaptive perfectionism may be especially relevant to understanding the comorbidity between SAD and eating disorders, whereas high standards might be more relevant for eating disorders because high standards are often seen within individuals with eating disorders (Bastiani et al., 1995; Boone, Soenens, Braet, & Goossens, 2010). Indeed, Bardone-Cone et al., (2007) reports that there are domains of perfectionism that are specific to eating disorders and not other psychopathology (e.g., concerns over mistakes). Maladaptive perfectionism can be conceptualized as critical self-evaluation, whereas adaptive perfectionism may be a healthy drive for personal achievement (DiBartolo et al., 2008).
In a review of the literature on perfectionism, Egan, Wade, and Shafran (2011) suggest that perfectionism may be a transdiagnostic mechanism (i.e., spanning across diagnoses) shared between anxiety (including social anxiety) and eating disorders, in that perfectionism helps explain the co-occurrence of these disorders and treatment of perfectionism prevent both types of symptoms. The earliest (to our knowledge) empirical demonstration of perfectionism as a transdiagnostic process between SAD and eating disorders showed that perfectionism moderated the relationship between social anxiety and bulimic behaviors in a group of individuals with high social anxiety; specifically, Silgado and colleagues (2009) found that individuals who displayed high levels of both social anxiety and perfectionism were most likely to be at risk for bulimic behaviors. However, many questions remain regarding the relationship between perfectionism, social anxiety, and disordered eating.
Fear of negative evaluation
Fear of negative evaluation is the fear that one's self will be judged negatively. Clinical samples of women with eating disorders report higher levels of fear of negative evaluation than controls (Hinrichsen, Wright, Waller, & Meyer, 2003). In a non-clinical sample, Gilbert & Meyer (2003) found that, in a cross-sectional dataset, fear of negative evaluation was associated with drive for thinness over and above depression and prospectively predicted bulimic symptoms (Gilbert & Meyer, 2005). In the social anxiety literature, fear of negative evaluation is considered a cognitive risk factor for social anxiety (Haikal & Hong, 2010). Heimberg, Brozovich, & Rapee (2010) outline a model of social anxiety in which social anxiety stems from heightened fears of negative evaluation in social situations in which the individual may be evaluated. Other research has examined fear of negative evaluation as a potential mediator between social anxiety and disordered eating, (Vander Wal & Thomas, 2004; Wonderlich-Tierney & Wal, 2010) but no study to date has demonstrated evidence for mediation in a dataset with sufficient waves across time to demonstrate temporal precedence, which has been argued is a necessity in tests of mediation (Maxwell & Cole, 2007). Additionally, recent research suggests that fear of negative evaluation is better conceptualized as a shared risk factor for social anxiety and disordered eating, rather than a mediator (Levinson & Rodebaugh, 2012).
Social appearance anxiety
Social appearance anxiety is defined as “the fear that one will be negatively evaluated because of one's appearance”(Hart et al., 2008). Social appearance anxiety is positively correlated with measures of social anxiety and negative body image (Claes et al., 2012), but does not represent mere overlap among these other constructs. Instead, social appearance anxiety taps into a unique proportion of variability in social anxiety beyond negative body image, depression, personality, and affect (Hart et al., 2008; Levinson & Rodebaugh, 2011). Moscovitch (2009) has proposed that perceived flaws in appearance may be one of the core fears causing individuals with SAD to fear public criticism. In the eating disorder field, Rieger et al., (2010) proposed that social evaluation of appearance leads to symptoms such as disordered eating in those individuals who place emphasis on their physical appearance. In support of these propositions, Levinson and Rodebaugh (2012) found that social appearance anxiety was associated with disordered eating over and above four other measures of social anxiety and that social appearance anxiety was a shared risk factor for disordered eating and social anxiety in an undergraduate sample. In a clinical sample, Koskina, Van den Eynde, Meisel, Campbell, and Schmidt (2011) found that individuals with a diagnosis of bulimia nervosa had significantly higher levels of social appearance anxiety than healthy controls, and Claes and colleagues (2011) found that social appearance anxiety was positively related to body mass index (BMI), drive for thinness, and body dissatisfaction in women diagnosed with an eating disorder.
Current Study
In summary, evidence suggests that perfectionism (maladaptive perfectionism and high standards), fear of negative evaluation, and social appearance anxiety may potentially be shared risk factors for social anxiety and eating disorder symptoms. However, only social appearance anxiety and fear of negative evaluation have been tested in the same model, and neither social appearance anxiety nor fear of negative evaluation has yet been tested in a model that included maladaptive perfectionism and high standards. In the current study we tested a combined model of risk in which maladaptive perfectionism, high standards (which may be thought of as adaptive perfectionism), fear of negative evaluation, and social appearance anxiety were included as shared risk factors for social anxiety and disordered eating. In the first sample we tested this model with the inclusion of gender and BMI because these variables are very highly related to disordered eating (e.g., Siever, 1994). We hypothesized that each of these risk factors would be uniquely associated with disordered eating and social anxiety. In the second sample, we sought to replicate the model from Sample 1 and to test if the relationships held over and above trait negative affect and depression.
Methods: Study 1
Participants
Participants were 236 undergraduates from a Midwestern university who were mostly white (n = 211; 90%) women (n = 172; 74%), with a median age of 19.00 years (SD = 1.49). Participants were recruited from an introductory psychology class and completed all measures listed below online. Participants were told the study was exploring anxiety, eating, and personality and were reimbursed with course credit. Portions of this dataset have also been used to test the relationship between social anxiety and avoidance of exercise (Levinson, Rodebaugh, Menatti, & Weeks, 2012), but these results do not overlap with the results presented here.
Measures
The Frost Multidimensional Perfectionism Scale (FMPS)
(Frost, Marten, Lahart, & Rosenblate, 1990) measures several dimensional aspects of perfectionism: Concern over Mistakes, Doubts about Actions, Parental Criticism, Parental Expectations, Personal Standards, and Order and Organization. We used a combination of these subscales to create a measure of adaptive and maladaptive perfectionism as used in previous research (Frost et al., 1993; DiBartolo et al., 2004). The Maladaptive Evaluative Concerns (MEC) subscale sums items from the Concern over Mistakes, Doubts about Actions, Parental Criticism, and Parental Expectations subscales. The MEC assesses critical self-evaluation and perceptions of parentally influenced perfectionism. An example item is People will probably think less of me if I make a mistake. The MEC is related to indicators of poor psychological functioning, such as self-concealment and depression (DiBartolo et al., 2008). We used the MEC subscale as a measure of maladaptive perfectionism (see Introduction for details). For adaptive perfectionism we used the Pure Personal Standards (PPS) subscale that includes the Personal Standards subscale items that are least related to fear of negative evaluation (DiBartolo et al., 2004) and represent a measure specifically of high standards. An example item is I set higher goals for myself than most people. We utilized this scoring because confirmatory factor analyses suggest that an adaptive and maladaptive perfectionism facet exhibit the best fit versus a single factor structure for the FMPS(Cox, Enns, & Clara, 2002). All internal consistencies for measures ranged from good to excellent and can be found on the diagonal of Table 1.
Table 1.
