Abstract
Objective
The objective of this study was to examine the role of social support in predicting depression in caregivers of adults aging with spinal cord injuries (SCI).
Design
Cross-sectional secondary data analyses were conducted for this study.
Setting
Participants were recruited from multiple community locations in Pittsburgh, PA and Miami, FL.
Subjects
Community-dwelling caregivers of aging adults with SCI (N=173) were interviewed as part of a multisite randomized clinical trial.
Main measures
The Center for Epidemiological Studies Depression Scale measured caregiver depression symptom levels. A hierarchical multiple regression analysis examined the effect of social support (social integration, received social support, and negative social interactions) on depressive symptoms levels for the caregivers of adults aging with SCI, controlling for demographic characteristics and caregiving characteristics.
Results
Caregivers were, on average, 53 years old (SD=15) and care-recipients were 55 years old (SD=13). Average Center for Epidemiological Studies Depression Scale scores indicated that sixty-nine (40%) caregivers had significant depressive symptoms (mean 8.69, SD=5.5). Negative social interactions (β̂ =.27, P<.01) and social integration (β̂ =−.25, P<.01) were significant independent predictors of depressive symptom levels in caregivers of adults aging with SCI.
Conclusions
Findings demonstrate that negative social interactions and social integration are associated with burden in caregivers of adults aging with SCI. Negative social interactions and social integration should be investigated in assessments and interventions intended to target caregiver depressive symptom levels.
Keywords: Spinal cord injuries, carers, depression, social support
Caregivers of individuals with chronic disabilities, such as individuals with spinal cord injury, experience high levels of psychiatric and physical morbidity,1, 2 including increased risk for mortality.3 A caregiver of an adult ageing with spinal cord injury may be at even greater risk of negative outcomes due to the long duration of the caregiving career and the unique challenges of caring for an adult ageing with a spinal cord injury.
Studies have examined the potential negative outcomes of caregivers’ experiences, with the studies reporting elevated levels of physical stress, emotional stress, burnout, fatigue, anger and resentment, and depression among caregivers of individuals with spinal cord injuries.4, 5 Manigandan et al. reported that 79% of caregivers of individuals with spinal cord injuries demonstrated psychological distress and 18% were depressed.6 Depression in caregivers can lead to difficulties with personal and professional lives, potentially affecting the care-recipients’ participation in daily activities and overall health.
Studies of caregivers of individuals with spinal cord injuries have shown that demographic characteristics (older age, female gender, and compromised health status) 7 and caregiving characteristics (co-residing with care-recipient and recent spinal cord injury) are strongly associated with compromised psychological well-being.
Social support facilitates coping and adjustment to the caregiving role,8, 9 especially as adults are ageing. Three distinct indicators of social support (social integration, received social support, and negative social interactions) have been shown to be related to psychological health. Studies demonstrated that higher levels of social integration (family and friend networks, helping others, confidant relationships, and living arrangements) were associated with better caregiver psychological health.10–13 Additionally, received social support (physical, emotional, and informational support) has the capability to diminish the negative effects of stress and mend psychological health.14 Social support aided psychological health,15 whereas negative social interactions (criticism, neglect, and too many demands made of the caregiver) compromise psychological health.16
While social support has been found to be important to caregivers in other ageing populations, the benefits of social support have not been established in caregivers of adults ageing with spinal cord injuries. Social support is of special interest in this population due to the potential social isolation and decreased social support for caregivers of adults ageing with spinal cord injuries.17 We presume that caregiver demographic characteristics (older age, female gender, and compromised health status) and caregiving characteristics (co-residing with care-recipient and recent spinal cord injuries) will be strongly associated with depression in caregivers of adults ageing with spinal cord injuries; however, the specific contribution of social support to caregiver depression has not been examined.
The purpose of this study was to examine the role of social support (social integration, received social support, and negative social interactions) in predicting depression in caregivers of adults ageing with spinal cord injuries. To accomplish this goal, we conducted a secondary analysis of baseline data from a published randomized-controlled trial examining the impact of a dual target (caregiver and care-recipient) intervention compared to a traditional caregiver-only intervention strategy on the physical and psychological well-being of caregivers and individuals with spinal cord injury.18 We controlled for caregiver demographics and caregiving characteristics in these analyses.