Zero-order correlations and internal consistencies between risk factors and social anxiety symptoms and disordered eating in Study 1.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | 0.01 (2.54) | 0.01 (1.91) | 40.76 (14.84) | 21.35 (7.08) | 57.07 (14.88) | 16.68 (4.15) | 24.15 (4.92) | |
| 1. ED symptoms | .80 | |||||||
| 2. Social Anxiety | .41** | .89 | ||||||
| 3. SAA | .68** | .64** | .96 | |||||
| 4. FNE | .48** | .64** | .64** | .87 | ||||
| 5. MPERF | .34** | .35** | .35** | .35** | .77 | |||
| 6. HSTAND | .11 | -.09 | .05 | -.01 | .23** | .84 | ||
| 7. BMI | .33** | .07 | .23** | .16* | .01 | .04 | ------- | |
Note. ED symptoms = eating disorder symptoms: composite of the EDI-2 body dissatisfaction, bulimic symptoms, and drive for thinness subscales; Social Anxiety = composite of the Straightforward Social Interaction Anxiety Scale and Social Phobia Scale; SAA = Social Appearance Anxiety; FNE = Fear of Negative Evaluation; MPERF = Maladaptive Perfectionism (from the Frost Multidimensional Perfectionism Scale); HSTAND = High Standards (from the Frost Multidimensional Perfectionism Scale); BMI = Body Mass Index. Cronbach's alpha is on the diagonal. BMI has no internal consistency.
p < .01
p < .05.
The Brief Fear of Negative Evaluation (BFNE) scale
(Leary, 1983) is a 12-item version of the original Fear of Negative Evaluation scale (Watson & Friend, 1969). The items (e.g., I am afraid others will not approve of me; I am usually worried about what kind of impression I am making on someone) assess fear of negative evaluation. The BFNE has been shown to correlate positively with other measures of social anxiety and has excellent psychometric properties both in college and clinical samples when the four reverse scored items are excluded, as they are here (for a discussion of the improved validity of the BFNE with removal of reverse-scored items please see Rodebaugh et al., 2011).
The Social Appearance Anxiety Scale (SAAS)
(Hart et al., 2008) is a 16-item measure developed to assess anxiety about being negatively evaluated by others because of one's overall appearance, including body shape. Research on the psychometric properties of the SAAS demonstrated high test-retest reliability, good internal consistency, and good factor validity, incremental validity (e.g., it was uniquely associated with social anxiety above and beyond negative body image indicators), and divergent validity in college age samples (Hart et al., 2008 Levinson & Rodebaugh, 2011). Example items from the SAAS are I am concerned people would not like me because of the way I look and I am afraid that people find me unattractive.
Social anxiety symptom composite
To create a measure of social anxiety disorder symptoms we standardized and summed scores on the Social Interaction Anxiety Scale and Social Phobia Scale (see scale information below). We decided to use this method because composite measures provide a more reliable estimate of the construct (Zeller & Carmines, 1980) and can simplify the number of analyses conducted; this method has been used in previous social anxiety studies (Clark et al., 2003; Clark et al., 2006) and has previously been used to combine these specific measures for an overall measure of both social interaction and specific social situation fears (Levinson & Rodebaugh, 2012). Further, research has supported the idea that both these scales represent a higher order construct of social anxiety (Safren, Turk, & Heimberg, 1998).
The Social Interaction Anxiety Scale (SIAS)
(Mattick & Clarke, 1998) is a 20-item measure designed to assess social interaction anxiety. The items describe anxiety-related reactions to a variety of social situations (e.g., I have difficulty talking with other people; I am tense mixing in a group). Overall, research on the scale suggests good to excellent reliability and good construct validity (Heimberg & Turk, 2002). When used for statistical analyses, the three reverse-scored items are omitted, as available evidence suggests that these items fail to load on the same factor as the other items (S-SIAS; Rodebaugh, Woods, Heimberg, Liebowitz, & Schneier, 2006) and appear less related to social anxiety and more related to extraversion than is desirable (Rodebaugh, Woods, & Heimberg, 2007). Removal of the reverse-scored items has no negative effects on the validity of the scale, and generally improves convergent validity (Rodebaugh et al., 2011). In the current study, internal consistency was excellent (α = .93).
The Social Phobia Scale (SPS)
(Mattick & Clarke, 1998) is a 20-item scale designed to assess fear of scrutiny. Items ask about fears of being scrutinized during routine activities (e.g., I would get tense if I had to carry a tray across a crowded cafeteria; I become anxious if I have to write in front of other people). The SPS has been shown to have high levels of internal consistency, and test-retest reliability, and to adequately discriminate between individuals with social phobia and other disorders (i.e., agoraphobia, depression). In the current sample, the internal consistency was excellent (α = .93).
The Eating Disorder Inventory-2 (EDI)
(Garner, Olmstead, & Polivy, 1983) is a 91-item self-report questionnaire designed to measure psychological features commonly associated with anorexia nervosa and bulimia nervosa (e.g., I eat when I am upset; I think about dieting). EDI scores have good internal consistency and good convergent and discriminant validity(Garner et al., 1983) and clinicians frequently use the EDI to assess for eating disorder symptoms (Brookings & Wilson, 1994). We used three of the eleven EDI subscales for this study: the Drive for Thinness (DT), Body Dissatisfaction (BD), and Bulimia (B) subscales. These subscales (the “symptom index”) were used because they assess major vulnerabilities for anorexia nervosa (AN) and bulimia nervosa (BN) and are most frequently used to identify possible eating disorder case status. The DT subscale includes 7 items that assess excessive concern with dieting, preoccupation with weight, and fear of gaining weight. The BD subscale includes 9 items that assess dissatisfaction with overall body shape as well as the size of specific regions of the body, such as hips, stomach, and thighs. The B subscale includes 7 items that assess bulimic behaviors such as bingeing and purging. These three subscales were standardized and combined to create a measure of eating disorder symptoms.
Body Mass Index (BMI)
(kg/m2) was calculated using participants’ self-reported height and weight, as extant research suggests that BMI may influence eating pathology and social anxiety (Fairburn et al., 1998; Jorm et al., 2003; Kowalski, Crocker, & Kowalski, 2001). In general, self-reported weight provides a relatively accurate estimate of current body size or is underestimated leading to more conservative estimates of the impact of BMI on other constructs (Stunkard & Albaum, 1981).
Data Analytic Procedure
Mplus program Version 6.21(Muthén & Muthén, 1998-2010) was used for all structural equation modeling analyses utilizing the maximum likelihood estimator to report standardized path estimates. All other analyses were conducted using SPSS version 19. Model fit was evaluated using the: (a) comparative fit index (CFI)(Bentler, 1990), (b) Tucker-Lewis incremental fit index (TLI)(Tucker & Lewis, 1973), (c) root mean square error of approximation (RMSEA)(Steiger & Lind, 1980), and (d) standardized root mean square residual (SRMR) (Jöreskog, 1979). The magnitudes of these indices were evaluated with the aid of recommendations by Hu and Bentler (1999). For the CFI and TLI, values of .90 and above were considered adequate, whereas values of .95 or above were considered very good; for the RMSEA and SRMR, values of .08 and below were considered adequate and .05 or less very good.
First, we will test a model with only the major variables of interest included (perfectionism, fear of negative evaluation, and social appearance anxiety). We will refer to this model as the first model. Then we will test a model that includes gender and BMI. Finally, we will test a model with all non-significant paths removed. We will refer to this latter model as the final model.
Results: Study 1
Descriptives and Zero-order Correlations
Means, standard deviation, ranges, and correlations of all variables are reported in Table 1. Participant scores on the S-SIAS ranged from very low to very high where a straightforward score of 28 or higher suggests probable social anxiety disorder (Range: 0 to 57; M = 19.26; SD = 11.85; 22% of participants scored above the cutoff, which is similar to what has been reported in other undergraduate samples)(Rodebaugh et al., 2011). Similarly, scores averaged across the eating disorder symptom subscales ranged from very low to very high where EDI scores greater than 42 indicate at-risk or possible eating disorder case status (Range: 5 to 54; M = 22.18; SD = 9.56; 20% of participants scored above the cutoff)(Bennett & Stevens, 1997). This range of scores on the EDI and anxiety scale suggest that we had a wide range of social anxiety and eating disorder scores and probable diagnoses of both disorders within our sample.
All relationships between eating disorder symptoms, social anxiety, maladaptive perfectionism, social appearance anxiety, fear of negative evaluation, and BMI were significant and positive, with the exception of BMI with social anxiety and maladaptive perfectionism (see Table 1). High standards were only significantly related to maladaptive perfectionism. To delineate the unique relationships between these variables we turn to structural equation modeling.
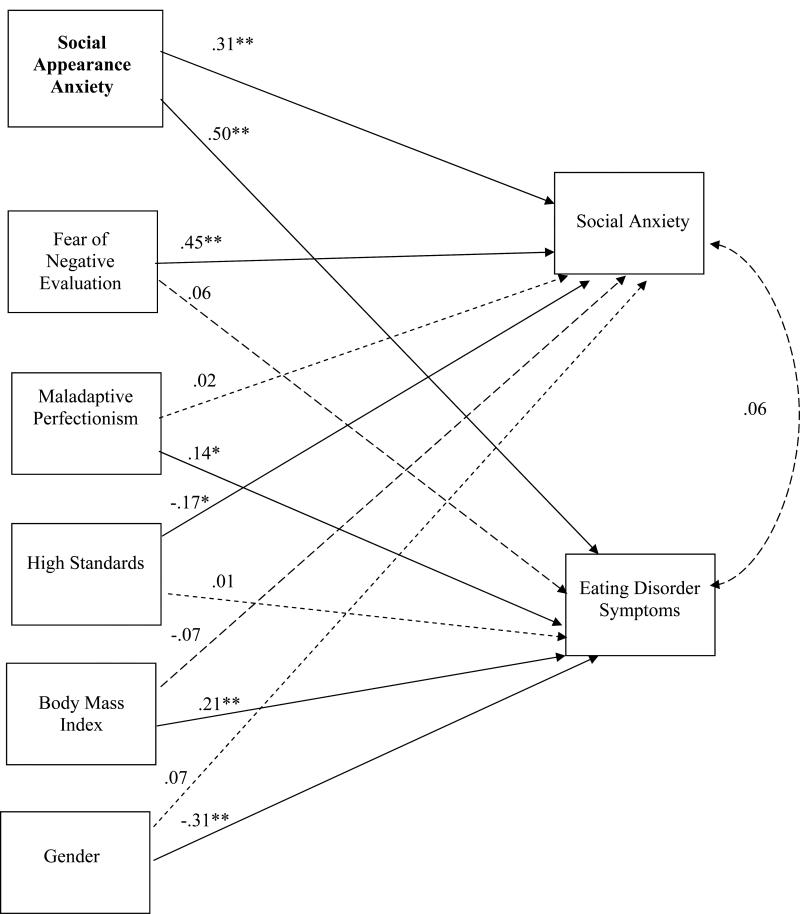
Structural Equation Model
The first model we tested included fear of negative evaluation, maladaptive perfectionism, high standards, and social appearance anxiety as associated with social anxiety and ED symptoms. Social anxiety was uniquely associated with fear of negative evaluation, social appearance anxiety, and high standards (a negative relationship between high standards and social anxiety was expected; see Introduction for details), and the only unique correlate of eating disorder symptoms was social appearance anxiety. In the final model presented in Figure 1, we included gender and BMI. When BMI and gender were included, maladaptive perfectionism was significantly associated with ED symptoms (in addition to BMI and gender). The model fit was perfect because the model was saturated. Thus, to test for model fit we removed all non-significant paths: Fit remained excellent (CFI= 1.00, TLI = 1.00, RMSEA = 0.00, SRMR = 0.02). Additionally, after inclusion of all variables, the relationship between social anxiety and eating disorder symptoms neared zero. We also tested if the relationship between eating disorder symptoms and social appearance anxiety was stronger than the relationship between social anxiety and social appearance anxiety by constraining the paths between social appearance anxiety and the symptom measures (eating and social anxiety) to be equal. Model fit when these paths were equal was significantly worse (CFI = .94, TLI = .86, RMSEA = .13, SRMR = .04; χ2 (1) = 20.78, p < .001), suggesting that social appearance anxiety has a significantly stronger relationship with eating disorder symptoms than social anxiety symptoms. When only women were included in the model (n = 172) the model retained excellent fit (CFI = 1.00,TLI = 1.00, RMSEA = 0.00, SRMR = 0.02), and there were no substantive changes to the relationships between variables: Fear of negative evaluation, social appearance anxiety, and high standards were associated with social anxiety symptoms, whereas maladaptive perfectionism, BMI, and social appearance anxiety were associated with eating disorder symptoms.
Figure 1.
A Model of Risk Factors for Social Anxiety and Eating Disorder Symptoms from Study 1. Solid lines indicate significant relationships; dashed lines indicate non-significant relationships. Bolded risk factors are shared between both disorders. ** p < .01, * p < .05.
Discussion: Study 1
In this study, we found that social appearance anxiety was the only shared risk factor for social anxiety and eating disorder symptoms. Social appearance anxiety had a strong, positive relationship with both social anxiety and eating disorder symptoms, though the relationship with eating disorder symptoms was stronger than with social anxiety. We found that fear of negative evaluation and high standards were uniquely associated with only social anxiety, whereas maladaptive perfectionism was uniquely associated only with eating disorder symptoms. Notably, high standards were associated with social anxiety such that higher standards were related to lower social anxiety. It should also be noted that maladaptive perfectionism was not significantly associated with social anxiety or eating disorder symptoms until gender and BMI were included in the model, suggesting that statistical suppression may be causing maladaptive perfectionism to be significant only when gender and BMI account for part of the variance.
Most noteworthy is that social appearance anxiety was uniquely associated with both social anxiety and eating disorder symptoms over and above perfectionism and fear of negative evaluation. We found this to be true for both a composite of eating disorder symptoms and all three subscales of the EDI-2 separately. However, to be fully confident in these results, we would prefer replication in an independent sample. Additionally, it seemed plausible that the effects of social appearance anxiety could be better accounted for by constructs such as depression and trait negative affect because these constructs are known to be highly correlated with both social anxiety and eating disorders (Heimberg et al., 1995; Mintz, OHalloran, Mulholland, & Schneider, 1997). Thus, we attempted to replicate and extend the model from sample 1 in a second, independent sample.