Methods
Community-dwelling caregiver and care-recipient dyads were recruited through radio and television announcements, newspaper articles and advertisements, newsletter articles, and community presentations. Caregivers were defined as individuals who provided physical or emotional support for an ageing adult with a spinal cord injury. Dyads participated in a two-site (Pittsburgh, Pennsylvania and Miami, Florida) randomized clinical trial, assessing the efficacy of dyad psychosocial interventions.18 Both sites obtained Institutional Review Board approval. Both members of the dyad provided written informed consent prior to study initiation.
For the parent study, caregivers’ inclusion criteria were as follows: (1) maintained weekly contact with their care-recipient for at least the previous six months, (2) were 18 years old or older, (3) planned to remain in the current community for at least the subsequent six months, (4) had a telephone, and (5) were fluent in English. Care-recipients’ inclusion criteria were as follows: (1) had acquired a spinal cord injury due to injury or disease and had a mobility impairment secondary to the spinal cord injury (2) were 35 years old or older, (3) lived in a community setting for at least one year before, (4) planned to remain in the current community for at least the subsequent six months, (5) had a telephone, and (6) were fluent in English. Dyads exclusion criteria were as follows: (1) were excluded if either member of the dyad had a terminal illness (<6 month life expectancy), (2) were in active cancer treatment other than maintenance use of tamoxifen or leuprolid, (3) were blind or deaf, or (4) had cognitive impairment [defined by the Short Portable Mental Status Questionnaire (≥ 4 errors)].19
All eligible participants in the parent study were included in the secondary analyses. After potential participants were deemed eligible from a telephone screen, trained assessors completed the battery of assessments. Compensation was provided to the dyad upon completion of the baseline assessment ($25).
The primary outcome was the Center for Epidemiological Studies Depression Scale. The Center for Epidemiological Studies Depression Scale is a widely used instrument for assessing the severity of depressive symptoms and includes items measuring depressive affect, somatic symptoms, and general well-being.20–22 The 10 items were rated on a 4-point scale ranging from 0 (experienced rarely or none of the time) to 3 (experienced most or all of the time), and we calculated a total score (range 0–30). Higher scores indicated greater depressive symptoms. Standardized Cronbach’s α was 0.75. On the 10-item Center for Epidemiological Studies Depression Scale, a score of 10 or higher indicates significant depressive symptoms.23 This score is comparable with a score of 16 or greater on the 20-item Center for Epidemiological Studies Depression Scale. Thus, this cutoff score has optimal sensitivity and specificity for depressive symptoms.24
Caregiver demographic characteristics were collected to identify potential confounding factors for depression. These characteristics included age, gender, race, and employment status.
Health status was assessed by asking caregivers to rate their health (1 item) on a 5-point scale ranging from 0 (excellent) to 4 (poor). A higher score indicated a compromised health perception. A recent meta-analysis found a statistically significant relationship between compromised health perception and mortality while controlling for functional status, depression, and co-morbidities.25
Caregiving characteristics collected were relationship to care-recipient and dyad co-residential status. Self-reported care-recipient spinal cord injury neurological level and severity (complete, incomplete, or do not know) were collected to identify potential confounding factors that may impact caregiver depression.
The Katz Index of ADL measured independence in the care-recipient’s ability to bathe, dress, toilet, transfer, maintain continence, and feed.26 The six items were rated dichotomously from 0 (no) to 1 (yes), and we calculated a total score (range 0 – 6). Higher scores indicated more assistance required in activities of daily living. Standardized Cronbach’s α was 0.81.
The Instrumental Activities of Daily Living Scale measured independence in the care-recipient’s ability to use a telephone, shop, prepare food, housekeep, do laundry, obtain transportation, manage medications, and manage finances.27 The items were rated dichotomously from 0 (no) to 1 (yes), and we calculated a total score (range 0 – 8). Higher scores indicated more assistance required in instrumental activities of daily living. Standardized Cronbach’s α was 0.79.
Formal care and services were measured by counting the number of housekeepers, personal care attendants, transportation services, and support services the care-recipient received. The 12 items were rated dichotomously from 0 (no service received) to 1 (service received), and we calculated a total score (range 0–12). Higher scores indicated more in-home support services were received.
Positive aspects of caregiving measured the degree to which caregivers felt useful, needed, appreciated, important, and confident.28 The 11 items were rated on a 5-point scale ranging from 0 (disagree a lot) through 4 (agree a lot), and we calculated a total score (range 0–44). Higher scores indicated a greater sense of positive aspects in caregiving. Standardized Cronbach’s α was 0.86.