Methods: Study 2
Participants
Participants were 156 undergraduate women from a large university in the southwestern United States, who were selected because undergraduate women are considered at high risk for the development of an eating disorder. (Taylor et al., 2006) Participants were of diverse ethnicities: White (n = 71; 45.8%), Asian (n = 37; 23.9%), Hispanic (n = 25; 16.1%), Black (n = 15; 9.7%), and other (n = 8; 4.5%), with a median age of 19.00 years (SD = 4.30). Participants were recruited from undergraduate psychology courses for a study examining the relationships between body image, personality, and mood, and completed all study measures online.
Measures
In addition to all Study 1 measures, we used:
The Beck Depression Inventory-II (BDI-2)
(Beck, Steer, & Brown, 1996) is a 21-item self-report measure of depression in adults and adolescents, and in the current study was used to test whether the three risk factors identified in Study 1 were associated with social anxiety and eating disorder symptoms over and above depression. BDI-2 items assess symptoms corresponding to criteria for diagnosing depressive disorders and each symptom is rated for severity based on endorsement of one of a series of statements arranged in order from least to most symptomatic. The BDI-2 has been validated in psychiatric and non-psychiatric (college) samples (Steer, Ball, Ranieri, & Beck, 1997).
The Positive and Negative Affect Schedule-Trait Version
(PANAS) (Watson, Clark, & Tellegen, 1988) is a measure of trait positive (e.g., excited) and negative (e.g., scared) activated affect. Trait affect is assessed through 10 items on a 5-point Likert-type scale from very slightly or not at all (1) to extremely (5). Watson et al. (1988) report good internal consistency, convergent, and discriminant validity. The trait (to what extent you generally feel this way- that is, how you feel on the average) instructions were given. In the current study, the negative affect scale of the PANAS was used to test if the three risk factors identified in Study 1 was associated with social anxiety and eating disorder symptoms over and above trait negative affect.
Results: Study 2
Descriptive Statistics and Zero-order Correlations
Means, standard deviations, ranges, and intercorrelations are presented in Table 2. Participant scores on the S-SIAS (see Measures, Study 1) ranged from very low to very high (Range: 0 to 58; M = 21.18; 28% above the cut-off for SAD). Recalling that a straightforward (reverse scored items removed) score of 28 or higher suggests probable SAD,(Rodebaugh et al., 2011) this suggests that we had a high number of probable diagnoses of SAD within our sample. Internal consistency for both the S-SIAS and SPS was excellent (α = .94 and α = .94). Scores on the eating disorder symptom subscales also ranged from very low to very high in this sample (Range: 0 to 45; M = 20.45). As can be seen in Table 2, all relationships from Study 1 were replicated. Additionally, trait negative affect and depression were significantly related to all measures except BMI and high standards.
Table 2.
Zero-order correlations and internal consistencies between risk factors and social anxiety symptoms and disordered eating in Study 2.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | -0.02 (2.5) | -0.01 (1.92) | 28.62 (13.91) | 19.42 (7.13) | 62.75 (15.42) | 17.79 (3.55) | 22.89 (4.80) | 23.08 (7.63) | 32.50 (9.28) | |
| 1. ED symptoms | .78 | |||||||||
| 2. Social Anxiety | .34** | .89 | ||||||||
| 3. SAA | .51** | .66** | .95 | |||||||
| 4. FNE | .42** | .68** | .79** | .90 | ||||||
| 5. MPERF | .22* | .36** | .37** | .47** | .79 | |||||
| 6. HSTAND | -.09 | -.08 | -.03 | .07 | .36** | .76 | ||||
| 7. BMI | .28** | .14 | .25** | .08 | -.17* | -.04 | ------- | |||
| 8. Trait NA | .32** | .58** | .47** | .49** | .45** | -.08 | -.01 | .86 | ||
| 9. BDI | .45** | .50** | .39** | .37** | .47** | .11 | .01 | .54** | .87 | |
Note. ED symptoms = eating disorder symptoms: composite of the EDI-2 body dissatisfaction, bulimic symptoms, and drive for thinness subscales; Social Anxiety = composite of the Straightforward Social Interaction Anxiety Scale and Social Phobia Scale; SAA = Social Appearance Anxiety; FNE = Fear of Negative Evaluation; MPERF = Maladaptive Perfectionism (from the Frost Multidimensional Perfectionism Scale); HSTAND = High Standards (from the Frost Multidimensional Perfectionism Scale); BMI = Body Mass Index ; Trait NA = Trait Negative Affect; BDI = Beck Depression Inventory; Cronbach's alpha is on the diagonal. BMI has no internal consistency.
p < .01
p < .05.
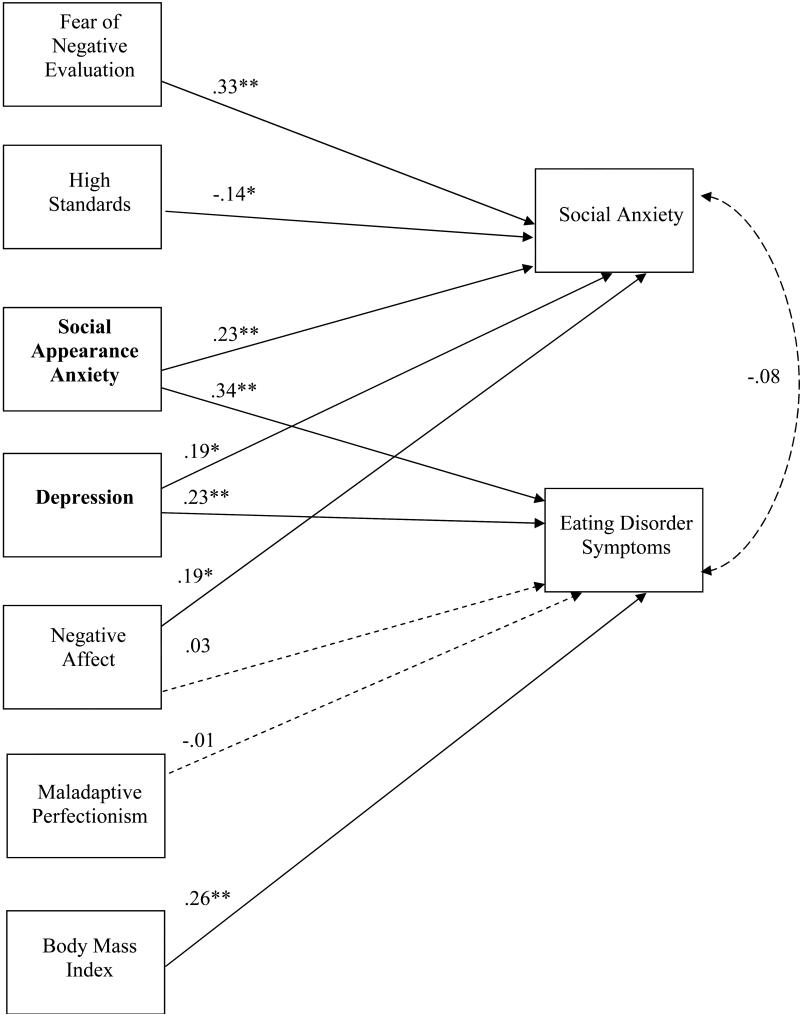
Structural Equation Model Replication and Extension
In Model 1, we replicated the model that was most well supported in Study 1, with all non-significant paths from Study 1 removed so that we could test replication of model fit; however, it should be noted that we did not include gender because all participants were women. This model was not saturated, and retained good to excellent model fit (CFI = .97; TLI = .94; RMSEA = .07; SRMR = .02). All significant paths were replicated, with the exception of maladaptive perfectionism, which was no longer significantly associated with eating disorder symptoms.
In a second model, we added trait negative affect and depression to test if these would account for the relationships between the four risk factors and social anxiety and eating disorder symptoms. This model retained excellent fit (CFI = 1.00; TLI = 1.00; RMSEA = 0.00; SRMR = .01). As seen in Figure 3, all paths that were significant in Model 1 retained their significance. Additionally, depression was uniquely associated with both social anxiety and eating disorder symptoms, whereas negative affect was uniquely associated only with social anxiety. Figure 3 shows all replicated significant paths from Study 1, in addition to all new paths tested in this model (depression and negative affect). When all non-significant paths were removed, the model retained excellent fit (CFI = 1.00; TLI = 1.00; RMSEA = 0.00; SRMR = .01).
Figure 3.
An Extended Model of Risk Factors for Social Anxiety and Eating Disorder Symptoms from Study 2. Trait negative affect and depression are included. Solid lines indicate significant relationships; dashed lines indicate non-significant relationships. Bolded risk factors are shared between both disorders. ** p < .01, * p < .05.
Overall Discussion
Overall, we found that our model of social appearance anxiety, fear of negative evaluation, and perfectionism exhibited excellent fit, and that social anxiety and eating disorder symptoms had no remaining correlation when all risk factors were included. Most strikingly, we found that social appearance anxiety was a shared risk factor for social anxiety and eating disorder symptoms. We found support for this proposition in two distinct samples. Notably, we also found that this relationship remained over and above the inclusion of fear of negative evaluation, maladaptive perfectionism, high standards, gender, BMI, trait negative affect, and depression, suggesting that social appearance anxiety is a unique construct of importance for both social anxiety and eating disorder symptoms. This research adds to a growing body of literature suggesting that social appearance anxiety is a key risk factor for the development of eating disorder symptoms, and may in part explain the high comorbidity between social anxiety and eating disorder symptoms (Levinson & Rodebaugh, 2012). Current results are consistent with research finding that social appearance anxiety is elevated in clinical populations of women with eating disorders (Claes et al., 2012; Koskina et al., 2011).
Regarding the other two proposed risk factors, we found that fear of negative evaluation was uniquely associated with only social anxiety and not eating disorder symptoms. This result is consistent with research that has found fear of negative evaluation to be a core feature of social anxiety, (Haikal & Hong, 2010) but not with research that has found fear of negative evaluation to predict drive for thinness and bulimic symptoms (Gilbert & Meyer, 2003; Gilbert & Meyer, 2005; Utschig, Presnell, Madeley, & Smits, 2010). There are two potential reasons for this discrepancy. First, some research shows that fear of negative evaluation is associated with symptoms of AN, such as drive for thinness, but not bulimic symptoms, (Gilbert & Meyer, 2005) whereas other research shows the opposite (Utschig et al., 2010). Thus, it seems that the relationship between fear of negative evaluation and eating disorder symptoms may depend on what symptoms are measured, in what sample, and under what time period (i.e., one or more than one time period). Second, and perhaps most compelling, is that previous research on fear of negative evaluation has not considered social appearance anxiety. We do not mean to imply that fear of negative evaluation is not important for the eating disorders: Rather, we think that it is very important, but that the more specific form of fear of negative evaluation focusing on appearance may be what drives the relationship between fear of negative evaluation in general and eating disorder symptoms. This latter interpretation is consistent with what we found in the current studies: When social appearance anxiety and general fear of negative evaluation are considered, social appearance anxiety emerges as having the strongest relationship with eating disorder symptoms. Consequently, future research on comorbidity between social anxiety and the eating disorders should include measures of social appearance anxiety.
Against hypothesis, perfectionism was not a shared risk factor for social anxiety and eating disorder symptoms. This finding was true for both maladaptive perfectionism and high standards (or adaptive perfectionism). In Study 1, maladaptive perfectionism was uniquely associated with eating disorder symptoms, but only when BMI was included. On the other hand, high standards were negatively associated with social anxiety symptoms, which is consistent with previous research on high standards and social anxiety (Shumaker & Rodebaugh, 2009). In the second study, we did not find a significant relationship between maladaptive perfectionism and eating disorder or social anxiety symptoms. It may be that a different measurement of perfectionism would have yielded alternate results. However, in every sample we are aware of, various measures of perfectionism correlate moderately to highly, so we find this explanation relatively unsatisfying (Shumaker & Rodebaugh, 2009).
Perfectionism has received significant attention as a potential risk factor, particularly for eating disorders (Bardone-Cone et al., 2007; Jacobi et al., 2004; Stice, 2002). In our models, perfectionism showed comparatively weak unique relationships with eating disorder symptoms. Our perfectionism measure did show significant zero-order relationships with eating disorder symptoms, suggesting that the additional constructs might explain our results. Perhaps perfectionism in the form measured here is primarily a pre-requisite to social appearance anxiety (i.e., social appearance anxiety may mediate the relationship between perfectionism and eating disorder symptoms). Silgado, Timpano, Buckner, and Schmidt (2009) suggested that women may become at risk for bulimic behaviors because they are afraid that others will judge them on their appearance and that they will not reach their perfectionistic standard of appearance. Therefore, it may be that the fear of appearance evaluation (i.e., social appearance anxiety) is what drives the relationship between perfectionism and eating disorder symptoms, rather than perfectionistic standards per se, which may only set the stage for fear of negative appearance evaluation. However, we found that a model including social appearance anxiety as a shared risk factor, fear of negative evaluation as a risk factor for social anxiety, and perfectionism as a risk factor for eating disorder symptoms exhibited excellent fit across two independent samples. This finding suggests that there is some importance to the inclusion of all three of these constructs in a given risk factor model. We hope that future research will continue to clarify the relationships in this model, both over time and with additional variables.
There were several limitations to the research presented here. First, it would be ideal to assess this model in a clinical sample of individuals diagnosed with social anxiety disorder and/or eating disorders. However, we believe that this research is a useful step towards understanding these processes. Undergraduate women are at an increased risk for disordered eating, and eating disorders frequently emerge during these years (Schwitzer, Bergholz, Dore, & Salimi, 1998), thus making this an important population in which to test this model. Furthermore, both samples included a large portion of participants who had clinically significant levels of both social anxiety and disordered eating (between 20-23 percent of both samples). Finally, a limitation worth noting is that these data are cross-sectional. We did not test mediation because of research suggesting that the results of mediation analyses using cross-sectional data do not generalize to longitudinal data (Maxwell & Cole, 2007). Therefore, we cannot state with certainty which of these constructs may lead to others over time. For instance, it may be that negative affect predisposes individuals to develop social appearance anxiety, which eventually leads to disordered eating. This question will be an important next step for research to discover.