We measured the degree to which caregivers experienced stress using a modified version of the risk appraisal measure from the REACH trials.29 The 7 items were rated on a 3-point scale ranging from 0 (never) through 2 (most of the time/always), and we calculated a total score (range 0–14). High scores indicated a greater sense of stress in caregiving. Standardized Cronbach’s α was 0.70.
Social support measures collected were social integration, received social support, and negative social interactions. The Lubben Social Network Index measured social integration experience by the caregiver through the number of individuals the caregiver interacts with monthly, talks with comfortably, and asks assistance from easily.30 The 3 items were rated on a 6-point scale ranging from 0 (no individuals) to 5 (9 or more individuals), and we calculated a total score (range 0 – 15). Higher scores indicated more social integration. Standardized Cronbach’s α 0.76.
Received social support measured social support received by the caregiver through the amount of instrumental (providing assistance), emotional (offering empathy), and informational (giving guidance) support (3 items) received, using a modified version of the social support scale from the REACH trials.29 The 3 items were rated on a 4-point scale from 0 (never) through 3 (very often), and we calculated a total score (range 0 – 9). Higher scores indicated more received social support. Standardized Cronbach’s α was 0.47, signifying distinct indicators of social support.
Negative social interactions measured the experience of negative interactions by the caregiver outside the dyad through demands, critical comments, and questions about personal affairs made by others.31 The 4 items were rated on a 4-point scale ranging from 0 (never) through 3 (very often), and we calculated a total score (range 0–12) where a higher score indicated more negative social interactions experienced. Standardized Cronbach’s α was .81.
Cross-sectional secondary data analyses were conducted for this study using self-reported measures from caregivers of adults ageing with spinal cord injuries. We employed descriptive statistics to describe our sample. We ran frequencies to inspect the distributions of the data. We correlated factors (Pearson and Kendall’s Tau analyses) to examine relationships between depression, demographic characteristics, caregiving characteristics, and social support (social integration, received social support, and negative social interactions). Items frequently cited as contributing to depression (demographics) and items with a moderate correlation strength (r ≥.10, caregiving characteristics) were subsequently entered in a hierarchical multiple regression analysis (Table 1). Next we conducted regression diagnostics to test for outliers and collinearity [variance inflation factor was <10 and tolerance was >.2]. We needed 149 caregivers to provide adequate power (95%; a=.05) to detect a moderate effect size (f2=.20) for 14 variables in the regression analysis. This sample size was determined based on the desire to detect a moderate effect size for rehabilitation research (f2=.20) and was calculated using G*Power 3.0™.
Table 1.
VARIABLE CATEGORIES
| Caregiver Demographics | Caregiving Characteristics | Social Support |
|---|---|---|
| Age (CG) | Formal Care and Services (CR) | Social Integration (CG) |
| Gender (CG) | Positive Aspects of CG (CG) | Received Social Support (CG) |
| Race (CG) | Dyad Co-residential Status (CG/CR) | Negative Social Interactions (CG) |
| Employment Status (CG) | Chronicity of spinal cord injury (CR) | |
| Perceived Health Status (CG) | Stress (CG) |
Note. CG=caregiver. CR=care-recipient.
Results
In the parent study, 459 potential caregiver participants were screened, 262 were excluded, 24 refused (stating they were not interested in study participation or were too busy) and 173 participated. A brief summary of the caregivers can be found in Table 2, but the sample is described in detail elsewhere.18 Caregivers had provided care for an average of 8 years, and care-recipients completed, on average, half of their daily activities independently. At least 86 caregivers (≥50%) assisted care-recipients with the following basic and instrumental activities of daily living: bathing, dressing, continence (bowel and bladder), transferring, shopping, food preparation, housekeeping, laundry, and transportation. Fewer than 86 caregivers (<50%) assisted care-recipients with the following basic and instrumental activities of daily living: feeding, ability to use telephone, managing medications, and managing finances. Sixty-nine (40%) of the caregivers in this study revealed significant depressive symptom levels consistent with high risk for clinical depression.
Table 2.