Our findings have clinical implications. Many individuals suffer from comorbid SAD and eating disorders (Pallister & Waller, 2008). However, there are few effective treatments for eating disorders, especially for anorexia nervosa (Bulik, Berkman, Brownley, Sedway, & Lohr, 2007) and often times an anxiety disorder may go undetected in the presence of an eating disorder (or vice versa)(Becker et al., 2004). There are, however, efficacious treatments for SAD (Rodebaugh, Holaway, & Heimberg, 2004), especially in the form of exposure therapy. Relatedly, recent arguments have stressed that exposure and response prevention therapy should be integrated into treatment for anorexia nervosa (Steinglass et al., 2011). It seems likely that social appearance anxiety could be an important target for exposure that would respond similarly to other forms of social anxiety. For example, it may be useful to have a patient gradually exposed to evaluation of her appearance by a confederate. Such an exposure would permit learning that the patient can withstand the anxiety experienced from appearance evaluation. Future research should test if these and similar types of exposures are successful in the reduction of disordered eating and social anxiety. Finally, it is worth considering incorporating these types of exposures and discussions around appearance evaluation in prevention efforts targeted at at-risk individuals. In sum, we think that social appearance anxiety is a construct with promising potential avenues for future treatments and prevention efforts that may help alleviate the suffering associated with social anxiety and the eating disorders.
Social anxiety and eating disorders are highly comorbid
Modeled evaluation fears and perfectionism as risk factors for these disorders
Across two samples, social appearance anxiety was a shared risk factor
Results held when including gender, BMI, trait negative affect, and depression
Acknowledgments
This research was funded in part by F31-MH096433-01 to Cheri A. Levinson.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Antony MM, Purdon CL, Huta V, Swinson RP. Dimensions of perfectionism across the anxiety disorders. Behaviour Research and Therapy. 1998;36:1143–1154. doi: 10.1016/s0005-7967(98)00083-7. [DOI] [PubMed] [Google Scholar]
- Bardone-Cone AM, Wonderlich SA, Frost RO, Bulik CM, Mitchell JE, Uppala S, Simonich H. Perfectionism and eating disorders: Current status and future directions. Clinical Psychology Review. 2007;27:384–405. doi: 10.1016/j.cpr.2006.12.005. [DOI] [PubMed] [Google Scholar]
- Bastiani AM, Rao R, Weltzin T, Kaye WH. Perfectionism in anorexia nervosa. International Journal of Eating Disorders. 1995;17:147–152. doi: 10.1002/1098-108x(199503)17:2<147::aid-eat2260170207>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. BDI-II, Beck depression inventory : manual. 2nd ed. Psychology Corporation; San Antonio, TX: 1996. [Google Scholar]
- Becker CB, Deviva JC, Zayfert C. Eating disorder symptoms among female anxiety disorder patients in clinical practice: The importance of anxiety comorbidity assessment. Journal of Anxiety Disorders. 2004;18:255–274. doi: 10.1016/S0887-6185(03)00002-1. [DOI] [PubMed] [Google Scholar]
- Bennett K, Stevens R. The internal structure of the eating disorder inventory. Health Care for Women International. 1997;18:495–504. doi: 10.1080/07399339709516303. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative Fit Indexes in Structural Models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Boone L, Soenens B, Braet C, Goossens L. An empirical typology of perfectionism in early-to-mid adolescents and its relation with eating disorder symptoms. Behaviour Research and Therapy. 2010;48:686–691. doi: 10.1016/j.brat.2010.03.022. [DOI] [PubMed] [Google Scholar]
- Brewerton TD, Lydiard RB, Herzog DB, Brotman AW, O'neil PM, Ballenger JC. Comorbidity of axis I psychiatric disorders in bulimia nervosa. Journal of Clinical Psychiatry. 1995;56:77–80. [PubMed] [Google Scholar]
- Brookings JB, Wilson JF. Personality and Family-Environment Predictors of Self-Reported Eating Attitudes and Behaviors. Journal of Personality Assessment. 1994;63:313–326. doi: 10.1207/s15327752jpa6302_10. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Eggleston AM, Schmidt NB. Social anxiety and problematic alcohol consumption: the mediating role of drinking motives and situations. Behavior Therapy. 2006;37:381–391. doi: 10.1016/j.beth.2006.02.007. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Berkman ND, Brownley KA, Sedway JA, Lohr KN. Anorexia nervosa treatment: A systematic review of randomized controlled trials. International Journal of Eating Disorders. 2007;40:310–320. doi: 10.1002/eat.20367. [DOI] [PubMed] [Google Scholar]
- Claes L, Hart TA, Smits D, Van Den Eynde F, Mueller A, Mitchell JE. Validation of the social appearance anxiety scale in female eating disorder patients. European Eating Disorder Review. 2012;20:406–409. doi: 10.1002/erv.1147. [DOI] [PubMed] [Google Scholar]
- Clark DM, Ehlers A, Hackmann A, Mcmanus F, Fennell M, Grey N, Wild J. Cognitive therapy versus exposure and applied relaxation in social phobia: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74:568–578. doi: 10.1037/0022-006X.74.3.568. [DOI] [PubMed] [Google Scholar]
- Clark DM, Ehlers A, Mcmanus F, Hackmann A, Fennell M, Campbell H, Louis B. Cognitive therapy versus fluoxetine in generalized social phobia: A randomized placebo-controlled trial. Journal of Consulting and Clinical Psychology. 2003;71:1058–1067. doi: 10.1037/0022-006X.71.6.1058. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Enns MW, Clara IP. The multidimensional structure of perfectionism in clinically distressed a nd college student samples. Psychological Assessment. 2002;14:365–373. [PubMed] [Google Scholar]
- Dibartolo P, Li C, Frost R. How Do the Dimensions of Perfectionism Relate to Mental Health? Cognitive Therapy and Research. 2008;32:401–417. [Google Scholar]
- Dibartolo PM, Frost RO, Chang P, Lasota M, Grills AE. Shedding Light on the Relationship Between Personal Standards and Psychopathology: The Case for Contingent Self-Worth. Journal of Rational-Emotive & Cognitive-Behavior Therapy. 2004;22:237–250. [Google Scholar]
- Egan SJ, Wade TD, Shafran R. Perfectionism as a transdiagnostic process: A clinical review. Clinical Psychology Review. 2011;31:203–212. doi: 10.1016/j.cpr.2010.04.009. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Doll HA, Welch SL, Hay PJ, Davies BA, O'connor ME. Risk factors for binge eating disorder - A community-based, case-control study. Archives of General Psychiatry. 1998;55:425–432. doi: 10.1001/archpsyc.55.5.425. [DOI] [PubMed] [Google Scholar]