CAREGIVER DEMOGRAPHICS AND CAREGIVING CHARACTERISTICS
|
n = 173
|
|
|---|---|
| Age, years, x̄±SD | 53±15 |
| CR Age, years, x̄±SD | 55±13 |
| Female | 131(76) |
| Race | |
| White | 128(74) |
| Other | 45(26) |
| Employment | |
| Employment Inside the Home (informal paid caregivers) | 6(4) |
| Employment Outside the Home | 81(47) |
| Unemployed | 86(49) |
| Relationship to individual with spinal cord injury | |
| Spouse | 120(69) |
| Parent | 4(2) |
| Child | 14(8) |
| Other (i.e., sibling or friend) | 34(20) |
| Length of caregiving relationship, years, x̄±SD | 8±9 |
| CR Activities of Daily Living Status (range 0–6)*, x̄ ±SD | 2.85±2.07 |
| CR Instrumental Activities of Daily Living Status (range 0–8)*, x̄±SD | 4.28±2.36 |
| Depression (range 0–30)*, x̄±SD | 8.69±5.5 |
| Perceived Health Status (range 0–4)*, x̄±SD | 1.53±1.00 |
| Formal Care and Services (range 0–12), x̄±SD | 2.10±1.52 |
| Positive Aspects of Caregiving (range 0–44), x̄±SD | 32.82±8.60 |
| Dyad Co-residential Status | 140(81) |
| Chronicity of Spinal Cord Injury | 12.41±12.07 |
| Stress (range 0–14)*, x̄±SD | 3.08±2.32 |
| Social Integration (range 0–15), x̄±SD | 9.08±3.17 |
| Received Social Support (range 0–9), x̄±SD | 2.97±1.78 |
| Negative Social Interaction (range 0–12)*, x̄±SD | 2.35±2.44 |
| CR Level of Spinal Cord Injury | |
| Cervical | 88(51) |
| Thoracic | 59(29) |
| Lumbar | 9(5) |
| Unknown | 25(14) |
| CR Severity of Spinal Cord Injury | |
| Complete | 63(36) |
| Incomplete | 84(49) |
| Unknown | 26(15) |
Note. Values expressed a n(%), unless otherwise noted.
Higher scores indicate negative outcomes. CR=care-recipient. CG=caregiving.
Stress, perceived health status, negative social interactions, social integration, positive aspects of caregiving, received social support, dyad co-residential status, formal care and services, and chronicity of spinal cord injuries were correlated with depression (i.e., r ≥.10) and were included in the model along with demographics (Table 3). Spinal cord injury severity (r=−.09), care-recipient activities of daily living status (r=.08), care-recipient instrumental activities of daily living status (r=.07), caregiver relationship to care-recipient (r=.05), and spinal cord injury level (r=01.) were not correlated with caregiver depression and were not included in the model.
Table 3.
CORRELATES OF CAREGIVER DEPRESSION
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Depression | |||||||||||||||
| 2. Age | −.00 | ||||||||||||||
| 3. Gender‡ | −.08 | .10 | |||||||||||||
| 4. White‡ | .04 | .22† | .06 | ||||||||||||
| 5.Employment Inside Home‡ | −.04 | −.11 | .11 | −.03 | |||||||||||
| 6.Employment Outside Home‡ | −.09 | −.36† | .01 | −.05 | −.18* | ||||||||||
| 7. Perceived Health Status | .38† | .12 | −.07 | −.02 | .12 | −.25† | |||||||||
| 8. Formal Care and Services | .10 | .02 | .08 | −.04 | .02 | .09 | −.02 | ||||||||
| 9. Positive Aspects of CG | −.21† | −.13 | −.10 | −.19† | −.03 | .05 | −.06 | .04 | |||||||
| 10. Dyad Co-Residential Status‡ | .14 | .11 | .14 | .22† | .01 | −.16* | −.04 | −.23 | −.19 | ||||||
| 11. Chronicity of Spinal Cord Injury | −.10 | −.05 | −.01 | −.02 | −.06 | .06 | −.18* | −.11 | .14 | .04 | |||||
| 12. Stress | .43† | −.02 | .02 | .15* | .05 | .00 | .25† | .30† | −.24† | .12 | −.18* | ||||
| 13. Social Integration | −.29† | .08 | .05 | .27† | .00 | .06 | −.06 | −.06 | −.09 | .01 | −.03 | −.17* | |||
| 14. Received Social Support | −.17* | −.08 | −.12 | .06 | −.08 | .05 | .02 | .20† | .18* | −.24 | −.00 | −.15 | .35† | ||
| 15. Negative Social Interactions | .31† | −.30† | −.18† | −.05 | .06 | −.02 | .16† | .13 | .01 | −.17 | −.08 | .13 | −.08 | .12 |
Note.
p≤.05.
p≤.01.
Pearson correlations, unless noted with ‡ (Kendall’s Tau).
CR=care-recipient. CG=caregiver. N/A=Not Applicable.
Caregiver depression was the dependent variable and 14 predictors of depression were included in the regression analyses (Table 4). Regression diagnostics were conducted. No outliers were detected, and the model’s average variance inflation factor was 1.34 and the tolerance ranged between .60 and .92, indicating no collinearity among predictors.
Table 4.
HIERARCHICAL MULTIPLE REGRESSION
| Block 1: Demographics | Block 2: Demographics + Caregiving Characteristics | Block 3: Demographics + Caregiving Characteristics + Social Support | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| β̂ | P | β̂ | P | β̂ | P | |
| Intercept | - | .00 | - | .02 | - | .03 |
| Age | −.12 | .17 | −.11 | .17 | −.02 | .80 |
| Gender, Female | .01 | .93 | −.04 | .60 | −.00 | .96 |
| Race, White | .10 | .19 | .00 | .97 | .10 | .20 |
| Unemployed (ref.) | - | - | - | - | - | - |
| Employment Inside the Home | −.13 | .08 | −.14 | .05 | −.13 | .05 |
| Employment Outside the Home | −.06 | .45 | −.08 | .30 | −.01 | .88 |
| Perceived Health Status | .40 | .00 | .31 | .00 | .30 | .00 |
| Formal Care and Services | .06 | .43 | .06 | .41 | ||
| Positive Aspects of CG | −.10 | .14 | −.10 | .13 | ||
| Dyad Co-residential Status | .15 | .05 | .17 | .02 | ||
| Chronicity of Spinal Cord Injury | .01 | .87 | −.01 | .90 | ||
| Stress | .31 | .00 | .22 | .00 | ||
| Social Integration | −.22 | .00 | ||||
| Received Social Support | −.07 | .34 | ||||
| Negative Social Interaction | .25 | .00 | ||||
| R2adj=.14 | R2adj =.28 | R2adj=.38 | ||||
| ΔR2adj=.14 | ΔR2adj=.10 | |||||
Note. CG=caregiver. ref.=referent.
In block 1, demographic characteristics contributed 14% of the variance in caregiver depression (F6,170=5.75; R2adj=.14, P<.01). Caregiver perceived health status significantly predicted caregiver depression (β̂ =.40, P<.01).
In block 2, caregiving characteristics, after controlling for caregiver demographic characteristics, contributed an additional 14% of the variance in caregiver depression (F11,170=7.02; R2adj=.28, P<.01). Stress (β̂ =.31, P<.01), caregiver perceived health (β̂ =.31, P<.01), dyad co-residential status (β̂ =.15, P<.05), and employment inside the home (informal paid caregivers) (β̂ =−.14, P<.05) significantly predicted caregiver depression.
In block 3, social support, after controlling for caregiving characteristics and caregiver demographic characteristics, contributed significantly (10%) to the variance in caregiver depression (F14,170=8.38; R2adj=.38, P<.01).32 Perceived health (β̂ =.30, P<.01), negative social interactions (β̂ =.25, P<.01), social integration (β̂ =−.22, P<.01), stress (β̂ =.22, P<.01), dyad co-residential status (β̂ =.17, P<.05), and employment inside the home (informal paid caregivers) (β̂ =−.13, P<.05) significantly predicted caregiver depression.
Discussion
Aside from the caregiver’s perceived health status, negative social interactions and social integration were the two strongest factors associated with caregiver depression. Negative social interactions and low social integration were moderately associated with high-levels of depressive symptoms in caregivers of adults ageing with spinal cord injuries.32 Given reports that negative social interactions negatively make an impact on health16 and social integration promotes health,11–13 the strong relationship between social support and depressive symptom levels is not surprising. These findings suggest that social support may be an important target of interventions for reducing caregiver depressive symptom levels.
Perceived health status was the strongest predictor of depression levels in this sample. Studies report strong associations between caregiver health status and poor psychological well-being.7 The nature of this association is unclear. It could be that caregivers with compromised health may find it difficult to fulfill their caregiving duties contributing to depressive symptoms, or that depressive symptoms associated with caregiving may contribute to compromised health.