- Frost RO, Heimberg RG, Holt CS, Mattia JI, Neubauer AL. A comparison of two measures of perfectionism. Personality and Individual Differences. 1993;14:119–126. [Google Scholar]
- Frost RO, Marten P, Lahart C, Rosenblate R. The Dimensions of Perfectionism. Cognitive Therapy and Research. 1990;14:449–468. [Google Scholar]
- Fyer AJ, Brown TA. Stress-induced and fear circuitry anxiety disorders : Are they a distinct group? In: Andrews G, Charney DS, Sirovatka PJ, Regier DA, editors. Stress-induced and fear circuitry disorders: Advancing the research agenda for DSM-V. 1st ed. American Psychiatric Association; Arlington, Va.: 2009. pp. 125–135. [Google Scholar]
- Garner DM, Olmstead MP, Polivy J. Development and Validation of a Multidimensional Eating Disorder Inventory for Anorexia-Nervosa and Bulimia. International Journal of Eating Disorders. 1983;2:15–34. [Google Scholar]
- Gilbert N, Meyer C. Social anxiety and social comparison: differential links with restrictive and bulimic attitudes among nonclinical women. Eating Behaviors. 2003;4:257–264. doi: 10.1016/S1471-0153(03)00026-6. [DOI] [PubMed] [Google Scholar]
- Gilbert N, Meyer C. Fear of negative evaluation and the development of eating psychopathology: A longitudinal study among nonclinical women. International Journal of Eating Disorders. 2005;37:307–312. doi: 10.1002/eat.20105. [DOI] [PubMed] [Google Scholar]
- Godart NT, Flament MF, Curt F, Perdereau F, Lang F, Venisse JL, Fermanian J. Anxiety disorders in subjects seeking treatment for eating disorders: a DSM-IV controlled study. Psychiatry Research. 2003;117:245–258. doi: 10.1016/s0165-1781(03)00038-6. [DOI] [PubMed] [Google Scholar]
- Godart NT, Flament MF, Lecrubier Y, Jeammet P. Anxiety disorders in anorexia nervosa and bulimia nervosa: co-morbidity and chronology of appearance. European Psychiatry. 2000;15:38–45. doi: 10.1016/s0924-9338(00)00212-1. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Fitzgibbon ML. Social anxiety as a barrier to treatment for eating disorders. International Journal of Eating Disorders. 2002;32:103–106. doi: 10.1002/eat.10051. [DOI] [PubMed] [Google Scholar]
- Haikal M, Hong RY. The effects of social evaluation and looming threat on self-attentional biases and social anxiety. Journal of Anxiety Disorders. 2010;24:345–352. doi: 10.1016/j.janxdis.2010.01.007. [DOI] [PubMed] [Google Scholar]
- Halmi KA, Eckert E, Marchi P, Sampugnaro V, Apple R, Cohen J. Comorbidity of psychiatric diagnoses in anorexia nervosa. Archives of General Psychiatry. 1991;48:712–718. doi: 10.1001/archpsyc.1991.01810320036006. [DOI] [PubMed] [Google Scholar]
- Hart TA, Mora DB, Palyo SA, Fresco DM, Holle C, Heimberg RG. Development and examination of the social appearance anxiety scale. Assessment. 2008;15:48–59. doi: 10.1177/1073191107306673. [DOI] [PubMed] [Google Scholar]
- Heimberg R, Juster H, Hope D, Mattia J. Cognitive-behavioral group treatment: Description, case presentation, and empirical support. In: Stein MB, editor. Social phobia: Clinical and research perspectives. American Psychiatric Association; Washington, DC: 1995. pp. 293–321. [Google Scholar]
- Heimberg RG, Brozovich FA, Rapee RM. A cognitive-behavioral model of social anxiety: Update and extension. In: Hofman SG, Di Bartolo PM, editors. Social Anxiety: Clinical, Developmental, and Social Perspectives. 2 ed. Academic Press; Waltham, MA: 2010. pp. 395–422. [Google Scholar]
- Heimberg RG, Turk CL. Assessment of social phobia. In: Heimberg RG, Becker E, editors. Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies. Guilford Press; New York, NY: 2002. pp. 107–126. [Google Scholar]
- Hewitt PL, Flett GL, Turnbull-Donovan W, Mikail SF. The Multidimensional Perfectionism Scale: Reliability, validity, and psychometric properties in psychiatric samples. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3:464. [Google Scholar]
- Hinrichsen H, Waller G, Van Gerko K. Social anxiety and agoraphobia in the eating disorders: associations with eating attitudes and behaviours. Eating Behaviors. 2004;5:285–290. doi: 10.1016/j.eatbeh.2004.04.008. [DOI] [PubMed] [Google Scholar]
- Hinrichsen H, Wright F, Waller G, Meyer C. Social anxiety and coping strategies in the eating disorders. Eating Behaviors. 2003;4:117–126. doi: 10.1016/S1471-0153(03)00016-3. [DOI] [PubMed] [Google Scholar]
- Hope DA, Heimberg RG, Klein JF. Social Anxiety and the Recall of Interpersonal Information. Journal of Cognitive Psychotherapy. 1990;4:185–195. [Google Scholar]
- Hu LT, Bentler PM. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria Versus New Alternatives. Structural Equation Modeling-a Multidisciplinary Journal. 1999;6:1–55. [Google Scholar]
- Hyman SE. Foreward. In: Phillips KA, First MB, Pincus HA, editors. Advancing DSM: Dilemmas in Psychiatric Diagnosis. American Psychiatric Association; Washington, DC: 2003. [Google Scholar]
- Jacobi C, Hayward C, De Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin. 2004;130:19–65. doi: 10.1037/0033-2909.130.1.19. [DOI] [PubMed] [Google Scholar]
- Jöreskog KG. Statistical estimation of structural models in longitudinal-developmental investigations. In: Nesselroade JR, Baltes PB, editors. Longitudinal research in the study of behavior and development. Academic Press; New York: 1979. pp. 303–374. [Google Scholar]
- Jorm AF, Korten AE, Christensen H, Jacomb PA, Rodgers B, Parslow RA. Association of obesity with anxiety, depression and emotional well-being: a community survey. Australian and New Zealand Journal of Public Health. 2003;27:434–440. doi: 10.1111/j.1467-842x.2003.tb00423.x. [DOI] [PubMed] [Google Scholar]
- Koskina A, Van Den Eynde F, Meisel S, Campbell IC, Schmidt U. Social appearance anxiety and bulimia nervosa. Eating and Weight Disorders. 2011;16:e142–145. doi: 10.1007/BF03325321. [DOI] [PubMed] [Google Scholar]
- Kowalski NP, Crocker PRE, Kowalski KC. Physical self and physical activity relationships in college women: Does social physique anxiety moderate effects? Research Quarterly for Exercise and Sport. 2001;72:55–62. doi: 10.1080/02701367.2001.10608932. [DOI] [PubMed] [Google Scholar]
- Laessle RG, Schulz S. Stress-induced laboratory eating be havior in obese women with binge eating disorder. International Journal of Eating Disorders. 2009;42:505–510. doi: 10.1002/eat.20648. [DOI] [PubMed] [Google Scholar]
- Leary MR. A Brief Version of the Fear of Negative Evaluation Scale. Personality and Social Psychology Bulletin. 1983;9:371–375. [Google Scholar]
- Levinson CA, Rodebaugh TL. Validation of the Social Appearance Anxiety Scale: factor, convergent, and divergent validity. Assessment. 2011;18:350–356. doi: 10.1177/1073191111404808. [DOI] [PubMed] [Google Scholar]