Additional factors associated with depressive symptoms confirm findings from previous studies. Stress and co-residing with the care-recipient have both been associated with compromised psychological well-being in caregivers. In particular, caregivers of individuals with degenerative diseases cite the need to maintain vigilance when co-residing with a care-recipient and the inability to obtain a reprieve.33–36
Surprisingly, demographic characteristics (age, gender, and race), spinal cord injury level and severity, functional status (basic and instrumental activities of daily living) were not correlated with depressive symptom levels in caregivers in this sample. Studies have reported that demographics, level and severity of injury, and functional status were associated with caregiver poorer quality of life.17, 18, 34 The chronicity of the care-recipient’s spinal cord injury in this sample may account for the differences in findings. Perhaps after the acute adjustment phase, these factors cease to be important, as care-recipient and caregiver dyads have adjusted their daily routines in response to the level and severity of the injury, and associated functional status. Thus, in the chronic phase, caregivers no longer experience depressive symptoms directly due to these factors. However, these adjustments in daily routines may encourage social isolation, and it is the social isolation in the chronic phase that is more directly associated with depressive symptom levels.
Caregivers employment inside the home (i.e., those who received financial support for their in-home caregiving duties) reported higher levels of depressive symptoms. No other known studies examined employment’s impact on the psychological well-being in caregivers of individuals with spinal cord injuries. Employment inside the home and being paid for your caregiving role may be associated with depressive symptoms due to added social isolation resulting from working inside the home and not interacting with peers.
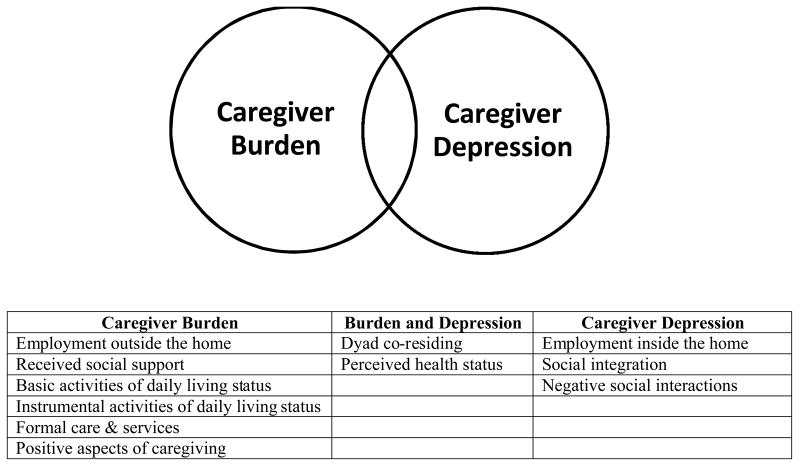
Previously, we conducted analyses that examined predictors of burden using the same sample (Rodakowski, Skidmore, Rogers, Schulz, in press). We assessed depression and burden in separate analyses, estimating that the constructs are moderately related but distinct. By analyzing them separately, we had the opportunity to compare factors associated with caregiver depressive symptom levels and caregiver burden. We discovered similarities and differences between factors associated with depressive symptom levels and burden for caregivers of adults ageing with spinal cord injuries (Figure 1). Employment inside the home, having limited social integration, and having negative social interactions were strongly associated with depressive symptom levels. Employment outside the home, received social support, basic and instrumental activities of daily living, formal care and services, and positive aspects of caregiving were significantly associated with burden. Compromised health status and co-residential status were significantly associated with depressive symptom levels and burden in caregivers of adults ageing with spinal cord injuries. The distinctions in factors associated with depressive symptom levels and burden may illustrate distinctions that can be explored as we identify appropriate targets for interventions directed at reducing caregiver depressive symptom levels and burden.
Figure 1.
Display of significant predictors for burden and depression in caregivers of ageing adults with spinal cord injuries.
These findings show promise, but should be interpreted with caution. The education level of the sample is fairly high, so the sample may not be representative of the population of caregivers of adults ageing with spinal cord injuries. Additionally, selection bias may have occurred when recruiting the sample. Caregivers who were experiencing difficulty may have been more willing to participate in the study, potentially increasing the number of caregivers with higher depressive symptom levels. Finally, these analyses examined cross-sectional data and therefore do not imply causality. It is plausible that caregivers with higher depressive symptom levels are more likely to perceive limited social support, or conversely are more likely to increase their social isolation as a result of their depressive symptoms.
In summary, caregivers of adults ageing with spinal cord injuries may be particularly vulnerable to the adverse effects of social isolation and lack of support. Perceived health, negative social interactions, social integration, dyad co-residential status, and employment status significantly predict depressive symptoms in caregivers of adults ageing with spinal cord injuries. Among these factors, perceived health status, social integration and negative social interactions contributed a significant amount to the caregivers’ depressive symptoms. Interventions addressing these factors should receive high priority in this population, enhancing the caregiver and care-recipient’s mental and physical health.
Clinical messages.
Many caregivers experienced depressive symptom levels consistent with a high risk for clinical depression.
Social support (negative social interactions and social integration) is associated with depressive symptom levels.
Assessments and interventions addressing caregiving for adults ageing with spinal cord injuries should consider social support.
Contributor Information
Juleen Rodakowski, Department of Occupational Therapy, University of Pittsburgh, USA.
Elizabeth R. Skidmore, Email: Skidmore@pitt.edu, Department of Occupational Therapy, Department of Physical Medicine & Rehabilitation, University of Pittsburgh, USA
Joan C. Rogers, Email: Jcr@pitt.edu, Department of Occupational Therapy, University of Pittsburgh, USA
Richard Schulz, Email: Schulz@pitt.edu, Department of Psychiatry, University of Pittsburgh, USA.
References
- 1.Biegel D, Sales E, Schulz R. Family caregiving in chronic illness: Heart disease, cancer, stroke, Alzheimer’s Disease, and chronic mental illness. Newbury Park, CA: Sage Publications; 1996. [Google Scholar]
- 2.Schulz R, Quittner AL. Caregiving for children and adults with chronic conditions: Introduction to the special issue. Health Psychology. 1998;17(2):107–11. [PubMed] [Google Scholar]
- 3.Schulz R, Beach SR. Caregiving as a risk factor for mortality - The caregiver health effects study. J Am Med Assoc. 1999;282(23):2215–9. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 4.Weitzenkamp DA, Gerhart KA, Charlifue SW, et al. Spouses of spinal cord injury survivors: The added impact of caregiving. Arch Phys Med Rehab. 1997;78(8):822–7. doi: 10.1016/s0003-9993(97)90194-5. [DOI] [PubMed] [Google Scholar]
- 5.Shewchuk RM, Richards JS, Elliott TR. Dynamic processes in health outcomes among caregivers of patients with spinal cord injuries. Health Psychology. 1998;17(2):125–9. doi: 10.1037//0278-6133.17.2.125. [DOI] [PubMed] [Google Scholar]
- 6.Manigandan C, Saravanan B, Macaden A, et al. Psychological wellbeing among carers of people with spinal cord injury: a preliminary investigation from South India. Spinal Cord. 2000;38(9):559–62. doi: 10.1038/sj.sc.3101035. [DOI] [PubMed] [Google Scholar]
- 7.Blanes L, Carmagnani MIS, Ferreira LM. Health-related quality of life of primary caregivers of persons with paraplegia. Spinal Cord. 2007;45(6):399–403. doi: 10.1038/sj.sc.3102038. [DOI] [PubMed] [Google Scholar]
- 8.Decker SD, Schulz R. Correlates of life satisfaction and depression in middle-aged and elderly spinal cord-injured persons. Am J Occup Ther. 1985;39(11):740–5. doi: 10.5014/ajot.39.11.740. [DOI] [PubMed] [Google Scholar]
- 9.Anson CA, Stanwyck DJ, Krause JS. Social support and health status in spinal cord injury. Paraplegia. 1993;31(10):632–8. doi: 10.1038/sc.1993.102. [DOI] [PubMed] [Google Scholar]
- 10.Drentea P, Clay OJ, Roth DL, et al. Predictors of improvement in social support: Five-year effects of a structured intervention for caregivers of spouses with Alzheimer’s disease. Soc Sci Med. 2006;63(4):957–67. doi: 10.1016/j.socscimed.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 11.Cohen S, Doyle WJ, Skoner DP, et al. Social ties and susceptibility to the common cold. J AM Med Assoc. 1997;277(24):1940–4. [PubMed] [Google Scholar]
- 12.Seeman TE, Berkman LF, Kohout F, et al. Intercommunity variations in the association between social ties and mortality in the elderly. A comparative analysis of three communities. Ann Epidemiol. 1993;3(4):325–35. doi: 10.1016/1047-2797(93)90058-c. [DOI] [PubMed] [Google Scholar]