- Levinson CA, Rodebaugh TL. Social anxiety and eating disorders: The role of negative social evaluation fears. Eating Behaviors. 2012;13:27–35. doi: 10.1016/j.eatbeh.2011.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson CA, Rodebaugh TL, Menatti A, Weeks JW. Development and validation of the Social Exercise and Anxiety Measure (SEAM): Assessing fears, avoidance, and importance of social exercise. Journal of Psychopathology and Behavioral Assessment. 2012 doi: 10.1007/s10862-012-9326-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy. 1998;36:455–470. doi: 10.1016/s0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- Maxwell SE, Cole DA. Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods. 2007;12:23–44. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- Mintz LB, Ohalloran MS, Mulholland AM, Schneider PA. Questionnaire for eating disorder diagnoses: Reliability and validity of operationalizing DSM-IV criteria into a self-report format. Journal of Counseling Psychology. 1997;44:132–132. [Google Scholar]
- Moscovitch DA. What Is the Core Fear in Social Phobia? A New Model to Facilitate Individualized Case Conceptualization and Treatment. Cognitive and Behavioral Practice. 2009;16:123–134. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. Fifth ed. Muthén & Muthén; Los Angeles, CA: 1998-2010. [Google Scholar]
- Pallister E, Waller G. Anxiety in the eating disorders: understanding the overlap. Clinical Psychology Review. 2008;28:366–386. doi: 10.1016/j.cpr.2007.07.001. [DOI] [PubMed] [Google Scholar]
- Rieger E, Van Buren DJ, Bishop M, Tanofsky-Kraff M, Welch R, Wilfley DE. An eating disorder-specific model of interpersonal psychotherapy (IPT-ED): Causal pathways and treatment implications. Clinical Psychology Review. 2010;30:400–410. doi: 10.1016/j.cpr.2010.02.001. [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Heimberg RG, Brown PJ, Fernandez KC, Blanco C, Schneier FR, Liebowitz MR. More reasons to be straightforward: Findings and norms for two scales relevant to social anxiety. Journal of Anxiety Disorders. 2011;25:623–630. doi: 10.1016/j.janxdis.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodebaugh TL, Holaway RM, Heimberg RG. The treatment of social anxiety disorder. Clinical Psychology Review. 2004;24:883–908. doi: 10.1016/j.cpr.2004.07.007. [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Woods CM, Heimberg RG. The Reverse of Social Anxiety Is Not Always the Opposite: The Reverse-Scored Items of the Social Interaction Anxiety Scale Do Not Belong. Behavior Therapy. 2007;38:192–206. doi: 10.1016/j.beth.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Woods CM, Heimberg RG, Liebowitz MR, Schneier FR. The factor structure and screening utility of the social interaction anxiety scale. Psychological Assessment. 2006;18:231–237. doi: 10.1037/1040-3590.18.2.231. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, Kessler RC. Social fears and social phobia in the USA: results from the National Comorbidity Survey Replication. Psycholgical Medicine. 2008;38:15–28. doi: 10.1017/S0033291707001699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, Turk CL, Heimberg RG. Factor structure of the social interaction anxiety scale and the social phobia scale. Behaviour Research and Therapy. 1998;36:443–453. doi: 10.1016/s0005-7967(98)00032-1. [DOI] [PubMed] [Google Scholar]
- Schwitzer AM, Bergholz K, Dore T, Salimi L. Eating disorders among college women: Prevention, educati on, and treatment responses. Journal of American College Health. 1998;46:199–207. doi: 10.1080/07448489809600223. [DOI] [PubMed] [Google Scholar]
- Shumaker EA, Rodebaugh TL. Perfectionism and social anxiety: Rethinking the role of high standards. Journal of Behavior Therapy and Experimental Psychiatry. 2009;40:423–433. doi: 10.1016/j.jbtep.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siever MD. Sexual orientation and gender as factors in socioculturally acquired vulnerability to body dissatisfaction and eating disorders. Journal of Consulting and Clinical Psychology. 1994;62:252. doi: 10.1037//0022-006x.62.2.252. [DOI] [PubMed] [Google Scholar]
- Silgado J, Timpano KR, Buckner JD, Schmidt NB. Social Anxiety and Bulimic Behaviors: The Moderating Role of Perfectionism. Cognitive Therapy and Research. 2010;34:487–492. [Google Scholar]
- Steer RA, Ball R, Ranieri WF, Beck AT. Further evidence for the construct validity of the Beck Depression Inventory-II with psychiatric outpatients. Psychological Reports. 1997;80:443–446. doi: 10.2466/pr0.1997.80.2.443. [DOI] [PubMed] [Google Scholar]
- Steiger JH, Lind JC. Statistically-based tests for the number of factors.. Paper presented at the Annual Spring Meeting of the Psychometric Society; Iowa City, Iowa. 1980. [Google Scholar]
- Steinglass JE, Sysko R, Glasofer D, Albano AM, Simpson HB, Walsh BT. Rationale for the application of Exposure and Response Prevention to the Treatment of Anorexia Nervosa. International Journal of Eating Disorders. 2011;44:134–141. doi: 10.1002/eat.20784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E. Risk and maintenance factors for eating pathology: A meta-analytic review. Psychological Bulletin. 2002;128:825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Albaum JM. The Accuracy of Self-Reported Weights. American Journal of Clinical Nutrition. 1981;34:1593–1599. doi: 10.1093/ajcn/34.8.1593. [DOI] [PubMed] [Google Scholar]
- Taylor CB, Bryson S, Luce KH, Cunning D, Doyle AC, Abascal LB, Wilfley DE. Prevention of eating disorders in at-risk college-age women. Archives of General Psychiatry. 2006;63:881–888. doi: 10.1001/archpsyc.63.8.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker L, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- Utschig AC, Presnell K, Madeley MC, Smits J. a. J. An investigation of the relationship between fear of negative evaluation and bulimic psychopathology. Eating Behaviors. 2010;11:231–238. doi: 10.1016/j.eatbeh.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Vander Wal JS, Thomas N. Predictors of body image dissatisfaction and disturbed eating attitudes and behaviors in African American and Hispanic girls. Eating Behaviors. 2004;5:291–301. doi: 10.1016/j.eatbeh.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and Validation of Brief Measures of Positive and Negative Affect - the Panas Scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watson D, Friend R. Measurement of social-evaluative anxiety. Journal of Consulting and Clinical Psychology. 1969;33:448–457. doi: 10.1037/h0027806. [DOI] [PubMed] [Google Scholar]
- Wonderlich-Tierney AL, Wal JSV. The effects of social support and coping on the relationship between social anxiety and eating disorders. Eating Behaviors. 2010;11:85–91. doi: 10.1016/j.eatbeh.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Zeller RA, Carmines EG. Measurement in the Social Sciences: The Link Between Theory and Data. Cambridge University Press; New York: 1980. [Google Scholar]