- 13.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–5. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 14.Cohen S. Social relationships and health. Am Psychol. 2004;59(8):676–84. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- 15.Berkman LF, Glass T, Brissette I, et al. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51(6):843–57. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 16.Schulz R. Psychosocial Aspects of Aging. In: Halter JB, Ouslander J, Tinetti M, Studenski S, High K, Asthana S, editors. Hazzard’s Geriatric Medicine and Gerontology. New York, NY: McGraw-Hill Inc; 2009. pp. 97–102. [Google Scholar]
- 17.Dreer LE, Elliott TR, Shewchuk R, et al. Family Caregivers of Persons With Spinal Cord Injury: Predicting Caregivers at Risk for Probable Depression. Rehabil Psychol. 2007;52(3):351–7. doi: 10.1037/0090-5550.52.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schulz R, Czaja SJ, Lustig A, et al. Improving the quality of life of caregivers of persons with spinal cord injury: a randomized controlled trial. Rehabil Psychol. 2009;54(1):1–15. doi: 10.1037/a0014932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433–41. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 20.Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: Criterion validity of the 10-item Center for Epidemiological Stuides Depression Scale (CES-D) Archives of Internal Medicine. 1999;159:1701–4. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- 21.Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 22.Dickson A, O’Brien G, Ward R, et al. Adjustment and Coping in Spousal Caregivers Following a Traumatic Spinal Cord Injury: an Interpretative Phenomenological Analysis. J Health Psychol. 2011;17(2):247–57. doi: 10.1177/1359105311411115. [DOI] [PubMed] [Google Scholar]
- 23.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Amer Journal of Prev Med. 1994:10. [PubMed] [Google Scholar]
- 24.Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Arch Intern Med. 1999;159(15):1701–4. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- 25.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. J Gen Intern Med. 2006;21(3):267–75. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of Illness in the Aged. The Index of Adl: A Standardized Measure of Biological and Psychosocial Function. JAMA. 1963;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 27.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–86. [PubMed] [Google Scholar]
- 28.Tarlow BJ, Wisniewski SR, Belle SH, Rubert M, Ory MG, Gallagher-Thompson D. Positive aspects of caregiving - Contributions of the REACH project to the development of new measures for Alzheimer’s caregiving. Res Aging. 2004;26(4):429–53. [Google Scholar]
- 29.Belle SH, Burgio L, Burns R, Coon D, Czaja SJ, Gallagher-Thompson D, et al. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized, controlled trial. Ann Intern Med. 2006;145(10):727–38. doi: 10.7326/0003-4819-145-10-200611210-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lubben F, Ramsden JB. Assessing pre-university students through extended individual investigations: teachers’ and examiners’ views. Int J Sci Educ. 1998;20(7):833–48. [Google Scholar]
- 31.Krause N. Negative interaction and satisfaction with social support among older adults. J Gerontol B Psychol Sci Soc Sci. 1995;50(2):P59–73. doi: 10.1093/geronb/50b.2.p59. [DOI] [PubMed] [Google Scholar]
- 32.Ferguson CJ. An effect size primer: A guide for clinicians and researchers. Prof Psychol-Res Pr. 2009;40(5):532–8. [Google Scholar]
- 33.Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- 34.Post MW, Bloemen J, de Witte LP. Burden of support for partners of persons with spinal cord injuries. Spinal Cord. 2005;43(5):311–9. doi: 10.1038/sj.sc.3101704. [DOI] [PubMed] [Google Scholar]
- 35.Schulz R, Hebert RS, Dew MA, Brown SL, Scheier MF, Beach SR, et al. Patient suffering and caregiver compassion: new opportunities for research, practice, and policy. Gerontologist. 2007;47(1):4–13. doi: 10.1093/geront/47.1.4. [DOI] [PubMed] [Google Scholar]
- 36.Ferrell B, Coyle N. The nature of suffering and the goals of nursing. Oxford ; New York: Oxford University Press; 2008. [DOI] [PubMed] [Google Scholar]